Abstract
Purpose
To examine the effectiveness of the Elderly Activity Performance Intervention on reducing the risk of readmission in elderly patients discharged from a short-stay unit at the emergency department.
Patients and methods
The study was conducted as a nonrandomized, quasi-experimental trial. Three hundred and seventy-five elderly patients were included and allocated to the Elderly Activity Performance Intervention (n=144) or usual practice (n=231). The intervention consisted of 1) assessment of the patients’ performance of daily activities, 2) referral to further rehabilitation, and 3) follow-up visit the day after discharge. Primary outcome was readmission (yes/no) within 26 weeks. The study was registered in ClinicalTrial.gov (NCT2078466).
Results
No between-group differences were found in readmission. Overall, 44% of the patients in the intervention group and 42% in the usual practice group were readmitted within 26 weeks (risk difference=0.02, 95% CI: [−0.08; 0.12] and risk ratio=1.05, 95% CI: [0.83; 1.33]). No between-group differences were found in any of the secondary outcomes.
Conclusion
The Elderly Activity Performance Intervention showed no effectiveness in reducing the risk of readmission in elderly patients discharged from a short-stay unit at the emergency department. The study revealed that 60% of the elderly patients had a need for further rehabilitation after discharge.
Introduction
The number of elderly people admitted to an emergency department (ED) is increasing and today, elderly patients (65+) account for up to 25% of all ED admissions.Citation1–Citation4 Elderly patients discharged from the ED are at high risk of adverse outcomes such as readmission and death.Citation5–Citation8 Some of the risk factors leading to readmission are limitations in performing daily activities, comorbidity, and changes in medical condition.Citation6–Citation10 A large proportion of the elderly patients admitted to the ED are discharged directly to their home.Citation4 After discharge, they often need treatment, care, and rehabilitation from both hospital and primary care.Citation4,Citation8 A safe and coherent discharge of elderly patients is, therefore, highly dependent on effective collaboration between health care providers across hospital and primary care sectors.Citation11,Citation12
Studies emphasize that current ED discharge processes should be optimized to meet the complex needs of elderly patients.Citation8,Citation13,Citation14 So far, a number of interventions have been designed to improve the outcomes of elderly patients discharged from the ED, including comprehensive geriatric assessment, discharge planning, follow-up initiatives, and care transition interventions. However, the evaluations of the effectiveness of these interventions vary.Citation15–Citation19 A meta-analysis from 2011 concluded that there was no clear evidence supporting comprehensive geriatric assessment in terms of reducing risk of readmission.Citation20 In accordance with the review from 2011, a meta-analysis from 2015 concluded that there was no effect of care transition interventions on reducing readmission and mortality rates.Citation21 However, a systematic review from 2016 implied that pre-discharge interventions consisting of a follow-up visit after discharge may reduce the risk of readmission.Citation22 Follow-up visits have been recommended as a way to ensure sustainable care for elderly patients after discharge from the hospital.Citation14,Citation15,Citation18,Citation23 Only a few studies aiming to reduce the risk of readmission in elderly patients have focused on enhancing performance of daily activities, although it is a well-known high-risk factor for readmission.Citation6,Citation10,Citation15,Citation24
Occupational therapy as part of the hospital discharge generally aims at enhancing the patients’ performance of daily activities and ensuring that discharge and transition of elderly patients’ rehabilitation needs are coordinated.Citation25,Citation26 In Denmark, occupational therapy as part of hospital discharge planning is not a part of the standard discharge procedure of elderly patients at the ED.Citation27 A focus on elderly patients’ performance of daily activities and on ensuring a coherent discharge may be essential in reducing elderly patients’ risk of readmission after discharge, as these factors are associated with the risk of readmission.Citation7,Citation10,Citation12
The current study proposes a novel discharge planning intervention focusing on two risk factors in the prevention of readmissions: 1) to enhance performance of daily activities and 2) to ensure a coherent discharge to home. The “Elderly Activity Performance Intervention” (EAP-intervention) was developed and designed as a theory- and evidence-based intervention using the Intervention Mapping approach.Citation28,Citation29
The objective of this study was to examine the effectiveness of the EAP-intervention compared to usual practice in terms of reducing the risk of readmission in elderly patients discharged from the ED. We hypothesized that the intervention would be superior to usual practice in reducing the risk of readmission measured 26 weeks after discharge.
