Abstract
Objective
To study the effectiveness of simply-performed balancing exercises in fall prevention.
Design
Pre- and post-trial.
Setting
University hospital from January 2009 to May 2010.
Participants
Elderly with falls in the previous year.
Intervention
Simple balancing exercise was performed at home every day and was recorded in the booklet.
Measurements
New falling events and a battery of balancing abilities including the Timed Up and Go Test (TUGT), chair stand, functional reach, and Berg balance scale-short form were evaluated at baseline, 3-, 6-, 9-, and 12-month periods. Fear of falling and quality of life scores were assessed at baseline and 12-month periods.
Results
146 subjects were recruited, 116 female (79.5%) with a mean age of 67.1 years. At the end of the study, 49% of participants had not fallen. All of the balancing abilities were compared between frequent and infrequent fallers and were significantly improved (P < 0.001) except for functional reach in the frequent fall group. Most subjects (72%–79%) complied well with the exercise program. However, compliance had no effect on balancing abilities. About 36.4% of participants had adverse events from exercise, of which knee pain was the top ranked. The quality of life and the fall efficacy scores increased significantly at the end of the study. Factors affecting falling were compliance with exercise (adjusted odds ratio [OR]: 2.55, 95% confidence intervals [CI]: 1.04, 6.30) and a history of falling ≥3 times in the previous year (adjusted OR: 3.76, 95% CI: 1.18, 11.98).
Conclusion
Performing simply-designed balancing exercises, at least 3 days per week, can increase balancing abilities, and decrease fall rates in the elderly with a history of previous falls. However, strategies to encourage elderly compliance may prevent falling.
Introduction
Falling is one of the most common problems in the elderly that can cause morbidity, including fracture and disability, and mortality. It may have negative effects on physical, psychological, and socioeconomic status. The incidence of falls in a population of community-dwelling older adults will increase with advancing age: DowntonCitation1 found that the incidence was 28%–35% in elderly aged more than 65 years, and 32%–42% in those aged more than 75 years. Elderly with a history of falls are at greater risk of falling again.Citation2 Approximately 30% of falls result in an injury that requires medical attention, and approximately 10% result in a fracture.Citation3 Fall prevention is an important strategy for reducing osteoporotic fractures. Hektoen et al estimated the cost-effectiveness of fall prevention, which can reduce health care costs for treating fall-related injuries, was 1.85 times higher than the cost of implementing a fall prevention program.Citation4
There is evidence that exercise can prevent falls.Citation5–Citation8 Exercise is beneficial even in those aged more than 80 years.Citation9 Petridou et al reported that exercise-alone interventions were about five times more effective in reducing recurrent falls among community-dwelling older people compared with multifactorial interventions.Citation10 Therefore, encouraging older adults to participate in exercise should be beneficial. Among multimodal exercises, a meta-analysis of the seven Frailty and Injuries: Cooperative Studies of Intervention Techniques (FICSIT) exercise trials suggests that balance exercise may be more effective in lowering falls risk than the other exercise components.Citation11
Models of exercise vary, including computerized feedback postural training programs; sophisticated exercise machines; and controlled group exercise in the hospital.Citation12,Citation13 However, older adults who are at risk usually refuse to participate in hospital-based exercise programs.Citation14 Home-based exercises may be appropriate for such a long term condition. Therefore, we aimed to study the effectiveness of simply-performed balancing training exercise, done at home, in reducing falls and improving balancing abilities in elderly patients who had already suffered from falls, and to follow up these effects for 1 year.
Methods
This study was conducted at Siriraj Hospital, Thailand, from January 2009 to May 2010. Following Siriraj Ethical Committee approval, we recruited elderly out-patients who had a history of falls in the previous 12 months. Our definition of fall was “an event that resulted in a person coming to rest unintentionally on the ground or other lower level, and which does not occur as a result of an intrinsic event or overwhelming hazard”.Citation15 The inclusion criteria were: elderly aged more than 50 years who fell; or those with a history of osteoporotic fracture in the previous year. Those who could not follow commands, or had a severe medical condition that prevented them from performing exercise, were excluded.
