Abstract
Background and purpose
Lacunar infarct (LI) is well known as a heterogeneous primary disorder of cerebral small vessel. Compelling results have demonstrated that age is a risk factor to the prevalence of LI. However, the relationship between age and the prevalence of LI remains obscure. It is essential to note the relationship between age and the prevalence of LI through more clinical data.
Methods
A total of 3,500 patients were included in the case-controlled study. All data were collected from the Examination Center of Magnetic Resonance Imaging, Lu’an People’s Hospital from January 2014 to December 2015. A primary discharge diagnosis of LI was done, and all subjects were evaluated as retrospective data. The relationship between the risk factors and the prevalence of diabetes and the relationship between age and the prevalence of diabetes was analyzed. A chi-square test was used to analyze the associations between different variables. A one-way analysis of variance was used to test the equality of three or more means at one time by using variances. Statistical significance was defined as a P-value of <0.05.
Results
The one-way analysis of variance demonstrated that the prevalence of LI increased with age before 60 years and decreased with age after 69 years. The same results were found in both the male and the female subjects. These results showed that the age-related risk factors (hypertension, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking) have no relationship with the prevalence of LI on the basis of age. There is a significant difference among the different age ranges (P=0.0006). Two-tailed P-value (unpaired t-test) showed the mean significant difference between 30–39 years and 40–49 years (P=0.009) and between 70–79 years and 80–100 years (P=0.0196). F-test (to compare variances) demonstrated that the variances of the different age ranges are significantly different between 30–39 years and 40–49 years (P=0.0002), between 40–49 years and 50–59 years (P=0.0424), and between 70–79 years and 80–100 years (P=0.0003).
Conclusion
The age-related risk factors (hypertension, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking) have no relationship with the prevalence of LI on the basis of age. A decreasing prevalence of LI with aging occurs in the elderly, while the prevalence of LI increases with aging in the young and in adults. This investigation implicates that age is not a risk factor for LI in the elderly.
Keywords:
Introduction
Lacunar infarct (LI), also known as lacunar stroke, is a small stroke that results from damage to, or a blockage of, small size penetrating brain arteries and arterioles that provide blood to the brain’s deep structures within the internal capsule, basal ganglia, thalamus, pons, and cerebral white matter.Citation1 LI may be asymptomatic, showing up only on brain imaging, or may have depression, pure motor, pure sensory, ataxic, or mixed motor and sensory symptoms.Citation2 A large number of results have shown that the prevalence of LI increases with age worldwide.Citation3–Citation5 With the rapid progress of aging, LI will become an important impact on family and is harmful to the society. Therefore, the prevention and treatment of LI are important.
It is well accepted that LI is closely associated with the following risk factors: hypertension, diabetes, cardiovascular diseases, the history of cerebral infarct, smoking, and drinking.Citation6–Citation8 However, the relationship between age and the prevalence of LI remains obscure. It is essential to clarify the relationship between age and the prevalence of LI with more clinical data. We sought to investigate the clinical data of LI from January 2014 to December 2015 at our hospital in Central China and to further clarify the relationship between the prevalence of LI and age. The relationship between the prevalence of LI and the risk factors was also analyzed based on the age. The present clinical investigation has demonstrated that the trend of the prevalence of LI decreases with aging in the elderly after 69 years and increases with aging before 60 years.
Methods
Study design
This case-controlled study was a retrospective cohort analysis implemented in the Examination Center of Magnetic Resonance Imaging, Lu’an People’s Hospital in Lu’an, Anhui Province, People’s Republic of China, which cares for ~70,000 inpatients and 800,000 outpatients per year. Cases of LI were identified by magnetic resonance imaging (MRI) examination, and control were those who did not. The review of patient’s data before its commencement was approved by the institutional medical ethics committee of Renmin Hospital, Hubei University of Medicine. This analysis was executed in accordance with the approved guidelines. The requirement for informed consent was waived due to the retrospective nature of this analysis.
