Abstract
Background
The purpose of this study was to determine whether self-perceived health status is predictive of a doctor’s office visit in the Longitudinal Study on Aging (LSOA).
Methods
This was a population-based longitudinal study of persons aged ≥70 years who participated in the Study on Aging in 1984 and a follow-up survey of the LSOA in 1986. The cohort for the study consisted of 560 blacks and 6880 whites who were 70 years or older in 1984. Multivariable logistic regression analysis was performed separately for blacks and for whites.
Results
The study sample was predominantly Caucasian (91.2%) with a mean age 76.8 ± 5.5 years and mean education grade 10 ± 3.7. The majority (82%) lived above the poverty level. Self-reported poor health status predicted the use of doctor’s office services among whites (odds ratio [OR] 5.15; 95% confidence interval [CI] 3.34–7.95), but not in blacks (OR 1.6; 95% CI 0.54–4.76).
Conclusion
Self-perceived health status predicted the use of doctor’s office services among older whites but not in older blacks in the LSOA.
Introduction
Improving equality in health and access to health care across different socioeconomic and demographic groups has been a priority for health policies in the US for several decades.Citation1 However, even in countries like the UK, where national health services provide universal coverage, health inequality still remains a major problem.Citation2,Citation3 It is well established that socioeconomic, demographic, and genetic factors not only influence the development and origin of diseases, but also modify susceptibility and resistance to diseases, leading to inequality in health.Citation4–Citation6 While much attention has been drawn to inequalities in crude and disease-specific mortalities, as well as in disease-specific morbidities, often showing racial and geographic variations,Citation7,Citation8 there has been less focus on individual characteristics, such as self-perceived health status and lifestyles of individuals, that may influence vulnerability to disease and even death.
The elderly African American population has a disproportionately higher need for health and social services compared with the white American elderly population.Citation9 In spite of these higher rates of morbidity and mortality, blacks and other ethnic minorities are less likely to undergo treatment for their conditions and are more likely to be admitted to hospital more severely ill than whites.Citation10 Blacks are also more likely to present to hospital late in the course of their illnesses and often with significantly more complicated disease status.Citation12,Citation20 It has also been reported that African Americans and indeed other ethnic minorities are more likely to use emergency services than Caucasians, but use fewer preventive health services than Caucasians.Citation11,Citation19,Citation20
Historically, access to health services differs among races in the US, and is influenced by income, geography, culture, and type of health care coverage.Citation14,Citation15 Based on history and personal experience, some African Americans reportedly view receiving health care as a degrading, demeaning, and humiliating experience. Some are reported to be resentful of health clinics because of long waiting times, medical jargon, feelings of racism, segregation, loss of identity, powerlessness, and alienation from the system, as well as poverty and lack of transportation.Citation12 Individual awareness and perception of their own health has always been described as central in influencing their health-seeking behaviors.Citation13
Several researchers have reported racial disparities in access to health care in the US over recent decades. However, most of the studies have overlooked the opinions of individuals about their health, and yet have acknowledged psychosocial factors as contributing to these racial disparities. Specifically, to date, there has been a paucity of published data on the modifying effects of race and ethnicity on the association between self-perceived health status and the utilization of doctor’s office services.
This study aimed to understand the effect of race in defining the association between self-perceived health status and the utilization of doctor’s offices for health services in the late 1980s using the Longitudinal Survey on Aging (LSOA) data for 1984–86.
Materials and methods
The LSOA is a prospective multicohort study of persons aged 70 years and over that was designed primarily to measure changes in the health, functional status, living arrangements, and health services utilization of two cohorts of elderly Americans as they grow older.Citation16 The study is a collaborative project between the National Center for Health Statistics and National Institute on Aging. The Supplement on Aging study conducted in conjunction with the 1984 National Health Interview Survey served as the baseline for the LSOA study.Citation17
Cohorts from a nationally representative civilian sample comprising 7541 persons were drawn from a national probability sample of 16,148 across the US in 1984 and were followed through 1991. Between 1984 and 1991, three sets of follow-up data were collected in 1986, 1988, and 1990. In this longitudinal analysis, the information collected in 1986 was used as the end point data for the study.
