Abstract
Objective
This study aimed at investigating the effectiveness of a robotic fall prevention program on knowledge, exercises, balance, and incidence of falls among elderly in senior housings.
Patients and methods
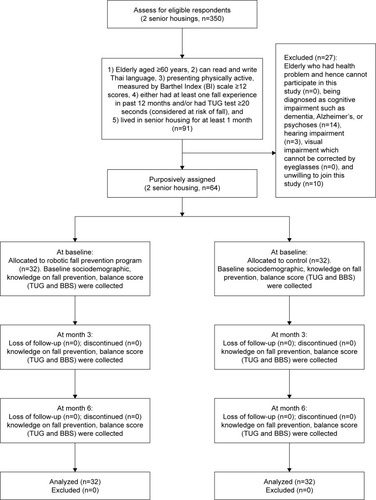
This is a quasi-experimental study. Sixty-four elderly in two senior housings in Bangkok with Barthel Index scale ≥12, who had either at least one fall experience in the past 12 months and/or had Timed Up and Go (TUG) test ≥20 seconds were recruited and purposively assigned to the intervention group (received a small robot-installed fall prevention software, personal coaching, and handbook, n=32) and control group (received only handbook, n=32). Outcomes were knowledge score evaluated by structured questionnaire through face-to-face interviews, number of exercises measured by self-recorded diary, and balance score assessed by TUG and Berg Balance Scale (BBS). The incidence of falls was assessed by face-to-face interviews. Both groups were assessed at baseline, 3rd, and 6th month after the intervention.
Results
There was a statistically significant improvement in knowledge mean score at 6th month in both the groups. However, the intervention group showed faster increase in knowledge mean score than the control group at 3rd month (P<0.01). The intervention group showed a statistically significant higher number of exercises than the control group at 3rd and 6th month (P<0.05). There was no statistically significant difference on TUG and BBS mean scores between the two groups at baseline, 3rd, and 6th month. However, the intervention group showed a statistically significant improvement in TUG and BBS at 6th month post-intervention (P<0.01). There was one fall reported in the control group.
Conclusion
The robotic fall prevention program increased knowledge on fall prevention and promoted exercises and balance among elderly in senior housings.
Introduction
Falls among elderly are a major health issue worldwide. One-third of elderly aged >65 years experienced fall each year. Prevalence of fall in elderly varies among settings. There is a higher prevalence of fall among elderly living in a long-term care institution than those who are living in a community.Citation1–Citation3 A previous study found that the prevalence of fall among elderly nursing home residents was ranged between 50% and 66%, while among hospitalized patients it was found to be at 50%.Citation4 In Thailand, in 2014, the prevalence of fall among elderly community-dwellers was 16.9%.Citation5
Fall is the second leading cause of unintentional injury death, after road traffic injuries.Citation6 An elderly who had experienced a fall tend to have 2–3 recurrences of falls.Citation7 Falling in elderly is risky. Just one time of falling in the elderly can affect the health status and daily living activities, or can even be bedridden. Approximately one-third of falls leads to injury severity levels ranging from light to heavy. Falling is one of the major causes of admission in hospitals among elderly aged ≥65 years. Elderly who have hip fracture from falling may have to stay at a hospital for over 20 days. The more comorbidity or higher aged the elderly is, the more hospital stay time.Citation8
Few of the direct costs of fall are medication treatment, pharmacy, and cost of transportation to health centers. The average health system cost per one fall injury for elderly aged ≥65 years has significantly increased.Citation9,Citation10 Indirect costs involve loss of man day work for a family member taking care of the elderly who fell. A previous study found the average lost earnings of 40,000 USD per year in the UK.Citation11
Falls exponentially increase with age-related biological changes. The fall incidents increased twofold in elderly aged >75 years.Citation12 Falling among elderly is going to be more challenging in the future. With a fast growing aging population worldwide, the number of elderly aged >60 years is growing faster than other age groups. Moreover, the oldest group of the population, aged ≥80 years, is the fastest growing group and expected to be 20% of the overall elderly population in 2050.Citation4
Many fall prevention guidelines from WHO,Citation4 Centers of Disease Control and Prevention (CDC),Citation13 and Ministry of Public Health of ThailandCitation8,Citation14 indicate that the risk factors of fall are usually classified as intrinsic and extrinsic risk factors. Intrinsic risk factors of fall include a history of fall, walking and balance problems, less muscle strength, visual impairment, incontinent, receiving many medications, cognitive problems. Extrinsic risk factors are referred to environmental hazards such as a wet floor, slippery and uneven ground surface, inadequate lighting, and inappropriate clothing.