Data collection
The MRI records of adult (≥16 years) patients with LI obtained from the Examination Center of Magnetic Resonance Imaging of our hospital between January 2014 and December 2015 were reviewed. A total of 3,500 patients, which contain all MRI data, were selected from inpatients and outpatients. All selected cases underwent examinations with conventional MRI sequences (including gradient echo sequence T1 and T2, T2 fluid attenuation inversion recovery, or diffusion-weighted imaging). Lacunes were defined by MRI as focal, discrete areas of apparent ischemic infarction measuring >5 mm and <15 mm at diameter. There were no uncertain cases for discussion. The clinical and demographic characteristics of all patients, including their age, sex, risk factors, initial vital signs, laboratory findings, and clinical outcomes, were obtained from the MRI Examination Center.
Statistical analysis
All statistical analyses were performed using SPSS for Windows Version 18.0 (SPSS Inc., Chicago, IL, USA). A chi-square test was introduced to analyze the associations between two different variables. A one-way analysis of variance was used to test the equality of three or more means at one time by using variances. A P-value of <0.005 was taken to indicate statistical significance.
Results
The analysis of age distribution for LI
The total cases were 3,500, including 1,032 LI patients and 2,468 non-LI ones. There are seven age ranges (10–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and 80–100 years), which each age range has 500 cases. In all, 1,032 LI cases included 544 males and 488 females.
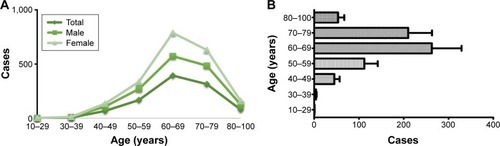
The data showed that the prevalence of LI increased with age before 60 years and decreased with age after 69 years. The same results were found in both the male and the female subjects ( and ). The one-way analysis of variance demonstrated that the prevalence of LI is associated with age, indicating that the prevalence of LI increased with age before 60 years and decreased with age in the elderly after 69 years.
Table 1 The distribution of LI by different age range and sex
The relationship between risk factors and the prevalence of LI
The association between the clinical risk factors and the prevalence of LI on the basis of age had been demonstrated in . These results showed that the age-related risk factors (hypertension, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking) have no relationship with the prevalence of LI on the basis of age. There is a significant difference among the different age ranges in (P=0.0006). Two-tailed P-value (unpaired t-test) showed the mean significant difference between 30–39 years and 40–49 years (P=0.009) and between 70–79 years and 80–100 years (P=0.0196). F-test (to compare variances) demonstrated that the variances of the different age ranges are significantly different between 30–39 years and 40–49 years (P=0.0002), between 40–49 years and 50–59 years (P=0.0424), and between 70–79 years and 80–100 years (P=0.0003). These results indicate that a decreasing prevalence of LI with aging occurs in the elderly, especially after 70 years, while the prevalence of LI increases with aging in the young and adults before 59 years.
Table 2 The relationship between risk factors and the prevalence of LI on the basis of age (one-way analysis of variance)
Table 3 The prevalence of LI according to risk factors on the basis of age (one-way analysis of variance)
Discussion
LI is a small cavitated lesion no larger than 20 mm in diameter in the distal distribution of deep penetrating vessels, including lenticulostriate, thalamoperforating, and pontine perforating arteries.Citation1,Citation9 LI is a common pathological entity that can result in various clinical manifestations in the adult and elderly population. In this study, the one-hospital clinical data were, retrospectively, assayed, and the patients with a diagnosis of LI by MRI were selected from an examination center of MRI. This clinical investigation identified that there was no relationship between the prevalence of LI and the age-related risk factors (hypertension, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking) according to the age range. This study has found that the prevalence of LI increases with age before 60 years and decreases with age after 69 years in the elderly. However, this result is different from the previous reports that the prevalence of LI increases with aging. Therefore, this analysis indicates that aging is not a contributor to the prevalence of LI in the elderly, in spite of the contrary to the precious evidence data that the prevalence of LI is proportional to the progress of age.
