Abstract
Purpose
To investigate the clinical outcomes of endovascular therapy (EVT) in octogenarians and nonoctogenarians with peripheral arterial disease.
Methods
A retrospective analysis of 511 patients (654 affected legs) who underwent EVT between July 2005 and December 2013 was conducted in a prospectively maintained database. Immediate results and long-term vascular outcomes were analyzed and compared between octogenarians and nonoctogenarians.
Results
Octogenarians were more likely to be female and have atrial fibrillation (AF), whereas nonoctogenarians had higher rates of obesity, claudication, and medical comorbidities. There were no differences in the rates of EVT success, 30-day major adverse vascular events, and 6-month functional improvement between groups. Over the 10-year follow-up period, the rates of 3-year limb salvage, sustained clinical success, freedom from major cerebrovascular and cardiovascular events, and composite vascular events were similar between groups, but the survival rate was better in nonoctogenarians than in octogenarians (73% vs 63%, respectively, P=0.004). In Cox regression analysis, dependence on dialysis and AF were significant predictors of death (odds ratio [OR] 4.44 in dialyzed and 2.83 in AF patients), major cerebrovascular and cardiovascular events (OR 3.49 and 2.45), and composite vascular events (OR 3.14 and 2.25).
Conclusion
EVT in octogenarians was feasible, without an increased risk of periprocedural complications. The rates of limb salvage, sustained clinical success, and long-term vascular events were comparable between groups. Dialysis dependence and AF are independent predictors for poor prognosis in patients with peripheral arterial disease. However, these observations require further confirmation in larger scale studies.
Introduction
Patients with peripheral arterial disease (PAD) have significantly increased rates of myocardial infarction (MI), cardiovascular mortality, and stroke.Citation1 Cross-sectional studies have shown that approximately half of all patients with PAD have some clinical evidence of coronary artery disease or cerebrovascular disease.Citation2,Citation3 The risk of mortality and major cardiovascular events (eg, heart attack and stroke) is approximately threefold higher in PAD patients than in those without PAD.Citation4–Citation6
With an aging population and improved quality of medical care, physicians face an ever-increasing number of elderly patients presenting with progressed forms of PAD.Citation7,Citation8 Advanced age is associated with increased perioperative and postoperative mortality after vascular operations because of multiple comorbidities.Citation9–Citation12 Untreated chronic critical limb ischemia (CLI), an advanced stage of PAD, is associated with a dismal prognosis.Citation1,Citation13 On the contrary, CLI patients with successful revascularization have a better quality of life and longer survival when compared to those treated conservatively or with primary amputation.Citation5,Citation14 The wide use of endovascular therapy (EVT) and evidence of better short-term survival compared with bypass surgeryCitation9,Citation10,Citation15 render angioplasty a tempting first-choice treatment in very elderly vascular patients. There are no specific guidelines for the treatment of elderly patients with PAD, and information regarding long-term vascular events following EVT in elderly versus younger patients is scarce in Asian countries.
In this study, we performed a retrospective review using a prospective registry of all patients undergoing EVT at our institution over a 10-year period. We compared the baseline demographics and procedural outcomes between octogenarians and nonoctogenarians. The immediate results, functional improvement, and long-term cardiovascular outcomes were analyzed to determine the safety and effectiveness of EVT between groups.
Methods
Study population
Subjects for this study were derived from the Tzuchi Registry of ENDovascular Intervention for Peripheral Artery Disease (TRENDPAD), which is an ongoing, prospective, physician-initiated, single-center observational registry of patients who underwent EVT for lower limb ischemia starting from July 2005. This database was interrogated to identify adult patients with symptomatic PAD treated between July 2005 and December 2013.
To be eligible for this analysis, patients were required to have an age ≥18 years, provide written consent to participate in this study, and a candidate for EVT originating from atherosclerotic PAD. Patients who had acute limb ischemia, nonatherosclerotic PAD, a life-threatening infection, follow-up duration <3 months in surviving patients, or refused to participate were not eligible. The protocol was approved by the local ethics committee and the institutional review board of Taipei Tzu Chi Hospital (IRB 03-X27-098), and all the study procedures were performed according to good clinical practices and the applicable laws of various governing bodies.
