Abstract
Purpose
High coronary calcium score (CCS) and post-procedural cardiac enzyme may be related with poor outcomes in patients with coronary stent implantation.
Methods
A total of 1,072 patients (63.2% male, mean age: 61.7±10.3 years) who underwent coronary multi-detect computed tomography at index procedure and follow-up coronary angiography (CAG) after drug-eluting stent (DES) were divided into two groups: those with and without target lesion revascularization (TLR; >50% reduction in luminal stent diameter or angina symptoms on follow-up CAG). The CCSs for predicting stent revascularization were elucidated.
Results
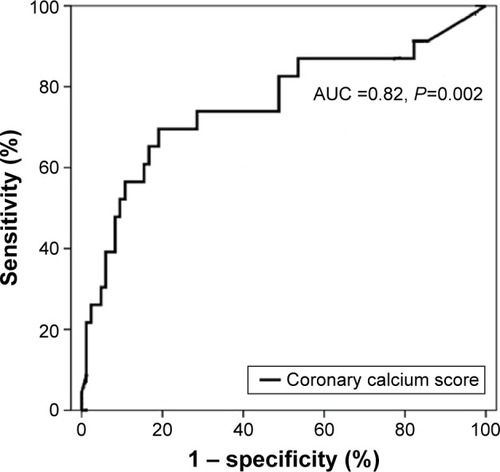
There were no significant differences between the two groups with regard to risk factors. The initial CCS was significantly higher in the TLR group (1,102.4±743.7 vs 345.8±51.05, P=0.04). After adjustment of significant factors for TLR, only CCS and post-procedural creatine kinase MB form (CK-MB) elevation were significant predictors of coronary artery TLR. Receiver operation curve revealed that >800 in CCS had 69% in sensitivity and 88% in specificity about predicting the TLR.
Conclusion
High CCS with post-procedural CK-MB might be the useful predictors for TLR after DES implantation.
Introduction
Noninvasive imaging for early detection of cardiovascular disease is actively investigated. Also, routine cardiovascular screening tests in diabetic and elderly patients are increasing. To detect coronary artery disease (CAD), various noninvasive techniques, such as the measurement of coronary calcium score (CCS), have quantitative correlation with the prevalence of CAD.Citation1–Citation6 According to a recent meta-analysis, low-dose coronary computerized tomography (CT) showed that CCS values of 0, 1–99, 100–400, 400–999, and ≥1,000, had 1.0, 1.9, 4.3, 7.2, and 10.8 as relative risk ratio of cardiovascular disease, respectively.Citation1,Citation2 The quantification of CCS has been reported to be a more reliable prognostic factor for cardiovascular disease.Citation7,Citation8 Highly calcified lesion was closely related with poor clinical outcomes due to stent underexpansion and edge dissection. Recently developed coronary stents show thin stent strut and high capability of conformational change, which increases the deliver-ability to highly calcified and angulated lesions. This kind of mechanical property has also increased the concern about stent deformation and restenosis, especially in highly calcified lesions. It must be elucidated what, other than the severity of coronary calcification, predicts stent restenosis.
We examined whether CCS was significantly correlated with target lesion revascularization (TLR) of the coronary artery after drug-eluting stent (DES) implantation.
Subjects and methods
Subjects
A total of 1,072 stable angina patients (mean age 61.7±10.3 years, 63.2% male) diagnosed with CAD on the basis of multidetector CT (MDCT) were enrolled in this study. All of them had DESs implantation of not less than 2.5 mm in diameter and had been assessed by follow-up coronary angiography (CAG). We excluded patients with acute coronary syndrome, coronary stent implantation in the setting of cardiogenic shock complicating acute myocardial infarction, patients with unsuccessful stenting (defined as failure to place the stent at the desired site or to achieve a satisfactory angiographic result), patients with stenting intended primarily as a bridge to coronary artery bypass, patients with any major cardiac event (including death, myocardial infarction, bypass, repeated percutaneous transluminal coronary angioplasty, or stent vessel occlusion) during the 30 days immediately after the procedure. Above exclusion criteria may have been related to procedural complications and a lot of confounding bias so patients were not suitable for inclusion in the study.
