Abstract
Benign prostatic hyperplasia (BPH) is a common health condition in aging men resulting in lower urinary tract symptoms (LUTS) and low quality of life (QoL). We aimed to review studies on laser enucleation of the prostate (LEP) due to LUTS in elderly patients (>65 years) comparing different age groups, particularly considering functional outcomes, safety, and perioperative complications. A comprehensive search was conducted using the PubMed-MEDLINE, Web of Science, Wiley Online Library and Cochrane Library databases over the last 10 years until 7 October 2021 with the following search terms solely or in combination: “laser enucleation”, “prostate”, “laser prostatectomy”, “aging”, “elderly patients”, “older patients” and “age”. We identified 12 articles for inclusion in our analysis. Five studies focussed mainly on holmium laser enucleation of the prostate (HoLEP), one compared HoLEP to other laser prostatectomy procedures, two studies examined thulium laser enucleation of the prostate (ThuLEP), and two studies focused on GreenLight laser, one study focussed on potassium-titanyl-phosphate (KTP) laser, and another study compared laser prostatectomy to transurethral resection of the prostate (TURP). These studies showed that LEP improved IPSS, Qmax and QoL compared to baseline regardless of age; no significant difference was reported among age groups. Although ASA scores and anticoagulation/antiplatelet therapy rates are higher in elderly patients, studies revealed no significant difference in perioperative complication rates between age groups. Laser enucleation of the prostate is an effective and safe procedure in elderly patients, resulting in good functional outcomes, low morbidity, and few perioperative complications.
Introduction
Benign prostatic hyperplasia (BPH) is a common health condition in aging men resulting in lower urinary tract symptoms (LUTS) and low quality of life (QoL).Citation1 Studies on BPH epidemiology from 25 countries show a combined prevalence of 26.2%, with its prevalence rising with age.Citation2 Transurethral resection of the prostate (TURP) and open prostatectomy (OP) have been considered for decades the surgical standard for treating BPH.Citation3 Yet TURP and OP are associated with intraoperative and postoperative complications such as bleeding, clot retention requiring intervention, genitourinary infections, fluid absorption, and TUR syndrome.Citation3–Citation5 Therefore, it is possible to deteriorate the quality of life after these procedures, especially in the elderly and comorbid patients. Elderly patients may be taking anticoagulants for cardiovascular disease and suffer from comorbidities such as hypertension, renal insufficiency or diabetes mellitus; they therefore require procedures less invasive than TURP and OP.Citation6
Laser enucleation of the prostate (LEP) is now a frequent and widespread alternative, minimally invasive approach to TURP and OP in the surgical treatment of BPH.Citation7,Citation8 Holmium: YAG, Thulium, potassium-titanyl-phosphate (KTP), lithium triborate (LBO) laser, GreenLight and Diode laser are the laser types now used in surgically treating symptomatic BPH.Citation7 There is evidence that LEP is similarly safe and efficacious as TURP.Citation7,Citation9,Citation10 In addition, LEP has also been shown to be associated with increased QoL.Citation11,Citation12 However, studies on LEP in elderly patients are scarce, and there is no collective evaluation study providing efficacy and safety results. We therefore saw the need to review the safety and efficacy of LEP according to age groups and in the elderly population. We aimed to discuss LEP due to LUTS in elderly patients (> 65 years) comparing different age groups, especially considering functional outcomes and safety.
Materials and Methods
Literature Search
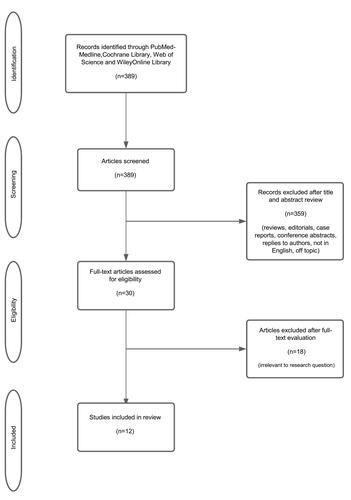
A comprehensive search was conducted using the PubMed-MEDLINE, Web of Science, Wiley Online Library and Cochrane Library databases over the last 10 years until 7 October 2021 with the following search terms solely or in combination: “laser enucleation”, “prostate”, “laser prostatectomy”, “aging”, “elderly patients”, “older patients” and “age”. After retrieving the titles and abstracts of selected articles, the full texts of related articles were screened. The article selection process is shown in . The PICOS: Population (P), Intervention (I), Comparison (C), Outcomes (O), and Study design (S) approach was used to determine eligibility criteria.Citation13 We thus selected studies in which BPH patients (P) underwent laser enucleation of the prostate and/or other laser prostatectomy procedures (I) specified various age groups were compared (including >65 years) (C), to assess functional outcomes, comorbidities, perioperative complications, and safety (O) in prospective or retrospective studies (S).