Patients and methods
Design
A nonrandomized, quasi-experimental, parallel study was conducted. Follow-up was performed at 30 days and at 26 weeks after discharge from the short-stay unit at the ED.
Participant enrollment and setting
The first part of the intervention took place in the period March–December 2014 at a short-stay unit in the ED at a 1,150-bed university hospital in Denmark, where ~42,000 patients are visiting the ED annually. In Denmark, a short-stay unit provides treatment and care for up till 48 hours, followed by patient discharge or transfer to an in-patient unit. The second part of the intervention took place at the patients’ home after discharge. In Denmark, the health care system is tax-financed and free of charge; home-based rehabilitation is offered after hospitalization.
The following criteria were used to recruit participants.
Inclusion criteria
Patients age 65+
Patients admitted with a medical diagnosis (as distinct from surgical or psychiatric diagnosis) to the short-stay unit
Patients who were residents in a larger municipality (Aarhus) in Denmark
Exclusion criteria
Patients transferred to other hospital departments
Patients admitted from a nursing home
Patients who were unable to communicate in Danish
Patients declared terminally ill
Patient allocation
Each week day at 8:00 am, a research occupational therapist reviewed a list of all patients admitted in the last 24 hours and screened them for eligibility. Due to limited resources and time, it was possible to include and allocate up to two patients to the intervention group per day. If more patients were eligible, allocation was based on the date of birth (day of the month). The two patients born closest to the first day of a month (eg, March 1) would be allocated to the intervention group. Patients not included in the intervention group were treated according to usual practice and formed the control group. Likewise, patients admitted after 8:00 am and meeting the inclusion criteria, but were discharged out of hours (afternoons and evenings) were allocated to the usual practice group.
Interventions
Usual practice
Patients in both groups received relevant medical treatment and care. Referral to occupational therapy and physiotherapy took place only if the medical or nursing staff considered it necessary. If the occupational therapist was summoned to asses a patient, the occupational therapist performed a short interview and a non-standardized observation of the patient’s performance of basic daily activities and the results were communicated to the municipality homecare staff. If necessary, nurses from the ED organized referral to nursing home care after discharge.
The EAP-intervention
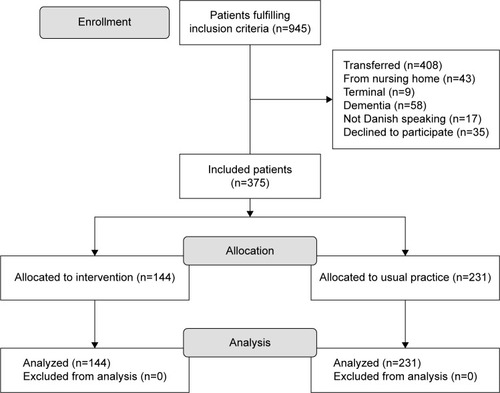
The EAP-intervention was offered in addition to usual practice. An extended description of how the intervention was developed and designed in accordance with theory and evidence is reported elsewhere.Citation29 The intervention was initiated immediately after the patient was allocated to the intervention group. The intervention consisted of three components ().
Figure 1 Overview of the Elderly Activity Performance Intervention.
Component 1
Assessment of the patients’ performance of daily activities using three performance-based measures: Timed Up and Go,Citation30,Citation31 30s-Chair Stand Test,Citation32 and Assessment of Motor and Process Skills.Citation33,Citation34 Limitations in performing daily activities were determined using the following cut-off values: Time Up and Go >12 seconds,Citation35 Chair Stand Test <8 times in 30 seconds,Citation36 and Assessment of Motor and Process Skills motor ability <1.50 logits and process ability <1.00 logits.Citation33 Component 1 was provided for all patients. Based on the results in component 1, patients with limitations in performing daily activities received components 2 and 3.
Component 2
A rehabilitation plan was prescribed for patients with identified limitations in performing daily activities. The rehabilitation plan included a description of the patient’s previous and current performance of daily activities and specified the need for further rehabilitation. Primary care was informed about the discharge, and visitation of the patient to further rehabilitation interventions was carried out on the same day in order to start the rehabilitation immediately after discharge.
