Abstract
Background
The performance of alcohol septal ablation (ASA) in elderly symptomatic patients with drug-refractory obstructive hypertrophic cardiomyopathy is still to be confirmed. The objective of this study was to compare the efficacy and safety of ASA in patients under and over 65 years old.
Methods and results
Fifty-one consecutive patients with obstructive hypertrophic cardio-myopathy who underwent ASA were retrospectively included and reviewed for in-hospital major acute cardiac events and follow-up. Twenty-eight patients were over 65 years old. Left ventricular outflow tract obstruction at rest, use of diuretic and average dose of diuretic were higher in patients over 65 years old. There was no difference in hospital stay between patients under and over 65 years old. Among patients over 65 years old, 2 (7%) died before being discharged. Major acute cardiac events were more frequent in patients over 65 years old in comparison with younger patients (43% versus 9%, respectively, P=0.007). The average follow-up duration was 16±15 months. There was no difference between patients under and over 65 years old regarding the efficacy of the procedure with a decrease of the New York Heart Association class of 1.3±0.6 and 1.4±0.7 (P=0.510) and the maximum left ventricular outflow tract gradient of 86±57 and 81±36 mmHg (P=0.733), respectively.
Conclusion
Elderly patients have the same benefits as younger patients after ASA but have more complications including mortality events.
Introduction
Percutaneous interventions have paved the way for new therapeutic areas on heart with a minimally invasive approach competing heart surgery. Consequently, indications of percutaneous interventions have grown over the last decade, particularly for elderly patients, who are frequently challenged for surgical approaches. Although percutaneous interventions have been well validated in most of the patients, their efficacy and safety in elderly patients continue to be debated. The use of interventional cardiology in continually aging population is known to carry a higher risk of complications, and because elderly patients are usually excluded from clinical studies, the performance of percutaneous intervention on elderly patients is still to be confirmed. This is particularly true for alcohol septal ablation (ASA) in symptomatic patients with drug-refractory obstructive hypertrophic cardiomyopathy (HCM). Although the comparison of myomectomy and ASA by randomized clinical trial seems impossible to perform,Citation1 ASA is widely used in Europe. It is nowadays admitted that short- and long-term outcomes of ASA are mostly favorable.Citation2,Citation3 This is well validated for young- and middle-age patients.Citation4 Although few studies suggest that the age is an independent predictor of mortality after ASA,Citation5 other studies suggest that the hemodynamic benefit is distinct according to the age of patients.Citation6 Efficacy and safety of ASA in elderly patients remain to be confirmed.
The objective of this study was to compare the efficacy and safety of ASA in patients under and over 65 years old.
Methods
Study sample
Fifty-one consecutive patients with obstructive HCM who underwent ASA in the University Hospital of Rangueil, Toulouse, France, between January 2010 and July 2015 were retrospectively included. The clinical diagnosis of obstructive HCM was based on the demonstration by bidimensional echocardiography of a nondilated and hypertrophied left ventricle (maximum left wall thickness ≥15 mm) in the absence of another cardiac or systemic disease that could produce a similar degree of hypertrophy.Citation7–Citation9 Indication of ASA was retained according to the European Society of Cardiology guidelines in patients with symptoms and left ventricular (LV) outflow tract obstruction ≥50 mmHg at rest or after exercise despite an optimal medical treatment. Demographic data, cardiovascular risk factors, electrocardiography, biochemistry, medication and procedural characteristics were abstracted from medical records.
The study was approved by our institutional review board (research ethics committee of the university hospital of Toulouse), and all patients were informed of the study design. Due to the retrospective design of the study the research ethics committee of the university hospital of Toulouse deemed written informed consent not necessary.
Echocardiography
All patients underwent a transthoracic echocardiography examination at baseline, during the procedure of ASA and during the follow-up with a commercially available ultrasound Vivid E9 system (GE Vingmed Ultrasound AS, Horten, Norway) or Philips IE33 (Philips Medical Systems, the Netherlands) using a 2.5 MHz transducer. A complete M-mode and two-dimensional gray scale echocardiography including the three standard apical views (four, three and two chambers) using high frame rates (>60 frames/sec) were performed for each patient. All echocardiographic data were synchronized to the electrocardiogram, and acquisition was performed during breath hold. The peak instantaneous LV outflow tract gradient was measured with continuous-wave Doppler in the apical five-chamber view with the simplified Bernoulli equation. Patients with LV outflow tract obstruction <50 mmHg at rest were tested by exercise echocardiography. Maximum LV wall thicknesses were measured in parasternal long-axis view. LV end-diastolic, end-systolic volumes and ejection fractions were measured using Simpson’s biplane method.