After participants signed the informed consent, demographic data including age, sex, underlying diseases, fall history, walking ability, turning, ability to go outside by oneself, and fear of fall history were recorded. Participants were evaluated for balancing abilities using a battery of tests including: Timed Up and Go test (TUGT)Citation16 (time taken to rise from a chair, walk a 3 m distance, turn around, walk back and sit down); chair standCitation17 (time taken to rise from a chair with arms folded and sit down, repeated five times); functional reachCitation18 (distance that participants can reach their arms forward as far as they can without losing balance); and Berg balance scale-short form (BBS-SF)Citation19 (score ranged from 0–28, high = good balance). The BBS-SF was composed of only seven items from the Berg balance scale (BBS).Citation20 It was proved to be psychometrically similar to the original BBS. All of the tests were conducted sequentially at baseline, and after 3 months, 6 months, 9 months, and 12 months in the exercise program. In addition, quality of life scores (SF-36)Citation21; a specific health questionnaire assessing physical functioning; psychological functioning; social functioning and vitality; and fall efficacy scale (FES),Citation22 a 14-activity questionnaire identifying early stages of fear of falling in active community-dwelling older people, were assessed both at baseline and after a 12-month period.
Participants were shown how to perform easy balancing exercises. They practiced the exercises until they could perform them correctly. All received brochures and a DVD reminding them how to exercise daily at home. The exercises included: strengthening exercise, emphasizing hip abductors and extensors; closed kinetic chain quadriceps exercise; marching; stepping over a bench; standing up from a chair with arms folded; and tandem walk (walking heel-to-toe in a straight line). They were asked to perform seven balance exercises, 10–20 repetitions for each, which took about 15–20 minutes per day, record the frequency of exercise or compliance in their diaries and bring these records to the researchers every visit. Participants who exercised less than 3 days per week were classified as having poor compliance, while good compliance was defined as performing exercise at least 3 days per week. In addition, the relationship between compliance with exercise and balancing abilities were analyzed. According to the classification of exercise compliance at 1-year follow up, subjects who were categorized in the good compliance group had to report good compliance at every visit; otherwise, they were classified in the poor compliance group. Moreover, new falls during the study period were also recorded prospectively in their diaries. The factors related to falls were also analyzed.
Statistical analysis
Demographic data was presented by descriptive statistics. A Chi-square test was applied to compare fall frequencies between the baseline and 1-year period by per-protocol and intention-to-treat analysis methods. Balancing abilities, quality of life scores (SF-36), and FES at baseline and 1 year after were compared by paired t-test. Factors associated with falls were analyzed using a Chi-square test or Fisher’s exact test for qualitative data. Multiple logistic regression was used to analyze the confounding factors. A P-value of ≤0.05 was considered statistically significant. Analyses were performed using PASW statistic 18 (SPSS Inc, Chicago, IL).
Results
One hundred and forty-six elderly subjects were recruited via an advertising board in our hospital. We compared the retained and drop-out subjects by age, sex and frequency of previous fall and fracture, and found that there were no significant differences except age (66.5 ± 8.0 and 70.0 ± 9.2 years in retained and drop-out groups respectively). There were 28 subjects (19.2%) lost to follow-up due to inability to contact (8, 5.5%), unavailability (9, 6.2%), being withdrawn from the study (8, 5.5%), and only three (2.0%) had serious medical problems (stroke, craniotomy and myocardial infarction). The craniotomy was due to a fall and the event occurred within the first month after recruitment. The patient had fallen four times in the previous year. No one died or suffered hip fractures in our study. Only 104 (71.2%) could be completely followed up through 1 year.
shows the demographic data of the 146 subjects. Most of the subjects were female (116, 79.5%) with a mean age of 67.1 years. The average BMI was 25.2 ± 4.4 kg/m2. About half of them were married. The three most frequent underlying diseases were dyslipidemia (47.9%), hypertension (47.3%), and diabetes mellitus (15.8%). Thirteen percent of subjects had a history of fracture due to falls. Almost all of them could walk independently (86.8%) and were able to go outside by themselves (90.4%). The number of subjects who used more than four medications was 44 (34.1%). Three-quarters (75.3%) reported fear of falling, 59.6% had swaying on turning, and 33.6% had difficulty on turning.