Fall can be prevented.Citation13 A systematic review of fall prevention interventions among elderly dwelling in the community indicates that home-based exercise program, home modification, reducing medications, and intervention of visual problem solving were effective interventions to prevent falls.Citation15
The Otago Exercise Program (OEP) is a recommended home-based exercise program for elderly in the community.Citation16,Citation17 It is an evidence-based fall prevention program which resulted from four separate control trials among 1,016 elderly in New Zealand. OEP was effective in reducing 35% in both the number of falls and the number of injuries resulting from falls.Citation16 The program is delivered by a physiotherapist or trained instructor with six home exercise visits, four telephone follow-ups, and monthly monitoring of the completed exercises and any fall incident over a 1-year period. Main features of the program compose of five leg muscle strengthening exercises and 12 balance retaining exercises, up to four levels of difficulty. The participants should exercise for ~30 minutes at least three times a week, and includes a walking plan for the rest day. Each participant receives a booklet with illustration and instructions for the exercises, one or more ankle cuff weights, calendar or diary to record their exercise or any falls.Citation16 In Thailand, a fall prevention guideline (2012)Citation8 has also recommended exercise for fall prevention which is modified from OEP for elderly in the community.
Many technology-based interventions are also developed for fall prevention. A 2016 systematic reviewCitation18 indicates that the wearable sensor and camera-based and floor sensors are installed in the living environment, which feed information back to the software monitoring the user’s interactions with that environment.
Among wearable sensors for monitoring falls during static and dynamic tasks in healthy elderly,Citation19 accelerometers and gyroscopes are widely used for fall risk assessment, fall prevention, and fall detection because they are low cost and sends reliable informative signals to the software. The most used body segment for positioning the sensors is the trunk.
There are limitations that wearable sensors are still in an experimental phase and the effect has not been conclusively validated.Citation19 Camera-based and floor sensors have a limited range within the monitored environment. Preserving privacy of elderly is also a challenge for camera-based technology.Citation18
Robotic technology has been developed for medicine and home care. Recently, Japan developed a Human Support Robot (HSR), operated remotely by patients themselves or by family and caregivers. The HSR can pick up objects off the floor and bring things down from the shelves. The nursing care robot lifts the elderly from bed into a wheelchair, or assist them to stand up.Citation20 In Europe, a robot is synced with a smart home technology such as environmental sensors, which is installed in the house feeding information about the occupant’s movements, alerting off-site caregivers in the event of a fall, and also provide physiological sensors to track health such as blood pressure.Citation20 While in Thailand, Dinsow Mini® robot is developed for a home user. It provides entertainment function such as listening to music or watching a video. The robot is synchronized with the mobile application, so the users or caregivers could operate the robot from their own smartphone such as updating information, songs, and photos, and/or making a video call.Citation21
However, the robotic technology, which focuses on behavioral change intervention specifically for fall prevention in Thailand is rare. This study aimed at investigating the effectiveness of robotic fall prevention program on knowledge score of fall prevention, number of exercises, balance score, and incidence of falls among elderly at risk of fall residing in senior housings in Bangkok, Thailand.
Patients and methods
Sample size, study design, and procedure
The sample size was calculated with two-tailed statistical hypothesis with effect size at 0.76,Citation22 α-error of probability at 0.05, and a power of 0.80. We used G-Power statistical analysis program version 3.1.9.2 to calculate the sample size of participants. The required number of sample size was 29 for each group, and 10% of participants were added to compensate for withdrawing or loss to follow-up during the intervention. Hence, the final number was 32 participants in each group (N=64).
To ensure the similarity of the living environment of participants between the intervention and control groups, the two senior housings were purposively sampled from the governmental bodies: Sawangkanivej and Ban Bang Khae. The facilities were designed for the convenience of the elderly such as wide doors for wheelchair, slop with handle, gym room, meeting room, yard, and garden. There are a routine nurse and physical therapist available at the health room at some specific time. The intervention and control groups were selected from different housings to ensure that there was no contamination of intervention between groups. There is 43.8 km distance between the two senior housings.
The fall risk screening conducted on all 350 residents in the two senior housings, followed the guideline from CDC.Citation23 Elderly who said “yes” to any of the following questions: 1) fall experienced in the past 12 months, 2) feel unsteady when standing or walking, and 3) worries about falling, was evaluated fall risk by Timed Up and Go (TUG) test.
To be an eligible participant, an elderly had to pass the following inclusion criteria: 1) aged ≥60 years, 2) can read and write Thai language, 3) presently physically active, measured by Barthel Index (BI) scale ≥12 score,Citation24 4) considered at risk of fall by either a previous fall experienced in past 12 months and/or had TUG test ≥20 seconds,Citation14,Citation23 and 5) lived in senior housing for at least 1 month. Among the total residents, 91 elderly were eligible to be subjects. Exclusion criteria of this study were elderly who had health problem that could not participate in this study, being diagnosed with cognitive impairment such as dementia, Alzheimer, or psychoses, hearing impairment, visual impairment which cannot be corrected by eyeglasses, and unwilling to join this study. Finally, 64 elderly were recruited in this study. Thirty-two participants residing in Sawangkanivej were purposively assigned to the intervention group and another 32 participants residing in Ban Bang Kae were purposively assigned to the control group ().