All patients received complete baseline medical examinations before EVT, which included a clinical examination, hemodynamic evaluation (ankle or toe pressure, pulse volume recording, and duplex ultrasound), and anatomic assessment (computed topographic angiography, magnetic resonance angiography, or diagnostic angiography). Toe pressure, pulse volume recording, and Doppler waveform pattern measurements were performed to assess the hemodynamic changes in patients with a falsely elevated ankle brachial index.
Interventions
The interventional procedure was usually conducted using an antegrade or crossover approach, but multiple access sites (brachial or pedal puncture) were used for complex cases. Detailed procedures for endovascular intervention have been described previously.Citation16 Plain balloon angioplasty and bare metal stents were the mainstream treatment in these study participants. With advances in and introduction of new devices, additional procedures including cutting balloons (Boston Scientific, Natick, MA, USA), excimer laser angioplasty (Spectranetics, Colorado Springs, CO, USA), and TurboHawk atherectomy (eV3, Irvine, CA, USA) were performed at the discretion of the operator to obtain better immediate success. Drug-eluting devices, introduced to improve vessel patency in femoropopliteal disease, have been used since November 2011.
The major variables of demographics included in statistical analyses were age at the time of procedure (≥80 years); sex (male); presence of comorbidities including hypertension (systolic blood pressure >140 mmHg or diastolic pressure >90 mmHg), diabetes mellitus (use of oral hypoglycemic agent or insulin, fasting plasma sugar ≥126 mg/dL, or glycated hemoglobin level ≥6.5%), atrial fibrillation (AF), congestive heart failure (CHF) (ejection fraction <40% by echocardiography or radionuclide ventriculography), coronary artery disease (diameter stenosis >50% in at least one of the three main coronary arteries), stroke, and dialysis dependence; and history of smoking (defined as smoking within the previous year). Serum C-reactive protein (CRP) values, determined by high-sensitivity assay, were obtained before EVT or at admission. Normolipidemia was defined as total cholesterol <200 mg/dL or low-density lipoprotein (LDL) cholesterol <100 mg/dL without the use of statin treatment, and baseline serum LDL cholesterol levels were determined using the most recent value within 3 months preprocedure.
Definition and outcome end points
A single-level intervention was defined as EVT for isolated aortoiliac, femoropopliteal, or below-the-knee lesions. A multilevel intervention was defined as EVT in more than one area.
Functional status was classified as ambulatory independently, ambulatory with assistive device, wheelchair-bound, and bed-ridden status. The changes in functional status at presentation and 6 months after EVT were compared between groups.
Nonfatal cardiovascular events included nonfatal MI, stroke, or transient ischemic attack; hospitalization with decompensated heart failure; percutaneous coronary intervention or coronary artery bypass surgery; and hospitalization with angina pectoris or ischemic hands.
Vascular death included fatal stroke, or sudden death due to MI, CHF, AF, nonrheumatic heart valve disease, and ruptured aortic aneurysm.
The safety end point was 30-day major adverse vascular events (MAVEs) (death, MI, stroke, emergent surgery, contrast-induced acute kidney injury requiring dialysis, subacute arterial occlusion, groin complications requiring manual compression or surgical repair, and unplanned reintervention), while efficacy was based on procedure success (successful access and deployment of the device and ≤30% residual stenosis by quantitative angiography with evidence of at least one patent tibial artery to the foot).
Outcomes in follow-up included major cerebrovascular and cardiovascular events (MACCEs) (any death and nonfatal cardiovascular events) and composite vascular events (CVEs) (vascular deaths, nonfatal cardiovascular events, and major amputation). Clinical improvement was defined as a ≥2 Rutherford category improvement, an increase in ankle brachial index (ABI) of at least 0.15, and wound healing in ≤4 months after the index intervention for patients with tissue loss. Sustained clinical success (SCS) was defined as clinical improvement without target vessel revascularization or major amputation (limb loss above the ankle).
