Abstract
Osteoarthritis (OA) is a degenerative disorder resulting from loss of joint cartilage and underlying bone and causes pain and loss of function. The treatment of knee OA is still a challenge because of the poor self-regeneration capacity of cartilage. The nonsurgical interventions include control of the aggravating factor (such as weight control and the use of walking aids), symptomatic treatment (such as acetaminophen or nonsteroidal anti-inflammatory drugs), prolotherapy, and viscosupplementation. However, the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) has not been widely used because of lack of clinical evidence and several limitations in patients with severe knee OA. Three patients who suffered from knee pain and poor walking endurance were diagnosed with advanced knee OA. They underwent PRP treatment in association with intra-articular HA injection and showed pain relief and functional improvement. The follow-up standard weight-bearing X-ray images of knees also confirmed the improvement and indicated the possibility of regeneration of the articular cartilage. These cases provide clinical and radiographic evidence for a new therapy for advanced knee OA. This treatment strategy of PRP in association with HA injection can offer a chance to treat severe knee OA, rather than immediate surgery, or a chance for those who cannot undergo surgery. It can also postpone the need of arthroplasty and can significantly improve the daily activity function.
Introduction
Osteoarthritis (OA) is a degenerative disorder resulting from loss of joint cartilage and underlying bone.Citation1 Articular cartilage is an avascular connective tissue and serves as a buffer material to weight-bearing and shearing forces together with the unique extracellular matrix, which is composed of high concentration of proteoglycans, polymeric hyaluronic acid (HA), and link protein. Under stimulation with repetitive mechanical injury, the elevated inflammatory cytokines, produced by fibroblast-like synovial cells, macrophage-like synovial cells, and chondrocytes such as interleukin (IL)-1 and tumor necrosis factor alpha result in a significant effect of cartilage damage.Citation1 Knee OA is the major cause of lower extremity disability in elderly adults, especially people older than 45 years.Citation2 Besides causing local pain, stiffness, and swelling, knee OA is also one of the most common causes of low back pain and decreased quality of life.Citation3
The 2013 treatment guideline of the American Academy of Orthopedic SurgeonsCitation4 strongly recommends conservative treatments such as physical therapy, aerobic exercises, weight control, and neuromuscular education. Medications and injections are also the treatment choice but they have the disadvantages of systemic side effects and short-term efficacy. The difficulty in treatment of knee OA is mainly due to the lack of an effective therapy to reverse the degeneration of joint cartilage. In the case of severe knee OA, joint replacement may be the final solution.
Viscosupplementation (such as HA), prolotherapy (such as dextrose), platelet-rich plasma (PRP) therapy, and stem cell therapy have been considered for the treatment of knee OA to increase tissue healing and to slow down the progression of degeneration.Citation4 High-molecular-weight HA is a natural disaccharide polymer that can mimic the synovial fluid. In addition to supporting joint lubrication, HA can inhibit the inflammatory process and stimulate cartilage regeneration.Citation5–Citation8 PRP is collected from the patient’s blood. After centrifugation and separation, PRP contains four to six times the native platelet count and high dose of growth factors; PRP is believed to have the capability to promote tissue repair and regeneration.Citation9 The trials of comparing PRP and HA have shown that PRP had better quality and quantity of pain relief than HA in mild-to-moderate OA but had equal effects in severe OA.Citation6,Citation10,Citation11 Both prolotherapy and viscosupplementation with either PRP or HA have shown limited effectiveness in severe knee OA.
However, the combination of PRP and HA had not been widely used because of lack of clinical evidence. Moreover, the treatment with PRP and HA still has many limitations, especially in patients with severe knee OA. We report three cases with severe knee OA. The patients received PRP in association with HA injection, and the follow-up via X-ray imaging documented the possibility of cartilage regeneration.
