Abstract
Background
Residents of aged care facilities use increasingly complex medication regimens. Reducing unnecessary medication regimen complexity (eg, by consolidating the number of administration times or using alternative formulations) may benefit residents and staff.
Objective
To develop and validate an implicit tool to facilitate medication regimen simplification in aged care facilities.
Method
A purposively selected multidisciplinary expert panel used modified nominal group technique to identify and prioritize factors important in determining whether a medication regimen can be simplified. The five prioritized factors were formulated as questions, pilot-tested using non-identifiable medication charts and refined by panel members. The final tool was validated by two clinical pharmacists who independently applied the tool to a random sample of 50 residents of aged care facilities to identify opportunities for medication regimen simplification. Inter-rater agreement was calculated using Cohen’s kappa.
Results
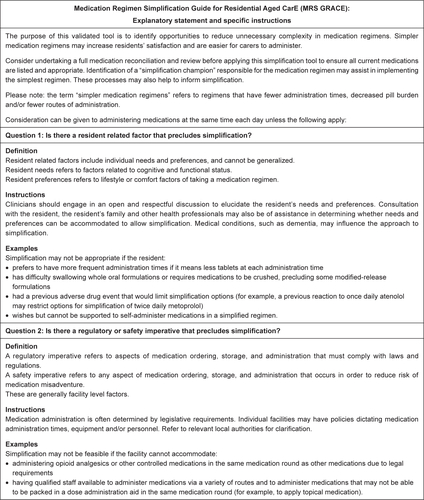
The Medication Regimen Simplification Guide for Residential Aged CarE (MRS GRACE) was developed as an implicit tool comprising of five questions about 1) the resident; 2) regulatory and safety requirements; 3) drug interactions; 4) formulation; and 5) facility and follow-up considerations. Using MRS GRACE, two pharmacists independently simplified medication regimens for 29/50 and 30/50 residents (Cohen’s kappa=0.38, 95% CI 0.12–0.64), respectively. Simplification was possible for all residents with five or more administration times. Changing an administration time comprised 75% of the two pharmacists’ recommendations.
Conclusions
Using MRS GRACE, two clinical pharmacists independently simplified over half of residents’ medication regimens with fair agreement. MRS GRACE is a promising new tool to guide medication regimen simplification in aged care.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Older people are using increasingly complex medication regimens. The number of people aged 65 years and older who use five or more medications in the USA tripled from 13% to 39% between 1988 and 2010.Citation1 Residents of aged care facilities, also known as “nursing homes,” “long-term care facilities,” or “residential aged care facilities,”Citation2 use an average of four to 17 regular medications.Citation3 Increasing regimen complexity accompanies increasing polypharmacy, which has been attributed to changing resident mix, better adherence to disease-specific clinical practice guidelines and reluctance to discontinue medications initiated by other prescribers.Citation4
Medication regimen complexity is a function of the number of medications, number of medication administration times, multiple or complicated dose formulations, and special instructions for medication administration (eg, to crush tablets, take with food or a specific fluid).Citation5 Initiatives to reduce the number of medications through “deprescribing” have attracted widespread attention.Citation6,Citation7 Simplification without altering therapeutic intent of medication regimens is possible through addressing the other factors that contribute to unnecessary complexity, and is of increasing interest.Citation8–Citation10 Medication regimen simplification has been identified as a priority area for geriatric pharmacotherapy by a panel of international experts.Citation11 The Victorian Government Department of Health and Human Services has introduced a new quality indicator for “more than four administration times” for aged care services in Victoria, Australia.Citation12 Recent Australian recommendations for the prevention of injury-related deaths in residential aged care services contain two recommendations (27 and 37) that support the need for medication regimen simplification. Recommendation 37 also recommends the development of standardized procedures to achieve medication simplification.Citation13
Although only a small number of residents may self-administer their medications,Citation2 there are multiple reasons to implement structured and comprehensive approaches to reduce medication regimen complexity in aged care facilities. Complexity is an independent risk factor for hospitalization from aged care facilities and discharge to aged care facilities.Citation14,Citation15 High complexity is associated with direct costs through time and workload to administer medications, and indirect costs through poorer resident health outcomes.Citation16,Citation17 Furthermore, unnecessarily complex medication regimens are burdensome and may lead to difficulty adhering to prescribed administration times, increased risk of potentially inappropriate medication use, increased risk of medication administration error, and decreased resident satisfaction.Citation18,Citation19 Reducing the number of medication administration times has been found to improve health-related quality of life in people with a variety of medical conditions.Citation20 Despite this, there remains no structured method to guide medication regimen simplification in aged care facilities. The aim of this study was to develop and validate a judgment-based (ie, implicit) toolCitation21 to facilitate medication regimen simplification in aged care facilities.
