Abstract
Purpose
This study aims to investigate the effect of transcutaneous electrical acupoint stimulation (TEAS) on postoperative delirium (POD) in elderly patients with silent lacunar infarct and preliminarily to determine the relationship among TEAS, blood–brain barrier (BBB), neuroinflammation, and POD.
Patients and methods
Sixty-four-old patients with silent lacunar infarct were randomly divided into two groups: group TEAS and control group (group C). Patients in the group TEAS received TEAS (disperse-dense waves; frequency, 2/100 Hz) on acupoints Hegu and Neiguan of both sides starting from 30 minutes before induction of anesthesia until the end of surgery, and the intensity was the maximum current that could be tolerated. In group C, electrodes were placed on the same acupoints before anesthesia induction, but no current was given. At 0 minute before the treatment of TEAS, 30 minutes after skin incision, and after completion of surgery (T1–3), blood samples were extracted to detect the concentration of serum tumor necrosis factor (TNF)-α, interleukin-6 (IL-6), matrix metalloproteinase-9 (MMP-9), and S100β. We assessed patients for delirium and coma twice daily in the first 3 postoperative days using the Confusion Assessment Method for the intensive care unit and the Richmond Agitation-Sedation Scale.
Results
This study preliminarily suggests that TEAS can reduce the development of POD in elderly patients with silent lacunar infarction (6.3% vs 25.0%; P=0.039). Compared with the baseline value at T1, the serum concentrations of IL-6, TNF-α, MMP-9, and S100β were significantly increased at T2–3 in both the groups (P<0.05). Compared with group TEAS, serum levels of TNF-α and IL-6 were higher at T2–3 and serum levels of MMP-9 and S100β were higher at T3 in group C (P<0.05). The intraoperative anesthetic consumptions were less in group TEAS than group C.
Conclusion
TEAS can alleviate POD in older patients with silent lacunar infarction and may be related to reduce the neuroinflammation by lowering the permeability of BBB.
Introduction
Postoperative delirium (POD) is a common complication of surgical procedures in the elderly and causes difficulty in postoperative care. Acute and fluctuating alterations of consciousness, attention, and cognition are characteristic features of delirium.Citation1 It is associated with increased length of stay, increased charges, decreased odds of discharge to home, and accelerated cognitive decline.Citation2,Citation3 The multifactorial reason and obscure pathogenesis of delirium have made it challenging to prevent and treat. So far, although various approaches (such as nimodipine) aimed at alleviating the incidence of POD have shown early promise in efficacy trials,Citation4–Citation6 there are no conclusive studies that support nonpharmaceutic technique to prevent or decrease POD.
The blood–brain barrier (BBB) is a multicellular vascular structure that separates the central nervous system (CNS) from the peripheral blood circulation. The main functions of this barrier, namely maintenance of brain homeostasis, regulation of influx and efflux transport, and protection from harm, are determined by its specialized multicellular structure. Endothelial cells (ECs), astrocytes, pericytes, and extracellular matrix (ECM) components provide both structural and functional supports to the BBB. Every constituent cell type makes an indispensible contribution to the BBB’s integrity. But, if one member of the BBB fails and, as a result, the barrier breaks down, there can be dramatic consequences, and neuroinflammation and neurodegeneration can occur.Citation7
Impairment of the BBB occurs as people age and may account for the greater susceptibility to stroke.Citation8 Lacunar infarcts accounts for up to 25% of stroke.Citation9 Involving small penetrating cerebral arteries, lacunes are usually attributed to cerebral microatheromatosis and lipohyalinosis, although the absence of pathological evidence of occluded vessels has raised doubts about this theory.Citation10,Citation11 Lacunar infarcts are often clinically silent, but these silent subclinical events contribute significantly to the risk of large vessel stroke,Citation12,Citation13 disability,Citation14 vascular dementia,Citation15 and death.Citation16 Wardlaw et alCitation10 found that lacunar stroke is associated with a generalized increase in BBB leakiness.
