Abstract
Background
It is not known whether amino acid supplementations may influence health status in hospitalized older acutely ill patients.
Aim
The aim of this study was to determine whether nutritional supplementation with amino acids (Aminoglutam®) is associated with multidimensional improvement assessed with the Multidimensional Prognostic Index (MPI).
Methods
In this randomized, double-blind, placebo-controlled pilot clinical trial, 126 patients aged ≥65 years were enrolled from 6 Italian geriatric wards. A multidimensional assessment to calculate the MPI was performed at baseline and after 4 weeks of treatment with nutritional supplementation (96 kcal, 12 g amino acids, 0.18 g fat, 11.6 g carbohydrate, and vitamins B1, B6, and C) or placebo administered twice a day. Logistic regression modeling was applied to determine the effect of treatment on the improvement of MPI (vs no-change/worsening), adjusting for gender, age, and MPI at baseline. Treatment’s interactions with age, gender, and MPI at baseline were tested adding the appropriate interaction parameter in the regression models.
Results
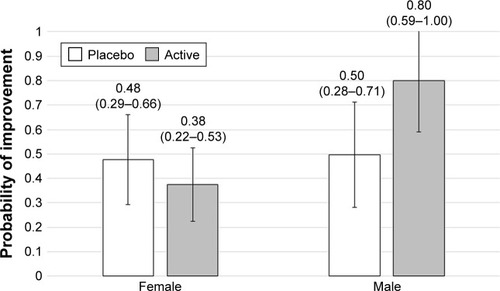
Of the 126 patients included, 117 patients (93%) completed the study. A significant improvement in the MPI score was detected in the overall population (mean difference post-pretreatment: −0.03, p=0.001), with no differences between active and placebo arms. Men in the amino acid supplementation group had a significantly higher rate of improvement in MPI (81%) compared to the placebo group (46%) (Fisher’s exact test p=0.03). Adjusting for age, diagnosis, and MPI at baseline, amino acid treatment was shown to be associated with an improvement in MPI in men (OR=4.82, 95% confidence interval [CI]: 0.87–26.7) and not in women (OR=0.70, 95% CI: 0.27–1.81). The interaction effect between active treatment and gender was significant (p=0.04).
Conclusion
A 4-week amino acid supplementation improved the MPI significantly in hospitalized older male patients but not in female patients. Further studies are needed to confirm the gender effect of amino acid supplementation on MPI in older patients.
Introduction
Hospitalization for an acute medical event represents a stressful and potentially hazardous event for older persons, which often leads to important clinical complications, including functional decline, prolonged length of stay, and death.Citation1 Besides the disabling effect of the acute event, hospitalization itself might represent an additional stressor in terms of environmental hazard, reduced caloric intake, low physical activity or prolonged bed rest, depressed mood, and social isolation.Citation2 For example, in older patients, hospitalization and prolonged bed rest have been associated with increased risk of incident sarcopenia and functional decline.Citation3
Malnutrition, and specifically energy–protein malnutrition, is common in older patients, and hospitalized patients are often at risk of malnutrition during hospital stay.Citation4 An optimal amino acid availability not only is fundamental to guarantee an adequate protein synthesis but also plays a crucial role in several conditions characterized by a hyper-catabolic state including many acute diseases, cancers, and inflammatory conditions.Citation5 Malnutrition is associated with poor health status and poor clinical outcomes in hospitalized adults, including prolonged hospital stay, increased risk of hospital readmission, and increased mortality.Citation6
Several studies investigated the effect of oral nutritional supplementation on nutritional status and clinical outcomes in older patients admitted to the hospital. Globally taken, these studies suggest that oral supplementation increased nutritional status, including body weight, but the effect on more relevant clinical outcomes is still controversial.Citation7
This pilot study evaluated the effect of a nutritional supplement containing 12 g of amino acids on post-discharge health status, assessed using the Multidimensional Prognostic Index (MPI). MPI is a prognostic instrument based on 6 commonly used geriatric assessment scales exploring cognitive, functional, nutritional, and clinical status, as well as on information about drugs taken and patient’s social support.Citation8 MPI is an accurate index to assess mortality risk and overall health status of older people; in older hospitalized patients, MPI predicts length of hospital stay, in-hospital mortality, and long-term mortality after hospital discharge.Citation9,Citation10 We hypothesized that compared to patients allocated to placebo, those randomized to amino acid supplementation significantly improve the MPI score over the follow-up.