Cardiac magnetic resonance
Cardiac magnetic resonance (CMR) was performed on a 1.5-T MR commercial scanners, either Avanto, Siemens Medical Solutions (Erlangen, Germany) or Intera, Philips Medical Systems (Best, the Netherlands) using a 12-element phased-array cardiac coil with vector-cardiac gating in all patients. Following scout imaging, balanced steady-state free precession breath-hold images were acquired: slice thickness 6 mm (long-axis and four-chamber views) or 8–10 mm (contiguous short-axis views [no gap between slices, from the atrioventricular ring to the apex]). Subsequently, delayed contrast-enhanced CMR images were obtained in the same long-axis, four-chamber and short-axis orientations 10 minutes after injection of 0.2 mmol/kg of gadolinium dimenglumine (Magnevist, Berlex Imaging, Wayne, NJ, USA) using a phase-sensitive inversion recovery spoiled gradient echo sequence. LV ejection fraction and mass were calculated using clinically available software (Argus [Siemens Medical Solutions] and ViewForum [Philips Medical Systems]). Left atrial diameter was measured in the long-axis and four-chamber view.
Alcohol Septal Ablation
A temporary pacemaker was placed in all patients except those who already had a permanent pacemaker. A 6F guiding catheter was engaged in the ostium of the left main coronary artery, and a 10–15×1.5–3-mm over-the-wire balloon catheter was advanced over a 0.014-inch wire into the target septal perforator artery. For two patients, the target septal artery was reached through the right coronary artery. Myocardial contrast echocardiography was used through the balloon lumen to delineate the culprit septal segments. Ethanol 1–5 mL was injected into the artery supplying the culprit septal segments and left in place for 5 minutes. If complete heart block was present at 48 hours after the procedure, a permanent dual-chamber pacemaker was implanted.
Follow-up
In-hospital major acute cardiac events (MACE) were defined by death and/or cardiac tamponade and/or third-degree atrioventricular block requiring permanent stimulation and/or hemorrhage from the vascular path requiring transfusion. Follow-up consisted of a functional and echocardiographical assessment and was performed by review of the patient’s last hospital consultation.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation. Nominal values were expressed as numbers and percentages. Univariate analyses were performed using the Mann–Whitney rank sum test for continuous variables and the Fisher’s exact test for categorical variables for intergroup comparisons. Association between nominal variables was investigated by the Fisher’s exact test. Comparisons of continuous variables were performed by a Mann–Whitney U test or Spearman’s correlation when appropriate. Simple linear regression was first performed between MACE and all subject characteristics. Then, two models of multivariate analysis were performed using a multiple regression model including, among baseline characteristics, all univariate parameters with a P-value <0.10 and either age in years (model 1) or age over 65 years (model 2). All statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) and P<0.05 defined statistical significance.
Results
Baseline characteristics
The average population age was 67±12 years. Twenty-eight patients were over 65 years old. All patients had symptoms with a balanced distribution of poor dyspnea (New York Heart Association [NYHA] class II) and severe dyspnea (NYHA class III and IV), without any difference between patients under and over 65 years old. The demographic, echocardiographic and CMR characteristics of patients are listed in . Comparing to patients under 65 years old, there were more females in the group over 65 years old, with a smaller weight and a trend to a higher rate of arterial hypertension. Younger patients had more history of smoking habits and a higher indexed LV mass. LV outflow tract obstruction at rest, use of diuretic and average dose of diuretic were higher in patients over 65 years old.
Table 1 Demographic, echocardiographic, CMR and procedural characteristics of patients
ASA procedure
Most of the patients (88%) had radial access, without any difference between young and elderly patients (P=0.242). There was no difference between young and elderly patients in terms of the morphine administration during the procedure with doses of 8.3±3.6 and 7.2±2.1 mg (P=0.081), respectively. As shown in , the target septal artery was the first one for most of the patients over 65 years old, whereas 35% of the patients under 65 years old required the ablation of another septal artery: most of the time the second one, except for two patients who required the ablation of the septal artery from the posterior descending artery.
Safety of the procedure
The average hospital stay was 8±3 and 9±4 days for patients under and over 65 years old, respectively (P=0.633).
shows in-hospital cardiac events after ASA among patients under and over 65 years old. Among patients over 65 years old, 2 (7%) died before being discharged. There was no fatal case in patients under 65 years old. MACE, defined by death and/or cardiac tamponade and/or third-degree atrioventricular block requiring permanent stimulation and/or hemorrhage from the vascular path requiring transfusion, were more frequent in patients over 65 years old in comparison with younger patients (12 [43%] versus 2 [9%], respectively, P=0.007).