Intervention in this study was a robotic fall prevention program, which composed of a small robot-installed fall prevention software together with personal coaching and a fall prevention handbook. The robot, Dinsow Mini® version M2070 was used in this study with 35 cm in height, 24 cm in length, 18 cm in width, and weighed 3.13 kg. (). The 8″ touchscreen was installed at the head section of the robot. The elderly can watch a video on this screen. Same as any other electric appliance, the robot needed to be plugged in.
Figure 2 Dinsow Mini® robot.Citation21
In this study, we developed a fall prevention software from social cognitive theory (SCT),Citation25 consumer information processing (CIP) model,Citation26 and literature reviews.Citation8,Citation14,Citation15 Many meetings were conducted between main research investigator, one physiotherapist, three elderly caregivers, and two software engineers to understand the need of the user and its feasibility in the software design. A preliminary survey was conducted in the two housings. Since Thai elderly (born before 1957) were not familiar with using new technologies, personal coaching was added into this program. Moreover, any equipment that relied on internet connectivity was not practically used among Thai elderly. Thus, many educational materials were embedded in the software that could be accessed without an internet connection.
Finally, the fall prevention software was provided with four videos on fall prevention and choosing appropriate walking assistive devices, two videos demonstrating how to make sandbag and choose an appropriate shoe, two videos on exercises, and 28 daily voice messages on fall prevention and daily exercise reminders.
SCT was used to develop a conceptual framework of this study in which fall prevention could occur in a social context with a dynamic and reciprocal interaction of the person, environment, and behavior. According to SCT, a person is able to perform a behavior through essential knowledge and skill. Thus, fall education was needed to implement this study. The participants learned fall prevention and exercises from video demonstrations displayed on the screen of the robot and a handbook with illustrations and instructions.
Two exercise videos including light and advanced exercise levels were chosen from Ministry of Public Health of Thailand.Citation27,Citation28 The contents of exercises in these two videos were modified from the OEP, which proved effective in reducing the number of falls and number of injuries resulting from falls.Citation16,Citation29
Light exerciseCitation27 required some equipment to hold for support such as a bar or a stable table. The advanced exerciseCitation28 performed activities such as walking and turning around without support. Each participant was evaluated for balance by these following questions:Citation8 1) can you perform activities of daily living (ADL) independently? 2) can you sit and stand independently? and 3) can you perform heel-to-toe standing? Elderly who said “no” to any of these questions was assigned to light level exercise. While elderly who said “yes” to all questions were assigned to advanced level exercise. Not only safety during exercise was considered, but also self-efficacy was promoted. The elderly had confidence to perform exercises successfully.
CIP was used to develop chunks of educational materials. Daily voice messages composed of 28 messages on fall prevention, which automatically notified daily at 8.00 PM, starting from the first message at day 1 to complete 28th message at day 28. Four videos on fall prevention education and choosing appropriate walking assistive devices were chosen from educational institutions.Citation30–Citation33 Two videos demonstrating how to make sandbag for exercise, and choosing appropriate shoe were filmed by paramedic principle investigator.Citation34,Citation35 Moreover, exercise reminder was developed and automatically notified at 8.00 AM.
Implementation of the intervention
We sent permission letters from Chulalongkorn University to the two senior housings. Then, invitation posters were pinned on the central board at the clubhouse and the office of the two senior housings, and staffs announced our project to their residents. Any resident who was interested in fall risk screening could join activities including a short interview and TUG test, ~5 minutes for each person. The elderly participants who met our inclusion criteria were invited to participate in this study.
The participants in the intervention group were scheduled date and time for setting the robots in their room for ~40–60 minutes. Principle investigator demonstrated how to use the robot, observed participants actually using it, and provided personalized feedback. Each participant received a robot-installed fall prevention software together with a handbook and personal coaching.
Personal coaching was conducted in the intervention group for ~1 hour, at the baseline, 2nd, and 3rd month to make sure the participants could use the robot and perform exercises independently. Video education was discussed in the coaching session. In addition, principle investigator assisted the participants, who required some help, anytime during the 6-month study period. If a problem regarding using robot emerged, the principal investigator demonstrated using robot again until participants can use the robot independently. If a problem arises regarding the robot being broken or malfunction, the principal investigator replaced it with a new robot.
There was neither robot nor coaching in the control group. Participants in the control group received a fall prevention handbook with exactly the same content as the intervention group, and engaged in their daily routine activities such as walking and doing housework.