We excluded studies unrelated to laser enucleation of the prostate, or without objectives or outcomes related to mainly age, those that did not perform age classification and/or failed to specify a specific age cut-off regarding surgical outcome, or were not written in English, as well as case reports, review articles, editorials, reply to authors, and conference abstracts.
Data Extraction
Articles relevant to our subject of interest were retrieved and evaluated independently by two authors (M.Y. and J.E.). Authors and date of study, study design, age stratifications, number of patients included, mean age, preoperative prostate volume (cc), total serum PSA (ng/mL), International Prostate Symptom Score (IPSS) (a questionnaire consisting of seven symptom questions and a global QoL question for LUTS diagnosis and treatment follow-up), maximum urinary flow rate (Qmax) (a basic noninvasive urodynamic test), quality of life (QoL) (a subjective concept determined by various surveys), length of hospital stay (LOS), operative time, American Society of Anesthesiology (ASA) scores (a classification system in which patients are evaluated according to the risk of anaesthesia before performing surgery), antiplatelet/anticoagulation (AP/AC) therapy status`, comorbidities, complications according to the Clavien- Dindo classification (a system for grading the severity of surgical complications) were recorded. Descriptive statistics were used for basic data, and a narrative synthesis was created.
Results
A total of 389 articles were identified through our search query. Overall, 359 publications were excluded after reviewing the title and abstract for these reasons: not related to laser enucleation of the prostate (n=28), objective or outcome not related to mainly age (n=222), not written in English (n=16), case reports (n=13), review articles (n=33), conference abstracts (n=31), editorials (n=8), reply to the authors (n=8). After full-text evaluation, we excluded 18 more articles that did not classify by age and/or failed to specify a specific age cut-off regarding surgical outcomes. The remaining 12 articles were ultimately incorporated in our review. presents a summary of baseline characteristics, perioperative data, and the main findings of the studies included in our review. Eight of them were retrospectiveCitation14–Citation21 and 4 prospective.Citation6,Citation22–Citation24 Five studies focussed mainly on Holmium laser enucleation of the prostate (HoLEP).Citation6,Citation17,Citation20–Citation22 One study focussed on comparing HoLEP to other laser prostatectomy procedures,Citation16 two studies examined Thulium laser enucleation of the prostate (ThuLEP) in more detail,Citation14,Citation18 and two other studies focussed on the GreenLight XPS 180-W laser procedure,Citation19,Citation23 one focussed on potassium-titanyl-phosphate (KTP) laserCitation24 and another compared laser prostatectomy to transurethral resection of the prostate (TURP).Citation15
Table 1 Summary of Demographics, Baseline Characteristics, and Perioperative Data and the Main Findings of Studies
Perioperative and Urinary Outcomes
Studies Comparing Men Aged ≥75 Years vs < 75 Years
Castellani et al compared the outcomes of ThuLEP in men aged ≥75 years vs < 75 years in a retrospective study including 412 men.Citation14 They observed no statistically significant difference in median operation times and LOS (p=0.452, p = 0.547; respectively) between groups. There were no differences in IPSS, Qmax, QoL, or reoperation rate between groups at the 1-year follow up.Citation14
Majumdar et al investigated prospectively the efficacy and safety of laser photoselective vaporization (LVP) in groups aged ≥75 (n=49) and <75 years (n=153).Citation24 In contrast to Castellani et al, the ≥75 age group’s median LOS was significantly longer (1 day vs 0 days; P = 0.001). In the 1st month follow-up, there was a significant improvement in median IPSS in both age groups (23 to 10 years in the younger group and from 19 to 16 in the elderly group; P < 0.001 and P = 0.01, respectively), while the elderly group’s IPSS was significantly higher than the younger group’s (16 vs 10; P = 0.01). However, no significant difference was observed between the groups in median IPSS at the postoperative 3rd-, 6th- and 9th-month follow-ups.