Method
Study design
This study was completed in two phases. Phase 1 focused on development of a regimen simplification tool. The developed tool was then validated in phase 2. Qualitative elements of this study in the development phase were reported according to the consolidated criteria for reporting qualitative studies where possible.Citation22 This study was approved by the Monash University Human Research Ethics Committee (project number 0731). For the validation in phase 2, individual resident consent to review their medication charts was waived by the Monash University Human Research Ethics Committee due to the non-identifiable nature of the copies of the medication charts used.
Phase 1: development of the medication regimen simplification tool
A modified nominal group technique (NGT) was used to develop the medication regimen simplification tool. NGT is a structured process to explore a research question, clarify ideas, and gain consensus among experts.Citation4,Citation23,Citation24 An expert panel was convened in October 2016. The panel was purposefully selected to comprise health professionals with practical experience in aged care and consumer representation. Potential panelists were identified through their clinical leadership roles and with the assistance of an organization that provides aged care services. Potential panelists were approached by email with a short statement of the purpose of the meeting. The panel was held at an aged care facility and moderated by two pharmacist researchers with experience using NGT (JSB and JS).
Following introductions, the facilitators introduced the concept of medication regimen complexity and the aim of the session. The focus was specifically identified as simplifying the existing regimen, rather than discontinuing medications. The panel was divided into two multidisciplinary pairs and one group of three. This approach was chosen to encourage collaboration and sharing of perspectives. Firstly, each pair and group of three generated and presented an exhaustive list of factors to consider when deciding whether a medication regimen could be simplified. Secondly, these factors were grouped into themes through moderated discussion with the full panel. Thirdly, each multidisciplinary pair or group of three was assigned a theme by facilitators, and separately tasked with formulating question or statement prompts that could be incorporated into an implicit tool. The panel discussed all the questions and statements for duplication, feasibility, and priority, and the final key questions for the tool were determined. Discussion points were transcribed during the session.
Each multidisciplinary pair and group of three applied the draft simplification tool to identify opportunities for simplification for a sample medication regimen listed on a non-identifiable medication chart of a resident of an aged care facility. The panel performed an initial face validity check and discussed the ordering of the prompts and saturation of factors important to consider for regimen simplification. The tool was refined by investigators, taking care to capture all ideas generated at the meeting. The five prioritized factors were formulated as questions and circulated to the full expert panel for endorsement.
Phase 2: validation of the medication regimen simplification tool
The validity of the developed tool was established by comparing the proportion of residents in a sample whose regular medications could be simplified (eg, any change to the administration time, route of administration, or use of combination or extended release preparations) when the tool was applied by two people independently.
Sample selection
A stratified random sample of 50 residents from a census sample of 439 residents from 10 Australian aged care facilities were used to validate the developed tool. Non-identifiable medication administration charts were collected as part of an earlier unrelated study undertaken by the research team. The random sample in the present validation study was selected from medication charts for residents with two or more medication administration times (n=432) because there was no scope to reduce the number of administration times for residents with one administration time.