Baseline data on sociodemographic, comorbidities, fall experienced, and knowledge on fall prevention were obtained through face-to-face interviews using questionnaires. Balance scores were evaluated by the ability to perform task-oriented tests including TUG and Berg Balance Scale (BBS). Each participant, in both intervention and control groups, was advised appropriate exercise according to his/ her physical condition. All participants were taught how to self-record their exercise on the given exercise diary.
Knowledge on fall prevention and balance scores were assessed again at 3rd and 6th month after intervention. Principle investigator gave feedback of knowledge scores and balance scores to both intervention and control groups. Any questions regarding the program were discussed. The number of exercises was assessed at 3rd and 6th month from the self-recorded exercise diary. All participants were free to contact principle investigator any time throughout the 6-month study period.
All participants were interviewed face-to-face for the new fall event(s) during the study period at 3rd and 6th month after the intervention was implemented. The principle investigator rechecked incidence of falls by interviewing in-house nurse, caregiver, or staff of the two senior housings. All coaching and data collections were conducted by the main research investigator.
This study was conducted in accordance with the Declaration of Helsinki, approved by the Ethics Review Committee for Research Involving Human Research Subjects, Health Sciences Group, Chulalongkorn University (COA No 201/2560).
Measurements
Sociodemographic questionnaire
The sociodemographic questionnaire was used to interview baseline characteristic of participants and incidence of falls during the intervention period. It has four parts as follows: 1) demographic: sex, age, marital status, education, income, and source of income;Citation36 2) health: comorbidity, medication, eyesight problem, eyeglasses/contact lens utilization, and physical activities;Citation8,Citation14,Citation36 3) environment: walking assistive devices and environmental hazards;Citation8,Citation14,Citation36,Citation37 and 4) experience of fall in the past 12 months prior to this study and new fall incident during the 6-month study period.
BI scale of ADL – Thai version
BI of ADL – Thai version was used to determine the level of physical activitiesCitation24 with an excellent correlation with the Dynamic Gait Index (r=0.067) among the elderly population,Citation38 high inter-rater reliability between therapists,Citation39 and the inter-class correlation was 0.87.Citation24 The BI is composed of ten items including 1) feeding, 2) grooming, 3) transfer, 4) toilet use, 5) mobility, 6) dressing, 7) stairs, 8) bathing, 9) bowels, and 10) bladder. The score is ranged from 1 to 20. The interpretation of the Thai version of BI scale was made according to cutoff of points:Citation24 0–4 scores, dependent or bedridden; 5–11 scores, partial dependent; and ≥12 scores, independent or active elderly.
TUG
TUG is widely used for fall risk screening with sensitivity at 73.7% and specificity at 65.8%.Citation40 It has good validity,Citation41 and is reliable, valid, and easy-to-administer for assessing balance,Citation42 and is also recommended for fall risk screening in elderly by Ministry of Public Health of Thailand.Citation43 First, the elderly were asked to sit comfortably on a straight-backed chair with both feet placed on the ground. Placing an object at 3 m in front of the chair, the elderly were instructed to rise from the chair, without trying to put hands for support, and walk straight, turn around over the placed object, walk back to the chair, and sit down on the chair. The elderly should walk as fast as they can. The examiner starts the stop watch from the time of asking the elderly to rise up until the elderly walked back and sat down. A cutoff of point ≥20 seconds is considered as having the risk of fall for Thai elderly.Citation14
BBS
BBS is widely used for assessing balance. It can also be used for patients with neuromuscular disease and lower-limb amputation.Citation44 In Thailand, Ministry of Public Health recommends BBS for fall risk assessment in the elderly.Citation43 The sensitivity in predicting fall was 0.72, specificity was 0.73, and accuracy was 0.84.Citation45 It is 14 task-oriented screening test including 1) sitting to standing, 2) standing unsupported, 3) sitting with back unsupported but feet supported on the floor or on a stool, 4) standing to sitting, 5) transfers, 6) standing unsupported with eyes closed, 7) standing unsupported with feet together, 8) reaching forward with outstretched arms while standing, 9) pick up object from the floor from a standing position, 10) turning to look behind over left and right shoulders while standing, 11) turn 360 degrees, 12) placing alternative foot on step or stool while standing unsupported, 13) standing unsupported one foot in front, and 14) standing on one leg. The item-level is ranged from 0 to 4, depending on the ability to perform the tasks. The score is ranged from 0 to 56.
Knowledge on fall prevention
The fall prevention questionnaire was developed from literature reviewCitation14 and tested on a pilot group. The Cronbach’s alpha coefficient was 0.77. It is composed of 31 items, and was rated 0 or 1 score. The total score ranged from 0 to 31. Interpretation was based on a mean score: <mean and ≥ mean.
Number of exercises
All participants were given a blank calendar template, considered as an exercise diary, which has be ticked on the day that they do exercise based on the given video and/or handbook guideline. The exercise diary was assessed by self-report and collected at 3rd and 6th month after the intervention was performed.
