Abstract
Although “chest distress” is the most frequent complication in the aged with chronic atrial frbrillation (AF) in clinical practice, there are few data on the association between chronic AF and coronary artery disease (CAD) in the aged in terms of medical treatment and long-term outcome. We assessed coronary artery lesions in such patients and evaluated the efficacy of medical treatment in long-term follow-ups. Of 315 elderly patients (mean age: 77.39 ± 6.33 years) who had undergone coronary angiography for chest distress, 297 exhibited sinus rhythm (SR), whereas 18 patients exhibited chronic AF. Patients with AF were followed for 4.22 ± 2.21 years. Average diastolic blood pressure (DBP) of AF patients was observed to be markedly less than that of patients with SR (57.33 ± 6.87 mmHg vs 71.08 ± 10.54 mmHg, t-test: P < 0.01). Compared with SR patients, severe stenosis of the coronary artery in AF patients was reduced (73.06% vs 44.44%, Chi-square test: P < 0.01). AF patients with chest distress had high CHADS2 score (3.72 ± 1.27), but only 33.3% patients received oral anticoagulants, and such patients had a significantly lower rate of revascularization (21.43% vs 55.63%, Chi-square test: P < 0.01), and higher rate of all-cause death (22.22% vs 4.38%, Chi-square test: P < 0.01) and thromboembolism (16.67% vs 1.68%, Chi-square test: P < 0.01) in the long-term follow-ups compared with SR patients. Chest distress in the aged with AF was related to insufficient coronary blood supply that was primarily due to a reduced DBP rather than to occult CAD. Adequate and safe medical therapy was difficult to achieve in these patients. Such patients typically have a poor prognosis, and optimal therapeutic strategies to treat them are urgently needed.
Introduction
Atrial fibrillation (AF) is a common arrhythmia that is strongly associated with age, and therein, its prevalence has increased due to the increasing size of the elderly population.Citation1–Citation3 According to recent data, the projected prevalence of AF in 2050 will increase to 7.56 million in the United States and will almost surpass 25 million by 2045 in China.Citation4,Citation5 AF is associated with increased morbidity and mortality. Coronary artery disease (CAD) is also an increasing problem in the elderly population and leads to an increased risk for cardiac events in comparison with younger patients.Citation6 Recently, more emphasis has been placed on the interaction of AF with CAD in elderly people. Several studies have investigated the prevalence and significance of new-onset AF following acute myocardial infarction (MI);Citation7,Citation8 however, there are few data on the association between chronic AF and CAD in elderly patients in terms of medical treatment and long-term outcome. Is occult CAD the main reason for “chest distress” in elderly AF patients? What is the clinical efficacy of practical medical treatment in elderly AF patients with chest distress vs sinus rhythm (SR) patients in the long-term follow-ups? And how can adequate and safe medical therapy be achieved in these patients?
There is a paucity of available data that can be used to guide the management of elderly chronic AF patients with chest distress. The present study assessed the coronary artery lesions and evaluated the long-term outcomes of AF in the aged with chest distress vs SR patients.
Methods
Study population
The study was conducted at the General Hospital of the Chinese People’s Liberation Army. The study was approved by the local ethics committee. We reviewed patients of age ≥65 years who had undergone coronary artery angiography for chest distress at our hospital from 1998 to 2009. Patients who had a pre-existing diagnosis of AF (International Classification of Diseases, Tenth Revision ICD-10 code I48) were included. CAD was defined as the presence of at least one lesion with ≥50% luminal stenosis as determined by coronary angiography.
In addition to evaluating the main clinical characteristics, the following parameters were retrospectively analyzed: (1) clinical type of AF; (2) concomitant diseases; (3) coronary angiography; (4) the influence of CHADS2 score on antithrombotic treatment and revascularization. CHADS2 is an acronym of a scoring scheme used for estimating stroke risk, containing the following conditions of the patients: C (congestive heart failure), H (hypertension), A (age >75 years), D (diabetes), and S (prior stroke or transient ischemic attack, TIA);Citation9 (5) clinical events in long-term follow-up, including all-cause death, MI, target lesion revascularization (TLR), thromboembolism, and bleeding episodes. TLR was defined as a re-intervention that was driven by any lesion located in the stented vessel. Indication for a repeat revascularization was based on angina symptoms, significant luminal stenosis (>50% diameter), and/or proven myocardial ischemia in the target vessel territory. Indication for a repeat revascularization was based on angina symptoms, significant luminal stenosis (>50% diameter), and/or proven myocardial ischemia in the target vessel territory. Patients who were unable or unwilling to follow-up were not included.
