Abstract
Background
Residents in nursing homes (NHs) are often frail older persons who have impaired physical activity. Urinary incontinence (UI) is a common complaint for residents in NHs. Reduced functional ability and residence in NHs are documented to be risk factors for UI.
Objective
To investigate if an individualized training program designed to improve activity of daily living (ADL) and physical capacity among residents in nursing homes has any impact on UI.
Materials and methods
This randomized controlled trial was a substudy of a Nordic multicenter study. Participants had to be >65 years, have stayed in the NH for more than 3 months and in need of assistance in at least one ADL. A total of 98 residents were randomly allocated to either a training group (n = 48) or a control group (n = 50) after baseline registrations. The training program lasted for 3 months and included accommodated physical activity and ADL training. Personal treatment goals were elicited for each subject. The control group received their usual care. The main outcome measure was UI as measured by a 24-hour pad-weighing test. There was no statistically significant difference between the groups on this measure at baseline (P = 0.15). Changes were calculated from baseline to 3 months after the end of the intervention.
Results
Altogether, 68 participants were included in the analysis, 35 in the intervention group and 33 in the control group. The average age was 84.3 years. The 3 months’ postintervention adjusted mean difference between groups according to amount of leakage was 191 g (P = 0.03). This result was statistically significant after adjusting for baseline level, age, sex, and functional status. The leakage increased in residents not receiving the experimental intervention, while UI in the training group showed improvement.
Conclusion
The intervention group had significant better results compared with the control group after an individualized training program designed to improve ADL and physical capacity. Further studies are needed to evaluate the effect of a goal-oriented physical training program toward NH residents UI complaints.
Introduction
Residents in nursing homes (NHs) could be described as “frail older persons who have impaired physical activity, mobility, muscle strength, cognition, nutrition, and endurance.”Citation1 Urinary incontinence (UI) is related to the severity of comorbidity and functional impairment and may be an early marker of frailty. UI is defined as “involuntary loss of urine that is a social or hygienic problem,”Citation6 and internationally recognized as a risk factor for NH placement. UI is a common complaint amongst NH residents with published prevalence rates ranging from 43% to 77%. The differences in prevalence can be explained by differences in research method, the way UI is defined, population characteristics, care settings, and care process.Citation2 UI presence and its quantification can be reliably determined by using the 24-hour pad-weighting test (24PWT).Citation3
In a recent systematic review using data from January 1997 to April 2008, Offermans et al reported that although factors influencing UI are poorly understood, dependency in activities of daily living (ADL), alertness, drugs, and mobility stand out as important risk factors for UI.Citation2 Boyington et al found that the prevalence of UI increased over their 4-year study from 65.4% to 74.3%Citation4 and that all comorbid conditions were higher at postadmission review compared with evaluation at admission. This supported the finding that an increase in UI prevalence is partly due to increasing age and frailty.
In the frail elderly, “a syndromic model” – which describes UI as multiple age-related risk factors both in and outside the lower urinary tract system – interacts synergistically to create UI.Citation1 Examples of risk factors in the lower urinary tract in men are prostate hyperplasia, while women are affected by decreases in detrusor contraction strength and urethra closure pressure, lack of estrogen, and pelvic floor dysfunctions.Citation1 Factors outside the lower urinary tract that are associated with UI are comorbid medical disease, dementia, falls, dizziness, decreased vision and hearing, neurological and psychiatric disorders, and medication.Citation1 The relationship between UI and disability is a complex phenomenon that includes clinical, pharmacological, environmental, and behavioral rehabilitative mechanisms.Citation5 However, to develop and test interventions that mediate the onset, severity, or improvement of UI in the frail elderly, several variables may be important.
Abrams et al offer an evidence-based guideline for the assessment and treatment of UI in the frail elderly.Citation6 An evidence grade of A was given to performing a functional assessment, including the evaluation of mobility, transfers, manual dexterity and the ability to toilet.Citation6 These authors recommend that treatment should depend on underlying causes.
Behavioral therapies such as prompted voiding, timed voiding, and habit training combined with exercises are recommended as UI treatment for persons with both physical and cognitive impairments. Still, there are insufficient data to determine what exactly improves UI. People undergoing treatment trials are often independently mobile and cognitively intact, which is not the case for residents in NHs who frequently experience mobility and cognitive problems.Citation7 Studies have found that functional impairment predicts subsequent UI in older adults. Likewise, UI is documented to be a risk factor for functional decline and reduced physical activity and an indicator for frailty. Therefore, given that UI is an indicator for frailty, would an intervention program focused on accommodated physical activity and ADL training decrease UI in frail older people? Functional incidental training (FIT) combines prompted voiding with low-intensity endurance and strength exercises. This approach addresses UI directly by toileting and indirectly by improving physical functioning. It is documented that FIT improves endurance and strength and reduces UI in older residents in NHs.Citation8 Still, as behavioral intervention programs have been disappointing with regard to staff compliance, it is interesting to explore what works in the FIT approach; the prompted voiding program or the exercise program?