Clinical and medication data
The medication charts had standard dose administration times of pre-breakfast, breakfast, mid-morning, lunch, mid-afternoon, tea, evening, and settling. The name, strength, dose, dose form, route, administration time, and start date were recorded for each medication. Resident age (in years), allergies, medical diagnoses, and any notes pertaining to medication administration were also recorded.
Application of the medication regimen simplification tool
Two clinical pharmacists (A and B) were introduced to the concept of medication regimen simplification and the developed tool. The two clinical pharmacists independently applied the developed tool to the non-identifiable medication charts. The clinical pharmacists had three and ten years’ experience performing medication reviews for residents of aged care facilities, respectively. A working relationship between the clinical pharmacists did not exist prior to this study. When applying the simplification tool, the pharmacists were instructed to assume each resident’s medication regimen had already been reviewed for clinical appropriateness. The pharmacists also assumed that the resident and facility would be willing and able to accommodate any recommendation. The pharmacists manually noted details of any recommended changes (medication name, form, route, dose, administration time, and any required monitoring or follow up), and reasons for not being able to simplify a medication regimen (if applicable).
Statistical analysis
Primary outcome measure
The agreement between two users of the developed tool when applied to a sample of residents whose regular medications could be simplified was established using inter-rater reliability analysis using Cohen’s kappa. A dichotomous variable of “able to simplify the medication regimen” and “not able to simplify the medication regimen” was used. The inter-rater reliability was considered slight if between 0.0 and 0.2, fair if between 0.21 and 0.4, moderate if between 0.41 and 0.6, substantial if between 0.61 and 0.8, and almost perfect if between 0.81 and 1.0.Citation25,Citation26 To assist interpretation of kappa, the maximum attainable kappa was also calculated.Citation27 Average proportions of agreement for positive and negative responses, and raw percentage agreement were also reported to support interpretation.Citation25 Microsoft Excel (2013) (Microsoft Corporation, Redmond, WA, USA) and SAS v9.4 (SAS Institute, Cary, NC, USA) were used for data analysis.
Secondary outcome measures
A secondary analysis was conducted for simplification that included a decrease in administration times. The inter-rater agreement for ability to decrease the number of regular administration times per day was calculated separately. All recommendations for and barriers to simplification were analyzed descriptively.
Sample size calculation for validation phase
To detect with 80% power a Cohen’s kappa value of 0.8 against a null hypothesis value of 0.4,Citation25 the minimum required sample size was estimated to be 42 residents.Citation27 A probability of simplification of 0.5 was assumed, based on a previous proportion of older people with medication regimens that could be simplified.Citation28 A random number generator was used to select the final sample of 50 residents.Citation29 The final sample contained the same proportion of residents with each number of dose administration times as the census sample.
Results
Phase 1: development of the simplification tool
Eleven people were approached to participate in the expert panel meeting. Two people declined an invitation to participate due to travel. Two people who agreed to participate did not attend the meeting. Seven people attended the expert panel meeting (five male and two female members). Panel members had experience in prescribing, reviewing, administering or receiving medications in aged care (a general medical practitioner [GP, or family physician], a clinical pharmacologist, a geriatrician, two medication review pharmacists, a nurse practitioner, and a consumer advocate).
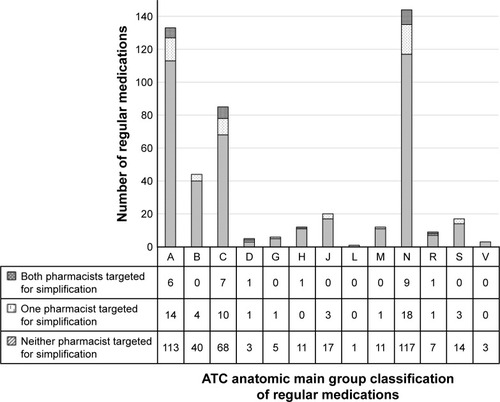
During the five-hour meeting, the expert panel generated 52 ideas in small groups. Investigators grouped these ideas into three broad themes: 1) environment/system (eg, multiple prescribers, continuity of care, a single “gate keeper” for the overall regimen); 2) resident/carer (eg, variation in symptoms with time, patient preference and understanding of medications); and 3) medication/regimen (eg, size and presentation of solid oral dose forms, medication absorption profile). A series of question or statement prompts were generated by further small group work. When applied to a medication chart, the panel were able to use the prompts to simplify the medication regimen. The prompts and the initial tool were assessed to have good content and face validity, respectively, after application to a sample medication chart from an aged care facility. The initial prompts were condensed into five questions for the final tool: the Medication Regimen Simplification Guide for Residential Aged CarE (MRS GRACE) and an accompanying explanatory statement (Box 1; see Figure S1 for full explanatory statement).