Acupuncture, an important component of traditional Chinese medicine, has been used for more than 2,000 years to treat diseases and relieve pain.Citation17 Transcutaneous electric acupoint stimulation (TEAS), or “needleless acupuncture”, is an easy and noninvasive alternative to needle-based electro-acupuncture (EA). It combines the advantages of both acupuncture and transcutaneous electrical nerve stimulation by pasting electrode pads on the acupoints instead of piercing the skin with needles. TEAS makes it possible to achieve better outcomes with fewer anesthetic drugs.Citation18 Studies showed that acupuncture exerts protective effect on the brain through maintaining the BBB integrity,Citation19 but its effect on alleviating POD remains to be discussed.
This research aims to investigate the effect of TEAS on POD in geriatric adults with silent lacunar infarct and preliminarily to determine the relationship among TEAS, BBB, neuroinflammation, and POD. Results may provide reference for clinical applications. We tested the hypothesis that TEAS could reduce POD and could be associated with alleviation of neuroinflammation by lowering the permeability of BBB.
Patients and methods
Patients and setting
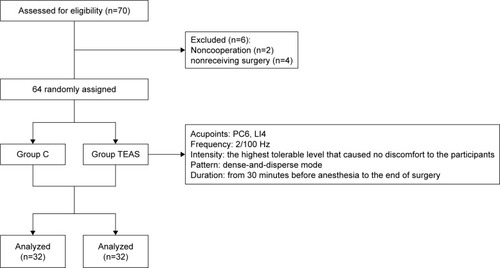
The present study has been performed with the approval of the ethics committee of the Third Hospital of Hebei Medical University (2016-012-1) and is in compliance with the Helsinki Declaration. Written informed consents of the study were collected from all the candidate subjects before randomization. The inclusion criterion was patients aged 65 years or older who underwent spine surgery in the Third Hospital of Hebei Medical University in July 2017. All patients were assessed for lacunar infarction by magnetic resonance imaging. The basic patient information was collected, including age, sex, body mass index (BMI), and American Society of Anesthesiologists’ physical status I or II. The mini-mental state examination (MMSE) was administered to screen for preoperative cognitive function 1 day before the surgery. Patients were excluded if they met any of the following criteria: MMSE score of less than 24 or dementia, due to various etiologies, preoperative delirium, history of neurological or mental illness, current use of tranquilizers or antidepressants, history of an endocrine or metabolic disorder, recent use of glucocorticoids or other hormones, suffering from infections or chronic inflammatory conditions, intake of anti-inflammatory drugs, unwillingness to complete the experimental procedures, inability to communicate in the preoperative period (language barrier or severe hearing or visual impairment), and alcohol or drug dependence. Six patients were excluded because of these criteria. As shown in , only 64 patients were enrolled in the study. The patients were divided into two groups (n=32) by using a random number table: transcutaneous electrical acupoint stimulation group (group TEAS) and control group (group C).
Anesthesia management
After entering the operating room, electrocardiogram, pulse oxygen saturation, respiratory rate, end-tidal carbon dioxide, bispectral index (BIS), and invasive blood pressure were continuously recorded in the both groups during the peri-operative period. All patients received ultrasound-guided retrograde puncture of internal jugular vein, then 12–14 cm of catheter was inserted into the deep vein catheter to jugular bulb using Seldinger method, and the location of the catheter was confirmed by X-ray.
Anesthesia induction
The patients were induced using 0.1–2 mg/kg sufentanil, 0.05–0.2 mg/kg midazolam, 0.3 mg/kg etomidate, and 0.2 mg/kg cisatracurium. A reinforced catheter was inserted after 2 minutes of cisatracurium administration. Ventilation frequency was set to 12 times per minute, inspiratory expiratory ratio to 1.0:1.5, inhaled oxygen concentration to 100%, oxygen flow to 2 L/min, and ETCO2 was maintained within the physiologic limits (35–45 mmHg).