Table 1 Demographic data of 146 participants
presents the number of falls in the test group at the baseline and at 1 year, compared between per-protocol (PP) and intention-to-treat (ITT) analysis methods. At baseline, all subjects had a history of at least one previous fall. At the end of the study, 51 (49%) participants had not fallen during the study period. The number of patients who fell was decreased at the 12-month period. At baseline, 69 subjects (47.3%) had fallen once and 77 subjects (52.7%) had fallen twice or more. During the 12-month study period, 24 patients (23.1%) fell once and 29 patients (27.9%) fell twice or more. After using ITT analysis, we hypothesized that all the subjects who were lost to the study fell at least once and the frequency of falls was summated during the whole year period. The results from ITT were related to the PP method (P < 0.001) as presented in .
Table 2 The number (%) and 95% confidence interval of subjects who fell at baseline and 12-month after recruitment (cumulative frequency), analyzed by per protocol (PP) and intention-to-treat (ITT) methods
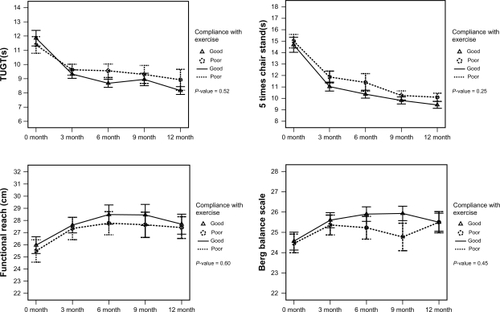
Balancing abilities including TUGT, chair stand, functional reach and Berg balance scale-short form, at baseline and 1-year follow up period, for both frequent and infrequent falls groups are shown in . They were significantly improved except for functional reach in the frequent fall group. The mean difference between infrequent and frequent falls at 12-month was not statistically significant between groups (using regression analysis). Compliance was good (72%–79%) with most subjects (). According to , compliance has no effect on balancing abilities.
Table 3 Mean (SD) of the balancing abilities at baseline and 12-month follow up period compared between infrequent fall and frequent fall groups (N = 118)
Table 4 Compliance with exercise during 3-month, 6-month, 9-month and 12-month follow up period
Figure 1 Balancing abilities including timed up and go test, chair stand, functional reach, and Berg balance scale based on compliance with exercise.
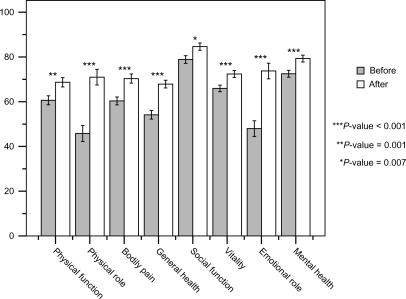
At the end of the study, the quality of life score increased significantly in 8 domains (). The fall efficacy score (FES) also increased significantly (116.6 ± 26.4 versus 121.7 ± 23.1 at baseline and 12-month respectively). Regarding the adverse events (AE) of exercise, 48 out of 132 participants (36.4%) had an AE, of which knee pain was the top ranked (20, 15.2%), followed by calf pain and hip pain (6, 4.5% and 5, 3.8%, respectively).
Figure 2 Quality of life score (SF-36) of 104 participants compared between baseline and 1-year after.
The factors affecting frequency of fall including age, sex, underlying diseases, fear of falling, history of falls, compliance with exercise, medication use, difficulty on turning, swaying on turning, ability to walk, and ability to go outside were analyzed. However, only compliance with the exercise program (adjusted odds ratio [OR]: 2.55, 95% confidence interval [CI]: 1.04, 6.30) and a history of fall ≥ three times in the previous year (adjusted OR: 3.76, 95% CI: 1.18, 11.98) were related to falls ().
Table 5 Crude odds and adjusted odds of the factors relating to fall frequency (N = 104)
Discussion
Our study showed that simply-designed balancing exercises used by the elderly who have a history of frequent falls can decrease fall rate, and significantly increase balancing abilities including TUGT, chair stand, functional reach and Berg balance scores. The improved outcomes may be due to the encouragement of the elderly to be aware of falls and to perform regular exercise at home. However, all the balancing abilities were secondary outcomes. Our primary outcome, number of falls, was significantly reduced after intervention.
There are many systematic reviews concerning fall prevention in the elderly.Citation23–Citation26 An analysis by Gillespie et al of 55,303 participants revealed that multiple-component group exercise could reduce the rate of falls in older people living in the community (rate ratio: 0.78, 95% CI: 0.71–0.86).Citation8 Another review also confirmed that balancing exercises can reduce the rate of falling (rate ratio: 0.83, 95% CI: 0.75–0.91).Citation27 It is beneficial even in those older than 80 years.Citation9,Citation28 However, the type of exercise that the elderly could accept and comply well with was still questionable. Therefore, we designed a simple balancing exercise that was easily done at home, with less adverse events, and which was appropriate for the elderly.