Follow-up
At 1 week, 1 month, and thereafter every 3 months after EVT, each patient was assessed by symptoms, ankle or toe brachial pressure index, and duplex ultrasounds. Repeat interventions were performed if recurrent symptoms, significant vessel stenosis (≥70%) with dampened Doppler waveform patterns by duplex ultrasound, and an ABI decrease of ≥0.15 were observed. The main events (death, amputation, failure of SCS, and late vascular events) were documented at discharge and at follow-up visits. If office follow-up visits were not feasible, alternate data sources included telephone interviews, medical records, the local electronic medical database, and the referring physician.
Statistical analysis
All continuous data were expressed as mean ± standard deviation and were analyzed using independent t-tests. A frequency comparison was performed using the chi-square test or Fisher’s exact tests. Variables with P<0.2 in the univariate analyses were backward selected into the multivariate analysis. Independent sample t-test was used to compare the functional changes after EVT between groups. Survival curves, MACCE, and CVE were plotted using the Kaplan–Meier method and analyzed using the log-rank test (SAS software version 9.2; SAS Institute Inc., Cary, NC, USA). A two-tailed P-value of <0.05 was considered significant. Odds ratios (ORs) were given with 95% confidence intervals (CIs).
Results
Study participants
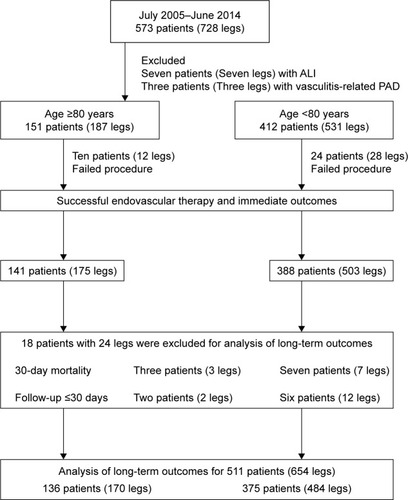
During the study period, 573 patients with 728 affected legs were treated with EVT. Of them, ten patients were excluded (seven with acute limb ischemia and three with vasculitis-related PAD). The remaining 563 patients were divided into two groups based on age (≥80 years or <80 years). Fifty-two patients (64 legs) were not entered into the analysis of long-term outcomes: 34 patients (40 legs) with failed procedures and 18 patients (24 legs) with a follow-up time <30 days or in-hospital mortality. The final cohort for long-term outcome analysis included 136 patients (170 legs) in octogenarians and 375 patients (484 legs) in nonoctogenarians. The flowchart of study participants is shown in .
Baseline patient and lesion characteristics
summarizes the baseline demographics and clinical characteristics between groups. Octogenarians were more likely to be female and have higher incidence of AF, whereas nonoctogenarians were more likely to have diabetes mellitus, dialysis dependence, history of smoking, hyperlipidemia, and a high body mass index (BMI). The hematocrit, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and levels of serum albumin and LDL cholesterol were similar between groups, but nonoctogenarians had higher levels of glycated hemoglobin (6.5%±1.4% vs 7.6%±1.9%, P<0.001) and CRP (3.19±4.94 mg/dL vs 5.13±6.96 mg/dL, P<0.001). Compared to nonoctogenarians, less usage of statin was noted in octogenarians during the follow-up period (21% vs 37%, P=0.001).
Table 1 Baseline demographics
summarizes the lesion characteristics in both groups. The ABI index was lower in octogenarians than in nonoctogenarians (0.46±0.17 vs 0.51±0.20, P=0.002). Octogenarians had more patients presenting with resting pain (26% vs 18%, P=0.022), in contrast with more disabling claudication in nonoctogenarians (12% vs 20%, P=0.008). There was no difference in the presentation of tissue loss between groups. The rates of procedure success, single or multilevel intervention, and stent implantation were similar between groups.
Table 2 Characteristics of the affected limb
Thirty-day outcomes and changes in functional status after EVT
Three patients in octogenarians (two with sepsis and one with rupture of an abdominal aortic aneurysm) and seven in nonoctogenarians (four with sepsis, two with cardiogenic shock, and one with hemorrhagic stroke) died in hospital. Detailed data regarding perioperative complications are shown in . No differences were observed with regard to the number of intensive care unit (ICU) transfers after EVT (8.8% vs 9.5%, P=0.792) and 30-day MAVE rate (12.4% vs 10.3%, P=0.466) between groups. The length of hospital stay was longer in nonoctogenarians than in octogenarians (8±8 vs 11±12 days, P=0.002). Octogenarians included a higher rate of wheelchair-bound patients (68% vs 48%, P<0.001) at presentation; however, percentage changes in functional status after EVT were not different between the groups (P=0.24).