Component 3
For patients with a prescribed rehabilitation plan, a home visit by an occupational therapist was performed the day after discharge. The home visit aimed to enhance the patient’s performance of daily activities and to start rehabilitation. The occupational therapist screened the home for safety risks and factors that potently could limit the performance of daily activities. If limitations and/or safety risks were identified, the occupational therapist made relevant modifications of the home environment. To ensure standardized procedures at the follow-up visit, a checklist was developed.
None of the three components in the EAP-intervention were applied to patients in the usual practice group.
Outcomes
The primary outcome was all-cause readmission within 26 weeks. Secondary outcomes were all-cause readmission within 30 days and all-cause mortality, number of contacts to general practitioners (GPs) and EDs (without admission) within 26 weeks, and time to first readmission. All data on outcome variables were obtained from the National Patient Register.
Data related to patient characteristics were extracted for both groups from the National Patient Register and included gender, age, civil status, admission diagnosis, comorbidity, and admission time. Comorbidity was measured with the Charlson’s Comorbidity Index calculated from International Statistical Classification of Diseases and Related Health Problems 10th Revision diagnosis retrieved from the National Patient Register, at the day of inclusion.Citation37–Citation39
Sample size estimation
Based on the literature, the intervention was expected to reduce the risk of readmission within 26 weeks with 16 percentage points, from 37% to 21%.Citation17 A total of 152 patients in each group were needed to achieve 80% power with a two-sided type I error of 5%, assuming that 10% of the participants were lost to follow-up, for example, due to death.
Statistical methods
A detailed statistical analysis plan was developed prospectively in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement, and data were reported according to the extended Consolidated Standards of Reporting Trials (CONSORT) statement.Citation40,Citation41 Hypothesis tests were conducted at the 5% level of significance and were two-sided. All analyses were performed using the Stata 14.2 statistics program. Biostatistician was consulted in developing the analysis plan and when performing the analyses.
First, a descriptive analysis was performed summarizing baseline characteristics for both the intervention group and the usual practice group. Data were presented as mean and SD or numbers and percentages. The two groups were compared and tested for significant differences at baseline using chi-square test, the Student’s t-test for normally distributed continuous variables, and the Wilcoxon rank sum test for nonparametric variables. Risk of readmission within 26 weeks was estimated by cumulative incidence proportion using a pseudo-value method accounting for death as a competing risk.Citation42,Citation43 The two groups were compared by risk difference (RD) and risk ratio (RR) with 95% CI. Due to the nonrandomized study design, similar analysis was performed by adjusting for factors that a priori were considered to be confounders: age, gender, and comorbidity. Thirty-day all-cause readmission and all-cause mortality within 26 weeks were estimated by RD and RR with 95% CI and secondly adjusted for potential confounding. Numbers of contacts to GPs and ED were described with median and range and differences were tested with nonparametric Wilcoxon rank sum test. Time to first readmission with unadjusted cumulative incidence proportions was illustrated in a graph. An explorative analysis was performed to compare the baseline differences for those patients in the control group admitted during the daytime and those admitted during afternoon and evenings, in order to include possible differences in the adjusted analyses. An exploratory analysis within the intervention group was performed to examine if the number of intervention components received was associated with the primary outcome, risk of readmission within 26 weeks.
Ethical approval and registrations
The ethical principles of the World Medical Association Declaration of Helsinki were followed.Citation44 The Regional Ethics Committee responded that no approval was required as the study was classified as a quality assurance project (J. nr.1-10-72-108-14). The study was approved by the Danish Data Protection Agency (J.nr. 2012-41-0763) and by the Danish Health Authority (3-3013-608/1/). The study was registered in ClinicalTrial.gov (NCT2078466). Patients included and allocated to the intervention group provided written informed consent. Patients allocated to the usual practice group were not informed about their participation, as only data from the National Patient Registry were used. The Danish Health Authority gave permission to obtain health-related data on patients in the usual practice group.