Statistical analysis
The data were analyzed by using SPSS (for Windows) version 20. Descriptive statistics were used to describe the sociodemographic of participants. Categorical data were presented in frequency and percentage. Numerical data were presented in frequency, percentage, mean, and SD. Chi-squared test was used for baseline comparison. Independent t-test was used to determine the statistically significant difference in knowledge score, number of exercises, TUG, BBS, and incidents of fall between intervention and control groups at baseline, 3rd, and 6th month after the intervention was implemented. Repeated measures ANOVA was performed to determine statistically significant difference in knowledge score, TUG, and BBS at baseline, 3rd, and 6th month within the groups. Bonferroni post hoc analysis was performed for pairwise comparisons in each group. Paired t-test was used to determine statistically significant difference on number of exercises at 3rd month compared to 6th month within the group. A P-value of <0.05 was considered as statistically significant in this study.
Result
Sociodemographic and health characteristics
The data on sociodemographic and health characteristics of participants are presented in . Majority of participants (79.7%) were female, 54.7% were aged 60–75 years, 54.7% had secondary and university education background, and 85.9% had enough income. More than half of the participants (51.6%) had ≥3 comorbidities. Most of the participants (79.7%) had medication risk using ≥4 medications: seizure, antihypertensives, sedative, and hypnotic. Moreover, 84.4% of participants had eyesight problem. Mean score and SD of TUG was 20.7±7.7; BBS score was 45.3±10.6; and knowledge score was 25.8±4.5. Most of the participants (70.3%) had physical activities for >30 minutes ≥3 times/week, and 70.3% had at least one fall experience in the past 12 months prior to this study. There was no statistically significant difference in baseline characteristics among the intervention and the control groups ().
Table 1 Baseline comparison on sociodemographic characteristics of participants (n=64)
Knowledge on fall prevention
Both intervention and control groups showed a statistically significant improvement in knowledge mean score (P<0.05). However, there was no significant difference between intervention and control groups at baseline, 3rd, and 6th month after the intervention. Interestingly, the intervention group showed a faster statistically significant improvement in knowledge mean score than those in the control group at the 3rd month (P=0.026; ).
Table 2 Multiple comparisons on knowledge, number of exercises, TUG, BBS, and incidence of falls within and between groups (n=64)
Number of exercises
The intervention group showed a statistically significant higher number of exercises than the control group at 3rd and 6th month (P<0.05). Moreover, the intervention group showed a statistically significant increment number of exercises over time (P<0.05; ).
Balance
There was no statistically significant difference in TUG and BBS mean score between the two groups at baseline, 3rd, and 6th month. However, the intervention group revealed statistically significant improvement in both TUG and BBS at 6th month after the intervention was performed (P<0.01; ).
Incidence of falls
During the 6-month study period, there was one fall incident in the control group, whereas no fall incident in the intervention group. The fall incident rate of participants in the control group was 0.06 person-year. The elderly reported that the fall happened during the walk and the knee collapsed, but it did not amount to injuries. There were no falls or injuries associated with performing the exercise fall prevention program.
Result from coaching
From the researcher’s observation and interview, the elderly in the intervention group were excited about using the robot by participating in setting the robot and watching videos provided in the program, while elderly in the control group did not show interest in using the handbook.
All participants in the intervention group were scheduled coaching by the same principle investigator throughout the study period to develop trust. In the first 2 months, the elderly rarely used the robot because they forgot “how to” use it, thus teaching was repeated many times to ensure elderly could use the robot independently.
The results from coaching found that few functions were not feasible with user behavior. From the interview it was gathered that the elderly switched off and unplugged the robot when they do not use it. The elderly reported the irregular use of alarm functions including daily voice messages and exercise reminders because they often forgot to switch on the robot at 8.00 AM and 8.00 PM.
Discussion
The robotic fall prevention program in this quasi-experimental study, which composed of a small robot-installed fall prevention software together with personal coaching and fall prevention handbook can improve knowledge on fall prevention, promote exercises activity, and enhance balance among the participants.
Both intervention and control groups showed statistically significant improvements in knowledge mean score. The result from our study indicates that both handbook and robotic program have successfully improved knowledge score on fall prevention among participants. However, the intervention group reveals a faster increment on knowledge mean score than the control group at 3rd month after the intervention was performed.
In the intervention group, the daily voice message to convey knowledge on fall prevention was setup at 8.00 PM. Although the participant often forgot to switch on the robot at 8.00 PM, they still received the benefit from the video education that is provided in the software. The faster increment of knowledge mean score may be due to the interest of the elderly toward the program. From the researcher’s observation and interview, the elderly in the intervention group were excited about using the robot. The attraction of the intervention affects participants’ motivation to being engaged in the program. This notion was supported by previous literature in the USA, 2009Citation46 that stated that videos have the potential to grab learner’s attention. Moreover, a previous studyCitation47 conducted on fall prevention education among inpatients in Australia, 2009 found that delivery video disc compared to a written workbook is more likely to achieve self-perceived risk of falling and higher levels of confidence and motivation to engage in self-protective strategies than participants who received the written workbook. The increment of knowledge mean score was also in line with a systematic review of 2013,Citation48 which suggested that an intensive face-to-face falls education program with multimedia materials should be considered for educating elderly patients during and after hospitalization.