Anan et al prospectively compared perioperative outcomes, complications and the King’s Health Questionnaire (KHQ scores) of 100 patients aged ≥75 years and <75 years after HoLEP.Citation22 KHQ is a special internationally validated QoL questionnaire containing the following 9 categories: health perceptions, physical limitations, role limitations, impact on life, social limitations, personal relationships, emotions, sleep/energy, and incontinence status. Scores in each category range from 0 to 100, with lower scores indicating better QoL. No significant differences were detected in IPSS, QoL, Qmax, International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF-Score), operative times, LOS, and urinary incontinence rates between the groups 6 months after HoLEP. Regarding the KHQ categories, general health perceptions, emotions, impact of life and sleep/energy 1, 3 and 6 months after HoLEP; role limitations, physical limitations, and social limitations 3 and 6 months after HoLEP; and personal relationships and incontinence severity 6 months after HoLEP were better in both age groups than at baseline levels (P<0.05).Citation22 There were no significant differences between groups.
Bouhadana et al compared the safety and durability of TURP (n= 12262) and laser prostatectomy (LP) (n= 17544) in men aged ≥ 75 and multi-morbid patients.Citation15 However, their study provides no results on the functional outcomes of surgical procedures.
Studies Comparing Different Age Groups
Piao et al compared outcomes in groups aged 50–59 (n=44), 60–69 (n=253), 70–79 (n=244), and ≥80 years (n=38). Patients aged ≥80 years revealed the longest LOS (group A, 2.3±0.7 days; group B, 2.3±0.7 days vs group C, 2.4±0.7 days; group D, 2.9±1.8 days, p=0.001).Citation6 Functional outcomes were significantly better than conditions at baseline, and there were no differences in IPSS, QoL, Qmax, and postvoid residual volume (PVR) among these groups at the 6-month follow-up (p>0.05).Citation6 Tamalunas et al retrospectively analysed 487 patients who underwent HoLEP.Citation21 Their study cohort was divided into 3 groups according to age (<70 years, 70–79 years and ≥80 years). At the 1-month follow-up, all groups revealed significantly higher median IPSS scores (p<0.001). Significant improvement was identified in QoL and Qmax, but without any differences between age groups (p=0.63 and p=0.467, respectively).Citation21 Mmeje et al assessed outcomes after HoLEP in 311 patients according to age groups (22 patients aged 50–59 years, 91 aged 60–69 years, 153 aged 70–79 years, and 45 ≥80 years).Citation20 They reported no significant difference in terms of IPSS, Qmax, PVR and LOS between groups at their 1-year follow-up.Citation20
Gu et al prospectively evaluated the efficacy and safety of GreenLight HPSTM (High Performance System) laser photoselective vaporisation prostatectomy (PVP) in male groups aged <70 (n=93) and ≥70 (n=71).Citation23 They observed significant improvements in the American Urological Association Symptom Score (AUASS), QoL, Qmax and PVR compared to baseline values at the 3rd-, 6th-, 12th-, and 36th-month follow-ups in both age groups (p< 0.05). They reported no significant difference between age groups in those parameters.
Studies Including Men Aged ≥ 80 Years
Gild et al performed a retrospective analysis including of 1816 men's perioperative outcomes after HoLEP.Citation17 Their study emphasises that the Qmax improvement was more pronounced in men aged under 60 years than in those over 80 [12 (IQR: 3.5–18) vs 18 mL/s (IQR: 9.0–27)], whereas the improvement in PVR was more pronounced in men aged 80 years and older than those <60 years [100 mL (IQR: 34–233) vs 85 mL (IQR: 35–180)]. Prolonged catheterisation was not associated with patient age.Citation17 Elshal et al compared the outcomes of 264 octogenarians (>80 years) who underwent various prostate laser surgeries [HoLEP, HoLAP (holmium laser ablation of the prostate), Hol-TUIP (holmium laser transurethral incision of the prostate) and PVP (photoselective vaporization].Citation16 Significant improvements in IPSS and QoL scores and improvements in Qmax and PVR were reported in all groups in the first year.Citation16 Liu et al retrospectively investigated the safety and effectiveness of GreenLight XPS 180-W laser photoselective vaporisation of the prostate (PVP) in 150 elderly patients (>80 years).Citation19 IPSS, QOL, Qmax, and PVR scores rose significantly after surgery at months 3, 6, and 12 when compared to baseline.Citation19 Hou et al retrospectively analysed the results of 303 patients who underwent thulium vapoenucleation of the prostate (ThuVEP).Citation18 The older group’s (age>80) Qmax did not differ significantly from the younger groups’ (p=0.103).Citation18
Comorbidities
illustrates ASA scores, AP/AC treatment status and comorbidities sorted by age groups of patients included in the studies.