Anesthesia maintenance
According to the theory of traditional Chinese medicine, as shown in , bilateral Hegu (LI4, located at the back of the hand, between the first and second metacarpal bones, at the midpoint of the second metacarpal radius) and Neiguan (PC6, located in the palmar of the forearm, 2 inches in the wrists) were chosen as the acupuncture points. In group TEAS, the patients received TEAS (disperse-dense waves; frequency, 2/100 Hz) on acupoints LI4 and PC6 on both sides starting from 30 minutes before induction of anesthesia until the end of the surgery, and the intensity was the maximum current that could be tolerated. In group C, electrodes were placed on the same acupoints before anesthesia induction, but no current was given. Propofol 4–6 mg/kg/h and remifentanil 0.1–0.3 mg/kg/min were intravenously (iv) infused and cisatracurium 0.05 mg/kg was administrated as intermittent iv boluses.
Figure 2 The location of the electrodes used for transcutaneous electrical acupoint stimulation.
Abbreviations: LI4, Hegu acupoint; PC6, Neiguan acupoint.

Intraoperative circulatory system was maintained by adjusting the anesthesia depth (controlling BIS, 40–60) and administering transfusions or cardiovascular agents as necessary. Blood pressure fluctuation amplitude did not exceed 20% of the base value. Atropine was used only to reverse bradycardia. After the surgery, tracheal intubation was removed when patients regained consciousness, tidal volume was 8 mL/kg, and all hemodynamic parameters such as heart rate and blood pressure returned to the normal level.
Pain control
Sufentanil (0.15 mg/kg) and tropisetron (5 mg) were administered 10 minutes before the end of the surgery for analgesia transition and prevention of postoperative nausea and vomiting (PONV). A patient-controlled iv analgesia pump was connected (1.5 mg/kg sufentanil and 6 mg tropisetron; flow rate, 2 mL/h; bolus, 0.5 mL; lockout time, 15 minutes). Postoperative pain was assessed using VASCitation20 in 24 hours after surgery. If the VAS score was greater than or equal to 4 or patients required analgesics within 24 hours, the patient received 50 mg flurbiprofen as rescue analgesia.
Blood sample collection and sample bank establishment
At 0 minute before the treatment of TEAS (T1), 30 minutes after skin incision (T2), and after completion of surgery (T3), 4 mL blood samples were taken from the jugular bulb. Blood samples were immediately placed into sterile EDTA test tubes and centrifuged at 3,000× g for 15 minutes to collect serum. Serum was aliquoted into polypropylene tubes and stored in a freezer at −80°C (Sanyo, Japan) until further assayed.
Cytokine measurement
The concentrations of tumor necrosis factor (TNF)-α, interleukin-6 (IL-6), matrix metalloproteinase-9 (MMP-9), and S100β in serum were quantified with a commercial ELISA kit (ExCell Biotech [Taicang] Co., Shanghai, People’s Republic of China) in accordance with the manufacturer’s instructions. The trained research personnel carrying out the assays was blinded to the group assignment.
Delirium evaluation
After enrollment, trained research personnel who were blinded to group assignment assessed patients’ results for POD and coma using the Confusion Assessment Method for the intensive care unit (CAM-ICU)Citation21,Citation22 and the Richmond Agitation-Sedation Scale (RASS)Citation23,Citation24 twice daily from the first to third postoperative day in the morning and in the afternoon or evening, with at least 6 hours elapsing between assessments. Patients were also assessed on the day of surgery at least 2 hours after the end of the surgery. We considered a patient delirious if they were not comatose (ie, had an RASS of −3 or more awake) and were CAM-ICU positive on either of the CAM-ICU assessments. Patients with an RASS of −4 (responsive to physical stimulus only) or −5 (completely unresponsive) were considered comatose.
Other outcomes
The primary outcomes were the incidence of POD. Secondary outcome included intraoperative propofol and remifentanil consumption.
Statistical analyses
All data were analyzed by SPSS (version 22.0 for Windows; IBM Corporation, Armonk, NY, USA). Measurement data of normal distribution were reported as the mean ± SD. Categorical variables were analyzed through chi-squared test or the Fisher’s exact probability test (when appropriate) and presented as numbers (%). Comparisons between two groups were performed with Student’s t-test. Repeated measurements were compared using repeated measure’ ANOVA. For all tests, P<0.05 was considered statistically significant.