Table 3 Thirty-day outcomes and changes in functional status after EVT
Long-term outcomes
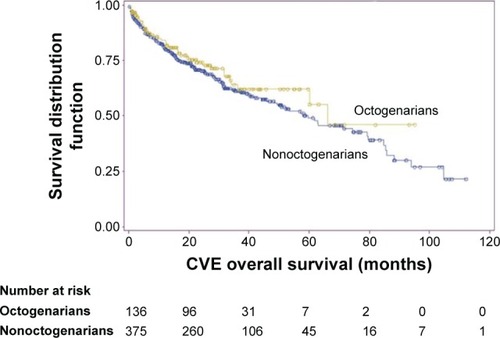
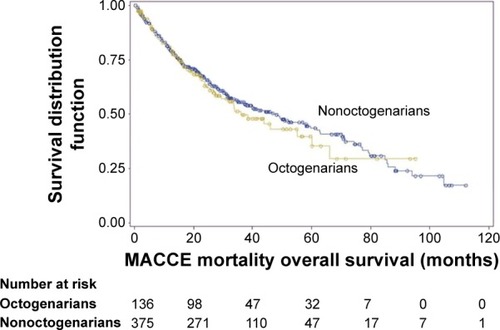
Over a mean follow-up period of 34±25 months (range 3–112), 157 patients died (50 in octogenarians and 107 in nonoctogenarians), and the rates of overall survival in both groups were significantly different at 3 (63% vs 73%) and 5 years (45% vs 67%, P=0.004) (). There were no significant differences between groups in the rates of limb salvage (91% vs 87%, P=0.07) and SCS at 3 years (51% vs 47%, P=0.297). The rates of freedom from cardiovascular death (84% vs 89%, P=0.122), nonfatal cardiovascular events (78% vs 73%, P=0.121), and stroke (86% vs 87%, P=0.504) at 3 years were similar between groups. More octogenarians died owing to noncardiovascular problems, mainly from sepsis followed by malignancy. There were no between-group differences at 3 years in the rates of freedom from MACCEs (50% vs 55%, P=0.47) or CVEs (63% vs 61%, P=0.38) ( and ). However, non-octogenarians had higher rates of nonfatal MI during the follow-up period compared with octogenarians (19% vs 8%, P=0.049). Multivariate analysis showed that the octogenarian factor was not significantly associated with MACCEs or CVEs. Dialysis dependence and AF were strong independent predictors of overall survival (OR 4.44; 95% CI 1.79–11.1; P=0.001 and OR 2.83; 95% CI 1.49–5.35; P=0.001, respectively), MACCE (OR 3.49; 95% CI 1.48–8.19; P=0.004 and OR 2.45; 95% CI 1.31–4.45; P=0.005, respectively), and CVE (OR 3.14; 95% CI 1.32–7.48; P=0.009 and OR 2.25; 95% CI 1.21–4.17; P=0.010, respectively) ().
Table 4 Crude and significant multivariate risk factors for long-term events
Figure 2 Kaplan–Meier curves for overall survival.
Notes: The survival rates for octogenarians and nonoctogenarians were 63% and 73% at 3 years and 45% and 67% at 5 years, respectively (P=0.004). Yellow line and blue line represent octogenarians and nonoctogenarians, respectively.
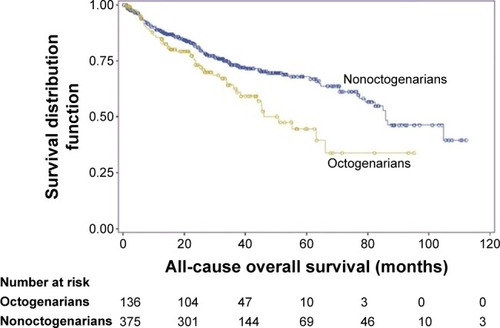
Figure 3 Kaplan–Meier curves for freedom from major cerebrovascular and cardiovascular events (MACCEs).