Table 2 ASA Scores, AP/AC Treatment Status and Comorbidities According to Age Groups of the Patients Included in the Studies
Castellani et al reported that patients ≥75 years underwent AP/AC therapy more frequently than <75-year-old patients (20.2% vs 7.1%; p< 0.05). Age groups ≥75 years had ASA scores 3–4 more frequently than age groups <75 (57.4% vs 17.0%; p< 0.05).Citation14 In the study by Majumdar et al, heart disease, haematuria and use of anticoagulants were more common in ≥75 age group than their younger group (p=0.03, p=0.05, p=0.002).Citation24 Anan et al reported that comorbidities were more likely in groups aged ≥75 years.Citation22 There was no significant difference between groups in AC therapy, (21% vs 34%; p= 0.16). There was no significant difference in ASA scores in the study by Gu et al, (2.3 ± 0.6 vs 2.4 ± 0.7; p=0.326) or in anticoagulation use (36.6% vs 26.8%; p=0.238) in <70 and ≥70 age groups.Citation23
On the other hand, Tamalunas et al and Mmeje et al demonstrated that ≥ 80-year-old patients were more likely to undergo AP/AC therapy than younger age groups (39.1% and 53.3%, respectively).Citation20,Citation21 They found that ASA ≥3 was higher in ≥80-year-old patients than in younger patients (≥80: 65.2%; <70: 24.9%; 70–79: 28.7%).Citation21 Mmeje et al reported that >80-year-olds had the highest ASA scores among age groups (50–59: n=2.18; 60–69: n=2.3; 70–79: n=2.46; >80: n=2.6).Citation20 Piao et al also showed that patients ≥80 years had significantly higher ASA scores (p=0.006) and higher anticoagulation use (p=0.008) prior to surgery.Citation6 Liu et al reported that most patients over 80 years old received an ASA score of 2 or 3 (45.4% and 44%). The patients included in their study probably had cardiovascular disease (61.4%), followed by hypertension (43.4%).Citation19
Complications
illustrates perioperative complications and adverse events according to Clavien- Dindo classification of the patients included in the study stratified by age.
Table 3 Age Groups and Complications According to Clavien-Dindo Classification of the Patients Included in the Study
Castellani et al identified comparable incidences of complications according to Clavien- Dindo classification between age groups (≥75 vs <75 years) (p= 0.743). The vast majority had no complications (85.9%), with no differences between age groups (82.5% vs 89.3%) for complications such as urethral stenosis and bladder-neck contracture.Citation14 They also found that urinary incontinence (UI) rates were similar in patients ≥75 and <75 years in their 1-year follow-up (5.8% vs 4.8%, respectively).
The study of Majumdar et al reported that the most common perioperative complications in the ≥75 age group were dysuria (10.2%), urinary tract infection (10.2%), and haematuria (10.2%).Citation24 They detected no significant difference between age groups in perioperative complications.
Anan et al reported postoperative fever at similar rates in their groups ≥75 years and <75 years (3% vs 2%; p=1.00).Citation22 They observed a higher rate of UI in the ≥75 years group at the postoperative 6th-month follow-up than in the younger group, but the difference was not significant (5% vs 2%, p=0.56).
Bouhadana et al found that TURP was associated with higher rates of 90-day hospital readmission and probability of emergency room visits than laser prostatectomy in their patients aged ≥75 (OR 1.07, %95 CI).Citation15 Post-TURP haematuria was also more likely (OR 1.28, %95 CI 1.03–1.59). However, TURP was also found to reduce the risk of reoperation by 20% at 6 months postoperatively or later (%95 CI 0.71–0.91).Citation15
Gu et al reported that the most common 1st-month postoperative complications were haematuria (lasting under 7 days) (64.8%), de novo retrograde ejaculation (21.2%), urinary tract infection (4.2%), and transient irritative voiding symptoms (4.2%) in the ≥70 years group after Greenlight PVP.Citation23 They detected no significant difference between age groups in perioperative complications, nor was any postoperative UI observed in either age group. Bladder-neck contracture and urethral stricture, which are late complications after the postoperative 1st month, were not observed in either group.