Methods
Study design
The Frailty and Amino acid supplementation (FRAMINO) study was a pilot multicenter, prospective, randomized, double-blind, placebo-controlled, parallel group study conducted in Italy between June 1, 2014, and January 31, 2016. The study evaluated the effects of Aminoglutam® (AG) vs placebo on the changes in the overall health status in older hospitalized adults. As per the initial protocol, change in the MPI score at 30 days after randomization was the primary outcome. Patient assessments were performed at baseline and 30 days after randomization or at study discontinuation and included the same clinical evaluation performed at baseline. The protocol received approval from the ethical committee of the coordinating center (Comitato Etico IRCCS “Casa Sollievo della Sofferenza” – San Giovanni Rotondo, Foggia) and from ethical committees of all other sites (Comitato Etico Azienda ULSS 16 – Padova – Nucleo per la Ricerca clinica; Comitato Etico unico della provincia di Ferrara; Comitato Etico Regionale [CER] – Regione Liguria; Comitato Etico per la Sperimentazione Clinica della Provincia di Rovigo; and Comitato Etico per la sperimentazione clinica delle province di Treviso e Belluno). All patients provided written informed consent.
Patients
All patients aged 65 years or more consecutively admitted to participating hospital wards entered the study protocol regardless of the diagnosis of admission. Eligible patients were required to have an MPI grade 2 or 3 (expression of moderate or severe mortality risk, respectively). Exclusion criteria were current active advanced cancer or severe organ failure that might prevent the 30-day follow-up evaluation.
MPI is a validated prognostic index based on a Comprehensive Geriatric Assessment (CGA) that accurately predicts short- and long-term mortality in older people in different clinical settings and affected by different medical conditions. To calculate the MPI, a standardized CGA was performed within 48 hours from admission to collect information on basic activities of daily living (ADL) and instrumental activities of daily living (IADL) according to the Katz et alCitation11 and the Lawton–BrodyCitation12 scales, respectively. Cognitive status was evaluated using the Short Portable Mental Status Questionnaire (SPMSQ).Citation13 Comorbidity burden was evaluated using the comorbidity subscale of the cumulative illness rating scale (CIRS),Citation14 and nutritional status was assessed through the mini nutritional assessment (MNA).Citation15 The Exton–Smith scale (ESS) was used to evaluate the risk of developing pressure ulcers.Citation16 The number of medications taken at home and co-habitation status (alone, in institution, and with family) was recorded. All site personnel were trained on MPI administration and evaluation.
Study treatments
After eligibility criteria were ascertained, patients were randomized (1:1) through a centralized allocation system to receive either AG or placebo twice daily during hospitalization and 30 days after randomization. After randomization, both groups of patients continued the pharmacological and/or dietetic prescription indicated by the attending physician, and after hospital discharge they continued that prescribed by the primary care physician. AG is a specialized, dietetic aliment (Errekappa Euroterapici S.p.a., Milan, Italy) with 96 kcal, 12 g amino acids (including essential amino acids), 0.18 g fat, 11.6 g carbohydrate, and vitamins B1, B6, and C. Placebo and AG formula share only excipients, intended as not therapeutic agents. The detailed nutritional composition of AG is presented in Table S1.
Outcomes
The primary outcome for the study was change in the MPI score at the end of the 4-week follow-up period. Other efficacy end points included change in distribution of the MPI group and likelihood of MPI improvement over the follow-up. As pre-specified in the study protocol, secondary analyses were stratified according to the baseline MPI group and gender.
Statistical analysis
Efficacy analyses were performed on the intention-to-treat (ITT) population, defined a priori as all enrolled patients who received any amount of allocated intervention. The sample size was calculated based on the 30-day change in the MPI score. With a sample size of 60 patients per arm, the study was 95% powered to detect a MPI change difference of ≥0.07 in the active arm, assuming no change in the placebo arm. The sample size calculation was performed assuming an SD of the MPI difference equal to 0.15 (previous studiesCitation27) and a 0.01 2-sided alpha level.
Demographics and clinical characteristics were summarized using mean and SD for continuous factors and absolute and relative (%) frequencies for categorical factors. Pearson chi-square or Fisher’s exact tests and independent sample t-test were adopted to compare categorical and continuous variables, respectively, between arms. Changes in primary (MPI) and component efficacy end points according to the treatments groups were analyzed and compared using the paired t-test and ANCOVA, setting the change in MPI as a dependent variable and treatment as explanatory, adjusting for main demographics and clinical factors. Logistic regression analysis was adopted to investigate the likelihood of MPI improvement (vs no change or worsening) at the end of the follow-up as a function of treatment group, adjusting for age and MPI at baseline.