Table 2 In-hospital cardiac events after alcohol septal ablation
As shown in , by univariate analysis, age, age over 65 years old, female and hypercholesterolemia were associated with a risk of increase for MACE after ASA. There was a trend for decreased risk with radial access. After multivariate analysis, there was still a trend of increased risk for MACE with age, and particularly age over 65 years, but the association was no longer statistically significant.
Table 3 Multivariate analysis for MACE
Efficacy of the procedure
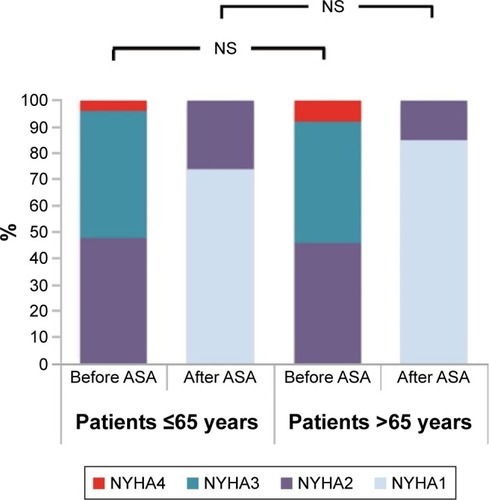
The average duration of follow-up was 22±19 and 16±15 months for patients under and over 65 years old, respectively (P=0.354). There was no difference between patients under and over 65 years old regarding the efficacy of the procedure with a decrease of the NYHA class of 1.3±0.6 and 1.4±0.7 (P=0.510) and the maximum LV outflow tract gradient of 86±57 and 81±36 mmHg (P=0.733), respectively. The average NYHA class at the time of follow-up was 1.3±0.4 and 1.2±0.4 (P=0.359) for patients under and over 65 years old, respectively. The impact of the procedure on the NYHA class for both groups is illustrated in .
Figure 1 Impact of alcohol septal ablation on the NYHA class before and after ASA upon follow-up.
Abbreviations: ASA, alcohol septal ablation; NS, non significant; NYHA, New York Heart Association.
Discussion
The incidence of cardiovascular disease rises with age, and age itself is considered as a risk factor for the development of cardiovascular diseases. Clinical and experimental evidence proves that the aging process promotes structural and functional remodeling of the heart, which occurs even in healthy older adults in the absence of an overt cardiovascular disease. It is legitimate to suppose that age-related effects on heart can modify the natural time course of heart disease. HCM may develop in various age groups as a consequence of different pathological processesCitation10 and may be a different disease in young and elderly patients. Whether the disease takes the same form in the elderly than in the young or middle-aged patients has not been clarified.Citation11 Consequently, the benefits and the risks of ASA may change with age. Our study shows that 1) ASA has the same efficacy among patients under and over 65 years old; and 2) patients over 65 years old have more in-hospital complications of the procedure.
Regarding the benefits of ASA in elderly when compared with younger patients, our results are consistent with the previous ample studies where ASA produced significant and similar improvements in LV outflow tract obstruction and symptoms, regardless of age, and despite baseline differences.Citation6,Citation12,Citation13 Faber et al provided conflicting results finding that younger age was associated with a less favorable hemodynamic outcome.Citation14 This could be partly explained by a higher basal interventricular septal thickness in younger patients at baseline, as reported by Gietzen et al.Citation6,Citation13 Anyway, all these studies confirm that the results of ASA on the elderly are at least as good as on younger patients up to 12 months.Citation6,Citation12 Our study confirms these results with an average follow-up of 16±15 months.
We found a higher rate of major acute in-hospital cardiac events following ASA in elderly patients compared with younger patients. These findings are consistent with the previous study of Leonardi et al, who have reported higher procedural complication rates for elderly patients in comparison to younger patients.Citation12 A recent study among 1,275 highly symptomatic patients treated with ASA demonstrated that age was an independent predictor of all-cause mortality over a follow-up of 5.7 years.Citation15 If the influence of age on long-term all-cause mortality seems logical, its impact on the procedural complication rate is still to confirm. In our cohort, by univariate analysis, absolute age and age over 65 years old are associated with an increased risk for acute procedural complication, but no longer after multivariate analysis. Whether the sample of our study is too small for allowing enough power to differentiate risk factors for procedural complications remains to be clarified. We cannot overlook that there were two deaths among elderly patients, whereas there was none among younger patients. However, the highest rate of complication among elderly in previous studies was wildly influenced by the difference of access site bleeding: all the procedures were performed with transfemoral arterial access.Citation12 In our cohort, most of the procedures were performed through radial access, which had a protective effect by univariate analysis. Although the impact of age on postprocedural complications was no longer significant by multivariate analysis, our study is probably underpowered to discriminate independent predictor of MACE. The trend of increased risk associated with age after multivariate analysis, in agreement with previous studies; suggests that ASA is associated with an increased rate of complications among elderly patients.