Increasing imaging and clinical research has demonstrated that LI is an age-related silent lacunar stroke and a common occurrence in the elderly.Citation10 LI is the most common type of stroke in the Japanese population,Citation11,Citation12 the Caucasian,Citation13 the African American,Citation14 the Caribbean blacks,Citation13,Citation15 the Chinese population,Citation16,Citation17 and worldwide. It was demonstrated that age-specific incidence rates for lacunar stroke in south Alabama were higher in blacks than whites, and highest for black females when the age-adjusted rates for initial stroke were 109 per 100,000 for whites and 208 per 100,000 for blacks,Citation18 indicating the black/white differences in stroke rate.Citation19 It was also found that African Americans have more lacunar stroke and more severe prestroke disability than Caucasians.Citation20,Citation21 Increasing studies pointed to the racial differences in ischemic cerebrovascular disease, including lacunar stroke.Citation15,Citation20,Citation22,Citation23 Clinical data evidenced that the racial differences in lacunar stroke are associated with the different diet, lifestyle, habits, air pollution, and so on, interfering with the age-related involvement.Citation15,Citation21,Citation23 Compelling clinical studies evidenced that LI has an age-adjusted incidence comparable with the incidence of large vessel atherosclerotic stroke.Citation24–Citation26 The trend of LI prevalence is increasing with age.Citation25,Citation27 Different from these previous research results, this investigation found that the prevalence of LI increases with age before 60 years and decreases with age after 69 years in the elderly, suggesting that aging is not a contributor to the prevalence of LI in the elderly after 69 years. The implications of these findings may require different interventions in the elderly.
It is well known that LI is the most important small vessel cerebrovascular disease, accounting for 20%–25% of all ischemic strokes.Citation6,Citation28 LI has been involved in the two major vascular pathologies with small size penetrating brain arteries and arterioles: thickening of the arterial media and obstruction of penetrating arteries.Citation1,Citation29 Considering that the prevalence of LI increases with age before 60 years and decreases with age after 69 years in the elderly, we inferred the pathogenesis of LI that age around 60 years is a fragile and vulnerable period to be easy to induce the small vascular pathologies and the occurrence of LI. It is possible that “lacune” ever cavitated from LI will be gradually absorbed and disappeared with the progress of aging. Therefore, it may be important to have a comprehensive prevention for LI before and during the fragile and vulnerable period. This study is not a randomized and controlled investigation; therefore, further studies have to be performed to determine these conclusions.
Acknowledgments
This work was supported by grants from the Natural Science Foundation of Hubei Province (2015CFB260), and the Hubei Province Health and Family Planning Scientific Research Project (WJ2015MB219) and the Shiyan Natural Science of Renmin Hospital, Hubei University of Medicine to Dr Zhiyou Cai.
Disclosure
The authors report no conflicts of interest in this work.
References
- CaplanLRLacunar infarction and small vessel disease: pathology and pathophysiologyJ Stroke20151712625692102
- WuRHLiQTanYLiuXYHuangJDepression in silent lacunar infarction: a cross-sectional study of its association with location of silent lacunar infarction and vascular risk factorsNeurol Sci201435101553155924752391
- SunXGWangTZhangNYangQDLiuYHIncidence and survival of lacunar infarction in a southern Chinese population: a 7-year prospective studyBrain Inj201529673974425830283
- KoppelmansVVernooijMWBoogerdWPrevalence of cerebral small-vessel disease in long-term breast cancer survivors exposed to both adjuvant radiotherapy and chemotherapyJ Clin Oncol201533658859325559803
- BasileAMPantoniLPracucciGLADIS Study GroupAge, hypertension, and lacunar stroke are the major determinants of the severity of age-related white matter changes. The LADIS (leukoaraiosis and disability in the elderly) studyCerebrovasc Dis2006215–631532216490940