Patients were divided into two groups. Group I included those patients who had no TLR on a follow-up CAG (n=910). Group II consisted of those patients who had TLR on a follow-up CAG (n=162). The mean age in group II was 62.1±9.0 years, and the proportion of male patients was 58.6% (n=95). TLR was defined as those who need to be revascularized for the stent restenosis due to ischemic-driven symptoms or angiographic restenosis >50% in diameter on a follow-up CAG. For all patients, MDCT was performed within a month before the initial CAG. Indications of MDCT in group I were angina (n=564, 62%), dyspnea (n=209, 23%) and asymptomatic (n=137, 15%). Group II had angina (n=115, 71%), dyspnea (n=30, 19%) and asymptomatic (n=17, 10%) as indications.
All patients submitted written informed consent. All tests and other procedures were approved by the Institutional Review Board of The Catholic University of Korea, Seoul, Korea.
Methods
Clinical data were obtained from medical records and through interviews with all study patients. MDCT images were obtained by reconstructing the cross-sectional and multi-planar images via imaging work stations. For calcification assessment, unenhanced electrocardiographically (ECG)-gated cardiac CT was performed by using a 64 detector row CT scanner (Light speed; General Electric Medical Systems, Milwaukee, WI, USA) with 2.5 mm section thickness (4×2.5 mm collimation), pitch of 0.16, 0.35-second rotation time, 100–120 kV, and 250 mA. In the CAG image of MDCT, iopromide (Ultravist®; Berlex Laboratories Inc, New Jersey, USA) was used as a contrast medium and was intravenously infused at a rate of 5 mL/sec. A total of 70 mL was intravenously infused. Subsequently, 20 mL of saline was infused at a rate of 5 mL/sec. A bolus tracking was performed for the ascending aorta. Thus, images were obtained extending from the time point of 100 house field unit (HU) to 6 sec. The cross-sectional thickness was increased from 0.625 mm by degrees of 0.3 mm. Then, images were obtained using an ECG-gated half-scan algorithm. All the patients were given oral beta blocker if they had high baseline heart rate (>85 beat per minute). None of the study patients need to be given additional intravenous injections of β-blockers.
CAG and intervention
Patients were given aspirin (100 mg) and clopidogrel (600 mg) prior to the percutaneous coronary intervention (PCI). CAG was performed via a femoral or radial artery, for which major epicardial coronary arteries >2.5 mm in length were evaluated. In the lesions, where a stenosis was observed at a magnitude of >70% on the CAG, the PCI was performed using various DESs: Cypher® (sirolimus-eluting stent), Taxus® (paclitaxel-eluting stent), Xience®/Promus® (everolimus-eluting stent) and Endeavor resolute® (zotarolimus-eluting stent). Dual or triple antiplatelet therapy was continued for at least 1 year. A follow-up CAG after a mean period of 11.2±1.01 month was performed in 1,072 patients. DESs were classified according to the stent-coating drugs and polymers. Post-procedural creatine kinase MB form (CK-MB) was measured 6 and 9 hours after the procedure. More than two times elevation from upper normal limit was defined as post-procedural CK-MB elevation. High sensitivity C reactive protein (hs-CRP), lipid profiles and cardiovascular risk factors were also compared.
Statistical analysis
In the comparison of the groups with and without TLR, the continuous variables were subjected to an independent t-test and the categorical variables were subjected to a Pearson’s chi-square test or Fisher’s exact test. All the data after confirmation of normal distribution were expressed as mean ± standard deviation and the frequency (%). In all cases, a value of P<0.05 was considered statistically significant. To analyze the factors affecting TLR, a binary logistic regression analysis was performed. Univariate variables with P<0.20 or known risk factor of TLR as proved in other studies were entered into the multivariate logistic models.Citation9 A value of P<0.05 in the multivariate logistic analysis was considered statistically significant. To predict the occurrence of TLR based on CCS, statistical analysis was performed using the receiver operating characteristic curve. The association between CK-MB elevation and CCS was compared by chi-square test. Statistical analysis was performed using SPSS Software, Ver. 15.