Results
Patients
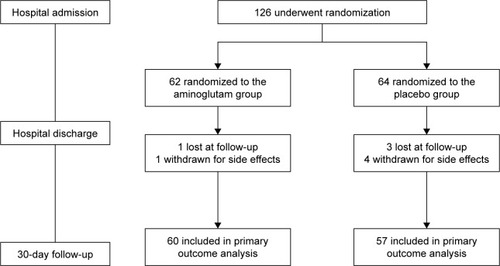
A total of 126 patients were enrolled from 6 sites (62 AG and 64 placebo) and are included in the ITT population; 9 patients (2 AG and 7 placebo) exited the study prior to the 30-day follow-up visit: 5 because of side effects and 4 because they were lost to follow-up (). Overall, clinical outcomes were unavailable from 2 and 7 patients in the AG and placebo groups, respectively. Demographics, clinical characteristics, and conditions leading to hospital admission were comparable between groups, except for the prevalence of patients malnourished or at risk of malnutrition (MNA score <24), which was greater in the active intervention group (). Patients randomized to placebo were more likely to be male and had more ADL impairment, but the differences were not statistically significant. Acute cardiovascular disease (34%) and acute pulmonary conditions (17.4%) were the most common causes of hospitalization.
Table 1 Baseline selected demographic and clinical characteristics of the treatment groups
Efficacy end points
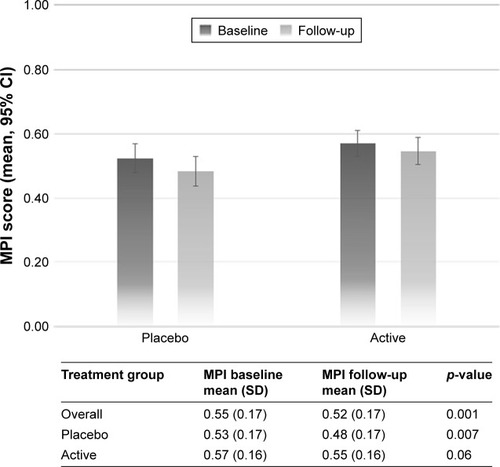
At the 30-day follow-up visit, the MPI score significantly decreased in the overall sample (−0.03, 95% confidence interval [CI] −0.05 to −0.01) without significant differences between study groups, suggesting an overall improvement of the health status of the study population over time, independently of AG treatment ().
Figure 2 Improvement in MPI score at follow-up, according to treatments and gender.
Analysis of single components of MPI () demonstrated similar difference between treatment groups; the placebo group experienced a greater increase in the ESS score compared to the AG group, although the difference was only of borderline statistical significance (p=0.07).
Table 2 Change in primary (MPI) and component efficacy end points according to the treatment groups
The MPI score improved in approximately 50% of patients at day 30 without significant difference between groups (51.7 and 47.4% in the AG and placebo groups, respectively) (). However, men in AG supplementation group had a significantly higher rate of improvement compared to the placebo counterpart (81.3 vs 45.8%, p=0.03). After adjustment for age and baseline MPI score, we found a significant interaction between gender and treatment (p=0.05), suggesting that the effect of amino acid supplementation on MPI change is different in men compared to women.
Safety
A very small proportion of patients (5, 3.9% of the study population) reported treatment adverse events, 1 in the AG group and 4 in the placebo group, respectively (Fisher’s exact test: 0.365). The reported adverse events were headache (1 patient in AG), diarrhea (3 cases in the placebo group), and vomiting (1 patient in the placebo group).
Discussion
Decline in health and functional status is common in older patients admitted to the hospital for an acute medical event, and sarcopenia is often associated with both hospitalization and loss of function.Citation17 Oral amino acid supplementation is considered an effective intervention to prevent or attenuate the loss of muscle mass and strength associated with inactivity and reduced intake of nutrients.Citation18,Citation19 Furthermore, it has been suggested that amino acid supplementation might counteract other negative multisystemic biological pathways, including insulin resistance, systemic inflammation, and enhanced oxidative stress, that are often activated in older acute patients.Citation20
This study investigated the effect of adding a specialized dietetic aliment with 12 g of amino acids to standard of care on change in global health status as measured by the MPI score. One month after treatment, the MPI score significantly decreased in the overall sample without significant differences in both study groups. This finding suggests that the overall improvement of the health status of the study population over time is independent of AG treatment. Nevertheless, in the analysis stratified according to gender, we found that men allocated in the experimental group had a significantly higher probability of MPI improvement compared to the counterpart allocated to placebo, whereas no difference was detected in women.