Statistical analysis
Continuous variables were tested for a normal distribution using the Kolmogorov–Smirnov test. The normally distributed continuous variables are shown as mean ± SD. Discrete variables are presented as frequencies (percentages). The discrete variables were compared via either the Chi-square test, continuity correction, or Fisher’s test (when the 2 × 2 table had <five patients). Comparison of the groups for continuous variables was performed with the t-test for independent samples that are parametrically distributed. All P values were two-sided, and a P value of <0.05 was considered to be statistically significant. Statistical analyses were performed using SPSS (v 18.0; SPSS, Inc, Chicago, IL).
Results
Patient characteristics
This study included 315 patients (312 men and 3 women) who underwent percutaneous coronary interventions (PCIs) from 1998 to 2009 and had detailed clinical records. Among these patients, 297 patients (294 men and three women) had an SR. In total, 18 patients (5.71%) with pre-existing AF were identified, in addition to six cases of permanent AF, ten cases of paroxysmal AF, and two cases of persistent AF. Mean age of the AF patients was 79 years (range: 65 to 87 years), and mean duration of AF was 10.21 ± 6.5 years (range: 0.7 to 27 years). The most frequent concomitant disease of AF with chest distress in the aged was heart failure (HF), followed by hypertension and diabetes mellitus ().
Table 1 Baseline characteristics of the study population
Average DBP of the investigated AF patients was lower than that of patients with SR (57.33 ± 6.87 mmHg vs 71.08 ± 10.54 mmHg, t-test: P < 0.01) ().
Table 2 Clinical assessment of elderly patients with chest distress
Coronary angiography
The angiographic results obtained from elderly patients with AF in comparison with those obtained from patients with SR are shown in . A narrowing of >75% was present in 44.44% of patients with AF and in 73.06% of patients with SR (Chi-square test: P < 0.01; ).
Table 3 The number of vessels with coronary disease in elderly patients with chest distress
Table 4 Coronary artery stenosis in patients with different heart rhythms
Revascularization and antithrombotic therapy
SR patients had a significantly higher rate of revascularization than AF patients (55.63% vs 21.43%, P = 0.012), 136 (51.12%) received stent, and 12 (4.51%) were treated with a coronary artery bypass graft. Most patients received a drug-eluting stent (DES). Antithrombotic medications in SR patients after stent implantation included lifelong aspirin (ASA) and clopidogrel 75 mg/day for 1 year, with a minimum recommended duration of 6 months in the DES and 1 month in the bare metal stent. Moreover, of the 18 patients with AF, seven (38.89%) were treated with both ASA and clopidogrel, five (27.78%) were prescribed a single antiplatelet drug (ASA or clopidogrel), and six (33.33%) received warfarin.
Influence of CHADS2 score on antithrombotic treatment
Based on the presence of concomitant diseases and a history of previous stroke or TIA, the mean CHADS2 score in AF patients was 3.72 ± 1.27. The distribution of the CHADS2 scores in these elderly patients with chest distress was as follows: 16.7% (3/18) = 2, 33.3% (6/18) = 3, 22.2% (4/18) = 4, 16.7% (3/18) = 5, and 11.1% (2/18) = 6. However, oral anticoagulant (OAC) was administered to only 33.3% of the patients. The patient with a CHADS2 score of 4 received triple therapy with OAC, ASA, and clopidogrel after implanting DES.
Long-term outcomes
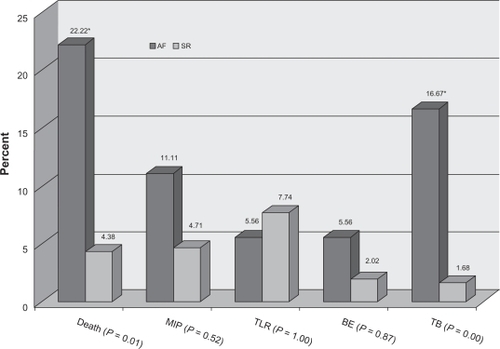
All patients were followed for 4.22 ± 2.21 years (range: 1–8 years) to ascertain the clinical outcomes. All-cause death (22.22% vs 4.38%, Chi-square test: P < 0.01) and thromboembolism (16.67% vs 1.68%, Chi-square test: P < 0.01) were higher in AF than SR patients. There were no significant difference in MI (11.11% vs 4.71%, P = 0.52), TLR (5.56% vs 7.74%, P = 1.00), or bleeding events (5.56% vs 2.02%, P = 0.87) between AF and SR patients ().