Results
Clinical characteristics
In the baseline characteristics of 1,072 stable angina patients, the mean age was 63.1±10.1 years and the number of males was 687 (64.0%). The non-TLR group comprised 910 patients, where the male-to-female ratio was 592 (56.2%):318 (35.8%), and their mean age was 63.4±10.1 years. In the TLR group, there were 162 patients with a male-to-female ratio of 95 (58.6%):77 (41.4%) and the mean age was 62.1±9.0 years. A comparison between the groups with and without TLR showed no significant differences in sex, age, body mass index, diabetes mellitus (DM), smoking, fasting blood sugar, hypertension, HbA1c, creatinine, CRP, total cholesterol, triglyceride, low-density lipoprotein, high-density lipoprotein, or NT-pro-BNP between the two groups ().
Table 1 Baseline clinical characteristics in groups with and without TLR
Angiographic data showed no significant difference in stent diameter and length between the TLR group and the non-TLR group (). Coronary stent type was significantly different between both groups. But this significance had disappeared after regression analysis ().
Table 2 Logistic regression analysis of the influencing factors for prediction of TLR in lesions
The mean CCS was 345.8±51.05 in the non-TLR group and 1,102.4±743.7 in the TLR group. This difference was statistically significant (P=0.04; ).
In univariate logistic regression analysis, parameters shown to differ significantly between the TLR and non-TLR groups included body mass index, hypertension, stent type, follow-up duration, post-procedural CK-MB elevation and calcium score. In a multivariate logistic regression analysis of these variables, the calcium score (P=0.006, odds ratio [OR] 1.30 [95% CI: 1.19–1.48]) and post-procedural CK-MB elevation (P=0.02, OR 1.45 [95% CI: 1.28–1.51]) were found to be independent predictors for TLR (). To analyze the prognostic value of the CCS for the occurrence of TLR, the receiver operating curve was used. The CCS was a more significant predictor of TLR. According to our results, at a CCS value of 800, TLR could be predicted with a sensitivity of 69% and a specificity of 88% (). The association with calcium score and CK-MB elevation was analyzed. The post-procedural CK-MB elevated patients (patients with high calcium score over 800), had a significantly high incidence of TLR rate ().
Table 3 Incidence of target lesion revascularization according to coronary calcium score and post-procedural CK-MB elevation
Discussion
The occurrence of TLR in the DES era has been markedly decreased as compared with cases of bare-metal stents.Citation10 But TLR still remains one of the most important clinical problems related to coronary interventions. TLR mainly occurs as a result of geometric remodeling and neointima hyperplasia based on vascular pathology.Citation11 These phenomena are also presumed to be a mechanism by which atherosclerosis occurs.Citation12,Citation13 Coronary calcification has been examined in many studies as a noninvasive surrogate by which atherosclerosis can be diagnosed and its severity can be assessed.Citation2–Citation7 In addition, other studies have reported that CCS is helpful for the early detection of asymptomatic atherosclerosis.Citation11,Citation14 Many studies have reported that the CCS measured on CT is a significantly predictive factor for the occurrence of asymptomatic and symptomatic CAD.Citation15–Citation18 Furthermore, the progression of coronary calcification has also been reported to be a useful indicator for treatment effects on CAD.Citation19,Citation20 The success rate of PCI is lower in calcified lesions of moderate or greater severity. Highly calcified lesions have a higher frequency of restenosis following PCICitation21,Citation22 due to stent failure of apposition or the poor attachment of arterial wall during the PCI.Citation23–Citation25 Our study showed that TLR patients had a significantly higher CCS than non-TLR patients. Post-procedural CK-MB elevation with high calcium score might be related with incomplete PCI, such as incomplete apposition, small branch jail and small emboli of calcified plaque. These results suggest that the CCS can be used as a predictor of TLR in patients after DES implantation.