Case presentation
Methods
The authors obtained written consent of the patients to describe their illness and publish this case report. We did not use patients’ data that could allow identifying them. Three patients with knee OA underwent PRP therapy in association with intra-articular HA injection at the outpatient department of the China Medical University Hospital from March to October 2014. PRP was prepared using SEPAX system (Biosafe SA, Eysins, Switzerland). An amount of 200 mL venous blood was drawn from the patient into the blood bag containing 22 mL of the anticoagulant citrate phosphate dextrose adenine (CPDA-1, USP) solution (JMS Singapore Pte., Ltd., Singapore). Each 100 mL of CPDA-1 contains 0.299 g citric acid (anhydrous), 2.63 g sodium citrate (dihydrate), 0.222 g monobasic sodium phosphate (monohydrate), 3.19 g dextrose (monohydrate), and 0.0275 g adenine. PRP, platelet-poor plasma, and red blood cells were collected individually after 20 minutes of processing using the generic volume reduction protocol (SEPAX). An amount of 20 cc PRP was drawn aseptically into four 5 cc sterile syringes. Subsequently, each patient was injected in the following areas: intra-articular, pes anserine, medial collateral, and lateral collateral ligament attachments. A total of 10 cc PRP (including 5 cc intra-articular injection) was used per knee joint at each visit.
Two different kinds of HA were used in these patients based on their personal insurance policy and practicability. Two of three patients were injected with Hyalgan® (molecular weight of 5.0–7.3×105 Da, 20 mg/2 mL; Fidia Farmaceutici S.p.A., Abano Terme, Italy), and the other patient was injected with Ostenil® (molecular weight of 1.2–1.4×106 Da, 10 mg/mL; TRB Chemedica AG, Munchen, Germany).
The subjective pain intensity over bilateral knees, which was rated with a visual analog scale (VAS), was assessed based on the patient’s subjective feeling before and after treatment. The VAS is a horizontal line, 100 mm in length, anchored by the words “No pain” at the left side and “Very severe pain” at the right side. The patient was asked to mark a point on the line that she felt represented her perception of her current pain state. The score was determined by measuring in millimeters from the left end of the line to the point that the patient marked.
Two functional indexes, the Lequesne index and the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index, were used to evaluate the patients’ clinical symptoms. The Lequesne index ranges from 0 to 24. A score ≥14 indicates extremely serious functional disability, and scores >11, 8–10, 5–7, and 1–4 indicate very severe, severe, moderate, and minor functional disability, respectively. The WOMAC index ranges from 0 to 96. It has three main sections: pain (total: 20 points), stiffness (total: eight points), and physical functional disability (total: 68 points). Higher scores relate to severe symptoms and worse function.
The joint space width (JSW) was measured as the minimum distance in the medial tibiofemoral compartment using a computer-automated measurement software in the follow-up knee X-rays, which were filmed in the full weight bearing, standing, and fully extended anteroposterior (AP) view with a fixed X-ray beam.
Case descriptions
Case 1
A 77-year-old female with no previous history of trauma or knee surgery visited our outpatient department in October 2007. Her body weight was 50 kg and height was 152 cm (body mass index [BMI]: 21.6 kg/m2). She complained of lower back pain and painful sensation over bilateral knees during walking for several years. The VAS was 63 mm in resting and aggravated up to 85 mm when squatting down and climbing stairs. Poor walking endurance and lower back soreness were also noted in the daytime. The physical examination showed varus deformity, crepitus, and bulking over bilateral knees. The Lequesne index was rated 11 and the WOMAC index was rated 77 ().
Table 1 The characteristics of the three cases, before and after treatment
She received regular physical therapy, oral nonsteroidal anti-inflammatory drug, and glucosamine sulfate plus intra-articular HA (Hyalgan®) injection once a week for three times every 6 months for 3 years. However, she still suffered from recurrent knee pain and showed no improvement in walking endurance. She lost to follow-up for 3 years and came back to our outpatient department again in October 2014 with similar symptoms and body weight. The follow-up bilateral standard extended weight-bearing X-ray images of knees in that visit revealed grade IV–V OA change (). The minimum JSW values of right and left medial tibiofemoral compartment were 0.30 mm and 0.21 mm, respectively ().
Figure 1 Standard weight-bearing knee X-rays of a 77-year-old female before (A) and 8 months after (B) one course of intra-articular PRP in association with HA injection, showing the increase in medial joint space (white arrows).