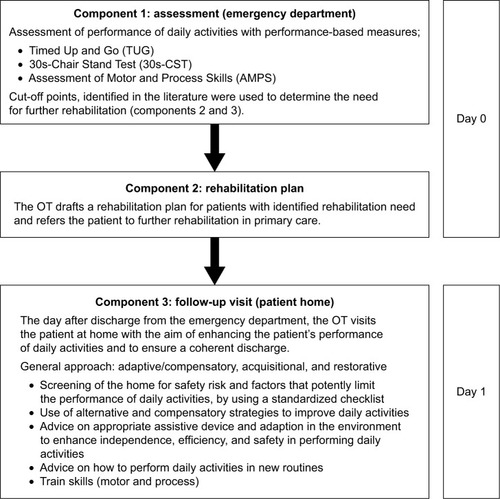
Results
During the inclusion period, 945 patients were screened for eligibility. A total of 410 patients met the inclusion criteria; 35 declined to participate. A total of 375 participants were enrolled in the study; 144 were allocated to the EAP-intervention and 231 to the usual practice group. The enrollment of study participants is shown in . No participants were excluded from the analysis.
Participant characteristics at baseline are shown in . Overall, the two groups appeared comparable at baseline concerning gender, diagnosis at discharge, comorbidity, and marital status. Patients in the intervention group were older on average than patients in the usual practice group (81 vs 78 years, p=0.003), and patients in the intervention group were admitted longer than patients in the usual practice group (0.94 [0.74; 1.33] vs 0.82 [0.57; 1.09] days, p=0.002).
Table 1 Baseline characteristics of the study population (N=375)
Readmission
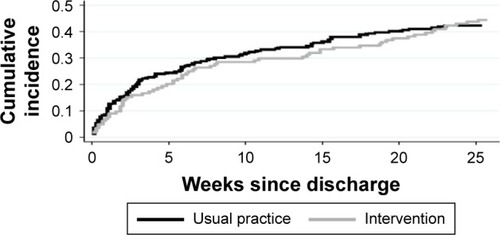
No between-group differences were found regarding the primary outcome readmission. A total of 44% of the patients in the intervention group and 42% of patients in the usual practice group were readmitted within 26 weeks (RD=0.02, 95% CI: [−0.08; 0.12] and RR=1.05, 95% CI: [0.83; 0.33]), as shown in and . There was no difference in 30 days readmission; 18% of the patients in the intervention group were readmitted and 23% in the usual practice group (RD=−0.05, 95% CI: [−0.13; 0.03] and RR=0.78, 95% CI: [0.51; 1.19]).
Table 2 Comparison of risk of readmission and risk of mortality for the study population (N=375)
Figure 3 Plots of cumulative incidence proportion for readmission within 26 weeks for the study population (N=375).
The within-group analysis of the usual practice group revealed differences in marital status and admission time on comparing those admitted in daytime with those admitted during afternoon and evenings. Patients in the usual practice group who were included in daytime had longer admission time; 1.06 (0.88; 1.92) vs 0.73 (0.42; 0.96) p<0.001 than those admitted during afternoons and evenings. Also, 47% of the patients in the usual practice group who were admitted in the afternoons and evenings and 34% of the patients admitted in daytime were married (p=0.044). Adjusting for those factors in combination with the a priori confounders age, gender, and comorbidity did not show any significant difference in either readmission within 26 weeks or readmission within 30 days ().
Mortality
Overall, the mortality 26 weeks after discharge was 10% in both groups. Adjustment for potential confounding did not show any difference ().
Contacts to GP and ED
The median number of contacts to the ED within a period of 26 weeks from inclusion in both groups was zero (). A total of 21% of the patients in the intervention group and 17% from the usual practice group had at least one contact to the ED during the 26 weeks.
Table 3 Contacts to GP and the ED within 26 weeks for the study population (N=375)
A total of 97% of the patients in the intervention group and 99% from the usual practice group had at least one contact to the GP during the 26 weeks. The median number of contacts to the GP for both groups was 9.
Exploratory analysis within the intervention group
shows the number of patients receiving each component of the intervention and the results from the performance-based assessment in component 1. All patients in the intervention group were assessed with at least one of the performance-based assessments in component 1. Based on the results from the assessment, a total of 87 (60%) of the patients in the intervention group were referred to primary care rehabilitation (component 2). Of these, 69 (79%) patients received a follow-up visit by the occupational therapist the day after discharge (component 3).