Objective
The objective of this study was to investigate if an individualized training program designed to improve ADL and physical capacity among residents in NHs had any impact on UI, as measured by the 24PWT.
Design
Study site
This UI intervention study was a Norwegian one-site substudy of the randomized controlled clinical trial and the Nordic multicenter study Physical Functioning and Activity of Daily Living among Residents in Nursing Homes.Citation9 The multicenter study was designed to test the influence of an individually tailored intervention program on physical capacity, degree of dependence on ADL, long-term participation in physical and/or daily activities, and self-rated well-being.Citation9 It included five Nordic cities: Stockholm and Uppsala (Sweden); Oslo and Trondheim (Norway); and Odense (Denmark). Altogether, 322 residents from 24 different NHs in the five cities were included. Results presented in this article are from the sub-study in Trondheim, which included four municipal NHs out of the 24 Nordic NHs.Citation10 The intervention took place from the fall of 2005 to the spring of 2006.
Subjects
Inclusion criteria were: age ≥ 65 years, residence of the NH for more than 3 months, and need for assistance in at least one ADL. Residents with a life expectancy of <6 months were excluded. In total 115 residents from the four NHs in Trondheim were invited to take part in the study. The average length of stay was 28.5 (standard deviation [SD] = 34.7) months, and the average mini-mental state examination (MMSE) score was 12.5 (median = 12). Four of the eligible residents were not willing to participate, and 13 more residents were excluded from the study due to incomplete UI data at baseline prior to randomization and initiation of the intervention. Hence, 98 residents (74 women and 24 men) – 33, 24, 21, and 20 from the four NHs, respectively, were included. The average age at enrollment was 85.7 (SD 8.2) years and women were older than men (87.2 versus 81.1 years, P = 0.001). The overall prevalence of UI was 80.6%.
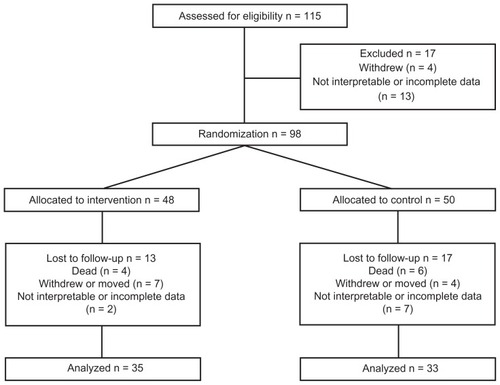
The randomization was based on a random numbers list. Consequently, 48 residents were randomized into the intervention group and 50 residents were placed in the control group. displays the accounting of the subjects through the phases of the study.
Sixty-eight residents (51 women and 17 men) were included in the final analysis with 35 (25 women and ten men) in the intervention group and 33 (26 women and seven men) in the control group. The average age at post-test was 84.3 (SD 8.6) years. There was no statistically significant difference between the intervention and control group in age, but women were older than men (85.7 versus 80.0 years, P < 0.05). The overall prevalence of UI was 89.7%.
Intervention program
The training program, which included physical activity and ADL training, was individually adjusted for each resident in the intervention group and lasted for 3 months. Personal treatment goals were elicited for each subject. Training in transfer and walking ability, balance, muscle strength, and endurance was offered to individuals and groups, while ADL training was performed when the resident needed help during meals, with personal care, or dressing. Each subject was asked to participate in creative and/or entertaining activities. All staff members on the wards were informed about each resident’s treatment goals and offered personal supervision regarding how to provide ‘just the right challenge’ to the residents. Two physiotherapists and two occupational therapists hired from outside the NH provided the intervention services. The control group received their usual care from the NH staff based on an individualized care plan.
Outcome measure
The outcome measure of the 24PWT was quantified prior to the intervention, immediately after the intervention and 3 months after the intervention. Due to insufficient data collection immediately after the intervention, only 3 months of post-intervention data was used in this analysis. No difference between the groups regarding this measure was found at baseline (P = 0.15). Furthermore, functional status related to toilet habits was registered, whether the resident was self-reliant, needed a reminder or some help, or was totally dependent on help at the beginning of the study.