Discussion
Chest distress in elderly patients with chronic AF is a common clinical problem faced by clinicians. The optimal therapeutic strategy for such patients is based on the major cause of the myocardial ischemia. Our findings reveal that in the elderly population with chronic AF, chest distress might not be associated with severe coronary stenosis. Elderly patients with chronic AF had lower occurrence of arterial narrowing (> 75%) than patients with SR. This observation agrees with those of Androulakis et al, who found that patients with paroxysmal AF or persistent AF with a duration >30 days and concomitant ischemic ST segment depression exhibited ST-segment changes that were not consistently associated with the presence of obstructive CAD, especially considering that approximately only one in three patients presented angiographically significant coronary lesions.Citation10 In another study, Lau et al screened 3393 patients with acute coronary syndrome (ACS), and observed that 149 (4.4%) patients had new-onset AF and 387 (11.4%) patients had previous AF. In contrast to cases of new-onset AF, a history of previous AF was less frequent in patients with ST-segment elevation MI and left main CAD.Citation11 Furthermore, we also found that the average DBP in elderly patients with chronic AF was markedly less than that in patients with SR, which most likely explains the chest distress experienced by chronic AF patients due to an insufficient coronary blood supply caused by a reduced DBP. More specifically, it is well known that most of the coronary flow occurs during diastole, and that good autoregulation between perfusion pressures of 60 and 200 mmHg can help maintain normal coronary blood flow. When the coronary perfusion pressure decreases, the subendocardial flow decreases. A further decrease in pressure to <60 mmHg will suppress midcardial layer autoregulation, and, furthermore, subepicardial regulation will eventually wane at pressures <50 mmHg.Citation12
AF patients with chest distress had high CHADS2 score (3.72 ± 1.27), but only about one-third of patients received OAC. And such patients had a significantly lower rate of revascularization. All-cause death and thromboembolism were obviously higher in AF than in SR patients at an average follow-up of 4.22 years. Similarly, Lau et al observed that ACS patients with previous histories of AF had greater mortality rates than those with SR at 12-month follow-up.Citation11 One reason is that the elderly patients with chronic AF had a greater incidence of HF than elderly patients with SR. A similar phenomenon was observed in the Pro.V.A. Study,Citation13 wherein patients with AF and low ejection fractions had the highest absolute risk for adverse cardiovascular outcomes.Citation14 An additional cause for it is that it is too difficult to achieve a sufficiently effective and safe antithrombotic therapy for this population after PCI. Halbfass et al found an 11.5% rate of major bleedings, a 5.3% rate of thromboembolic events, and a 2.7% rate of stent thromboses in the high-risk group of patients with AF and coronary stent implants.Citation15 Triple antithrombotic therapy (clopidogrel, ASA, and OAC) seemed to be clearly superior to a combination of clopidogrel and ASA in the prevention of cardiovascular events;Citation16,Citation17 however, a high rate of major bleeding was observed in AF patients with triple antithrombotic therapy.Citation18 The optimization of antithrombotic strategies in such patients is a delicate balance between the efficacy of these therapies and the bleeding risk. Based on the available evidence of the use, safety, and efficacy of the various antithrombotic agents, there are three suggested treatment strategies. (1) Triple therapy with OAC, ASA, and clopidogrel should be used for patients with a low-risk of hemorrhage. (2) Implantation of drug-eluting stents should be avoided in patients with a high hemorrhagic risk due to the prolonged need for dual antiplatelet administration. (3) For patients who are at risk for both thrombosis/thromboembolism and hemorrhage, bare metal stents are preferred, and a combination of clopidogrel and OAC should be used for 1 month before continuing to antithrombotic treatment with OAC.Citation19,Citation20
Conclusion
In conclusion, elderly AF patients with chest distress exhibited less frequent occurrence of CAD than SR patients. It was found that the chest distress observed in elderly patients with AF resulted from insufficient coronary blood supply due to a low DBP instead of from occult CAD. Such patients had high CHADS2 score (3.72 ± 1.27), but only about one-third of patients received OAC. A significantly lower rate of revascularization in AF patients was observed, while all-cause death and thromboembolism were obviously higher in the long follow-up. Antithrombotic therapy, especially after PCI, is a challenging problem in clinical practice, and optimal therapeutic strategies are needed. Prospective, randomized, and larger population studies are needed to confirm our results and to derive practical guidelines that clinicians can use to manage elderly AF patients with chest distress.