Results
Clinical characteristics of patients and operation/anesthesia duration
All the patients received 100 mg aspirin once daily for preventing lacunar infarction. As shown in , there were no significant differences in clinical characteristics between the two groups, including gender, age, BMI, American Society of Anesthesiologists (ASA), operation duration, and anesthesia duration (P>0.05).
Table 1 Clinical characteristics of patients and operation/anesthesia duration (n=32)
IL-6, TNF-α, S100β, and MMP-9 Levels
As shown in , compared with the baseline value at T1, the serum concentrations of IL-6, TNF-α, MMP-9, and S100β were significantly increased at T2–3 (P<0.05). Compared with group TEAS, serum levels of TNF-α and IL-6 were higher at T2–3 and serum levels of MMP-9 and S100β were higher at T3 in group C (P<0.05).
Table 2 Serum IL-6, TNF-α, MMP-9, and S100β levels (n=32)
The prevalence of POD, intraoperative propofol, and remifentanil consumption
As shown in , the prevalence of POD was statistically significantly lower in group TEAS than in group C (P<0.05). Compared with group C, intraoperative propofol and remifentanil consumptions were significantly decreased in the TEAS group (P<0.05).
Table 3 The prevalence of postoperative delirium, intraoperative propofol, and remifentanil consumption (n=32)
Discussion
In this study, we preliminary found that TEAS can reduce the development of POD in geriatric patients with silent lacunar infarction undergoing spine surgery. The underlying mechanism may be related to the inhibition of neuroinflammation by lowering the permeability of BBB, which is consistent with our hypothesis.
Intraoperative anesthetic use was linked to significantly higher odds of delirium.Citation25 Perioperative opioids have been linked to sleep disturbances, which may negatively impact cognitive function.Citation26 In one review of opioid usage among chronic pain patients, the cognitive side effects from opioids were most apparent within several hours of an initial dose,Citation27 which could explain the increased risk for POD among patients who received opioids intraoperatively. The anesthetic propofol can also directly increase tau protein phosphorylation,Citation28 which is associated with the development of neurofibrillary pathology. Another mechanism is that anesthetics weaken BBB, and then surgery-induced inflammation may cross the damaged BBB and directly injure neurons, causing elevated biomarkers of neuronal injury and perhaps some of the long-term adverse effects of delirium.Citation29 Several studies indicated that TEAS could reduce the narcotics consumption.Citation30–Citation32 In the present study, TEAS decreased the anesthetics consumption during operation compared with those in group C. It is consistent with the previous studies.
Markers of neurologic injury, which are released into the blood when neurons or the BBB is damaged, provide a more feasible measure of BBB injury. Of the markers previously studied, S100β is the one that mostly correlated with BBB injury.Citation33–Citation35 S100β is expressed and secreted by astrocytes after CNS injury or ischemia and cell death.Citation36 MMPs are proteolytic enzymes that degrade all components of the ECM.Citation37 MMP-9 is one of the inducible MMPs, which are held in an inactive state until a neuroinflammatory process begins and they become active through the action of free radicals and other enzymes. Once the inducible MMPs are activated, they degrade the basal lamina and tight junctions of ECs, thereby opening the BBB.Citation38 By using ELISA, we found the significantly lower level of S100β and MMP-9 in patients of the group TEAS than those of the group C. These results indicate that TEAS can reduce the occurrence of POD, which may be related to alleviate the damage of BBB.
CNS-resident cells react to the peripheral immune signal and produce cytokines and other inflammatory mediators in the brain due to the altered permeability of the BBB.Citation39,Citation40 The amount of production of TNF-α and IL-6 is considered as the main cause of the cognitive impairment in POD, and this process may be accelerated in the elderly.Citation41–Citation44 TNF-α can stimulate the expression of other mediators responsible for the recruitment of additional inflammatory cells.Citation45,Citation46 Studies evidence that TNF-α is also in the communication between the periphery tissue and the brain.Citation47–Citation49 The high level of IL-6 is considered to be an indicator of delirium. The relationship between increased IL-6 and neuronal damage has been proposed in some studies.Citation50–Citation52 In the present study, significant difference of serum TNF-α and IL-6 levels existed between group TEAS and group C, suggesting that TEAS could significantly reduce neuroinflammation.