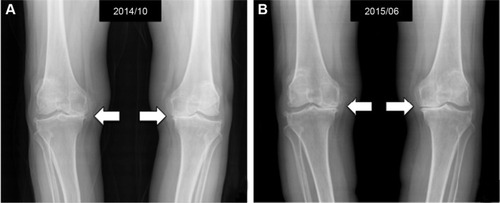
We arranged PRP injection in the same visit, followed by intra-articular HA (Hyalgan®) injection for each knee once a week for three times separately in the total 6 weeks of treatment course. No obvious body weight change was observed during this period. After completing the treatment course, she kept receiving the medication with glucosamine (Camine®, crystalline glucosamine sulfate [314 mg per capsule]; Purzer pharmaceutical Co., Ltd., Taipei, Taiwan), one capsule three times a day for 3 months, and then started another 6-week course of intra-articular HA (Hyalgan®) injection from April 2015 to June 2015. She reported marked improvement of walking endurance and decreased bilateral knee pain. The VAS was improved to 12 mm when resting and 23 mm when climbing stairs. The Lequesne index was rated 7 and the WOMAC index was rated 34 (). The follow-up standard weight-bearing X-ray images in June 2015 also showed an increase in minimal JSW from 0.30 mm to 0.91 mm over the right side and from 0.21 mm to 0.52 mm over the left side of the medial tibiofemoral compartment (, ).
Case 2
A 69-year-old female, whose body weight was 66 kg and height 155 cm (BMI: 27.4 kg/m2), suffered from bilateral knee pain and gait disturbance for years and visited a physical medicine and rehabilitation clinic in March 2014. She had tenderness over bilateral medial knees with VAS at 50 mm in resting status. The painful sensation had aggravated when going down stairs and squatting down with VAS at 87 mm. She also showed poor walking endurance. The Lequesne index was rated 14 and the WOMAC index was rated 88 (). The standard weight-bearing X-ray images of knees in that visit showed significant narrowing of medial joint space with minimal JSW values of 0.32 mm and 0.46 mm over the right and left medial tibiofemoral compartment, respectively (, ).
Figure 2 Standard weight-bearing knee X-rays of a 69-year-old female before (A) and 15 months after (B) one course of intra-articular PRP in association with HA injection, showing significant improvement in the narrowing joint space (white arrows).

PRP injection was arranged at that time, followed by 3 weeks of intra-articular HA (Hyalgan®) injection course for each knee separately (once a week on one knee, a total of 6 weeks). During the next clinic visit, she reported being pain free when resting and decreased tenderness (VAS =30 mm) when doing activity. Her body weight had no change compared to that in the initial visit. The Lequesne index was rated 8 and the WOMAC index was rated 30 (). The follow-up standard weight-bearing X-ray images of bilateral knees showed significant improvement in the narrowing joint space with minimal JSW values of 0.60 mm and 0.49 mm over the right and left medial tibiofemoral compartment, respectively (, ).
However, multiple tender points over bilateral medial collateral ligament and pes anserine were observed. Thus, she received 25% dextrose prolotherapy injection over those tender points each week for 2 months. She also received physical therapy in our clinic, but the symptoms of knee OA had not been reported to progress.
Case 3
A 76-year-old female, who suffered from bilateral knee pain and gait disturbance for years, visited a physical medicine and rehabilitation clinic in March 2014. Her body weight was 63 kg and height was 158 cm (BMI: 25.2 kg/m2). No obvious change was observed during the next visit. She complained of whole knee tenderness, especially at the medial side. Limitation of range of motion and aggravated pain while going down stairs were noted. The VAS was 81 mm. The Lequesne index was rated 16 and the WOMAC index was rated 64 (). The standard weight-bearing X-ray images of bilateral knees showed femorotibial OA and knee OA grade V at the right knee and grade IV at the left knee (). The minimal JSW values of the medial compartment were 0.55 mm and 1.09 mm over the right and left knees, respectively ().