Phase 2: validation of the simplification tool
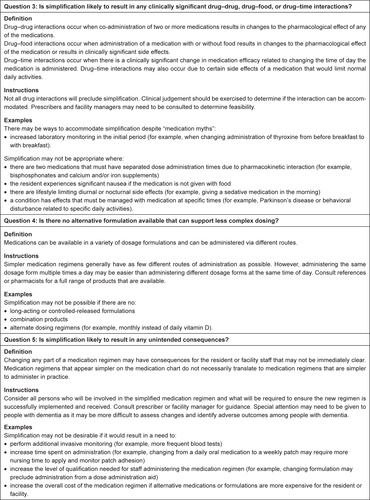
Of the 50 residents included in the validation phase, the mean age (±SD) was 82.3±9.8 years and 76% were female (n=38). Residents took a mean (±SD) of 9.9±4.2 regular medications. In total, residents in the validation sample took 491 regular medications. The most frequent number of regular administration times per day was four (34%, n=17), while 14% (n=7) of residents had two administration times per day, 26% (n=13) had three, 16% (n=8) had five, and 10% (n=5) had six or more ().
Figure 1 Agreement and ability to (A) simplify and (B) decrease regular administration times for residents in the validation sample, stratified by number of administration times per day for regular medications.
Consideration can be given to administering all medications at the same time each day unless the following apply:
Is there a resident related factor that precludes simplification?
Is there a regulatory or safety imperative that precludes simplification?
Is simplification likely to result in any clinically significant drug–drug, drug–food, or drug–time interactions?
Is there no alternative formulation available that can support less complex dosing?
Is simplification likely to result in any unintended consequences for the resident or facility?
Each pharmacist identified opportunities and made recommendations for simplification for 30/50 and 29/50 residents’ medication regimens (). There were 22 residents who both pharmacists agreed could have simplified medication regimens, and 13 residents’ medication regimens that both pharmacists agreed could not be simplified. Simplification recommendations were made for all residents with five or more administration times (). Three quarters of simplification recommendations were to move an administration time without changing the dose administered (). The raw agreement between pharmacists was 70%. The proportions of positive and negative agreement were 75% and 63%, respectively. The pharmacists had fair agreement regarding simplification of medication regimens (Cohen’s kappa=0.38±0.13, 95% CI 0.12–0.64). The maximum obtainable kappa statistic was 0.96.
Table 1 Frequency of each type of recommendation to simplify medication charts
Each pharmacist decreased the number of regular administration times for 23/50 residents, of which 18 were for the same residents (). Both pharmacists eliminated one administration time for 21 residents, and two administration times for two residents (not the same residents). Neither pharmacist was able to recommend simplification for residents with two administration times. The pharmacists had moderate agreement regarding decreasing administration times only (Cohen’s kappa=0.48±0.12, 95% CI 0.24–0.72).