These findings are in line with the results of a recent meta-analysis of trials conducted on medical inpatients that did not show any significant effect of nutritional supplementation on mortality, inhospital infection, and functional status.Citation14 Similarly, a previous Cochrane systematic review and meta-analysisCitation21 failed to demonstrate a clear significant benefit of protein and energy supplementation in terms of functional status in older people at risk of malnutrition. A more recent study, not included in the abovementioned meta-analyses,Citation22 demonstrated that among acutely ill malnourished older patients, oral nutrition and caloric supplementation including known essential macro- and micronutrients, high protein composition supplemented with beta-hydroxy beta-methylbutyrate decreased mortality and improved indices of nutritional status during the 90-day observation period, but no information was collected on functional and overall health status. Conversely, when oral nutritional supplementation has been combined with physical exercise program, a significant benefit in terms of muscle mass, muscle strength, physical performance, and quality of life has been demonstrated in both frail institutionalized older peopleCitation23 and sarcopenic patients enrolled in rehabilitation programs.Citation24
Only a few studies specifically investigated the effect of oral amino acid supplementation using a composite indicator of global health status like the MPI. Indeed, most of the previous studies investigated single specific aspects of health status including muscle mass, grip strength, physical performance, ADL disability, and quality of life. MPI summarizes in a single score the status of several domains of health of older people including functional and cognitive status, nutritional status, multimorbidity, polypharmacy, and social status. Impairment of these domains has been recognized as key determinant of frailty of older people. Globally taken, the results of our study did not confirm the hypothesis that oral amino acid supplementation for a period of 4 weeks significantly reduces the frailty status and overall health condition in acutely ill patients after being discharged from the hospital. However, in line with previous studies that demonstrated a greater response to amino acid supplementation in men compared to women,Citation25,Citation26 this study suggests that oral amino acid supplementation might be more effective in men compared to women.
MPI might not be sensitive enough to capture the effect of amino acid supplementation. Although no effect was detected on any of the different domains assessed by MPI, we were not able to assess differences in other potential end points including muscle mass, strength, and function. A second potential explanation for the lack of difference in the primary outcome of the study might be a very high rate of MPI improvement during the follow-up. Indeed, in a previous observational study conducted in a large cohort of hospitalized older patients, we demonstrated a mean MPI change of −0.003 points between baseline and hospital discharge.Citation27 Conversely, in this study, the average MPI change was −0.03, which is 10 times higher compared to the previous observation; furthermore, MPI score significantly improved in both study groups reducing the likelihood of detecting a significant effect of the active intervention. Finally, 4 weeks of nutritional supplementation might not be sufficient to achieve a significant improvement of the overall health status of older frail patients.
This double-blind, randomized, placebo-controlled study showed that a specialized, dietetic aliment with 12 g amino acids did not alter the primary composite end point of MPI change after 30-day treatment period in an unselected sample of acutely ill older adults hospitalized for an acute medical problem. However, oral amino acid supplementation in addition to the standard care was associated with higher likelihood of MPI improvement among men. Further analyses are required to confirm and understand the biological mechanism(s) underlying these observed effects.
Acknowledgments
The abstract of this paper was presented at the XXXI Conference of the Società Italiana di Geriatria Ospedale Territorio as oral presentation with interim findings. The poster’s abstract was published in “Abstract book” in Geriatric Care. 2017;3 (1S): https://doi.org/10.4081/gc.2017.6813.
Disclosure
The authors report no conflicts of interest in this work.