The location of lacunar infarcts in the thalamus and the basal ganglia is more likely to show cognitive impairment.Citation53–Citation55 The number of silent lacunar infarction was associated with mild neuropsychological abnormalities.Citation56 In our study, the lacunar infarcts were mainly in the basal ganglia, and all the patients suffered from multiple silent lacunar infarctions. We tested MMSE with patients before the surgery to rule out confounding factors. In future studies, it will be useful to take into consideration the region and the number of silent lacunar infarction, whose impact on POD has not been recognized.
The current research exhibits certain limitations. Patients with POD had an increased risk of dementia at follow-up.Citation57–Citation59 In the current study, the observation time is short. Prolonging the observation time might be helpful in guiding the management of delirious patients and assessing whether POD disturbances are a predictive factor of vascular dementia in the mid-term. In our patient population, there were only two patients with the age of ≥85 years, but it should be proposed as an interesting area of research to analyze the effect of TEAS on very elderly patients who have a worse prognosis compared to the rest of lacunar infarcts.Citation60 As acupuncture and related technique are traditional practices in Chinese culture, the psychological effect of higher acceptance might create a higher satisfactory result than in other ethic population. Moreover, this is a single-center study in a strictly defined patient population, which may be interpreted with care. A prospective randomized, double-blind, multicenter trial is justified.
Conclusion
TEAS exerts beneficial effect on POD in geriatric population with silent lacunar infarction, and such effect may be related to reduce neuroinflammation by lowering the permeability of BBB. However, the favorable effects of TEAS on improving long-term treatment outcomes remain unknown. Further work should be conducted to elucidate the mechanisms by which TEAS can intervene the development of delirium.
Acknowledgments
We would like to thank Meng Zhao, Chunping Yin, and Yangyang Guo for their advice and support on the design and analysis of this project. This work was supported by the National Natural Science Foundation of China (81771134), Natural Science Foundation of Hebei Province (H2018206305), and Hebei Provincial Government Funded Clinical Talents Cultivation and Basic Research Projects (361005).
Disclosure
The authors report no conflicts of interest in this work.
References
- InouyeSKWestendorpRGSaczynskiJSDelirium in elderly peopleLancet2014383992091192223992774
- BrownCHLaflamAMaxLDelirium after spine surgery in older adults: incidence, risk factors, and outcomesJ Am Geriatr Soc201664102101210827696373
- DavisDHMuniz-TerreraGKeageHAAssociation of delirium with cognitive decline in late life: a neuropathologic study of 3 population-based cohort studiesJAMA Psychiatry201774324425128114436
- ChanMTChengBCLeeTMGinTCODA Trial GroupBIS-guided anesthesia decreases postoperative delirium and cognitive declineJ Neurosurg Anesthesiol2013251334223027226
- HudetzJAPattersonKMIqbalZKetamine attenuates delirium after cardiac surgery with cardiopulmonary bypassJ Cardiothorac Vasc Anesth200923565165719231245
- YnLZhangQWangQJEffect of nimodipine on postoperative delirium in elderly patients with lacunar infarctionChin J Anesthesiol2018383262265
- ObermeierBDanemanRRansohoffRMDevelopment, maintenance and disruption of the blood-brain barrierNat Med201319121584159624309662
- ZeeviNPachterJMcculloughLDWolfsonLKuchelGAThe blood-brain barrier: geriatric relevance of a critical brain-body interfaceJ Am Geriatr Soc20105891749175720863334
- HinmanJDLeeMDTungSVintersHVCarmichaelSTMolecular disorganization of axons adjacent to human lacunar infarctsBrain2015138Pt 373674525614025
- WardlawJMDoubalFArmitagePLacunar stroke is associated with diffuse blood-brain barrier dysfunctionAnn Neurol200965219420219260033