Table 4 Number of patients receiving each component of the EAP-intervention and results from the performance-based assessment in component 1 (n=144)
An exploratory analysis within the intervention group showed that 51% of the patients who had a need for all of the components in the EAP-intervention were readmitted within 26 weeks compared to 33% of the patients who only had need for component 1 (RD=0.18, 95% CI: [0.02; 0.35] and RR=1.55, 95% CI: [1.02; 2.36]), as shown in .
Table 5 Risk of readmission in the intervention group (n=144)
Discussion
The aim of this nonrandomized, quasi-experimental, parallel study was to examine the effectiveness of the EAP-intervention compared to usual practice on reducing the risk of readmission in elderly patients discharged from a short-stay unit at the ED. We did not find the EAP-intervention to be superior compared to usual practice in reducing the risk of readmission in our study population. In addition, none of the secondary outcomes differed significantly between the two groups. When exploring the effectiveness in relation to different subgroups such as gender, comorbidity, and age, no differences were found.
The intention with the EAP-intervention was to improve usual practice by enhancing the elderly patients’ performance of daily activities and ensure a coherent discharge, without changing the overall organization of the Danish health care system.
We hypothesized that the EAP-intervention was more efficient compared to usual practice, but our results did not corroborate this. The EAP-intervention was developed to enhance the elderly patients’ performance of daily activities and ensure a coherent discharge to home, assuming that this would reduce the risk of readmission. This assumption was based on evidence in the literature and the use of a logic model as recommended in the Intervention Mapping approach.Citation28,Citation29 The use of a logic model in the developing phase allowed us to focus directly on factors and their underlying determinants associated with risk of readmission. Although limitations in performing daily activities are a well-known risk factor for readmission in elderly patients, the EAP-intervention may not have been sufficiently intensive to address the complexity in the health needs of elderly patients as only two factors were specifically addressed: performance of daily activities and a coherent discharge.Citation7,Citation10,Citation12 Other risk factors for readmission, such as nutritional status and polypharmacy, were not specifically addressed in this intervention, although they are known to be important elements in geriatric interventions.Citation18,Citation23 Further studies should investigate the effectiveness of a multidisciplinary approach in a multicomponent intervention addressing the ability to perform daily activities and other selected factors such as psychosocial, socioeconomic, nutritional, and medication.
Although the EAP-intervention was designed to address the patients’ performance of daily activities, the design of the study did not allow us to test its effectiveness on the patients’ performance of daily activities. This was due to the fact that the assessments of the patients’ performance of daily activities were one of the three components of the EAP-intervention. It would have been preferable to collect other measures on performance of daily activities for patients in both groups. However, this was not possible as solely register-based data were collected in the usual practice group. Measures on the performance of daily activities may have contributed with a deeper insight to whether the EAP-intervention resulted in enhancing the elderly patients’ performance of daily activities. A more comprehensive intervention, including task-specific training over a longer period, may potentially increase elderly patients’ performance of daily activities. Benefits from such interventions in elderly populations have been described broadly.Citation45–Citation48 A systematic review of home- and community-based occupational therapy from 2017 concluded that there is strong evidence that occupational therapy improves the ability to perform daily activities in elderly.Citation45
Participants in our study were comparable with participants in similar studies with regard to age and comorbidity, but may have differed in other factors such as socioeconomic status or home care received before admission.Citation15,Citation49 Age at 65 or above was an inclusion criterion in our study, which is in accordance with other studies aimed at reducing the risk of readmission in elderly patients.Citation19,Citation49 We did not select the participants due to their limitations in performing daily activities or other factors associated with the risk of readmission. If we had used a risk stratification instrument to screen and identify patients at high risk of readmission, it may have resulted in a different study population. Our results showed that 60% of patients in the intervention group had limitations in performing daily activities as identified with the performance-based assessment of performance of daily activities (component 1) and, thereby, the need for a rehabilitation plan and follow-up visits by an occupational therapist (components 2 and 3). If we had used a risk stratification instrument to select patients at high risk, we may have included a more homogenous population, which potentially could have benefitted from the EAP-intervention. Two systematic reviews highlight that studies using risk stratification instruments to identify high-risk patients most frequently show beneficial results.Citation14,Citation50 Further research is needed in order to examine if risk stratification before an occupational therapy discharge planning intervention would be beneficial in reducing the risk of readmission in elderly patients.