Piao et al reported no significant difference between age groups (50–59, 60–69, 70–79 and ≥80 years) in terms of intraoperative, immediate postoperative (recatheterisation, blood transfusion, urinary tract infection) and late postoperative complications (urethral stricture and bladder-neck contracture). They found no significant difference between age groups in terms of transient stress UI (p=0.180).Citation6 Similarly, Mmeje et al reported no significant difference in 30-day complications in Clavien- Dindo grades among groups aged 50–59, 60–69, 70–79, and 80 years.Citation20 Continence rates were similar between age groups at their 1-year follow-up (100, 95, 93 and 88% for groups, respectively; P = 0.192). Tamalunas et al reported no significant difference between age groups (<70, 70–79, ≥80 years) in perioperative complications- Clavien- Dindo grade ≥II- (indwelling suprapubic catheter, persistent haematuria, urethral flap, right ureteral ostium injury, aspiration pneumonia) (p = 0.176).Citation21 On the other hand, Gild et al reported that patients aged ≥80 suffered Clavien- Dindo grade ≥3b complications more frequently (requiring surgical, endoscopic or radiological intervention under general anaesthesia) than their other age groups (≤60, 60–69, 70–79, ≥80 years), as well as a significant difference between groups in Clavien- Dindo grade ≥ 3b complications (1.5, 1.9, 3.9 and 7.1%; respectively, p= 0.02).Citation17
Discussion
Urinary Outcomes
In recent years, LEP has come to the fore as one of the most popular surgical treatments for BPH.Citation25 HoLEP in particular, a minimally-invasive alternative to TURP and open prostatectomy, has contributed substantially to LEP’s worldwide popularity.Citation26,Citation27 The studies included in this review support the efficacy and safety of HoLEP. Moreover, different surgical approaches using holmium laser have also been shown to improve voiding function in elderly patient groups. Elshal et al showed that HoLEP, HoLAP and Hol-TUIP all enable good functional outcomes in elderly patients.Citation16 Both the Holmium laser and other laser types such as Thulium or Greenlight improved functional urinary parameters compared to baseline in elderly patients. Noteworthy, studies show improved functional outcomes at 1,Citation21 3,Citation6,Citation19 6,Citation6,Citation22 and 12 monthsCitation14,Citation16,Citation19,Citation20 follow-up. Although these follow-up periods are relatively short, laser enucleation of the prostate fulfills the functional expectations of elderly patients.
One of the most challenging potential complications after LEP surgery is UI. Krambeck et al included 1000 patients who underwent HoLEP and reported the postoperative incontinence rate < 5%.Citation28 Elderly patients may have weaker sphincteric tissue than younger patients, which may lead to greater susceptibility to damage caused by straining the tissue. In addition, an overactive bladder (39–61%) and detrusor instability (48%) are common in elderly patients.Citation29 Studies on the effect of age on postoperative incontinence after HoLEP have been inconsistent. Houssin et al showed that age was significantly associated with UI after HoLEP.Citation29 But in another study, Elmansy et al showed that age is not associated with postoperative stress incontinence after HoLEP.Citation30 The studies we reviewed reveal no significant difference in postoperative UI between age groups. Note that as most of the studies we reviewed provide no preoperative UI rates that can cause bias. Liu et al reported that no UI was observed in any patient in the 3rd month aged >80 years after Greenlight PVP.Citation19 Similarly, Gu et al found no difference in postoperative UI after PVP between age groups <70 and ≥70.Citation23 However, Mmeje et al noted that men aged ≥80 years suffered from the highest rates of incontinence (12%) at the 1-year follow-up after HoLEP. Furthermore, they reported that patients aged >80 years presented a 20% rate of urinary leakage before HoLEP. The difference between these two studies may be due to the different laser types. Another possible explanation is that the higher rate of incontinence after HoLEP in elderly patients may be due to the age-related, radical removal of enlarged prostate glands, which may have adapted and served as part of the men's continence mechanisms.
QoL
LUTS associated with BPH have a negative impact on the QoL of patients.Citation31 The studies we included show that the postoperative QoL scores of patients rose significantly compared to baseline, but also no significant difference between age groups in terms of QoL scores. The studies indicate that laser enucleation of the prostate increases the QoL of patients over 75 and 80 years of age, with no significant difference from younger patient groups.Citation6,Citation14,Citation16,Citation19,Citation21,Citation22 Only three studies failed to provide data on postoperative QoL changes in patients.Citation17,Citation18,Citation20 Note that most of the studies failed to mention which QoL scale they had used. Only one study used King’s Health Questionnaire (KHQ scores).Citation22 Nevertheless, according to the studies’ outcomes, LEP preserves QoL in elderly patients.