Supplementary material
Table S1 Composition of one sachet of Aminoglutam®
References
- CreditorMCHazards of hospitalization of the elderlyAnn Intern Med19931182192238417639
- VolpatoSOnderGCavalieriMCharacteristics of nondisabled older patients developing new disability associated with medical illnesses and hospitalizationJ Gen Intern Med20072266867417443376
- MartoneAMBianchiLAbetePThe incidence of sarcopenia among hospitalised older patients. Results from the Glisten StudyJ Cachexia Sarcopenia Muscle2017890791428913934
- SullivanDHSunSWallsRCProtein-energy undernutrition among elderly hospitalized patients: a prospective studyJAMA19992812013e910359390
- SolerteSBFioravantiMLocatelliEImprovement of blood glucose control and insulin sensitivity during a long-term (60 weeks) randomized study with amino acid dietary supplements in elderly subjects with type 2 diabetes mellitusAm J Cardiol200810182E88E
- LimSLOngKCChanYHLokeWCFergusonMDanielsLMalnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortalityClin Nutr201231345e5022122869
- BallyMRBlaser YildirimPZBounoureLNutritional support and outcomes in malnourished medical inpatients: a systematic review and meta-analysisJAMA Intern Med2016176435326720894
- PilottoAFerrucciLFranceschiMDevelopment and validation of a Multidimensional Prognostic Index for one-year mortality from comprehensive geriatric assessment in hospitalized older patientsRejuvenation Res20081115116118173367
- VolpatoSBazzanoSFontanaAFerrucciLPilottoAon behalf of the MPI-TriVeneto Study GroupMultidimensional prognostic index predicts mortality and length of stay during hospitalization in the older patients: a multicenter prospective studyJ Gerontol A Biol Sci Med Sci201570323329
- PilottoASancarloDPellegriniFon behalf of the FIRI-SIGG Study GroupThe Multidimensional Prognostic Index predicts in-hospital length of stay in older patients: a multicenter prospective studyAge Ageing201645909626764398
- KatzSDownsTDCashHRProgress in the development of an index of ADLGerontologist19701020305420677
- LawtonMPBrodyEMAssessment of older people: self-maintaining and instrumental activities of daily livingGerontologist196991791865349366
- PfeifferEA short portable mental status questionnaire for the assessment of organic brain deficit in elderly patientsJ Am Geriatr Soc1975234334411159263
- LinnBLinnMGurelLThe cumulative illness rating scaleJ Am Geriatr Soc1968166226265646906
- GuigozYVellasBThe mini nutritional assessment (MNA) for grading the nutritional state of elderly patients: presentation of the MNA, history and validationNestle Nutr Workshop Ser Clin Perform Progr19991311
- BlissMRMcLarenRExton-SmithANMattresses for preventing pressure sores in geriatric patientsMon Bull Minist Health Public Health Lab Serv1966252382686013600
- BianchiLAbetePBellelliGGLISTEN Group InvestigatorsPrevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: the GLISTEN studyJ Gerontol A Biol Sci Med Sci2017721575158128329345
- FerrandoAAPaddon-JonesDHaysNPEAA supplementation to increase nitrogen intake improves muscle function during bed rest in the elderlyClin Nutr201029182319419806
- DeerRRGoodlettSMFisherSRA randomized controlled Pilot trial of interventions to improve functional recovery after hospitalization in older adults: feasibility and adherenceJ Gerontol A Biol Sci Med Sci20187318719328591764
- PasiniEAquilaniRDioguardiFSD’AntonaGGheorghiadeMTaegtmeyerHHypercatabolic syndrome: molecular basis and effects of nutritional supplements with amino acidsAm J Cardiol200810111E15E
- MilneACPotterJVivantiAAvenellAProtein and energy supplementation in elderly people at risk from malnutritionCochrane Database Syst Rev20092CD003288
- DeutzNEMathesonEMMatareseLENOURISH Study GroupReadmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: a randomized clinical trialClin Nutr2016351182626797412
- AbizandaPLópezMDGarcíaVPEffects of an oral nutritional supplementation plus physical exercise intervention on the physical function, nutritional status, and quality of life in frail institutionalized older adults: the ACTIVNES studyJ Am Med Dir Assoc201516439.e9e16
- RondanelliMKlersyCTerracolGWhey protein, amino acids, and vitamin D supplementation with physical activity increases fat-free mass and strength, functionality, and quality of life and decreases inflammation in sarcopenic elderlyAm J Clin Nutr201610383084026864356
- SmithGIAthertonPVillarealDTDifferences in muscle protein synthesis and anabolic signaling in the postabsorptive state and in response to food in 65–80 year old men and womenPLoS One20083e187518365020
- Alemán-MateoHMacíasLEsparza-RomeroJAstiazaran-GarcíaHBlancasALPhysiological effects beyond the significant gain in muscle mass in sarcopenic elderly men: evidence from a randomized clinical trial using a protein-rich foodClin Interv Aging2012722523422866000
- VolpatoSDaragjatiJSimonatoMFontanaAFerrucciLPilottoAChange in the Multidimensional Prognostic Index Score during hospi-talization in older patientsRejuvenation Res20161924425126905632