Notes: The rates of 3-year freedom from MACCEs were similar between groups (50% in octogenarians vs 55% in nonoctogenarians, P=0.564). Yellow line and blue line represent octogenarians and nonoctogenarians, respectively.
Discussion
Our results show that the safety and efficacy of EVT in terms of procedure success, 30-day MAVEs, functional improvement, limb salvage, and SCS are comparable between octogenarians and nonoctogenarians. Although younger patients had more traditional risk factors, age did not increase the risk of long-term vascular events over the 10-year study period. Nonoctogenarians have a survival advantage as compared to octogenarians. Regular dialysis and AF were independent predictors for long-term survival, MACCEs, and CVEs.
PAD is a progressive disease of atherosclerosis, and PAD-related death and disability has increased globally and regionally in the past 20 years.Citation13 There are few reports comparing cardiovascular risk factor profiles between octogenarians and nonoctogenarians, especially in the Asian countries. Our findings that nonoctogenarians with PAD had a higher BMI and more atherosclerotic risk factors are in agreement with an earlier study of octogenarians and septuagenarians, which suggested that younger PAD patients have more comorbid disease.Citation17 On the contrary, more patients with AF and female sex were noted with PAD in octogenarians.
Patients with symptomatic PAD were considered candidates for revascularization, either endovascular or surgical therapy. Untreated chronic CLI, an advanced stage of PAD, is associated with a dismal prognosis.Citation1,Citation13 Instead, patients with CLI who undergo successful revascularization survive longer and experience greater improvements in quality of life when compared to patients treated conservatively or with primary amputation.Citation5,Citation12 The benefits of revascularization may be attenuated when taking into account the aging of the population, which significantly increases the number of elderly patients at high risk of perioperative mortality due to limb-saving procedures, adverse cardiovascular events, and other medical comorbidities.Citation9–Citation12 There are no specific guidelines regarding revascularization procedures in elderly patients with symptomatic PAD. Our study highlights the comparable safety of EVT in both treatment groups. The rates of procedure success, number of ICU transfers, and 30-day MAVEs were similar between groups. Nonoctogenarians had a longer hospital stay when compared to octogenarians, which was related to more tissue inflammation and debridement surgery in these patients. Our results are consistent with previous reportsCitation9–Citation11,Citation14 showing that minimally invasive EVT is safe in octogenarians and does not increase the risk of periprocedural complications as compared to nonoctogenarians. Recent advances in endovascular techniques and devices, coupled with improved quality of medical care, render EVT a tempting first-choice treatment in very elderly vascular patients.
Although more octogenarians, associated with age-related neurologic or musculoskeletal problems, were wheelchair-bound at presentation than nonoctogenarians, no significant difference was found in both groups regarding the changes of functional status 6 months after EVT. These findings suggested that EVT has beneficial effect in improving ambulatory function in elderly patients.
The long-term survival rate of octogenarians in our study remained lower than that of nonoctogenarians (63% and 73% at 3 years and 45% and 67% at 5 years, respectively). Although cardiovascular death remained a major cause of death in this study cohort (35%, 55/157), no differences were observed in subsequent cardiovascular deaths between groups. The leading cause of death in octogenarians was infectious disease (52% due to sepsis and pneumonia), which reflects the impaired immune and functional status in the aging population.