Figure 3 Standard weight-bearing knee X-rays of a 76-year-old female before (A) and 1 year after (B) two courses of intra-articular PRP in association with HA injection, showing more significant bone spur growth and the cartilage remains at a healthy size with the normal joint space (white arrows).

She received PRP injection, followed by 3 weeks of intra-articular HA (Ostenil®) injection course for bilateral knees separately (once a week on bilateral knees, a total of 3 weeks) in March 2014. The symptoms were improving but still she had tenderness and impaired walking endurance. Therefore, she received another course of PRP plus HA (Ostenil®) injection in August 2014. The tenderness over medial knee and walking endurance were improving but still she had no complete relief, with VAS being 50 mm. She was followed up two times in the clinic for intra-articular HA (Ostenil®) injection in December 2014. PRP injection once over bilateral knees in January 2015 was also arranged. She mentioned that the knee pain was completely relieved after the aforementioned treatment. However, the follow-up standard weight-bearing X-ray images of bilateral knees showed more significant bone spur growth but with improved joint space narrowing, with JSW values of 5.50 mm and 5.20 mm over the right and left knees, respectively (, ).
Discussion
According to recent studies, OA is a result of progressive loss of joint cartilage and leads to a “whole joint” disease, which includes loss of articular cartilage, synovitis, subchondral bone remodeling, and osteophyte formation; OA also results in pain and loss of function.Citation12,Citation13 The treatment of knee OA is still a challenge because of the poor capacity for self-regeneration of cartilage. Before performing joint replacement, nonsurgical interventions are arranged to relieve the pain and to improve the physical functions. These nonsurgical interventions include control of the aggravating factor, symptomatic treatment, prolotherapy, and viscosupplementation.Citation14
Radiography is currently the most widely used method that can classify the severity of knee OA using the Kellgren and Lawrence system or the Ahlbäck classification system.Citation15 In 1999, the US Food and Drug Administration claimed JSW as a reliable marker to tracking the progression of knee OA in the guidance of treatment of OA.Citation16 However, there are still several different opinions about using JSW in standing AP view to follow the progression of cartilage damage. The sensitivity of JSW measured in standing extended AP view was challenged, and more evidence indicated that a flexion AP view (knee flexion 20°–30°) is a better choice to measure the JSW.Citation17 The correlation between JSW and cartilage thickness is also controversial. Cicuttini et alCitation18 concluded that the narrowing of JSW might reflect meniscal extrusion rather than the loss of volume of cartilage. Despite these arguments, regular measurement of joint space narrowing on standard weight-bearing X-ray images of the knees should be the appropriate primary end point for follow-up and demonstration of treatment efficacy.
Sampson et alCitation9 injected PRP in 14 patients with primary or secondary OA and measured the cartilage thickness via ultrasound. The result showed increased cartilage thickness in six patients. Many case series and at least four randomized controlled trials concluded PRP injection as an effective and safe therapy in knee OA treatment, with only limited complication of transient pain and swelling after procedure.Citation10,Citation11,Citation19 PRP is believed to have the potential to provide pain relief and functional improvement in 6–9 months after injection, with therapeutic effects up to 24 months; this reduction in pain is due to the capability of PRP to promote the proliferation of chondrocytes, stimulate the production of synovial fluid, and limit the inflammatory response.Citation7,Citation19–Citation21 Further subgroup analysis revealed the better outcomes of pain relief in a group of younger patients with early OA. Kon et alCitation22 published a case series of PRP injection including 91 patients of knee OA and showed less improved result in the high degree of OA classification (Kellgren–Lawrence IV) in the final follow-up result. A similar result was also reported by the same authors in a prospective comparative study; the further analysis showed that only patients with early OA have better results.Citation23 Filardo et alCitation24 and Jang et alCitation25 also confirmed this result and suggested the role of PRP as a safe and effective therapy in a group of younger patients with early OA. The hypothesis is that few living chondrocytes indicate less response to the growth factor. Furthermore, severe OA indicates the irreversible change of the joint damage, in which PRP may have only little influence.Citation23