- LiYLiuNHuangYWeiWChenFZhangWRisk factors for silent lacunar infarction in patients with transient ischemic attackMed Sci Monit20162244745326864634
- YanBPengLDongQReverse-dipper pattern of blood pressure may predict lacunar infarction in patients with essential hypertensionEur J Neurol20152261022102525614275
- ShinDWLeeKBSeoJYAssociation between hypertriglyceridemia and lacunar infarction in type 2 diabetes mellitusJ Stroke Cerebrovasc Dis20152481873187826004860
- NgMSinghPUse of lacunar infarction as a marker of small vessel diseaseEur J Neurol2015223e3925677457
- PalacioSMcClureLABenaventeORBazanC3rdPergolaPHartRGLacunar strokes in patients with diabetes mellitus: risk factors, infarct location, and prognosis: the secondary prevention of small subcortical strokes studyStroke20144592689269425034716
- HiroseTHashimotoMTotsuneKAssociation of (pro)renin receptor gene polymorphisms with lacunar infarction and left ventricular hypertrophy in Japanese women: the Ohasama studyHypertens Res201134453053521228785
- TaguchiAMikiMMutoAAssociation between oral health and the risk of lacunar infarction in Japanese adultsGerontology201359649950623942139
- CorbinDOPoddarVHennisAIncidence and case fatality rates of first-ever stroke in a black Caribbean population: the Barbados register of strokesStroke20043561254125815087558
- NyquistPABilgelMSGottesmanRExtreme deep white matter hyperintensity volumes are associated with African American raceCerebrovasc Dis201437424425024686322
- KochSGuptaRMcClendonMSRomanoJGRacial-ethnic differences in lacunar infarction in a multiethnic stroke populationJ Stroke Cerebrovasc Dis201322210711221821432
- TsaiCFAndersonNThomasBSudlowCLRisk factors for ischemic stroke and its subtypes in Chinese vs Caucasians: systematic review and meta-analysisInt J Stroke201510448549325907735
- TsaiCFThomasBSudlowCLEpidemiology of stroke and its subtypes in Chinese vs white populations: a systematic reviewNeurology201381326427223858408
- GrossCRKaseCSMohrJPCunninghamSCBakerWEStroke in south Alabama: incidence and diagnostic features – a population based studyStroke19841522492556701932
- FridayGLaiSMAlterMStroke in the Lehigh Valley: racial/ethnic differencesNeurology1989399116511682771065
- SinghRCohenSNKruppRAbediAGRacial differences in ischemic cerebrovascular diseaseJ Stroke Cerebrovasc Dis19987535235717895112
- HassaballaHGorelickPBWestCPHansenMDAdamsHPJrIschemic stroke outcome: racial differences in the trial of danaparoid in acute stroke (TOAST)Neurology200157469169711524481
- HajatCDundasRStewartJACerebrovascular risk factors and stroke subtypes: differences between ethnic groupsStroke2001321374211136911
- WolmaJNederkoornPJGoossensAVergouwenMDvan SchaikINVermeulenMEthnicity a risk factor? The relation between ethnicity and large- and small-vessel disease in White people, Black people, and Asians within a hospital-based populationEur J Neurol200916452252719222554
- ZhangCWangYZhaoXChinese IntraCranial AtheroSclerosis Study GroupFactors associated with severity of leukoaraiosis in first-ever lacunar stroke and atherosclerotic ischemic stroke patientsJ Stroke Cerebrovasc Dis201423102862286825280817
- LawrenceESCoshallCDundasREstimates of the prevalence of acute stroke impairments and disability in a multiethnic populationStroke20013261279128411387487
- Le PiraFGiuffridaSGiammonaGSaponaraRLanzaSLa SpinaVLeukoaraiosis and lacunar infarcts in ischemic stroke: role of age and vascular risk factorsAnn Ital Med Int199712272759284598
- KitagawaKMiwaKYagitaYOkazakiSSakaguchiMMochizukiHAssociation between carotid stenosis or lacunar infarction and incident dementia in patients with vascular risk factorsEur J Neurol201522118719225164480
- ForsterAMurleBBohmeJPerfusion-weighted imaging and dynamic 4D angiograms for the estimation of collateral blood flow in lacunar infarctionJ Cereb Blood Flow Metab Epub20151014
- ArakiYKumakuraHKanaiHPrevalence and risk factors for cerebral infarction and carotid artery stenosis in peripheral arterial diseaseAtherosclerosis2012223247347722766330