Complications
The two main challenges in elderly patients undergoing surgery are firstly, the acute morbidity events associated with the procedure and, secondly, maintaining quality of life (QOL) without chronic morbidity.Citation16 Several studies provide evidence for the safety and low perioperative morbidity of laser enucleation of the prostate.Citation32,Citation33
We found that in those studies that assessed complications according to age groups, they observed no significant differences between age groups.Citation6,Citation14,Citation20–Citation22 However, Gild et al found that Clavien- Dindo Grade >3b complications were significantly higher in the ≥80-years patient group than in younger age groups.Citation17 The 8.2% perioperative blood transfusion rate of patients aged >80 was significantly higher than those in other age groups (1.3% vs 2.7% vs 8.2%; p< 0.001).Citation17 We emphasise that unlike other studies, Gild et al did not classify ASA scores or AC/AP therapy according to age. We have no information on ASA scores or AC/AP therapy rates in their elderly group. Their elderly group’s ASA scores and AC/AP therapy rates may have been higher, which could have caused the significantly higher incidence of complications in that elderly group. On the other hand, although there was no difference in AC use between age groups <70 and ≥70; Gu et al found that postoperative haematuria was more common in the ≥70 age group.
The other studies we reviewed did not compare complication rates among groups; they only provided the complications and/or rates in men aged ≥80 years.Citation16,Citation18,Citation19 Whereas Elshal et al reported 19.6% perioperative complications in patients ≥80 years, Liu et al reported short- and long-term postoperative complication rates were 29.8%, and 13.3%, respectively, in the same age group. According to studies investigating patients over the age of 80, the low rates of perioperative and postoperative complications they report are encouraging.
Comorbidities
It is not surprising that older men reveal higher ASA scores. Studies in this review reported an ASA score of 2 and above in patients aged >75 and >80 years. This fact is evidence that much older patients carry a substantial risk, as well as the importance of choosing a safe surgical method. Moreover, AC/AP treatment is common in the BPH age group. AC/AP treatment may cause significant complications in older patients undergoing surgery. Studies show that LEP in elderly patients taking AP/AC is as safe as in younger populations. Elshal et al showed that ongoing anticoagulation therapy in the patient group >80 years old is not an independent predictor of perioperative morbidity in patients undergoing HoLEP (OR, 1.03; 95% CI, 1.07–3.9;P= 0.2).Citation16 Similarly, Liu et al detected no significant difference in postoperative haematuria in patients >80 years with and without oral anticoagulant use who underwent PVP (9.1% vs 6.6%, p=0.6).Citation19 However, those studies (see Complications) report a difference in perioperative complications.This difference observed among the same age groups is attributable to the fact that Lui et al study patients had ASA scores 3 and higher, and suffered more often from cardiovascular diseases.Citation16,Citation19 Gild et al found that taking low-dose acetylsalicylic acid (OR: 1.5, 95%; CI:1.0–2.2, p=0.015), or oral anticoagulation (OR: 2.3, 95% CI: 1.2–4.0, p=0.022), as well as low-molecular-weight heparin (OR: 2.2, 95% CI: 1.4–3.6, p=0.037) were independently associated with prolonged catheterisation in patients who underwent HoLEP.Citation17 Such differences between studies may be due to their diverging pre- and post-surgical AC/AP regimens.
Various age groups have different impacts on the surgical outcomes, perioperative complications and safety. The main reasons can be assumed as higher ASA score, various comorbidities, use of AC/AP, advanced age-related sphincteric insufficiency and therefore the risk of perioperative and postoperative complications are common. In general, it is expected that the surgical outcome is worse and the risks are higher in elderly patients. However, the studies included in our review revealed that LEP is an effective and safe method in patients of various age groups. To the best of our knowledge, this is the first review focussing on LEP procedures in elderly patients. However, our review has certain limitations. Firstly, most of the studies were of retrospective nature, revealed large differences in patient numbers, varying study designs; all these factors make our data heterogeneous. Secondly, because of the paucity of published studies investigating the effect of laser enucleation of the prostate together with age-stratification, the number of studies included in the review is small.
Conclusion
Laser enucleation of the prostate due to LUTS is an efficient and safe procedure in elderly patients, resulting in improved functional outcomes, low morbidity, and few perioperative complications. LEP procedures can be also offered to patients over 65 years of age suffering LUTS associated with BPH. Future studies with more patients will enable us to more clearly demonstrate the efficacy and safety of LEP in elderly patients.
Ethics
This research did not involve human subjects or animals. As this is a review of the literature, no ethics approval was necessary.