Statistical methods
Descriptive statistics were used to describe the sample and the study measures. Univariate analysis of variance was used to compare differences between the intervention and control group at 3 months post-intervention, adjusting for baseline leakage, age, sex and functional status. The alpha level was set at P < 0.05. Analyses were also carried out separately among women and men. In the intervention group, multiple linear regression analysis was performed to identify predictors including age, gender, and functional status related to toilet habits dichotomized into need all help versus self-reliant or need some help for the outcome of change in leakage as measured by 24PWT. SPSS software (v 17.0; SPSS, Inc, Chicago, IL) was used for the analyses. Because this study drew on the participants and resources of a larger study, a priori power analysis was not performed.Citation9
Ethics
The study was approved by the Regional Ethics Committee and by the Norwegian Social Science Data Services. Participants gave their written consent to participate. In cases where residents did not have competence to consent, next of kin gave written consent on their behalf (58% of the included).
Results
shows the distribution of functional status related to toilet habits. Very few residents were self-reliant; 60 out of 68 residents were in need of some help with toileting.
Table 1 Functional status related to toilet habits and according to group among the 68 included nursing home patients
Mean leakage of urine at baseline and 3 months post-intervention is shown in . There was a decrease of leakage in the intervention group while the control group increased in leakage. This difference between groups was statistically significant after adjusting for baseline leakage, age, sex, and functional status. Analysis carried out separately among women and men showed the same tendency for both genders.
Table 2 Daily amount of leakage (grams) at baseline and 3-month post-intervention adjusted for baseline level, age, sex, and functional status
In the intervention group, the regression analysis showed that increasing age and low functional level (need all help) was statistically significant predictors for improvement after intervention, while being a woman significantly predicted poorer result ().
Table 3 Multiple linear regression analysis with change in leakage as dependent variable (intervention group only)
Discussion
This study confirms previous findings that in a NH population, UI increases over time. On the other hand, our results signal that this deterioration may be controlled or reversed following an individualized training program designed to improve overall ADL abilities and physical capacity.
Of the 17 residents excluded before randomization, eleven did not have the 24PWT data, and two 24PWTs, although provided, were not interpretable. An explanation for this could be that the 24PWT required a systematic effort from staff members through three shifts. The staff across the 24-hour time period had to understand why and how to complete the test and adhere to the process. An earlier study by Vinsnes et al found that the staff lack knowledge about UI in general and more specifically do not have the skills to investigate UI problems.Citation11 Even if the staff believe in the importance of UI assessment and the value of a treatment program, they often fail when it comes to implementation. Hence, lack of staff adherence may explain the uninterpretable or incomplete data at baseline. A combined bladder and drinking chart is a commonly used measure of bladder function, but due to a severe amount of missing data we decided to use the 24PWT as the main outcome measure. In addition, ten residents passed away during the study even though residents with life expectancy less than 6 months were excluded at the beginning. This underscores the fact that the subjects were frail older persons who needed help to perform some or all ADL. The increase of frailty over time is congruent with other studies.Citation4
In addition to the passing away of residents, there may be other resident and staff factors leading to withdrawal from the study. One reason for withdrawal might be that the training program required active involvement from the participants. Even if the residents had given their consent to participate, and the program was individually adjusted for each resident, it is reasonable to assume that the extra effort it took to participate may explain why some residents dropped out during the study period. However, this does not explain the drop-out in the control group. A more likely explanation is that the 24PWTs demanded too great an effort from staff members on the different day, evening, and night shifts. The incomplete data at baseline, the subsequent need to exclude these participants from our study, and the loss of subjects throughout the study do present a challenge to generalizability. Therefore, we draw our conclusions with caution.
As shown in , only a few residents were self-reliant in toileting. The larger Nordic study was designed to accept most residents in order to include a case-mix with a wide range of medical diagnoses and functional limitations.Citation9 The population in our smaller Norwegian UI study was frail according to the definition of frailty,Citation1 which is often the case for residents in NH.Citation7 Evidence-based guidelines for the assessment and treatment of UI in the frail elderly in NH are available.Citation6 The guidelines recommend active screening for UI along with screening for the person’s frailty.Citation1 The treatment guidelines recommend basing interventions on the resident’s preferences for UI care and treatment. Residents’ preferences for UI care are of great importance because even cognitively impaired persons can express treatment preferences and treatment satisfaction.Citation1
One of the primary findings of our study is that UI differences between groups increased. The 3-month post-intervention adjusted mean difference between groups according to amount of leakage was 191 g (P = 0.03). This result was statistically significant after adjusting for baseline level, age, sex, and functional status. The leakage increased in residents not receiving the experimental intervention of focused physical and ADL training, while UI in the training group showed improvement. This finding challenges us to consider the importance of overall physical functioning in the prevention of deteriorating UI in the frail elderly. In older people, it is documented that functional impairment is a predictor for UI, and that UI is a risk factor for reduced physical activity, functional decline, and frailty. This cause and effect cycle is complicated but this study demonstrates that intervention aimed at overall physical ability improvement may modestly improve UI, as UI may exacerbate functional decline.