Similar to that of PRP, the evidence of intra-articular HA injection also indicates less improvement of pain in advanced knee OA. A systematic review by Trigkilidas and AnandCitation26 concluded that intra-articular HA injection is efficacious for pain control in mild-to-moderate knee OA. Kon et alCitation23 published a 2- and 6-month follow-up clinical comparative study with similar findings; the intervention effective peak was at ∼6–8 weeks and the residual effectiveness was up to 6 months. However, HA injection serves as a transient synovial fluid supplement when endogenous HA in the synovial joint decreases in concentration and production during the process of degeneration; HA injection also provides further metabolic anti-inflammatory effects by normalizing the synthesis of endogenous HA and induces chondroprotection.Citation5,Citation7,Citation27 Some case series have already reported the positive result of combined HA and PRP for pressure sore and wound healing.Citation28–Citation30 The positive result showed that the chondroprotective effect of intra-articular HA might offer a better environment for cartilage regeneration. Considering the promotion of the few living chondrocytes in the advanced degenerative knee, some physicians have attempted combining PRP and HA injection to treat knee OA. A recent study showed the potential of combined use of HA and PRP due to the different mechanisms in reducing inflammation, indicated by decreased IL-6 and synoviocyte matrix metalloproteinase-13 expression.Citation21 Moreover, another study by Chen et alCitation27 revealed that the combined use of PRP and HA can promote chondrogenesis of OA chondrocytes in both cell and animal models. Therefore, the combined use of HA and PRP is considered to provide a better method to treat knee OA. However, evidence verifying the combined use of HA and PRP in severe knee OA remains weak.
Our cases provide clinical and radiographic evidence for a new therapy for advanced knee OA. This combined therapy can offer a chance to treat severe knee OA, rather than immediate surgery, or a chance for those who cannot undergo surgery. This combined therapy can also postpone the need of arthroplasty and can significantly increase the daily activity function. To the best of our knowledge, this report presents the first case series with X-ray imaging before and after PRP therapy in association with HA injection.
Limitations
The limitations of this clinical observation cases include the following: 1) a small number of patients to report a strong clinical effect, 2) the absence of standardization of standing knee radiographs to measure real articular cartilage changes, and 3) the use of only two viscosupplement products in these three patients. Further research with a randomized setting, control group, and larger case population is needed. Furthermore, other noninvasive examinations, such as ultrasonography and magnetic resonance imaging, are necessary to evaluate the thickness of cartilage after treatment.
Conclusion
We report three elderly patients with advanced knee OA who received PRP in association with HA injection and showed pain relief and functional improvement. The follow-up standard weight-bearing X-ray images of knees also confirmed the improvement and indicated the regeneration of the articular cartilage. This case series suggests that the treatment strategy of PRP in association with HA injection may be useful to treat advanced knee OA before these patients receive arthroplasty.
Acknowledgments
This work was supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019) and by the China Medical University under the Aim for Top University Plan of the Ministry of Education, Taiwan.
Disclosure
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated. The authors report no conflicts of interest in this work.