Author Contributions
M.Y., J.E. and A.M. designed the study. M.Y. and J.E. wrote the manuscript. M.Y., J.E., R.S.I., C.G. and A.M. performed the analysis and interpretation of data as well as the manuscript revision. C.G. and A.M. reviewed the manuscript. A.M. supervised the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Prof. Dr. Christian Gratzke is advisor for Astellas Pharma GmbH, DE, Ipsen Pharma GmbH, DE, Steba Biotech S.A., LUX, Bayer Pharma, DE, Olympus Winter & Ibe GmbH, DE, Medi-Tate Ltd., IL, MSD, DE, Astra-Zeneca, UK and Roche, CH. He receives speaker fees from Amgen, USA, Astellas Pharma GmbH, DE, Ipsen Pharma GmbH, DE, Janssen-Cilag GmbH, BEL, Bayer Pharma, DE, Takeda Pharmaceuticals, JPN and medac GmbH, DE. A. Miernik receives research funding from the German Federal Ministry of Education and Research, Berlin (D). He receives support for his travel activities from the European Society of Urology, Arnhem (NL), and German Society of Urology, Düsseldorf (D). A. Miernik is also a consultant for: KLS Martin, Tuttlingen (D), Avateramedical, Jena (D), LISA LaserProducts GmbH, Katlenburg-Lindau (D), Schoelly fiber optics GmbH, Denzlingen (D), Dornier MedTech Laser GmbH (D), Medi-Tate Ltd. (IL, USA) and B. Braun New Ventures GmbH, Freiburg (D). A. Miernik is speaker for the companies Richard Wolf GmbH (D) and Boston Scientific (USA). He also served as a reviewer for the Ludwig Boltzmann Gesellschaft, Wien (A). In addition, Prof. Dr. Arkadiusz Miernik has a patent WO2014173468A1 licensed to Purenum GmbH, German start-up, a patent EP2988681A1 licensed to Purenum GmbH, German start-up, a patent WO2015082372A1 pending; a patent WO2017207361A1 pending; a patent DE102019220537A1 pending; a patent DE102019134352A1 pending; a patent DE102015003560B3 issued; a patent WO2021005060A1 pending. M. Yilmaz, J. Esser and Rodrigo Suarez have no conflicts of interest to declare.
Additional information
Funding
References
- Gratzke C, Bachmann A, Descazeaud A, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67(6):1099–1109. doi:10.1016/j.eururo.2014.12.038
- Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep. 2017;7(1):7984. doi:10.1038/s41598-017-06628-8
- Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64(1):118–140. doi:10.1016/j.eururo.2013.03.004
- Reich O, Gratzke C, Bachmann A, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180(1):246–249. doi:10.1016/j.juro.2008.03.058
- Shah AA, Gahan JC, Sorokin I. Comparison of robot-assisted versus open simple prostatectomy for benign prostatic hyperplasia. Curr Urol Rep. 2018;19(9):71. doi:10.1007/s11934-018-0820-1
- Piao S, Choo MS, Kim M, Jeon HJ, Oh SJ. Holmium laser enucleation of the prostate is safe for patients above 80 years: a prospective study. Int Neurourol J. 2016;20(2):143–150. doi:10.5213/inj.1630478.239
- Nair SM, Pimentel MA, Gilling PJ. A review of laser treatment for symptomatic BPH (Benign Prostatic Hyperplasia). Curr Urol Rep. 2016;17(6):45. doi:10.1007/s11934-016-0603-5
- Rieken M, Ebinger Mundorff N, Bonkat G, Wyler S, Bachmann A. Complications of laser prostatectomy: a review of recent data. World J Urol. 2010;28(1):53–62. doi:10.1007/s00345-009-0504-z
- Xiao KW, Zhou L, He Q, et al. Enucleation of the prostate for benign prostatic hyperplasia thulium laser versus holmium laser: a systematic review and meta-analysis. Lasers Med Sci. 2019;34(4):815–826. doi:10.1007/s10103-018-02697-x
- Vincent MW, Gilling PJ. HoLEP has come of age. World J Urol. 2015;33(4):487–493. doi:10.1007/s00345-014-1443-x
- Alkan I, Ozveri H, Akin Y, Ipekci T, Alican Y. Holmium laser enucleation of the prostate: surgical, functional, and quality-of-life outcomes upon extended follow-up. Int Braz J Urol. 2016;42(2):293–301. doi:10.1590/s1677-5538.ibju.2014.0561
- Sun I, Yoo S, Park J, et al. Quality of life after photo-selective vaporization and holmium-laser enucleation of the prostate: 5-year outcomes. Sci Rep. 2019;9(1):8261. doi:10.1038/s41598-019-44686-2
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi:10.1371/journal.pmed.1000100