- ArboixALópez-GrauMCasasnovasCGarcía-ErolesLMassonsJBalcellsMClinical study of 39 patients with atypical lacunar syndromeJ Neurol Neurosurg Psychiatry200677338138416484649
- ArsavaEMBayrleeAVangelMSeverity of leukoaraiosis determines clinical phenotype after brain infarctionNeurology2011771556121700580
- VermeerSEHollanderMvan DijkEJSilent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan StudyStroke20033451126112912690219
- SonoharaKKozakiKAkishitaMWhite matter lesions as a feature of cognitive impairment, low vitality and other symptoms of geriatric syndrome in the elderlyGeriatr Gerontol Int2008829310018713161
- DecarliCClinically asymptomatic vascular brain injury: a potent cause of cognitive impairment among older individualsJ Alzheimers Dis201333Suppl 1S417S42623034523
- ConijnMMKloppenborgRPAlgraACerebral small vessel disease and risk of death, ischemic stroke, and cardiac complications in patients with atherosclerotic disease: the Second Manifestations of ARTerial disease-Magnetic Resonance (SMART-MR) studyStroke201142113105310921868739
- TaubAAcupunctureScience1972178405695070522
- WangHXieYZhangQTranscutaneous electric acupoint stimulation reduces intra-operative remifentanil consumption and alleviates postoperative side-effects in patients undergoing sinusotomy: a prospective, randomized, placebo-controlled trialBr J Anaesth201411261075108224576720
- WangJWanYAcupuncture mechanisms: anesthesia, analgesia and protection on organ functionsWorld J Tradit Chin Med201515966
- KjeldsenHBKlausenTWRosenbergJPreferred presentation of the visual analog scale for measurement of postoperative painPain Pract201616898098426310997
- ElyEWInouyeSKBernardGRDelirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU)JAMA2001286212703271011730446
- ElyEWMargolinRFrancisJEvaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU)Crit Care Med20012971370137911445689
- SesslerCNGosnellMSGrapMJThe Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patientsAm J Respir Crit Care Med2002166101338134412421743
- ElyEWTrumanBShintaniAMonitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS)JAMA2003289222983299112799407
- WeinsteinSMPoultsidesLBaakliniLRPostoperative delirium in total knee and hip arthroplasty patients: a study of perioperative modifiable risk factorsBr J Anaesth20181205999100829661417
- KrenkLRasmussenLSKehletHNew insights into the pathophysiology of postoperative cognitive dysfunctionActa Anaesthesiol Scand201054895195620626359
- ChapmanSLByas-SmithMGReedBAEffects of intermediate- and long-term use of opioids on cognition in patients with chronic painClin J Pain2002184 SupplS83S9012479258
- WhittingtonRAVirágLMarcouillerFPropofol directly increases tau phosphorylationPLoS One201161e1664821304998
- MarcantonioERPostoperative delirium: a 76-year-old woman with delirium following surgeryJAMA20123081738122669559
- ZhouJChiHChengTOAcupuncture anesthesia for open heart surgery in contemporary ChinaInt J Cardiol20111501121621570137
- LiuXWangJWangBEffect of transcutaneous acupoint electrical stimulation on propofol sedation: an electroencephalogram analysis of patients undergoing pituitary adenomas resectionBMC Complement Altern Med2016163326817460
- YaoYZhaoQGongCTranscutaneous electrical acupoint stimulation improves the postoperative quality of recovery and analgesia after gynecological laparoscopic surgery: a randomized controlled trialEvid Based Complement Alternat Med2015201532436026170873
- BlythBJFarhavarAGeeCValidation of serum markers for blood-brain barrier disruption in traumatic brain injuryJ Neurotrauma20092691497150719257803
- KannerAAMarchiNFazioVSerum S100beta: a noninvasive marker of blood-brain barrier function and brain lesionsCancer200397112806281312767094
- MarchiNRasmussenPKapuralMPeripheral markers of brain damage and blood-brain barrier dysfunctionRestor Neurol Neurosci2003213–410912114530574
- CataJPAbdelmalakBFaragENeurological biomarkers in the peri-operative periodBr J Anaesth2011107684485822065690