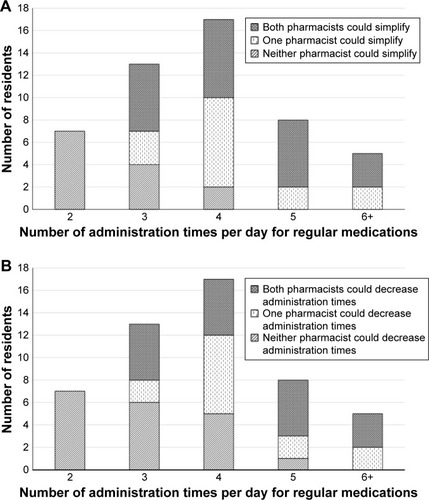
When classified by the anatomical therapeutic chemical (ATC) main group, nervous system medications were the most frequently implicated in recommendations (ATC group N) (). Paracetamol was the most frequently implicated drug in this class (n=10/60 and 8/46 recommendations). Twelve percent of nervous system medications could be simplified (n=19/144 and 17/144). Cardiovascular medications (ATC group C, eg, atorvastatin, furosemide) had the highest level of disagreement, with pharmacists A and B recommending simplification for 19% and 9% of cardiovascular medications (n=16/85 and 8/85 medications), respectively.
Figure 2 Agreement and ability to simplify regular medications in medication regimens of residents in the validation sample, categorized by Anatomic Therapeutic Chemical (ATC) main group classification.
All barriers to simplification noted during the validation were possible barriers identified during the development phase. Barriers related to medication, resident, and facility factors. Medication factors included frequent dosing of medications for Parkinson’s disease, and time-specific administration of medications due to behavior or symptomatic management. Examples of resident related factors were swallowing difficulty, and existing anxiety about taking multiple tablets. Facility related barriers included special administration procedures surrounding controlled analgesic medications and warfarin.
Discussion
To our knowledge, MRS GRACE is the first tool to assist clinicians to identify opportunities to simplify medication regimens in aged care facilities. Taking medications is a burden for both staff and residents in aged care facilities, with many residents resisting medications. Reducing the number of times a day that the stress of taking medications occurs has benefits for both staff and residents. Furthermore, the residents can benefit from the opportunity costs that arise from freeing up nursing time from unnecessarily frequent medication administration. This tool provides a standardized approach to regimen simplification which may counteract the variability that may already be present in clinical pharmacist and other medication reviews for consistent results.
The scope for simplification of medication regimens in aged care facilities is substantial, despite pharmacists regularly performing similar clinical work and undergoing accreditation to perform full medication reviews. The medication charts used in the present study were from aged care facilities where clinical pharmacists conduct Australian Government funded residential medication management reviews (RMMRs).Citation2 Therefore, it would appear that further simplification is possible even among recipients of medication review. MRS GRACE may serve as a prompt and reminder for pharmacists or physicians when conducting medication management reviews.
A wide range of stakeholders were consulted in the development of MRS GRACE. At the beginning of the development phase, our panel of experts generated a comprehensive list of distinct factors. Although a number of concepts were subsequently considered peripheral to regimen simplification, concepts judged important to optimizing medication regimens were incorporated into the explanatory statement where relevant. Examples included ensuring the accuracy of medication records, recognizing that residents may have multiple prescribers with different treatment priorities and the need to ensure continuity across transitions of care. The expert panel recognized that regimen simplification is distinct from “medication reconciliation” and “deprescribing”,Citation30 although successful simplification is dependent on first obtaining an accurate medication list and ensuring all medications are clinically indicated. The incorporation of all relevant aspects identified contributed to face validity of the developed tool.
MRS GRACE was purposefully developed as a judgement-based, or implicit, tool.Citation21 Implicit tools, such as the Medication Appropriateness Index (MAI), avoid making recommendations for specific medications or situations.Citation31 Clinicians are thereby able to use it in different aged care settings and across different countries because the tool prompts evaluation of each individual facility’s protocols and processes. The implicit format was considered the most appropriate for older people living in aged care facilities, due to its flexibility and the lack of evidence to inform prescribing in this setting.Citation32,Citation33 This also means there is no single ideal “solution” as to how a medication regimen may be simplified. MRS GRACE includes in the explanatory statement some further guidance should clinical knowledge be limited (eg, consult a pharmacist for full range of formulations). Therefore, although agreement calculated by Cohen’s kappa was fair, the higher raw agreement demonstrates that the tool is effective in aiding pharmacists to simplify medication regimens. The similar proportion of positive and negative agreements also indicates a lack of bias during interpretation and application of the tool.