Acknowledgements
This work was supported by grants from the Beijing Natural Science Foundation (7093134). The sponsors did not have a role in the design or conduct of the study, analysis of data, or preparation of the manuscript. We thank the participants and all of the staff involved in this study.
Disclosure
The authors declare no conflicts of interest in this work.
References
- Lloyd-JonesDMWangTJLeipEPLifetime risk for development of atrial fibrillation the Framingham heart studyCirculation20041101042104615313941
- ZhouZQHuDYChenJZhangRHLiKBZhaoXLAn epidemiological survey of atrial fibrillation in ChinaChinese Journal of Internal Medicine200426491494 Chinese.
- QiWenhangRetrospective investigation of hospitalized patients with atrial fibrillation in mainland ChinaInt J Cardiol200510528328716274769
- NaccarelliGVVarkerHLinJSchulmanKLIncreasing prevalence of atrial fibrillation and flutter in the United StatesAm J Cardiol20091041534153919932788
- MaCSQiWHManagement of atrial fibrillation in Chinese patientsCVD Prev Control200947983
- TeoKKSedlisSPBodenWECOURAGE Trial InvestigatorsOptimal medical therapy with or without percutaneous coronary intervention in older patients with stable coronary disease: a pre-specified subset analysis of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation) trialJ Am Coll Cardiol2009541303130819778673
- LopesRDElliottLEWhiteHDAntithrombotic therapy and outcomes of patients with atrial fibrillation following primary percutaneous coronary intervention: results from the APEX-AMI trialEur Heart J2009302019202819502623
- JaneSSDavidMZhengZTrends in atrial fibrillation complicating myocardial infarctionAm J Cardiol200910416917419576341
- GageBFWatermanADShannonWBoechlerMRichMWRadfordMJValidation of clinical classification schemes for predicting stroke. Results form the National Registry of Atrial FibrillationJAMA20012852864287011401607
- AndroulakisAAznaouridisKAAggeliCJTransient ST-segment depression during paroxysms of atrial fibrillation in otherwise normal individuals: relation with underlying coronary artery diseaseJ Am Coll Cardiol2007501909191117980260
- LauDHHuynhLTChewDPAstleyCMSomanASandersPPrognostic impact of types of atrial fibrillation in acute coronary syndromesAm J Cardiol20091041317132319892044
- FumihikoKMasahitoKTaroMPhysiomics of coronary perfusion and cardiac pumpingCardiac perfusion and pumping engineeringDhanjooNGEddieYKNWashington, DCWorld Scientific Publishing Co2007115
- BilatoCCortiMCBaggioGPrevalence, functional impact, and mortality of atrial fibrillation in an older Italian population (from the Pro.V.A. Study)Am J Cardiol20091041092109719801031
- OlssonLGSwedbergKDucharmeACHARM InvestigatorsAtrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity (CHARM) programJ Am Coll Cardiol2006471997200416697316
- HalbfassPJankoSDorwarthURiessGAntoniDHoffmannEDilemma of antithrombotic therapy in anticoagulated atrial fibrillation patients squeezed between thrombosis and bleeding events: a single-centre experienceEuropace20091195796019493910
- MaegdefesselLSchlittAFaerberJAnticoagulant and/or anti-platelet treatment in patients with atrial fibrillation after percutaneous coronary intervention. A single-center experienceMed Klin (Munich)200810362863218813885
- AndrewZFrederickFOptimizing antithrombotic strategies in patients with concomitant indications for warfarin undergoing coronary artery stentingAm J Cardiol.2009104Suppl49C54C
- Manzano-FernándezSPastorFJMarínFCambroneroFCaroCPascual-FigalDAIncreased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stentingChest200813455956718641090
- Manzano-FernándezSCaroCCambroneroFPastorFJMarínFValdés-ChavarriMAntithrombotic therapy after coronary stenting in patients with indication for oral anticoagulationInt J Cardiol200913412512718353470
- StevenFJonathanLH“Triple therapy” or triple threatJ Am Coll Cardiol20085182682718294567