- VandoorenJvan DammeJOpdenakkerGOn the structure and functions of gelatinase B/matrix metalloproteinase-9 in neuroinflammationProg Brain Res201421419320625410359
- RempeRGHartzAMSBauerBMatrix metalloproteinases in the brain and blood-brain barrier: versatile breakers and makersJ Cereb Blood Flow Metab20163691481150727323783
- AliMSHarmerMVaughanRSerum S100 protein as a marker of cerebral damage during cardiac surgeryBr J Anaesth200085228729810992840
- NguyenDNSpapenHSuFElevated serum levels of S-100beta protein and neuron-specific enolase are associated with brain injury in patients with severe sepsis and septic shockCrit Care Med20063471967197416607230
- ShenXDongYXuZSelective anesthesia-induced neuroinflammation in developing mouse brain and cognitive impairmentAnesthesiology2013118350251523314110
- TaoGZhangJZhangLSevoflurane induces tau phosphorylation and glycogen synthase kinase 3β activation in young miceAnesthesiology2014121351052724787352
- ZhengHDongYXuZSevoflurane anesthesia in pregnant mice induces neurotoxicity in fetal and offspring miceAnesthesiology2013118351652623314109
- SpiegelDRChenVA case of postoperative cognitive decline, with a highly elevated C-reactive protein, status post left ventricular assist device insertion: a review of the neuroinflammatory hypothesis of deliriumInnov Clin Neurosci2012913541
- BjornssonGLThorsteinssonLGudmundssonKOJonssonHGudmundssonSGudbjornssonBInflammatory cytokines in relation to adrenal response following total hip replacementScand J Immunol20076519910517212773
- KragsbjergPHolmbergHVikerforsTSerum concentrations of interleukin-6, tumour necrosis factor-alpha, and C-reactive protein in patients undergoing major operationsEur J Surg1995161117227727600
- AlexanderJJJacobACunninghamPHensleyLQuiggRJTNF is a key mediator of septic encephalopathy acting through its receptor, TNF receptor-1Neurochem Int200852344745617884256
- QuTUzTManevHInflammatory 5-LOX mRNA and protein are increased in brain of aging ratsNeurobiol Aging200021564765211016533
- ThompsonWLKarpusWJvan EldikLJMCP-1-deficient mice show reduced neuroinflammatory responses and increased peripheral inflammatory responses to peripheral endotoxin insultJ Neuroinflammation200853518706086
- BagnallNFaizODDelirium, frailty and IL-6 in the elderly surgical patientLangenbecks Arch Surg2014399679980024711102
- LiuPLiYWWangXSHigh serum interleukin-6 level is associated with increased risk of delirium in elderly patients after noncardiac surgery: a prospective cohort studyChin Med J2013126193621362724112153
- VasunilashornSMNgoLInouyeSKCytokines and postoperative delirium in older patients undergoing major elective surgeryJ Gerontol A Biol Sci Med Sci201570101289129526215633
- BenistySGouwAAPorcherRLocation of lacunar infarcts correlates with cognition in a sample of non-disabled subjects with age-related white-matter changes: the LADIS studyJ Neurol Neurosurg Psychiatry200980547848319211595
- Grau-OlivaresMBartrés-FazDArboixAMild cognitive impairment after lacunar infarction: voxel-based morphometry and neuropsychological assessmentCerebrovasc Dis2007235–635336117268166
- GoldGKövariEHerrmannFRCognitive consequences of thalamic, basal ganglia, and deep white matter lacunes in brain aging and dementiaStroke20053661184118815891000
- Blanco-RojasLArboixACanovasDGrau-OlivaresMOliva MoreraJCParraOCognitive profile in patients with a first-ever lacunar infarct with and without silent lacunes: a comparative studyBMC Neurol20131320324341857
- BickelHGradingerRKochsEFörstlHHigh risk of cognitive and functional decline after postoperative delirium. A three-year prospective studyDement Geriatr Cogn Disord2008261263118577850
- LundströmMEdlundABuchtGKarlssonSGustafsonYDementia after delirium in patients with femoral neck fracturesJ Am Geriatr Soc20035171002100612834522
- WitloxJEurelingsLSde JongheJFKalisvaartKJEikelenboomPvan GoolWADelirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysisJAMA2010304444345120664045
- ArboixAGarcía-ErolesLMassonsJOliveresMTargaCLacunar infarcts in patients aged 85 years and olderActa Neurol Scand20001011252910660148