While highly mobile, implicit tools rely on the user having good pharmacological knowledge and familiarity with different product formulations. For example, to effectively consider question 4 “Is there an alternative formulation that can support less complex dosing?”, clinicians must combine knowledge of available formulations with knowledge of each resident’s ability to use alternative formulations (eg, due to swallowing difficulties that require medications to be crushed). While MRS GRACE was validated by two pharmacists, it was piloted during the expert panel meeting by a range of different health professionals. The expert panel perceived that application of MRS GRACE could be undertaken by any health professional group with the knowledge required to apply the implicit tool in their context.
The expert panel identified and the validation study subsequently confirmed that medication regimen complexity may be unavoidable for various reasons. This may be due to the medication itself. “Time critical” medications, such as short-acting insulins or medications for Parkinson’s disease, may cause harm or reduced efficacy if administration is early or delayed.Citation34 Other reasons relate to the resident. Some residents may prefer to spread their medications over multiple administration times rather than take all medications at the same time each day. The expert panel recognized that, “Is there a resident related factor that precludes simplification?”, was considered an important first prompt to elucidate whether residents desire a simplified medication regimen. However, a specific list of medications or reasons that preclude simplification is not included in the tool as there may be cases where barriers can be addressed at the discretion of the clinician. This also increases the generalizability of MRS GRACE, as medications or reasons that preclude simplification may also be country-specific.
MRS GRACE prompts users to evaluate barriers to simplification through the wording “clinically significant” in question 3. In the validation phase, this was a source of disagreement. For example, one pharmacist considered that the falls risk associated with administering mirtazapine at dinner outweighed the potential benefit of administering mirtazapine with residents’ other dinner medications, and therefore did not suggest changing bedtime administration times. The “clinically significant” judgement was also a source of simplification recommendations through correcting common medicine misconceptions. A recurring example in the validation was moving the administration time of atorvastatin. The misconception was that statins should be taken at night to increase drug efficacy. However, while short-acting statins are slightly but significantly more effective if taken at night, long-acting statins (eg, atorvastatin) are effective at any time.Citation35
Limitations
In developing the tool, a limitation was that we were unable to consult with residents directly to ascertain resident related factors prioritized as important to residents taking medication regimens. We instead engaged a resident advocate to contribute to the development of MRS GRACE. However, the resident perspective would also be considered when deciding whether to implement the identified opportunities for simplification, a step that may often be outside the scope of MRS GRACE.
In the validation phase, agreement was measured between two pharmacists despite the tool not being specifically targeted for pharmacist use. Clinical information about the resident that may impact on decision making was not available and pharmacists A and B were unable to speak with residents, caregivers or facility staff. Therefore, it was not possible to fully consider the resident perspective or facility resources section of the simplification tool (questions 1 and 2, respectively), or clarify any unintended consequences that the simplified medication regimen may have (question 5). This may have decreased agreement as disagreement between the pharmacists in the validation phase may be resolved in practice by consulting the prescriber or care manager in the aged care facility.
There was also no scope to assess the clinical appropriateness of the simplified regimen, or if a prescriber would have accepted and implemented the simplification recommendations generated as a result of using the tool. While the safety of the regimen is the ideal measure, it is very difficult to quantify. We used inter-rater reliability as an adequate surrogate marker, assuming that the pharmacists applied the tool as intended, to simplify medication regimens without sacrificing safety.