The intervention group shows the higher number of exercises than the control group both at 3rd and 6th month. The exercise reminder was setup at 8.00 AM. Even when the elderly forgot to switch on the robot at 8.00 AM, they still got the benefit from videos and coaching. Thus, these participants were more adherent to exercise than the control group. This notion is supported with a previous qualitative studyCitation48 of 2016, which indicated that the adherence to exercise could be enhanced by increasing the attractiveness of exercise programs, providing a model or feedback, and the feeling of being supported by care providers. Elderly patients prefer the possibility of being guided or supervised when doing exercise, and regularly checked and discussed with their care providers.
The intervention group shows a statistically significant improvement in the number of exercises after 6 months post-intervention. These may be due to participants becoming more familiar with using the robot. According to personal coaching, the elderly were not familiar using the robot in the first few months. After many repeated training and coaching, they could turn on and operate robot by themselves. Thus, the trend of exercise is increasing at 6th month compared to 3rd month.
There was no statistically significant difference in balance score between intervention and control groups at baseline, 3rd, and 6th month after the intervention was performed. The possible reason why the participants in our control group could maintain their balance might be that they were engaged in other exercise activities such as walking, jogging, and arm swing, hence the balance score between intervention and control groups were not different.
The intervention group showed statistically significant improvements in balance with both TUG and BBS at 6th month post-intervention. The improvement in TUG and BBS mean scores in the intervention group is correspondent with number of exercises (). The intervention group performed more exercises than the control group, and eventually increased their balance score.
In this study, we chose exercise videos which were modified from the OEP,Citation27,Citation28 and we innovated a robotic program together with coaching and handbook. The improvement of balance in this study is correspondent with previous studies on OEP in Iran (2016),Citation49 New Zealand (2003),Citation16 and a systematic review (2010).Citation29 Moreover, the finding of this study is also correspondent with recent studies in USACitation50,Citation51 that conducted another delivery method of Otago exercise by the non-physical therapist. The data suggest that the action of doing the exercises may be the essential element of the OEP, providing opportunities to develop and test new delivery models.
One fall incident happened in the control group during the 6-month study period. Fall happened while the participant was walking in the community. The fall incidence rate of participants in the control group was 0.06 person-year or 62.49 per 1,000 person-year. There were no falls or injuries associated with performing the exercise program in both groups. The robotics program was implemented safely among the participants.
Strengths, limitations, and practical recommendations
The first strength of this study is that the quasi-experimental study was used to investigate the effectiveness of robotic fall prevention program in a real-life environment. The second strength is the 100% follow-up rate of all participants in both intervention and control groups. Thus, we can ensure the power of statistics at 0.80. The third strength is that the validated and reliable measurement tools on balance were used in this study.Citation41,Citation42,Citation45,Citation52 And the fourth strength is that the education videos were chosen from trustable sources: exercise videosCitation27,Citation28 from the Ministry of Public Health, and fall prevention videos from educational institutions.Citation30–Citation33
However, some limitations existed in this study. First was the limitation of time. As fall incidence was found only 0.3–1.6 falls/year/person,Citation12 further study is recommended to take a longer period of time. Second, hardware components such as a small screen or low volume speaker was considered as a limitation. The future software and hardware developed for elderly should be more user-friendly by providing a wider screen on the robot, television screen connection, louder voice adjustable, and having a hearing equipment connection.
As a practical recommendation, a technology designed for the elderly should be considered with the behavior of the user in mind. The elderly switches off and unplug the robot when they do not use it. Thus, chargeable robot or embedded battery should be considered to ensure all-time functioning of the robot. Moreover, Thai elderly are not familiar with using new technologies. Thus, adoption of this program should come together with three components: robot-installed fall prevention program, fall prevention handbook, and coaching session from trained staff or caregiver.
This study provides an alternative delivering model of fall prevention intervention by using the robot. This innovation is in correspondence with a future trend of shrinkage of child population and increase of the elderly globally.Citation53 Innovation-assisted elderly is more important in the future.
Conclusion
The robotic fall prevention program, which composed of a small robot-installed fall prevention software together with personal coaching and fall prevention handbook, can increase knowledge on fall prevention, promote exercises, and improve balance among physically active elderly who is at risk of fall, residing in senior housings.
Acknowledgments
This study was funded by the Thailand Research Fund and Scholarship from the Graduate School, Chulalongkorn University to commemorate the 72nd Anniversary of His Majesty King Bhumibol Adulyadej and the 90th Anniversary Chulalongkorn University (Ratchadaphiseksomphot Endowment Fund).