The exploratory analysis within the intervention group revealed that patients (60%) who were identified with decreased ability to perform daily activities in component 1 were at higher risk of readmission within 26 weeks than patients with no limitations in performing daily activities. This indicates that a large proportion of elderly patients discharged from short-stay units at EDs have limitations in performing daily activities and thereby need further rehabilitation.
Strength and limitations
Due to the quasi-experimental design, we were able to include nearly all patients meeting the inclusion criteria, thus providing a representative result. The intervention was performed during routine clinical practice and not in selected cases, which enhances the clinical relevance. Furthermore, an important strength of the study is the use of register-based data, which ensured a complete follow-up (100%) on all outcomes measured.
The study did have some limitations. First, the nonrandomized allocation may have led to unequal distribution of unmeasured factors, for example, socioeconomic factors or physical functioning between the two groups. Although the patients in the two groups were similar in terms of gender, marital status, and comorbidity, patients in the intervention group were older and admitted longer than patients in the usual practice group. In the statistical analyses, we used a multiple regression model to control for those differences in baseline characteristics. However, there may be several unidentified or unmeasured confounding factors that possibly could have influenced the outcome.
Given the available resources and experiences from a previous pilot study, a randomized trial was not a viable option.Citation29 In our previous pilot study, the randomization procedures were not feasible for the patients, which resulted in 67% of the patients refusing to participate. The quasi-experimental study design may be inferior to the randomized controlled trials on the study design hierarchy. However, the use of it may be beneficial in situations where randomization is not an option.Citation51
Allocation of patients to the usual practice group may have introduced selection bias, as some of the patients were included in daytime and others in afternoons and evenings. The within-group analysis of the usual practice group revealed differences in the group in relation to marital status and admission time. This was handled by adjusting for the influence of these two factors in the analyses, and the subanalysis did not alter the overall findings of the study. Referral to further rehabilitation in the municipality was planned to be carried out immediately after discharge from the hospital. However, it was not possible to get data on the actual services delivered from the municipality, and we do not know whether rehabilitation in primary care was carried out as planned. This may have affected the impact of the intervention on the risk of readmission, and the lack of data is considered a limitation of the study.
Due to the nature of the study, we were not able to blind patients or staff at the short-stay unit as to who received the intervention. In order to reduce the possibility of contamination, the occupational therapists delivering the EAP-intervention were not allowed to treat patients in the usual practice group. None of the patients in the usual practice group received follow-up visits after discharge, though some of them may have, by self-referral, received some kind of rehabilitation and/or home care after discharge.
Conclusion
The EAP-intervention showed no effectiveness in reducing the risk of readmission in elderly patients discharged from a short-stay unit at the ED. The results highlight the importance of assessing elderly patients’ ability to perform daily activities before discharge in order to determine the need for further rehabilitation. Although the intervention was not effective in reducing the risk of readmission, it revealed that 60% of patients in the intervention group had decreased ability to perform daily activities and there was a need for further rehabilitation after discharge. Further studies are needed to examine if a more intensive occupational therapy intervention with task-specific training over a longer period will increase elderly patients’ ability to perform daily activities and, thereby, reduce their risk of readmission after discharge from a short-stay unit at the ED.
Acknowledgments
We are grateful to the participants and their relatives, the occupational therapists, physiotherapist, doctors, and nurses at the participating short-stay unit, and to therapists from primary care/the municipality who actively participated in this project.