For NH residents – given the decline of their medical, physical, and mental state over time – it might be unrealistic to expect a great UI improvement or cure. Another study underlined this when they found that UI increased over time, as did other comorbid conditions.Citation4 In light of this, the improvement in our study is noteworthy. However, it may be that our modest improvement in UI reflects the fact that the training program was aimed at all NH residents and may need to be tailored to have optimal impact on UI in frail elderly residents. A more goal-oriented physical and behavioral training program tailored for residents with UI may lead to a greater decrease of leakage. Overall, the general physical training program was effective in improving UI and, most notably, this improvement was achieved without using the standard behavioral interventions of prompted voiding, timed voiding, and habit training, which are the standard recommended UI treatments in persons with cognitive and physical impairments. FIT combines prompted voiding with low-intensity endurance and strength exercises. There is still a need to further investigate what works; the prompted voiding program or the exercise program, or how these programs can be translated into practice.Citation8
The regression analysis showed that increasing age was a predictor for improvement in the intervention group. This finding can be explained by the fact that it is the oldest ones who might have ‘gone downhill’ the most and accordingly have more to gain from physical activity. This was also the case for the residents who were the most physically dependent; they had more to gain from the training program. Being a woman predicted a poorer result. This result was surprising because we relied on the assumption that UI in women is easier to improve by physical training than UI in men. One explanation for this result could be that UI in women has had more attention in general, and therefore they have been more exposed to treatment.
Conclusion
Living in a NH is a risk factor for worsening UI. An individualized training program designed to improve ADL and physical capacity may prevent this worsening or reduce UI. Further studies are needed to evaluate the effect of a more tailored goal-oriented physical training program toward residents’ UI along with other behavioral interventions.Citation12 These trials should also include resident quality of life and cost outcomes.
Acknowledgments
The study was financed by the Norwegian Ministry of Health and Care Services, the Health Authorities of Mid Norway, supported by grants from Norwegian Nurses Organisation and was carried out as a study under Søbstad Teaching Nursing Home.
Disclosure
Other than those outlined in the Acknowledgments, the authors declare no conflicts of interest in this work.
References
- DuBeauCEKuchelGAJohnsonTPalmerMHWaggAIncontinence in the frail elderly: report from the 4th International Consultation on IncontinenceNeurourol Urodyn201029116517820025027
- OffermansMPWDu MoulinMFMTHamersJPHDassenTHalfensRJGPrevalence of urinary incontinence and associated risk factors in nursing home residents: A systematic reviewNeurourol Urodyn200928428829419191259
- DylewskiDAJamisonMGBorawskiKMShermanNDAmundsenCLWebsterGDA statistical comparison of pad numbers versus pad weights in the quantification of urinary incontinenceNeurourol Urodyn20072613717080415
- BoyingtonJEHowardDLCarter-EdwardsLDifferences in resident characteristics and prevalence of urinary incontinence in nursing homes in the southeastern United StatesNurs Res20075629710717356440
- Coll-PlanasLDenkingerMDNikolausTRelationship of urinary incontinence and late-life disability: Implications for clinical work and research in geriatricsZ Gerontol Geriatr200841428329018685805
- AbramsPAnderssonKEBirderLFourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinenceNeurourol Urodyn201029121324020025020
- LeungFWSchnelleJFUrinary and fecal incontinence in nursing home residentsGastroenterol Clin North Am2008373697707x18794004
- OuslanderJGGriffithsPCMcConnellERioloLKutnerMSchnelleJFunctional incidental training: a randomized, controlled, crossover trial in Veterans Affairs nursing homesJ Am Geriatr Soc20055371091110016108924
- FrandinKBorellLGronstedtHA Nordic multi-center study on physical and daily activities for residents in nursing home settings: design of a randomized, controlled trialAging Clin Exp Res2009214–531432219959920
- VinsnesAGHelbostadJLNyrønningSGranboRSeimAA general physical training programme for residents in nursing homes and the effect on urinary incontinence: a randomized controlled trialNeurourol Urodyn2010296852853
- VinsnesAGHarklessGENyrønningSUnit-based intervention to improve urinary incontinence in frail elderlyVard Nord Utveckl Forsk20072735356
- PalmerMHUrinary incontinence quality improvement in nursing homes: where have we been? Where are we going?Urol Nurs200828643944445319241782