It has been alluded that CCS is a more reliable indicator for the prediction of cardiovascular diseases than CRP.Citation16 As MDCT has become common in clinical settings, CCS has been widely used as a noninvasive test to examine CAD. In this way, coronary artery calcification can be quantified more accurately and easily than with electron beam computerized tomography (EBCT).Citation26
Parameters, such as DM, multiple stents, small final minimal luminal diameter, stent type, small coronary artery, and CRP have been reported as risk factors of TLR following DES implantation.Citation27–Citation29 Also, DM, renal failure on hemodialysis, lesion length, reference vessel diameter, and post-interventional intravascular ultrasound (IVUS) lumen area had been reported as predictors for angiographic restenosis.Citation27–Citation29
Conclusion
In this study, post-procedural CK-MB and calcium score were significant predictors of TLR. This means that the CCS, as measured on MDCT prior to PCI, could be used as a noninvasive technique to predict TLR. High coronary calcium score does not directly indicate that the target lesion is heavily calcified. But it seems that the coronary lesion with high coronary calcium score should be thoroughly prepared for stent deployment. After the procedure, post-procedural CK-MB evaluation might be useful in patients with high calcium score. We suggest that the CCS reflects the multiple factors involved in TLR (the mechanical properties such as incomplete stent expansion), incomplete coverage of lesion for calcified lesions during stent deployment and the severity of coronary atherosclerosis. MDCT has broad clinical utility such as a screening tool, assessment of abnormal coronary anatomy in chronic total occlusion and cost benefit replacing the invasive angiography. However, it has concerns with radiation hazard. This study does have some limitations. No analysis was performed for the PCI through quantitative coronary anatomy or IVUS. Although many variables such as lesion characteristics, balloon inflation time, coadministrative medications are involved in the pathophysiology of TLR after DES implantation, these variables were not included in the retrospective data analysis. Calcium score measured by MDCT seems to be overestimated.Citation30 The current study was a retrospective, cross-sectional study at a single center. Also, there were a lot of biases to influence the clinical outcomes. Enrolled patients, in this study, were stable angina patients who took planned CAG. This meant that they had mild symptoms and severity. So, we could not say for sure that our conclusion could be applied in acute coronary syndrome patients. In this study, the frequencies of TLR and periprocedural CK elevation seem to be higher than in other studies. This might be because we enrolled patients who received follow-up angiography without exception. So asymptomatic restenosed patients were included, which was unique and different from other studies. Considering these limitations, further studies will need to verify the noninvasive surrogates to predict the stent restenosis.
Acknowledgments
This research was supported by the grant of research foundation of Internal Medicine of the Catholic University of Korea.
Disclosure
The authors report no conflicts of interest in this work.
References
- BermanDSArnsonYRozanskiACoronary artery calcium scanning: the agatston score and beyondJACC Cardiovasc Imaging20169121417141927931526
- BeigneuxYSablayrollesJLVarenneOMasJLCalvetDCoronary artery calcium score improves the prediction of occult coronary artery stenosis in ischemic stroke patientsJ Am Heart Assoc2016511 piie00377027799237
- Isma’eelHMinDAl-ShaarLAssessing level of agreement for atherosclerotic cardiovascular disease risk categorization between coronary artery calcium score and the American College of Cardiology/American Heart Association Cardiovascular Prevention Guidelines and the Potential Impact on Treatment RecommendationsAm J Cardiol2016118101480148527642113
- SchuhbaeckASchmidJZimmerTInfluence of the coronary calcium score on the ability to rule out coronary artery stenoses by coronary CT angiography in patients with suspected coronary artery diseaseJ Cardiovasc Comput Tomogr201610534335027461528
- MillerTDRodriguez-PorcelMYour coronary calcium scan is positive: now what?JACC Cardiovasc Imaging20169559059227085439
- KelkarAASchultzWMKhosaFLong-term prognosis after coronary artery calcium scoring among low-intermediate risk women and menCirc Cardiovasc Imaging201694e00374227072301
- BreuckmannFOlligsJHinrichsLCoronary artery calcium as an independent surrogate marker in the risk assessment of patients with atrial fibrillation and an intermediate pretest likelihood for coronary artery disease admitted to a German chest pain unitClin Cardiol201639315716427001202