The work was supported by the Tryg Foundation (grant number 107632), the Foundation of Public Health in the Middle (grant number 1-30-72-141-12), and Aase and Ejnar Danielsen’s Foundation (grant number 10-001233). The foundations played no role in the design, execution, analysis, and interpretation of data, or writing of the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- McCabeJJKennellySPAcute care of older patients in the emergency department: strategies to improve patient outcomesOpen Access Emerg Med20157455427147890
- HastingsSNBarrettAWeinbergerMOlder patients’ understanding of emergency department discharge information and its relationship with adverse outcomesJ Patient Saf20117192521921863
- SamarasNChevalleyTSamarasDGoldGOlder patients in the emergency department: a reviewAnn Emerg Med20105626126920619500
- Danish Health and Medicine AuthorityEnhanced Efforts for the Elderly Medical Patient–Approach for a National Action PlanCopenhagenDanish Health and Medicine Authority2011
- XuKTNelsonBKBerkSThe changing profile of patients who used emergency department services in the United States: 1996 to 2005Ann Emerg Med200954805810 e1–7.19811852
- DeschodtMDevriendtESabbeMCharacteristics of older adults admitted to the emergency department (ED) and their risk factors for ED readmission based on comprehensive geriatric assessment: a prospective cohort studyBMC Geriatr2015155425928799
- GreysenSRStijacic CenzerIAuerbachADCovinskyKEFunctional impairment and hospital readmission in Medicare seniorsJAMA Intern Med201517555956525642907
- McCuskerJRobergeDVadeboncoeurAVerdonJSafety of discharge of seniors from the emergency department to the communityHealthc Q200912t2432
- CampbellSESeymourDGPrimroseWRACMEPLUS ProjectA systematic literature review of factors affecting outcome in older medical patients admitted to hospitalAge Ageing20043311011514960424
- MatzenLEJepsenDBRygJMasudTFunctional level at admission is a predictor of survival in older patients admitted to an acute geriatric unitBMC Geriatr2012123222731680
- KreversBNarvanenALObergBPatient evaluation of the care and rehabilitation process in geriatric hospital careDisabil Rehabil20022448249112097217
- SlatyerSToyeCPopescuAEarly re-presentation to hospital after discharge from an acute medical unit: perspectives of older patients, their family caregivers and health professionalsJ Clin Nurs20132244545523301580
- BachmannSFingerCHussAEggerMStuckAEClough-GorrKMInpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trialsBMJ2010340c171820406866
- KaramGRaddenZBerallLEChengCGruneirAEfficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic reviewGeriatr Gerontol Int2015151107111726171554
- CaplanGAWilliamsAJDalyBAbrahamKA randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–the DEED II studyJ Am Geriatr Soc2004521417142315341540
- MionLCPalmerRMMeldonSWCase finding and referral model for emergency department elders: a randomized clinical trialAnn Emerg Med200341576812514683
- NaylorMDBrootenDCampbellRComprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trialJAMA199928161362010029122
- RytterLJakobsenHNRonholtFComprehensive discharge follow-up in patients’ homes by GPs and district nurses of elderly patients. A randomized controlled trialScand J Prim Health Care20102814615320429738
- BuurmanBMParlevlietJLAlloreHGComprehensive geriatric assessment and transitional care in acutely hospitalized patients: the transitional care bridge randomized clinical trialJAMA Intern Med201617630230926882111
- ConroySPStevensTParkerSGGladmanJRA systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: ‘interface geriatrics’Age Ageing20114043644321616954
- LowthianJAMcGinnesRABrandCABarkerALCameronPADischarging older patients from the emergency department effectively: a systematic review and meta-analysisAge Ageing20154476177026265674
- Goncalves-BradleyDCLanninNAClemsonLMCameronIDShepperdSDischarge planning from hospitalCochrane Database Syst Rev2016271CD000313
- PedersenLHGregersenMBaratIDamsgaardEMEarly geriatric follow-up after discharge reduces readmission – a quasi-randomised controlled trialEur Geriatr Med20167443448
- CourtneyMEdwardsHChangAParkerAFinlaysonKHamiltonKFewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up programJ Am Geriatr Soc20095739540219245413
- ClemsonLLanninNAWalesKOccupational therapy predischarge home visits in acute hospital care: a randomized trialJ Am Geriatr Soc2016642019202627603152