Previous reports have shown that elderly patients are at higher risk of adverse events following PAD treatment because of multiple comorbidities and relatively reduced physiologic reserve.Citation2 However, reported outcomes of EVT for octogenarians mainly focused on mortality, amputation, and reintervention in prior studies.Citation9–Citation15,Citation17,Citation18 Long-term data regarding late CVEs in symptomatic PAD patients are scarce.Citation19 We included major amputation in our CVE outcomes, which led to more PAD-related predictors. In this study, only nonfatal MI reached the marginal significance between groups (P=0.049), which may be associated with the longer life expectancy and more atherosclerosis risk factors in nonoctogenarians. After successful EVT, octogenarians showed no increase in the rates of MACCEs and CVEs as compared to nonoctogenarians. In addition, late vascular events can be prevented by optimal medical care, such as increased use of beta-blockers periprocedure, coupled with antiplatelet agents, statin and angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers during long-term management.Citation20–Citation24
The Cox regression model showed that dialysis dependence and AF are independent risk factors predicting subsequent cardiovascular events despite age stratification. AF is an independent risk factor for survival in patients with CLI.Citation25 In this study, AF remained an independent predictor of survival, MACCE, and CVE outcomes. The prevalence of AF is higher in patients with systemic atherothrombosis.Citation26,Citation27 Severe PAD and a high CHADS2 (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke) scoreCitation28 were observed in many of our patients, which might explain why AF played an important role in late cardiovascular events. Dialyzed patients with PAD have a higher rate of mortality and cardiovascular events.Citation29,Citation30 Despite improved limb salvage from EVT in dialyzed patients with PAD, the overall survival in this group remained poor.Citation31,Citation32 Our results are consistent with prior reports,Citation33,Citation34 wherein dialysis is an important predictor of mortality and subsequent cardiovascular events in PAD patients when other risk factors are adjusted. Traditional risk factors, coupled with vascular inflammation and malnutrition, were associated with general atherosclerosis in dialyzed patients with PAD.
Study limitations
This study has some limitations. First, it was a single-center, observational study using a prospective database. Treatment allocation was made at the discretion of the operator and the patient’s policy of reimbursement. Second, the fact that all patients were treated at a single center in Taiwan opens up the possibility of referral/selection bias based on the current practice of this group. As with all observational studies, the reported association may not represent the underlying causality. The unavoidable risk of selective bias and differences in long-term survival not due to exposure to the treatment being studied threatens the observations made in a cohort study. Third, underutilization of statins may have negatively impacted our ability to prevent late ischemic events, which may relate to reimbursed policy and less hyperlipidemia in octogenarians and dialyzed patients. Finally, we did not investigate the mechanisms underlying the effect of AF on PAD.
Conclusion
In conclusion, EVT in octogenarians is feasible, without an increased risk of periprocedural complications. Nonoctogenarians have a survival advantage as compared to octogenarians. However, the rates of limb salvage, SCS, long-term CVEs, and MACCEs were comparable between groups. Dialysis dependence and AF are independent predictors of long-term survival, MACCEs, and CVEs.
Acknowledgments
The authors thank the cardiac catheterization laboratory medical staff and clinical research coordinators of Taipei Tzu Chi hospital who had participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- HirschATHaskalZJHertzerNRACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease FoundationCirculation200611311e463e65416549646
- HooiJDStoffersHEKnottnerusJAThe prognosis of non-critical limb ischaemia: a systematic review of population-based evidenceBr J Gen Pract199949438495510622019
- HooiJDStoffersHEKesterADRisk factors and cardiovascular diseases associated with asymptomatic peripheral arterial occlusive disease. The Limburg PAOD Study. Peripheral Arterial Occlusive DiseaseScand J Prim Health Care19981631771829800232
- PandeRLPerlsteinTSBeckmanJASecondary prevention and mortality in peripheral artery disease: National Health and Nutrition Examination Study, 1999 to 2004Circulation20111241172321690489
- SmithGDShipleyMJRoseGIntermittent claudication, heart disease risk factors, and mortality. The Whitehall StudyCirculation1990826192519312242518