The data collected at both baseline and follow-up included self-reported information on morbidity, health status, and use of health services, as well as a variety of sociodemographic, economic, and health variables. Individual and household incomes were used to measure socioeconomic status. The poverty line threshold for individual income was $4979 (1984 US dollar value) for a single person aged 65 years or older. Household income was classified into two groups based on a $20,000 (1984 value) threshold, and flashcards were used to detail family income (eg, number of dependants, expenditure, veteran or social security benefits or pension, any mortgage/home equity). Self-rated health status was classified as excellent, very good, good, fair, and poor. Education was recorded as the highest level reached by each person and was defined as a categorical variable with four levels (no education, below second grade, 1–3 years of college, and more than three years of college). Questions about marital status and living arrangements were asked, and responses categorized into four levels (living with spouse, living with relative, living with nonrelative, and living alone).Citation18
Use of health care services was recorded as the number of doctor’s office visits for consultation in the previous year and in the two weeks prior to the survey. For the number of doctor’s visits in the last two weeks, responses were categorized as 0 visits, 1–3 visits, 4–6 visits, or >7 visits, while for visits in the previous year, responses were categorized as 7–12 visits and >12 visits. For those who were hospitalized in the previous year and/or two weeks prior to their interviews, responses were recorded as number of hospital days. Medicare insurance coverage was recorded as “covered” or “not covered”. Citation18
Information about social life and well being, such as frequency of contact with family members not living in the same household and with friends/neighbors over the past two weeks in the form of visits, mail, phone calls, or outings was categorized according to “yes” or “no” responses. Similarly, the response to a question on outings, including shopping, church, sporting activities, and other activities of daily living was also recorded as “yes” or “no”.Citation18 During the baseline interview, data were collected by face to face interviews and computer-assisted telephone interviews, and by paper questionnaires in the 1986 follow-up survey. All interviews were undertaken by US Census Bureau interviewers. A complete description of the LSOA has been published previously by Kovar et al.Citation17
Data analysis
After initial univariate analysis, separate logistic regression models for African Americans and Caucasians were used to analyze the relationship between numbers of doctor’s office visits during the previous year as the dependent variable and self-perceived health status as the independent variable. To remove the effects of sociodemographic variables, the final model included adjustments for education, poverty status, family relationship, family income, Medicare coverage, social activities (eg, getting together with relatives or friends, talking to them on the telephone, or going to church, the movies, sporting activities), and activities of daily living. For the final data analysis, we used SUDAAN® statistical software which takes into account multistage sampling design to compute variance.
Results
About 92% of the subjects interviewed in 1984 were reinter-viewed in 1986, comprising 91.4% whites, 7.4% blacks, and 1.2% other races. Sixty-two percent were women and 38% were men. The mean age was 76.8 + 5 (range 70–99) years. About 57% did not complete high school, 50% achieved 10 grades, 25% completed high school (12 years of education), and 18% had more than high school education. About 48% of the sample were married, 43% were widowed, 9% were either separated or never married, 37% lived alone, 47% lived with their spouse, and 16% lived with relatives or other people. Approximately 85% of whites compared with 54% of blacks lived above the poverty level.
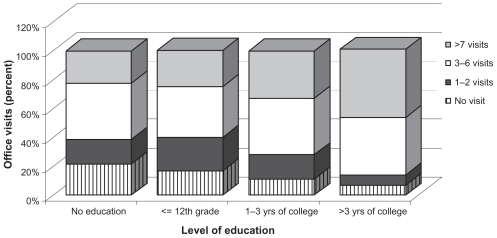
shows the socioeconomic and demographic characteristics of the study population. The level of education was inversely correlated with “no office visits” and “1–2 office visits per year” among blacks. Regardless of level of education, the percentage number of office visits for 3–6 visits per year appears relatively unchanged.
Table 1 Socioeconomic and demographic characteristics of the study population (n = 7540)
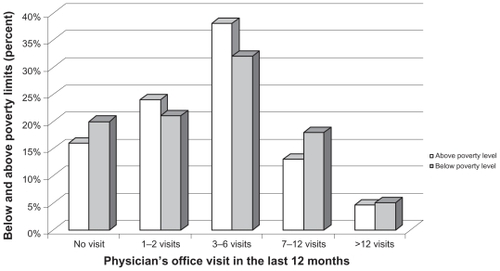
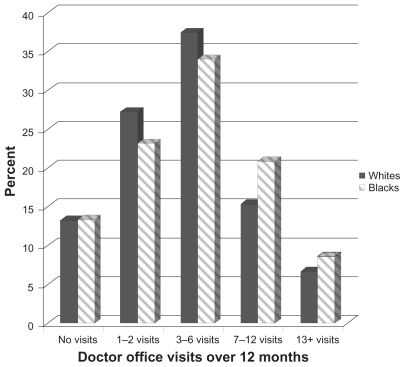
shows the relationship between number of doctor’s office visits and level of education among blacks. More blacks than whites living below the poverty threshold reported making no doctor’s office visits or making ≥7 doctor’s office visits within 12 months of the baseline interview, compared with those living above the poverty threshold. In contrast, fewer older blacks living below the poverty threshold made 1–6 visits to the doctor’s office. shows doctor’s office visits in relation to poverty level for blacks. Doctor’s office visits differed between blacks and whites; whites were disproportionately represented among those making up to six doctor’s office visits per year, whereas the converse was true for persons making more than six doctor’s office visits per year, where blacks are disproportionately represented compared with whites.
shows the percentage distribution of frequency of visits to the doctor’s office by race. Fewer blacks rated their health status as excellent (9.4%, 95% confidence interval [CI] 7.4–11.4) compared with whites (15.5%, 95% CI 14.6–16.4). In addition, a higher percentage of blacks compared with whites rated their health status as fair (28.8% versus 21.0%) or poor (22.2% versus 10.9%). Twice as many blacks compared with whites rated their health status as poor (22.2% versus 10.9%; P value = 0.00; χ2 = 40.42; DF 4.0).