There are many factors relating to falls including age, muscle power, impaired balance, use of psychoactive drugs, poor vision and degenerative joint disease.Citation3, Citation29 Our study revealed that one of the factors affecting fall rate was a history of previous falls. This was in accordance with other studies which reported that patients with a history of falls during the previous year showed an increased risk of falls.Citation30–Citation32 Those who had repeated falls will have an increased risk of trauma and fracture as well. Therefore, strategies to prevent falls, including reviewing medications, correction of environment, improvement of strength, and regular balance training, should be encouraged in the elderly.
Compliance is another factor affecting fall rate in our study. Most subjects performed exercise regularly at least 3 days per week. However, we could not demonstrate that compliance had any effect on balancing abilities. The reasons may be because 1) the number of subjects in each group was insufficient (60 in good compliance and 44 in poor compliance groups) to demonstrate significant changes in each groups’ balancing abilities, 2) most of our participants were “young-old” (mean age was 67.1 ± 8.4 years, and 88 patients (60.3%) were less than 70 years), so their balance would be better than in participants in other studies where the mean age was higher, 3) difficulty experienced by elderly patients in recording the frequency of exercise, 4) these balancing abilities may not be sensitive enough to represent true balance, 5) the final classification group of compliance with exercise may be our limitation because to be classified in the good compliance group, subjects had to perform well at every visit; otherwise, they were classified in the poor compliance group. However, encouraging the elderly to participate in exercise regularly should be emphasized because this method was an effective strategy. Moreover, prevention of falls using exercise is cost-efficient, so it can be implemented in countries with fewer resources.Citation10
This simply-designed exercise also affects quality of life (QoL) in both physical and mental health dimensions. The results in this study showed the benefits of balancing exercise in decreased fall rates, and increased QoL. Our study was in line to that of Lin et al,Citation33 who reported that QoL scores in an exercise group of elderly with recent falls was greater than in those in an education group or a home safety assessment and modification group. Therefore, we can conclude that exercise improves both balance and quality of life. Encouraging the elderly to exercise regularly is an effective way to prevent falls, and should be emphasized in medical practices.
There are some limitations in our study. 1) We had no control group. We only compared pre- and post-intervention in the frequent faller group, so our results were not suitable for a randomized controlled trial (RCT) design. We did not recruit non-fallers because our objective was to study the efficacy of simple balance exercise in frequent fallers. 2) The number of participants who could be completely followed up was only 104 from 146 (71.2%). In addition, the 28 subjects who were lost to follow up were older than the retained subjects. This may be due to the need to make multiple visits to the clinic during the study period. 3) The record of compliance of exercise in elderly patients is rather difficult to validate.
Conclusion
A simply-designed balancing exercise program, performed at least 3 days per week, can increase balancing abilities, and decrease fall rates in the elderly with previous falls. However, strategies to encourage elderly compliance may prevent falling.
Acknowledgements
This study was supported by a grant from The National Research Council of Thailand. We would like to thank Ms P Lymampai, Mrs A Leurcharusmee, Mrs K Sungkarak, and Mrs S Salika for their cooperation.
Disclosure
The authors report no conflicts of interest in this work.