- Ankle Brachial Index CollaborationAnkle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysisJAMA2008300219720818612117
- FowkesFGRudanDRudanIComparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysisLancet201338299011329134023915883
- DiehmCSchusterAAllenbergJRHigh prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross-sectional studyAtherosclerosis200417299510514709362
- BrosiPDickFDoDDRevascularization for chronic critical lower limb ischemia in octogenarians is worthwhileJ Vasc Surg20074661198120718154996
- DosluogluHHLallPCherrGSSuperior limb salvage with endovascular therapy in octogenarians with critical limb ischemiaJ Vasc Surg200950230531519631865
- ArvelaEVenermoMSöderströmMInfrainguinal percutaneous transluminal angioplasty or bypass surgery in patients aged 80 years and older with critical leg ischaemiaBr J Surg201198451852621271556
- DickPBarthBMlekuschWComplications after peripheral vascular interventions in octogenariansJ Endovasc Ther200815438338918729563
- NorgrenLHiattWRDormandyJAfor TASC II Working GroupInter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)J Vasc Surg200745Suppl SS5S6717223489
- KlevsgårdRRisbergBOThomsenMBA 1-year follow-up quality of life study after hemodynamically successful or unsuccessful surgical revascularization of lower limb ischemiaJ Vasc Surg200133111412211137931
- AdamDJBeardJDClevelandTfor BASIL trial participantsBypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomized controlled trialLancet200536695011925193416325694
- HuangHLChouHHWuTYEndovascular intervention in Taiwanese patients with critical limb ischemia: patient outcomes in 333 consecutive limb procedures with a 3-year follow-upJ Formos Med Assoc20141131068869525240302
- ChangJBSteinTAInfrainguinal revascularizations in octogenarians and septuagenariansJ Vasc Surg200134113313811436086
- JonesDWSiracuseJJGrahamASafety and effectiveness of endovascular therapy for claudication in octogenariansAnn Vasc Surg2015291344125194550
- Van HattumESTangelderMJLawsonJALong-term risk of vascular events after peripheral bypass surgery. A cohort studyThromb Haemost2012108354355322871801
- WestinGGArmstrongEJBangHAssociation between statin medications and mortality, major adverse cardiovascular event, and amputation-free survival in patients with critical limb ischemiaJ Am Coll Cardiol201463768269024315911
- ChungJTimaranDAModrallJGOptimal medical therapy predicts amputation-free survival in chronic critical limb ischemiaJ Vasc Surg201358497298023993439
- LindenauerPKPekowPWangKPerioperative beta-blocker therapy and mortality after major non-cardiac surgeryN Engl J Med2005353434936116049209
- PoldermansDBaxJJKertaiMDStatins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgeryCirculation2003107141848185112695283
- YusufSSleightPPogueJEffects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study InvestigatorsN Engl J Med2000342314515310639539
- ChangSHTsaiYJChouHHClinical predictors of long-term outcomes in patients with critical limb ischemia who have undergone endovascular therapyAngiology201465431532224357434
- WinkelTAHoeksSESchoutenOPrognosis of atrial fibrillation in patients with symptomatic peripheral arterial disease: data from the REduction of Atherothrombosis for Continued Health (REACH) RegistryEur J Vasc Endovasc Surg201040191620385507
- GotoSBhattDLRötherJfor REACH Registry InvestigatorsPrevalence, clinical profile, and cardiovascular outcomes of atrial fibrillation patients with atherothrombosisAm Heart J2008156585586319061698
- GageBFWatermanADShannonWValidation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial FibrillationJAMA2001285222864287011401607
- RajagopalanSDellegrottaglieSFurnissALPeripheral arterial disease in patients with end-stage renal disease: observations from the Dialysis Outcomes and Practice Patterns Study (DOPPS)Circulation2006114181914192217060384
- O’HareAJohansenKLower-extremity peripheral arterial disease among patients with end-stage renal diseaseJ Am Soc Nephrol200112122838284711729255
- NakanoMHiranoKIidaOPrognosis of critical limb ischemia in hemodialysis patients after isolated infrapopliteal balloon angioplasty: results from the Japan below-the-knee artery treatment (J-BEAT) registryJ Endovasc Ther201320111312423391091
- KawaradaOYokoiYHigashimoriAImpact of end-stage renal disease in patients with critical limb ischaemia undergoing infrapopliteal interventionEurointervention201410675376025330507
- SchanzerAMegaJMeadowsJRisk stratification in critical limb ischemia: derivation and validation of a model to predict amputation-free survival using multicenter surgical outcomes dataJ Vasc Surg20084861464147119118735
- OwensCDHoKJKimSRefinement of survival prediction in patients undergoing lower extremity bypass surgery: stratification by chronic kidney disease classificationJ Vasc Surg200745594495217391900