Results of multivariable logistic regression analysis examining the relationship between self-perceived health status and use of doctor’s office services was fitted separately for blacks and whites, as shown in . Elderly persons who did not get together with friends and neighbors had fewer doctor’s office visits. Impairment in activities of daily living and low family income predicted the number of doctor’s office visits in whites, but was not contributory in blacks. Whites living below the poverty threshold were nearly twice as likely (odds ratio [OR] 1.66; 95% CI 1.14–2.41) to use doctor’s office services compared with whites living above the poverty threshold. However, blacks living below the poverty threshold were about 70% less likely (OR 0.33; 95% CI 0.16–0.68) to use doctor’s office services compared with those living above the poverty threshold. Among whites, those reporting very good health status were 1.5 times more likely to use doctor’s office services (OR 1.38; 95% CI 1.00–1.92) than whites with excellent health status, and blacks who reported very good health status were 70% less likely to use doctor’s office services compared with their black counterparts who reported excellent health status (OR 0.27; 95% CI 0.10–0.72). Although whites who reported good and poor health compared with excellent health, were about three and five times, respectively, more likely to use doctor’s office services, a similar health status was not predictive of doctor’s office visits among older blacks in the LSOA. Further, blacks living alone appeared to be twice as likely to use health care services compared with blacks living with a spouse (OR 2.19; 95% CI 1.17–4.08).
Table 2 Rating of self-perceived health status by race
Table 3 Multivariable logistic regression analysis modeling doctor’s office visits for blacks and whites (separate models)
Discussion
Using data from the 1984–1986 LSOA, we have demonstrated important ongoing differences in predictors and use of health care services among older Americans. Specifically, blacks living below the poverty level made fewer visits to the doctor’s office over a one-year period compared with blacks living above the poverty level.
Conversely, elderly whites living below the poverty threshold were nearly twice as likely to use doctor’s office services as elderly blacks. This indicates that blacks living below the poverty level have reduced access to both preventive health care services and medical treatment, even where such services are provided free.
Cost has been reported as an important factor in delaying health care services for patients of lower socioeconomic class. Weissman et al reported that the odds of delaying care because of cost for patients who were poor and uninsured were 12 times greater than the odds for other patients.Citation20 However, we did not observe any predictive influence of health insurance on the utilization of doctor’s office services in these studies. This could be due to the overriding effect of the predictive weight of other variables like self-perceived health status and its temporal relationship with health care utilization. Individuals must first perceive before they act or react. The stimulus for action here appears to be self-perceived health status, whereas insurance coverage merely enables the reaction.
We also found that as the number of doctor’s office visits increased beyond six visits, blacks tended to make more visits than whites (). This result is consistent with the finding by Buckle et alCitation10 that blacks are admitted significantly more often in a severely ill state than whites, and are discharged sooner than whites regardless of severity of illness, a finding that was unaccounted for by comorbid conditions, surgery, age, gender, hospital, and payer. Thus, blacks’ use of services appears likely to be driven by delay in medical diagnosis and increased burden of disabling diseases.Citation12,Citation20 Our observation that elderly whites living with a relative compared with spouses were slightly more likely to utilize the doctor’s office, and that elderly blacks living alone compared with those living with spouses were twice as likely to use health care services, is not surprising since spouses are often the main providers of care and social support, and an elderly person lacking such support is probably more likely to seek outside care for conditions that could otherwise be addressed at home.
In this study, elderly blacks compared with whites who reported excellent health status were three times less likely to use doctor’s office services. Conversely, whites who reported good health and poor health were three and five times, respectively, more likely to use doctor’s office services than whites with excellent health. This finding for perceived health status by race () is a reflection of the increasing disparity in access to health care services (ie, access to ambulatory care, rates of procedures performed in hospitals, length of short hospital stays/admissions, utilization of specialty) that exist between racial ethnic groups in the US.Citation21–Citation24
Some previous researchers have reported a lack of difference in overall health care use between blacks and whites. The results of the present analysis suggest the presence of a significant disparity in access to health care in the elderly. It is possible that methodological flaws may account for the differences among studies. Further, blacks and whites were often not examined separately in many of such studies, and the use of potential preventive services were not separated from the use of acute and chronic health care services, which could have further compounded the dissimilarities among studies. It is possible that older blacks living alone make more doctor’s office visits than whites because of psychosomatic challenges and associated stigma and social isolation, and more so given that older blacks are less likely to be married or living with a spouse.