Limitations
First, our study is a retrospective observational study conducted at a single center, and, therefore, unmeasured confounding factors may influence the observed associations. Second, as aforesaid, the sample of our study is probably too small for allowing enough power to discriminate age as a risk factor for adverse cardiac events following ASA. However, the lower impact of age after multivariate analysis highlights the weight of comorbidities and confounding factors in the age-related procedural complications. Finally, our study focused on ASA and did not integrate a control group with optimal medical treatment alone or myomectomy.
Conclusion
Although it is considered as disease of the young age and because of its age-related penetrance, obstructive HCM is commonly diagnosed in the elderly, which are frequently challenged for surgical management. Consequently, symptomatic patients despite optimal medical treatment referred for ASA have increased. Our study shows that elderly patients referred for ASA have the same benefits as younger patients through an average follow-up of 16±15 months. However, elderly patients have more complications including mortality events.
Disclosure
The authors report no conflicts of interest in this work.
References
- OlivottoIOmmenSRMaronMSCecchiFMaronBJSurgical myectomy versus alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Will there ever be a randomized trial?J Am Coll Cardiol200750983183417719467
- SorajjaPOmmenSRHolmesDRJrSurvival after alcohol septal ablation for obstructive hypertrophic cardiomyopathyCirculation2012126202374238023076968
- VeselkaJKrejciJTomasovPZemanekDLong-term survival after alcohol septal ablation for hypertrophic obstructive cardiomyopathy: a comparison with general populationEur Heart J201435302040204524464834
- VeselkaJKrejciJTomasovPSurvival of patients ≤50 years of age after alcohol septal ablation for hypertrophic obstructive cardiomyopathyCan J Cardiol201430663463824882534
- SteggerdaRCDammanKBaltJCLiebregtsMten BergJMvan den BergMPPeriprocedural complications and long-term outcome after alcohol septal ablation versus surgical myectomy in hypertrophic obstructive cardiomyopathy: a single-center experienceJACC Cardiovasc Interv20147111227123425326737
- VeselkaJDuchonovaRPalenickovaJAge-related hemodynamic and morphologic differences in patients undergoing alcohol septal ablation for hypertrophic obstructive cardiomyopathyCirc J200670788088416799242
- MaronBJHypertrophic cardiomyopathy: a systematic reviewJAMA2002287101308132011886323
- MaronBJMcKennaWJDanielsonGKAmerican college of cardiology/European society of cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American college of cardiology foundation task force on clinical expert consensus documents and the European society of cardiology committee for practice guidelinesEur Heart J200324211965199114585256
- GershBJMaronBJBonowRO2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice GuidelinesCirculation2011124242761279622068435
- FayWPTaliercioCPIlstrupDMTajikAJGershBJNatural history of hypertrophic cardiomyopathy in the elderlyJ Am Coll Cardiol19901648218262212364
- LeverHMKaramRFCurriePJHealyBPHypertrophic cardiomyopathy in the elderly. Distinctions from the young based on cardiac shapeCirculation19897935805892917389
- LeonardiRATownsendJCPatelCAAlcohol septal ablation for obstructive hypertrophic cardiomyopathy: outcomes in young, middle-aged, and elderly patientsCatheter Cardiovasc Interv201382583884522936613
- GietzenFHLeunerCJObergasselLStrunk-MuellerCKuhnHTranscoronary ablation of septal hypertrophy for hypertrophic obstructive cardiomyopathy: feasibility, clinical benefit, and short term results in elderly patientsHeart200490663864415145866
- FaberLWelgeDFassbenderDSchmidtHKHorstkotteDSeggewissHOne-year follow-up of percutaneous septal ablation for symptomatic hypertrophic obstructive cardiomyopathy in 312 patients: predictors of hemodynamic and clinical responseClin Res Cardiol2007961286487317891518
- VeselkaJJensenMKLiebregtsMLong-term clinical outcome after alcohol septal ablation for obstructive hypertrophic cardiomyopathy: results from the Euro-ASA registryEur Heart J201637191517152326746632