Future directions
Simplification could be undertaken as a stand-alone activity, or as part of comprehensive medication review programs and geriatric assessments undertaken by physicians and pharmacists in aged care facilities. However, further research is needed to explore possible differences and similarities in application of the tool by different health professionals. It may also be appropriate to use MRS GRACE following medication reconciliation on admission to aged care facilities, or after returning from hospital. The panel suggested that a single “simplification champion” could act as a “gate keeper” to take responsibility for coordinating regimen simplification in aged care facilities at these times. Research to understand uptake of simplification recommendations, and impact of medication simplification on outcomes for residents and aged care providers, is currently underway in an ongoing randomized controlled trial (SImplification of Medications Prescribed to Long-tErm care Residents [SIMPLER]).Citation36
Conclusion
By applying MRS GRACE, two clinical pharmacists independently simplified two-thirds of residents’ medication regimens with fair agreement. MRS GRACE is a validated tool that may be adopted by clinicians and aged care providers as a standardized approach to simplification and may reduce the burden of medication administration for aged care providers.
Acknowledgments
The authors gratefully acknowledge funding provided by the National Health and Medical Research Council (NHMRC) Partnership Centre on Dealing with Cognitive and Related Functional Decline in Older People. The contents of the published materials are solely the responsibility of the individual authors identified, and do not reflect the views of the NHMRC and any other Funding Bodies or the Funding Partners.
The abstract of this paper was presented at the NHMRC’s National Institute for Dementia Research Australian Dementia Forum in Melbourne, VIC, Australia in October 2017 as a poster presentation with interim findings. The poster’s abstract was published in “Special Supplement: Australian Dementia Forum Abstracts” in the Australian Journal of Dementia Care.
Disclosure
JI is supported by an NHMRC Early Career Fellowship. MC is employed by Helping Hand Aged Care, an organization providing residential aged care services. CPA was employed by Ward Medication Management, an organization providing medication review services to aged care facilities. The authors report no other conflicts of interest in this work.
References
- CharlesworthCJSmitELeeDSHAlramadhanFOddenMCPolypharmacy among adults aged 65 years and older in the United States: 1988–2010J Gerontol A Biol Sci Med Sci201570898999525733718
- SluggettJKIlomäkiJSeamanKLCorlisMBellJSMedication management policy, practice and research in Australian residential aged care: current and future directionsPharmacol Res2017116202827965033
- JokanovicNTanECKDooleyMJKirkpatrickCMBellJSPrevalence and factors associated with polypharmacy in long-term care facilities: a systematic reviewJ Am Med Dir Assoc2015166535.e1535.e12
- JokanovicNTanECDooleyMJKirkpatrickCMElliottRABellJSWhy is polypharmacy increasing in aged care facilities? The views of Australian health care professionalsJ Eval Clin Pract201622567768226804719
- GeorgeJPhunY-TBaileyMJKongDCMStewartKDevelopment and validation of the medication regimen complexity indexAnn Pharmacother20043891369137615266038
- ScottIAHilmerSNReeveEPotterKCouteurDRigbyDReducing inappropriate polypharmacy: the process of deprescribingJAMA Intern Med201517582783425798731
- TurnerJPEdwardsSStannersMShakibSBellJSWhat factors are important for deprescribing in Australian long-term care facilities? Perspectives of residents and health professionalsBMJ Open201663e009781
- WittickeDSeidlingHMLohmannKSendAFHaefeliWEOpportunities to reduce medication regimen complexity: a retrospective analysis of patients discharged from a university hospital in GermanyDrug Saf2013361314123315294
- ElliottRAO’CallaghanCPaulEGeorgeJImpact of an intervention to reduce medication regimen complexity for older hospital inpatientsInt J Clin Pharm201335221722423212732