- FolsomARKronmalRADetranoRCCoronary artery calcification compared with carotid intima-meida thickness in the prediction of cardiovascular disease incidence: the multi-ethnic study of atherosclerosis (MESA)Arch Intern Med2008168121333133918574091
- BasavarajaiahSNaganumaTLatibATreatment of drug-eluting stent restenosis: comparison between drug-eluting balloon versus second-generation drug-eluting stents from a retrospective observational studyCatheter Cardiovasc Interv201688452252826715370
- ShimadaYKataokaTCourtneyBKInfluence of plaque calcium on neointimal hyperplasia following bare metal and drug-eluting stent implantationCatheter Cardiovasc Interv200667686686916649232
- FuchsAKühlJTChenMYFeasibility of coronary calcium and stent image subtraction using 320-detector row CT angiographyJ Cardiovasc Comput Tomogr20159539339826091841
- KongLLiuWYanGPoly-l-lactic acid/amorphous calcium phosphate bioabsorbable stent causes less inflammation than poly-l-lactic acid stent in coronary arteriesInt J Clin Exp Med20147125317532325664037
- HondaYToyamaTMiyaishiYCoronary artery calcification as a new predictor of non-target lesion revascularization during the chronic phase after successful percutaneous coronary interventionCardiovasc Interv Ther201429431532324906449
- PregowskiJJastrzebskiJKępkaCRelation between coronary plaque calcium deposits as described by computed tomography coronary angiography and acute results of stent deployment as assessed by intravascular ultrasoundPostepy Kardiol Interwencyjnej20139211512024570702
- TanabeKKishiSAokiJImpact of coronary calcium on outcome following sirolimuseluting stent implantationAm J Cardiol2011108451451721624546
- LiuXTsujitaKMaeharaAIntravascular ultrasound assessment of the incidence and predictors of edge dissections after drug-eluting stent implantationJACC Cardiovasc Interv2009210997100419850262
- ShawLJRaggiPCallisterTQBermanDSPrognostic value of coronary artery calcium screening in asymptomatic smokers and nonsmokersEur Heart J200627896897516443606
- FangHYLeeCHFangCYApplication of penetration device (Tornus) for percutaneous coronary intervention in balloon uncrossable chronic total occlusion-procedure outcomes, complications, and predictors of device successCatheter Cardiovasc Interv201178335636221413119
- RaggiPCallisterTQShawLJProgession of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapyArterioscler Thromb Vasc Biol20042471272127715059806
- RaggiPCooilBRattiCCallisterTQBudoffMProgression of coronary artery calcium and occurrence of myocardial infarction in patients with and without diabetes mellitusHypertension200546123824315851627
- BangaloreSVlachosHASelzerFPercutaneous coronary intervention of moderate to severe calcified coronary lesions: insights from the national heart, lung, and blood institute dynamic registryCatheter Cardiovasc Interv2011771222820506328
- MaffeiEArcadiTZuccarelliAThe impact of training on diagnostic accuracy with computed tomography coronary angiographyJ Cardiovasc Med (Hagerstown)2013141071972524335883
- ParkJHSohnISJinESChoJMKimCJLeeYKHeavy coronary calcium mimicking in-stent restenosisKorean Circ J201141742121860648
- XuKMintzGSKuboTLong-term follow-up of attenuated plaques in patients with acute myocardial infarction: an intravascular ultrasound substudy of the HORIZONS-AMI trialCirc Cardiovasc Interv20125218519222438429
- KawaguchiRTsurugayaHHoshizakiHToyamaTOshimaSTaniguchiKImpact of lesion calcification on clinical and angiographic outcome after sirolimuseluting stent implantation in real-world patientsCardiovasc Revasc Med2008912818206630
- VenkitachalamLKipKEMulukutlaSRNHLBI-Sponsored Dynamic Registry InvestigatorsTemporal trends in patient-reported angina at 1 year after percutaneous coronary revascularization in the stent era: a report from the national heart, lung, and blood institute-sponsored 1997–2006 dynamic registryCirc Cardiovasc Qual Outcomes20092660761520031899
- ZellerTKrankenbergHSteinkampHOne-year outcome of percutaneous rotational atherectomy with aspiration in infrainguinal peripheral arterial occlusive disease: the multicenter pathway PVD trialJ Endovasc Ther200916665366219995118
- LiQHeYChenLChenMIntensive plaque modification with rotational atherectomy and cutting balloon before drug-eluting stent implantation for patients with severely calcified coronary lesions: a pilot clinical studyBMC Cardiovasc Disord20161611227230875
- YinDMaeharaAMezzafonteSMosesJWMintzGSShlofmitzRAExcimer laser angioplasty-facilitated fracturing of napkin-ring peristent calcium in a chronically underexpanded stent: documentation by optical coherence tomographyJACC Cardiovasc Interv201588e137e13926205458
- DeprezFCVlassenbroekAGhayeBRaaijmakersRCocheEControversies about effects of low-kilovoltage MDCT acquisition on agatston calcisum scoringJ Cardiovasc Comput Tomogr201371586123333185