Disclosure
The authors report no conflicts of interest in this work.
References
- WuHOuyangPHong WuPOFall prevalence, time trend and its related risk factors among elderly people in ChinaArch Gerontol Geriatr20177329429928910753
- BuckinxFCroisierJLReginsterJYPrediction of the incidence of falls and deaths among elderly nursing home residents: the senior studyJ Am Med Dir Assoc2018191182428757332
- BurtonELewinGO’ConnellHHillKDFalls prevention in community care: 10 years onClin Interv Aging2018131326126929483772
- Ageing and life-course: Falls prevention in older ageWorld Health organization (WHO)2016 Available from: http://www.who.int/ageing/projects/falls_prevention_older_age/en/AccessedMay 17, 2016
- AekplakarnWichaiThai National health Examination Survey5th edNonthaburi, ThailandHealth Systems Research Institute (HSRI)2014 Available from: http://thaitgri.org/?p=37869Accessed September 12, 2018
- FallsWorld Health Organization2018 Available from: http://www.who.int/news-room/fact-sheets/detail/fallsAccessed June 12, 2018
- National Center for Injury Prevention and ControlPreventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention ProgramsAtlanta, GA2015 Available from: https://www.cdc.gov/homeandrecreationalsafety/falls/community_preventfalls.htmlAccessed October 29, 2018
- Thanyaluck AnothaisinthaweeSTSrisawanPYothasamutCFall Prevention Medication.BangkokResearch Institution and Elderly Development Foundation2012 Available from: www.thaitgri.orgAccessed May 30, 2016
- HendrieDInjury in Western Australia: The Health System Costs of Falls in Older Adults in Western AustraliaPerth, Western AustraliaWestern Australian Government2003
- NurmiILüthjePIncidence and costs of falls and fall injuries among elderly in institutional careScand J Prim Health Care200220211812212184711
- The University of YorkThe Economic Cost of Hip Fracture in the UKEnglandHealth Promotion2000
- RubensteinLZFalls in older people: epidemiology, risk factors and strategies for preventionAge Ageing200635suppl_2ii37ii4116926202
- ThomasRFriedenDHBaldwinGDellingerALeeRPreventioning Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs2nd edAtlanta, GACenters for Disease Control and Prevention National Center for Injury Prevention and Control2015
- Areerat SuphutitadaRBSathanonPElderly Handbook: Good Walking, No Falling Nonthaburi Health Systems Research Institute (HSRI)2016 Available from: https://www.hsri.or.th/researcher/media/printed-matter/detail/7256Accessed September 10, 2018
- GillespieLDRobertsonMCGillespieWJSherringtonCInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20129CD007146
- John CampbellAMCR. Otago Exercise Programme to Prevent Falls in Older AdultsNew ZealandOtago Medical School, University of Otago2003
- UKAFalls Prevention Exercise – Following the EvidenceUK2013 Available from: www.ageuk.org.ukAccessed August 12, 2018
- HammJMoneyAGAtwalAParaskevopoulosIFall prevention intervention technologies: a conceptual framework and survey of the state of the artJ Biomed Inform20165931934526773345
- RuccoRSorrisoALiparotiMType and location of wearable sensors for monitoring falls during static and dynamic tasks in healthy elderly: a reviewSensors (Basel)20181851613
- Robots are ready and welcome to assist the elderly2016 Available from: http://www.scmp.com/native/tech/topics/premier-living/article/1867828/robots-are-ready-and-welcome-assist-elderlyAccessed November 10, 2016
- CT Asia Robotics Co. L.Dinsow Mini 2012–2012 Available from: http://www.ctasiarobotics.com/home/index.phpAccessed June 12, 2018
- PiphatvanitchaNThe Effect of a Fall Prevention Program on Gait and Balance of Community – Dwelling Elders. Nursing SciencesBangkokChulalongkorn University2016
- Centers for Disease Control and PreventionAlgorithm for fall risk screening, assessment, and interventionCenter for Disease Control and Prevention NCfipacUSACenter for Disease Control and Prevention, National Center for Injury Prevention and Control2017
- RmPDPrasertpornJSomluckPSaowaluckJAmpaiYThe inter-rater reliability of Barthel index (Thai version) in stroke patientsJ Thai Rehabil200616119
- Behavioral Change Models: The Social Cognitive TheoryBoston University School of Public Health2013 Available from: http://sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/BehavioralChangeTheories/BehavioralChangeTheories5.htmlAccessed February 2, 2019
- BettmanJRMethods for Analyzing Consumer Information Processing ModelsPaper presented at: SV – Proceedings of the Second Annual Conference of the Association for Consumer Research1971Labovitz School of Business & Economics, University of Minnesota Duluth