References
- Martel-PelletierJBoileauCPelletierJPRoughleyPJCartilage in normal and osteoarthritis conditionsBest Pract Res Clin Rheumatol200822235138418455690
- LawrenceRCFelsonDTHelmickCGEstimates of the prevalence of arthritis and other rheumatic conditions in the United States part IIArthritis Rheum2008581263518163497
- MurakiSAkuneTOkaHHealth-related quality of life in subjects with low back pain and knee pain in a population-based cohort study of Japanese men: the research on osteoarthritis against disability studySpine (Phila Pa 1976)201136161312131921730819
- BrownGAAAOS clinical practice guideline: treatment of osteoarthritis of the knee: evidence-based guideline, 2nd editionJ Am Acad Orthop Surg201321957757923996989
- VincentKPercivalSSConradBPSeayANMonteroCVincentKRHyaluronic acid (HA) viscosupplementation on synovial fluid inflammation in knee osteoarthritis: a pilot studyOpen Orthop J201320737838424093052
- RaeissadatSARayeganiSMHassanabadiHKnee osteoarthritis injection choices: hyaluronic acid versus platelet rich plasmaClin Med Insights Arthritis Musculoskelet Disord2015781825624776
- AndiaIAbateMKnee osteoarthritis: hyaluronic acid, platelet-rich plasma or both in association?Expert Opin Biol Ther201414563564924533435
- MorelandLWIntra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanisms of actionArthritis Res Ther200352546712718745
- SampsonSReedMSilversHMengMMandelbaumBInjection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot studyAm J Phys Med Rehabil2010891296196921403592
- ChangKVHungCYAliwargaFWangTGHanDSChenWSComparative effectiveness of platelet-rich plasma injections for treating knee joint cartilage degenerative pathology: a systematic review and meta-analysisArch Phys Med Rehabil201495356257524291594
- KhoshbinALerouxTWassersteinDThe efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesisArthroscopy201329122037204824286802
- GoldringMBThe role of the chondrocyte in osteoarthritisArthritis Rheum20004391916192611014341
- AyhanEKesmezacarHAkgunIIntraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritisWorld J Orthop20145335136125035839
- McAlindonTEBannuruRRSullivanMCOARSI guidelines for the non-surgical management of knee osteoarthritisOsteoarthritis Cartilage201422336338824462672
- HunterDJConaghanPGImaging outcomes and their role in determining outcomes in osteoarthritis and rheumatoid arthritisCurr Opin Rheum200682157162
- FDA/CDER Resource Page. Food and Drug Administration WebsiteGuidance for Industry: Clinical Development Programs for Drugs, Devices, and Biological Products Intended for the Treatment of Osteoarthritis1999 Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071577.pdfAccessed November 28, 2002
- VignonEPipernoMLe GraverandMPMeasurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee: comparison of standing anteroposterior and Lyon schuss viewsArthritis Rheum200348237838412571846
- CicuttiniFHankinJJonesGWlukaAComparison of conventional standing knee radiographs and magnetic resonance imaging in assessing progression of tibiofemoral joint osteoarthritisOsteoarthritis Cartilage200513872272715922634
- PourchoAMSmithJWisniewskiSJSellonJLIntraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: review and recommendationsAm J Phys Med Rehabil20149311 suppl 3S108S12124879553
- SánchezMAnituaEAzofraJAguirreJJAndiaIIntra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort studyClin Exp Rheumatol200826591091319032827
- SundmanEAColeBJKarasVThe anti-inflammatory and matrix restorative mechanisms of platelet-rich plasma in osteoarthritisAm J Sports Med2014421354124192391
- KonEBudaRFilardoGPlatelet-rich plasma: intraarticular knee injections produced favorable results on degenerative cartilage lesionsKnee Surg Sports Traumatol Arthrosc201018447247919838676
- KonEMandelbaumBBudaRPlatelet-rich plasma intraarticular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritisArthroscopy201127111490150121831567
- FilardoGKonEPereira RuizMTPlatelet-rich plasma intraarticular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approachKnee Surg Sports Traumatol Arthrosc201220102082209122203046
- JangSJKimJDChaSSPlatelet-rich plasma (PRP) injections as an effective treatment for early osteoarthritisEur J Orthop Surg Traumatol201323557358023412170
- TrigkilidasDAnandAThe effectiveness of hyaluronic acid intra-articular injections in managing osteoarthritic knee painAnn R Coll Surg Engl201395854555124165334
- ChenWHLoWCHsuWCSynergistic anabolic actions of hyaluronic acid and platelet-rich plasma on cartilage regeneration in osteoarthritis therapyBiomaterials201435369599960725176059
- CervelliVLucariniLSpalloneDUse of platelet-rich plasma and hyaluronic acid in the loss of substance with bone exposureAdv Skin Wound Care201124417618121422842
- NicoliFBalzaniALazzeriDSevere hidradenitis suppurativa treatment using platelet-rich plasma gel and hyalomatrixInt Wound J201512333834323834343
- YamadaYNakamuraSUedaMItoKPapilla regeneration by injectable stem cell therapy with regenerative medicine: long-term clinical prognosisJ Tissue Eng Regen Med20159330530923533047