- JonssonMAppelrosPFredrikssonCOlder people readmitted to hospital for acute medical care–implications for occupational therapyScand J Occup Ther20172414315027633187
- DarbyJWilliamsonTLoganPGladmanJComprehensive geriatric assessment on an acute medical unit: a qualitative study of older people’s and informal carer’s perspectives of the care and treatment receivedClin Rehabil20173112613426801585
- Eldredge BartholomewLKMarkhamCMRuiterRAFernándezMEKokGParcelGSPlanning Health Promotion Programs, an Intervention Mapping Approach4th edCA, USAJohn Wiley & sons inc2016
- NielsenLMMariboTKirkegaardHPetersenKSOestergaardLGDevelopment of a complex intervention aimed at reducing the risk of readmission of elderly patients discharged from the emergency department using the Intervention Mapping protocolBMC Health Serv Res In review
- FreibergerEde VreedePSchoeneDPerformance-based physical function in older community-dwelling persons: a systematic review of instrumentsAge Ageing20124171272122885845
- PodsiadloDRichardsonSThe timed “Up & Go”: a test of basic functional mobility for frail elderly personsJ Am Geriatr Soc1991391421481991946
- JonesCJRikliREBeamWCA 30-s chair-stand test as a measure of lower body strength in community-residing older adultsRes Q Exerc Sport19997011311910380242
- FisherAGBrayKAssessment of Motor And Process SkillsDevelopment, Standardization, and Administration Manual7th edColoradoFort Collins Three Star Press2010
- MerrittBKValidity of using the Assessment of Motor and Process Skills to determine the need for assistanceAm J Occup Ther20116564365022214108
- BischoffHAStahelinHBMonschAUIdentifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly womenAge Ageing20033231532012720619
- RikliREJonesCJDevelopment and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later yearsGerontologist20135325526722613940
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis1987403733833558716
- van DoornCBogardusSTWilliamsCSConcatoJTowleVRInouyeSKRisk adjustment for older hospitalized persons: a comparison of two methods of data collection for the Charlson indexJ Clin Epidemiol20015469470111438410
- QuanHLiBCourisCMUpdating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countriesAm J Epidemiol201117367668221330339
- ChanAWTetzlaffJMAltmanDGSPIRIT 2013 statement: defining standard protocol items for clinical trialsAnn Intern Med201315820020723295957
- SchulzKFAltmanDGMoherDCONSORT GroupCONSORT 2010 statement: updated guidelines for reporting parallel group randomised trialsPLoS Med20107e100025120352064
- GrawFGerdsTASchumacherMOn pseudo-values for regression analysis in competing risks modelsLifetime Data Anal20091524125519051013
- ParnerETRegression analysis of censored data using pseudo-observationsThe Stata Journal20103408
- World Medical AssociationWMA Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects Available from: http://www.wma.net/en/30publications/10policies/b3/index.htmlAccessed 03/27, 2017
- De ConinckLBekkeringGEBouckaertLDeclercqAGraffMJLAertgeertsBHome- and community-based occupational therapy improves functioning in frail older people: a systematic reviewJ Am Geriatr Soc2017651863186928369719
- De VriendtPPeersmanWFlorusAVerbekeMVan de VeldeDImproving health related quality of life and independence in community dwelling frail older adults through a client-centred and activity-oriented program. A pragmatic randomized controlled trialJ Nutr Health Aging201620354026728931
- NielsenTLPetersenKSNielsenCVStromJEhlersMMBjerrumMWhat are the short-term and long-term effects of occupation-focused and occupation-based occupational therapy in the home on older adults’ occupational performance? A systematic reviewScand J Occup Ther201621114
- OrellanoEColonWIArbesmanMEffect of occupation- and activity-based interventions on instrumental activities of daily living performance among community-dwelling older adults: a systematic reviewAm J Occup Ther20126629230022549594
- RostedEPoulsenIHendriksenCPetersenJWagnerLTesting a two step nursing intervention focused on decreasing rehospitalizations and nursing home admission post discharge from acute careGeriatr Nurs20133447748524041934
- GrafCEZekryDGiannelliSMichelJPChevalleyTEfficiency and applicability of comprehensive geriatric assessment in the emergency department: a systematic reviewAging Clin Exp Res20112324425420930499
- CraigPDieppePMacintyreSDeveloping and evaluating complex interventions: the new Medical Research Council guidanceBMJ2008337a165518824488