References
- DowntonJHFallsTallisRFillitHBrocklehurstJCGeriatric Medicine and Gerontology5th edEdinburgh, ScotlandChurchill Livingstone199813591370
- FormigaFNavarroMDuasoEFactors associated with hip fracture-related falls among patients with a history of recurrent fallingBone20084394194418656561
- BerrySDMillerRRFalls: epidemiology, pathophysiology, and relationship to fractureCurr Osteoporos Rep2008614915419032925
- HektoenLFAasELuråsHCost-effectiveness in fall prevention for older womenScand J Public Health20093758458919666674
- KannusPUusi-RasiKPalvanenMParkkariJNon-pharmacological means to prevent fractures among older adultsAnn Med20053730331016019730
- BakerMKAtlantisEFiatarone SinghMAMulti-modal exercise programs for older adultsAge Ageing20073637538117537741
- SkeltonDABeyerNExercise and injury prevention in older peopleScand J Med Sci Sports200313778512535321
- GillespieLDRobertsonMCGillespieWJInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20092CD00714619370674
- DavisJCRobertsonMCAsheMCLiu-AmbroseTKhanKMMarraCADoes a home based strength and balance programme in people aged ≥80 years provide the best value for money to prevent falls? A systematic review of economic analyses of falls prevention interventionsBr J Sports Med201044808920154094
- PetridouETMantiEGNtinapogiasAGNegriESzczerbinskaKWhat works better for community-dwelling older people at risk to fall?: a meta-analysis of multifactorial versus physical exercise-alone interventionsJ Aging Health20092171372919494361
- ProvinceMAHadleyECHornbrookMCThe effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FIC-SIT Trials. Frailty and Injuries: Cooperative Studies of Intervention TechniquesJAMA1995273134113477715058
- LajoieYEffect of computerized feedback postural training on posture and attentional demands in older adultsAging Clin Exp Res20041636336815636461
- JudgeJOLindseyCUnderwoodMWinsemiusDBalance improvements in older women: effects of exercise trainingPhys Ther1993732542628456144
- BarrRMacdonaldHStewartAAssociation between vitamin D receptor gene polymorphisms, falls, balance and muscle power: results from two independent studies (APOSS and OPUS)Osteoporos Int20102145746619629616
- ClarkRDLordSRWebsterIWClinical parameters associated with falls in an elderly populationGerontology1993391171238514201
- PodsiadloDRichardsonSThe timed “Up and Go”: a test of basic functional mobility for frail elderly personsJ Am Geriatr Soc1991391421481991946
- GuralnikJMSimonsickEMFerrucciLA short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admissionJ Gerontol199449M85M948126356
- DuncanPWWeinerDKChandlerJStudenskiSFunctional reach: a new clinical measure of balanceJ Gerontol199045M192M1972229941
- ChouCYChienCWHsuehIPDeveloping a short form of the Berg Balance Scale for people with strokePhys Ther20068619520416445333
- BergKWood-DauphineeSWilliamsJIGaytonDMeasuring balance in the elderly: preliminary development of an instrumentPhysiother Can198941304311
- KongsakonRSilpakitCThai version of the medical outcome study 36 items short form health survey: an instrument for measuring clinical results in mental disorder patientsRama Med J200023819
- HillKDSchwarzJAKalogeropoulosAJGibsonSJFear of falling revisitedArch Phys Med Rehabil199677102510298857881
- GillespieLDGillespieWJCummingRLambSERoweBHInterventions for preventing falls in the elderlyCochrane Database Syst Rev20002CD00034010796348
- GillespieLDGillespieWJRobertsonMCLambSECummingRGRoweBHInterventions for preventing falls in elderly peopleCochrane Database Syst Rev20013CD00034011686957
- GillespieLDGillespieWJRobertsonMCLambSECummingRGRoweBHInterventions for preventing falls in elderly peopleCochrane Database Syst Rev20034CD00034014583918
- HoweTERochesterLJacksonABanksPMBlairVAExercise for improving balance in older peopleCochrane Database Syst Rev20074CD00496317943831
- SherringtonCWhitneyJCLordSRHerbertRDCummingRGCloseJCEffective exercise for the prevention of falls: a systematic review and meta-analysisJ Am Geriatr Soc2008562234224319093923
- RobertsonMCCampbellAJGardnerMMDevlinNPreventing injuries in older people by preventing falls: a meta-analysis of individual-level dataJ Am Geriatr Soc20025090591112028179
- JungYMShinDSChungKSLeeSEHealth status and fall-related factors among older Korean women: implications for nursesJ Gerontol Nurs200733122017955734
- NevittMCCummingsSRKiddSBlackDRisk factors for recurrent nonsyncopal falls. A prospective studyJAMA1989261266326682709546
- Clough-GorrKMErpenTGillmannGPreclinical disability as a risk factor for falls in community-dwelling older adultsJ Gerontol A Biol Sci Med Sci20086331432018375881
- StalenhoefPADiederiksJPKnottnerusJAKesterADCrebolderHFA risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort studyJ Clin Epidemiol2002551088109412507672
- LinMRWolfSLHwangHFGongSYChenCYA randomized, controlled trial of fall prevention programs and quality of life in older fallersJ Am Geriatr Soc20075549950617397426