The relatively small number of blacks and the possibility of reporting bias may have influenced our observations and therefore the conclusion of this study. Nevertheless, this research provides information on health service provider response and patient ability to seek medical help when dictated by health care needs. The knowledge gained will help health care providers understand the health behaviors of elderly white and black patients. It is imperative that a larger minority sample is included in future surveys to enhance statistical power. Increased access of older blacks to preventive health care services will serve to ameliorate further the race-related and/or ethnicity-related disparity in health status of older Americans, lessen the burden of disease, and prevent future disability in this population. In conclusion, health programs designed and targeted towards elderly persons who report fair to poor health status should promote early intervention and prevent future disabilities.
Acknowledgment
TO Obisesan was supported by grant 20-C-90721/3 from CMS, career development award AG00980 and research award RO1-AG031517 from the National Institute on Aging, and research award 1UL1RR031975-01 from the National Center for Research Resources.
Disclosure
The authors report no conflicts of interest in this work. The authors’ conclusions do not represent the views of the National Center for Health Statistics or that of the National Institute on Aging.
References
- StronksKGunning-ShepersLJShould equity in health be target number 1Eur J Public Health19933104111
- AdlerNEBoyceWTChesneyMAFolkmanSSymeLSocioeconomic disparities in health. No easy solutionJAMA1993269314031458505817
- KalzSJHoferTPSocioeconomic disparities in preventive care persist despite universal coverageJAMA19942725305348046807
- SmithGDBartleyMBlaneDThe black report on socioeconomic inequalities in health 10 years onBMJ19903013733772205320
- IllsleyROccupational class, selection and the production of inequalities in healthQ J Soc Aff19862151165
- TownsendPDavidsonNThe black reportTownsendPDavidsonNWhiteheadMInequalities in HealthHarmondsworth, UKPenguin1988
- MarmotMGShipleyMJRoseGInequalities in death, specific explanations of a general patternLancet19861100310066143919
- MarmotMGSmithGDStansfeldSHealth inequalities among British civil servants: the Whitehall II studyLancet1991337138713931674771
- Current Population Reports Money income of households, families, and persons in the United States: 1992Consumer income series, P-60 No 184Washington, DCUS Dept of Commerce, Economic and Statistics Administration, Bureau of the Census1993
- BuckleJMHornSDOatesVMAbbeyHSeverity of illness and resource use differences among white and black hospitalized elderlyArch Intern Med1992152159616031497393
- WituckiJMWallaceDCDifferences in functional status, health status, and community-based service use between blacks and white diabetes eldersJ Cult Divers199859410010025302
- SpectorRECultural Diversity in Health and Illness5th edUpper Saddle River NJPrentice Hall2003
- McGeeDLLiaoYCaoGCooperRSSelf-reported health status and mortality in a multiethnic US cohortAm J Epidemiol199914941469883792
- AdayLAAndersonRMA framework for the study of access to medical careHealth Serv Res197492082204436074
- AndersenRMRevisiting the behavioral model and access to medical care: does it matterJ Health Soc Behav1995361107738325
- National Center for Health StatisticsVital and Health Statistics: The National Interview Survey Design, 1973–1984 and Procedures, 1975–1983Washington, DCUS Government Printing Office1985
- KovarMGFittiJEChybaMMThe longitudinal study of aging: 1984–1990Vital Health Stat 11992112481502817
- National Center for Health StatisticsThe Supplement on Aging to the 1984 National Health Interview SurveyWashington, DCUS Dept of Health and Human Services, Government Printing Office1987
- AliyuMHAdediranASObisesanTOPredictors of hospital admissions in the elderly: Analysis of data from the Longitudinal Study on AgingJ Natl Med Assoc2003951158116714717472
- WeissmanJSSternRFeildingSLEpsteinAMDelayed access to health care: risk factors, reasons, and consequencesAnn Intern Med199111143253311899012
- SchappertSMAmbulatory care visits of doctor offices, hospital outpatient department, and emergency department: United States, 1995Vital Health Stat199713138
- McBeanAMGornickMDifferences by race in the rates of procedures performed in hospitals for Medicare beneficiariesHealth Care Financ Rev199415779010172157
- FalconeDBroylesRAccess to long-term care: race as a barrierJ Health Polit Policy Law1994195835957844323
- ClancyCMFranksPUtilization of specialty and primary care: the impact of HMO insurance and patient-related factorsJ Fam Pract1997455005089420586