- ThaiHITAPLight exercise of fall prevention in elderly Health Intervention and Technology Assessment ProgramThailandMinistry of Public Health2016
- ThaiHITAPAdvance exercise of fall prevention in elderly Health Intervention and Technology Assessment ProgramThailandMinistry of Public Health2014
- ThomasSMackintoshSHalbertJDoes the ‘Otago exercise programme’ reduce mortality and falls in older adults?: a systematic review and meta-analysisAge Ageing201039668168720817938
- Faculty of Medicine Siriraj Hospital MUFall prevention in elderlyBangkokSiriraj Pr2008
- TaninnitLeerapunHow to use cane for knee pain. Faculty of MedicineChiang MaiChiang Mai University2016
- TV program Happy body hm. Walker. dmc tv2014 Available from: https://www.youtube.com/watch?v=aoHrovMfi5Y&t=73sAccessed January 12, 2018
- Department of RehabilitationHow to use wheel chair for caregiver. Department of Rehabilitation, Faculty of MedicineChiang MaiChiang Mai Univerity2016
- ManeepromNChoosing appropriate shoe. Research Project Fall Prevention in Elderly, College of Public Health SciencesBangkokChulalongkorn University2017
- ManeepromNMaking sand bag Research Project Fall Prevention in Elderly, College of Public Health SciencesBangkokChulalongkorn University2017
- CurrieLFall and Injury Prevention2008HughesRGPatient Safety and Quality: An Evidence-Based Handbook for NursesRockvilleAgency for Healthcare Research and Quality (US)
- Checklist for safety: A home fall prevention checklist for older adults Center for Disease Control and Prevention, National Center for injury prevention and control, U.S. Department of Health & Human Services2016 Available from: https://www.cdc.gov/steadi/Accessed April 2017
- Shumway-CookABaldwinMPolissarNLGruberWPredicting the probability for falls in community-dwelling older adultsPhys Ther19977788128199256869
- Barthel Index (BI) Available from: https://commondataelements.ninds.nih.gov/Doc/NOC/Barthel_Index_NOC_Public_Domain.pdfAccessed September 21, 2015
- TiagoSAlexandreDMMNatáliaCRSimoneKMAccuracy of Timed Up and Go Test for screening risk of falls among community-dwelling elderlyRev Bras Fisioter2012165381388
- SebastiãoESandroffBMLearmonthYCMotlRWValidity of the timed up and Go test as a measure of functional mobility in persons with multiple sclerosisArch Phys Med Rehabil20169771072107726944709
- ChanPPSi TouJITseMMNgSSReliability and validity of the timed up and Go test with a motor task in people with chronic strokeArch Phys Med Rehabil201798112213222028392324
- Institute of Geriatric MedicineMedical practice guideline for prevention/ evaluation fall in elderly Thailand Health Department, Ministry of Public Health Thailand2008 Available from: www.dms.moph.go.th/dmsweb/cpgcorner/2009021784231.pdfAccessed February 2, 2019 Thai
- MajorMJFatoneSRothEJValidity and reliability of the Berg balance scale for community-dwelling persons with lower-limb amputationArch Phys Med Rehabil201394112194220223856150
- ParkSHLeeYSSeong-Hi ParkY-SLThe diagnostic accuracy of the Berg balance scale in predicting fallsWest J Nurs Res201739111502152527784833
- BerkRAMultimedia teaching with video clips: TV, movies, YouTube, and mtvU in the College classroomInt J Technol Teach Learn200951121
- SmA-MHHoffmannTHillKA randomized trial comparing digital video disc with written delivery of falls prevention education for older patients in hospitalJ Am Geriatr Soc20095781458146319515102
- PalazzoCKlingerEDornerVBarriers to home-based exercise program adherence with chronic low back pain: patient expectations regarding new technologiesAnn Phys Rehabil Med201659210711327050664
- DadgariAAizan HamidTHakimMNRandomized control trials on Otago exercise program (OEP) to reduce falls among elderly community dwellers in Shahroud, IranIran Red Crescent Med J2016185e2634027478629
- ShubertTESmithMLGotoLJiangLOryMGOtago exercise program in the United States: comparison of 2 implementation modelsPhys Ther201797218719728204770
- ShubertTEGotoLSSmithMLJiangLRudmanHOryMGThe Otago exercise program: innovative delivery models to maximize sustained outcomes for high risk, Homebound older adultsFront Public Health201755428386536
- Berg Balance ScaleRehabilitation measures database2010 Available from: http://www.rehabmeasures.org/Lists/RehabMeasures/PrintViewaspx?ID=888Accessed May 28, 2016
- United NationsWorld Population Prospects: The 2017 Revision, Key Findings and Advance Tables Vol Working Paper No ESA/P/WP/248New York, USAUnited Nations, Department of Economic and Social Affairs, Population Division2017