- TamSHYHirschJDWatanabeJHMedication regimen complexity in long-term care facilities and adverse drug events-related hospitalizationsConsult Pharm201732528128428483008
- TanECKSluggettJKJohnellKResearch priorities for optimizing geriatric pharmacotherapy: an international consensusJ Am Med Dir Assoc201819319319929361432
- SluggettJKStasinopoulosJBellJSMedication management by informal caregivers – under-recognized and under-supportedRes Social Adm Pharm201814321521729153621
- IbrahimJERecommendations for Prevention of Injury-Related Deaths in Residential Aged Care ServicesSouthbankHealth Law & Ageing Research Unit, Department of Forensic Medicine, Monash University2017
- LalicSSluggettJKIlomäkiJPolypharmacy and medication regimen complexity as risk factors for hospitalization among residents of long-term care facilities: a prospective cohort studyJ Am Med Dir Assoc201617111067.e11067.e627780570
- WimmerBCDentEVisvanathanRPolypharmacy and medication regimen complexity as factors associated with hospital discharge destination among older people: a prospective cohort studyDrugs Aging201431862363024862100
- SchoonoverHCorbettCFWeeksDLWillsonMNSetterSMPredicting potential postdischarge adverse drug events and 30-day unplanned hospital readmissions from medication regimen complexityJ Patient Saf201410418619125408236
- Hixson-WallaceJADotsonJBBlakeySAEffect of regimen complexity on patient satisfaction and compliance with warfarin therapyClin Appl Thromb Hemost200171333711190902
- StangeDKristonLvon WolffABaehrMDartschDCMedication complexity, prescription behaviour and patient adherence at the interface between ambulatory and stationary medical careEur J Clin Pharmacol201369357358022828657
- NothelleSKSharmaROakesAHJacksonMSegalJBDeterminants of potentially inappropriate medication use in long-term and acute care settings: a systematic reviewJ Am Med Dir Assoc2017189806.e1806.e17
- RichterAAntonSEKochPDennettSLThe impact of reducing dose frequency on health outcomesClin Ther20032582307233514512137
- HamiltonHJGallagherPFO’MahonyDInappropriate prescribing and adverse drug events in older peopleBMC Geriatr20099519175914
- TongASainsburyPCraigJConsolidated criteria for reporting qualitative research (Coreq): a 32-item checklist for interviews and focus groupsInt J Qual Health Care200719634935717872937
- Van de VenAHDelbecqALThe nominal group as a research instrument for exploratory health studiesAm J Public Health19726233373425011164
- HarveyNHolmesCANominal group technique: an effective method for obtaining group consensusInt J Nurs Pract201218218819422435983
- GisevNBellJSChenTFInterrater agreement and interrater reliability: key concepts, approaches, and applicationsRes Social Adm Pharm20139333033822695215
- LandisJRKochGGThe measurement of observer agreement for categorical dataBiometrics1977331159174843571
- SimJWrightCCThe kappa statistic in reliability studies: use, interpretation, and sample size requirementsPhys Ther200585325726815733050
- ElliottRAReducing medication regimen complexity for older patients prior to discharge from hospital: feasibility and barriersJ Clin Pharm Ther201237663764222607618
- HaahrMHaahrSTrue random number generator [homepage on the Internet]1998 Available from: https://www.random.org/Accessed January 24, 2017
- PageACliffordRPotterKEtherton-BeerCA concept analysis of deprescribing medications in older peopleJ Pharm Pract Res Epub201837
- HanlonJTSchmaderKESamsaGPA method for assessing drug therapy appropriatenessJ Clin Epidemiol19924510104510511474400
- HilmerSNMcLachlanAJLe CouteurDGClinical pharmacology in the geriatric patientFundam Clin Pharmacol200721321723017521291
- ReeveETrenamanSCRockwoodKHilmerSNPharmacokinetic and pharmacodynamic alterations in older people with dementiaExpert Opin Drug Metab Toxicol201713665166828460576
- Institute for Safe Medication Practices (ISMP)Acute Care Guidelines for Timely Administration of Scheduled Medicines2011
- AwadKSerbanM-CPensonPEffects of morning vs evening statin administration on lipid profile: a systematic review and meta-analysisJ Clin Lipidol201797298528826569
- SluggettJKChenEYHIlomäkiJSImplification of Medications Prescribed to Long-tErm care Residents (SIMPLER): study protocol for a cluster randomised controlled trialTrials20181913729329559