- Castellani D, Pirola GM, Gasparri L, et al. Are outcomes of thulium laser enucleation of the prostate different in men aged 75 and over? A propensity score analysis. Urology. 2019;132:170–176. doi:10.1016/j.urology.2019.06.025
- Bouhadana D, Nguyen DD, Zhang X, et al. Safety and efficacy of TURP vs. laser prostatectomy for the treatment of benign prostatic hyperplasia in multi-morbid and elderly individuals aged ≥ 75. World J Urol. 2021. doi:10.1007/s00345-021-03779-2
- Elshal AM, Elmansy HM, Elhilali MM. Transurethral laser surgery for benign prostate hyperplasia in octogenarians: safety and outcomes. Urology. 2013;81(3):634–639. doi:10.1016/j.urology.2012.11.042
- Gild P, Lenke L, Pompe RS, et al. Assessing the outcome of holmium laser enucleation of the prostate by age, prostate volume, and a history of blood thinning agents: report from a single-center series of >1800 consecutive cases. J Endourol. 2021;35:639–646. doi:10.1089/end.2020.0605
- Hou C-M, Chen C-L, Lin Y-H, Yang P-S, Chang P-L, Tsui K-H. Treatment outcomes of benign prostate hyperplasia by thulium vapoenucleation of the prostate in aging men. Urol Sci. 2016;27(4):230–233. doi:10.1016/j.urols.2016.03.006
- Liu X, Yuan F, Xue Md B. GreenLight XPS 180-W laser vaporization of prostate in high-risk elderly patients: a single-center experience. Photobiomodul Photomed Laser Surg. 2020;38(6):380–384. doi:10.1089/photob.2019.4735
- Mmeje CO, Nunez-Nateras R, Warner JN, Humphreys MR. Age-stratified outcomes of holmium laser enucleation of the prostate. BJU Int. 2013;112(7):982–989. doi:10.1111/bju.12063
- Tamalunas A, Westhofen T, Schott M, et al. The clinical value of holmium laser enucleation of the prostate in octogenarians. Low Urin Tract Symptoms. 2021;13(2):279–285. doi:10.1111/luts.12366
- Anan G, Iwamura H, Mikami J, et al. Efficacy and safety of holmium laser enucleation of the prostate for elderly patients: surgical outcomes and King’s Health Questionnaire. Transl Androl Urol. 2021;10(2):775–784. doi:10.21037/tau-20-1309
- Gu X, Strom K, Spaliviero M, Wong C. Does age affect the efficacy and safety of GreenLight HPS laser photoselective vaporization prostatectomy? Aging Male. 2012;15(1):63–67. doi:10.3109/13685538.2011.632452
- Majumdar R, Mirheydar HS, Palazzi KL, Lakin CM, Albo ME, Parsons JK. Prostate laser vaporization is safe and effective in elderly men. Urol Ann. 2015;7(1):36–40. doi:10.4103/0974-7796.148595
- Herrmann TRW, Gravas S, de la Rosette JJ, Wolters M, Anastasiadis AG, Giannakis I. Lasers in transurethral enucleation of the prostate-do we really need them. J Clin Med. 2020;9(5):1412. doi:10.3390/jcm9051412
- Elzayat EA, Habib EI, Elhilali MM. Holmium laser enucleation of the prostate: a size-independent new “gold standard”. Urology. 2005;66(5 Suppl):108–113. doi:10.1016/j.urology.2005.06.006
- Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53(1):160–166. doi:10.1016/j.eururo.2007.08.036
- Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol. 2013;189(1Suppl):S141–145. doi:10.1016/j.juro.2012.11.027
- Houssin V, Olivier J, Brenier M, et al. Predictive factors of urinary incontinence after holmium laser enucleation of the prostate: a multicentric evaluation. World J Urol. 2021;39(1):143–148. doi:10.1007/s00345-020-03169-0
- Elmansy HM, Kotb A, Elhilali MM. Is there a way to predict stress urinary incontinence after holmium laser enucleation of the prostate? J Urol. 2011;186(5):1977–1981. doi:10.1016/j.juro.2011.06.063
- Giuliano F. Lower urinary tract symptoms and sexual dysfunction: a common approach. BJU Int. 2008;101(Suppl 3):22–26. doi:10.1111/j.1464-410X.2008.07494.x
- Shah HN, Mahajan AP, Hegde SS, Bansal MB. Peri-operative complications of holmium laser enucleation of the prostate: experience in the first 280 patients, and a review of literature. BJU Int. 2007;100(1):94–101. doi:10.1111/j.1464-410X.2007.06867.x
- Vavassori I, Valenti S, Naspro R, et al. Three-year outcome following holmium laser enucleation of the prostate combined with mechanical morcellation in 330 consecutive patients. Eur Urol. 2008;53(3):599–604. doi:10.1016/j.eururo.2007.10.059