Abstract
Introduction
Lifestyle-integrated Functional Exercise (LiFE) is an effective, individually delivered fall prevention program but comes with substantial resource requirements; hence, a group-format was developed (gLiFE). This study 1) evaluates the program content of two different LiFE formats (group vs individual) and 2) examines the relationship between predictors of training response (dose) and improvements in balance, strength, and physical activity (PA) (response).
Material and Methods
The analysis included n = 252 (gLiFE = 126, LiFE = 126) community-dwelling older adults (78.6±5.2 years). LiFE was administered in seven sessions either in a group (gLiFE: 8–12 participants) or individually at home (LiFE). Questionnaire-based, descriptive content evaluation (frequency distributions) included reported frequency of practice (days/week, number of activities), activity preferences, safety, intensity, integrability of activities, and acceptance after 6 months of LiFE practice. Predictors (ie, dose [reported frequency and intensity], safety, and integrability of activities) for improvements in balance, strength, and PA were analyzed using radar charts.
Results
In both formats, 11.2 activities were practiced on average. Strength activities were more frequently selected than balance. Content evaluation showed some marginal advantages for the LiFE participants for selected aspects. The effects on balance, strength, and PA were nearly similar in both groups. Participants who performed balance activities more frequently (≥4 days/week) scored better in the balance and PA domain. Those who performed strength activities more frequently (≥4 days/week) performed better in all three outcomes. Higher perceived safety was associated with better performance. Those who reported activities as “not physically exhausting” performed better in all three outcomes. Those who found activities easily integrable into daily routines scored higher in the balance and strength domain.
Discussion and Conclusion
Overall, both program formats are comparable with respect to content evaluation and effects. Participants need to perceive the activities as safe, not exhausting, and should practice ≥4 days/week to generate a high benefit from the intervention.
Trial Registration
ClinicalTrials.gov, NCT03462654. Registered on 12 March 2018.
Introduction
Deterioration in motor capacity and performance accelerates from the seventh decade of life.Citation1 This can lead to reduced mobility, illness, limited independence, increasing need for care and higher mortality.Citation1–Citation4 Falls play a major role in this regard due to their strong connection to motor capacity, their high incidence in older age, and severe outcomes such as hip and wrist fractures.Citation5,Citation6 As a major means to counteract this possible chain of events, health care systems must shift focus from treatment towards promoting an active and healthy lifestyle.Citation7 Multifactorial training consisting of balance and strength exercises for lower limbs have been effective in reducing falls.Citation8–Citation11 In addition, training concepts should be tailored individually, adapting their contents to the respective person and their individual circumstances. However, this is a time, resource, and cost consuming process.Citation12–Citation15 Latest results from Sherrington et al show that exercise programs delivered in a group are also successful in terms of fall prevention.Citation9
Up to now there are structured training concepts specifically developed for the prevention of functional decline and falls in older adults,Citation15–Citation17 which prevalently lack sustainability and adherence.Citation18,Citation19 This fact is mainly observed in structured training formats including standardized exercises, pre-specified repetition numbers and intensity.Citation20 Older adults in general prefer exercises that are integrable into their everyday life.Citation21 This approach of lifestyle-integrated training in general has shown positive effects on fall prevention.Citation17,Citation22 The Lifestyle-integrated Functional Exercise (LiFE) program is a home-based exercise program developed as an alternative approach to structured exercise programs. LiFE aims to embed balance and strength activities and activities to increase physical activity (PA) into daily routines to create new movement habits and thereby prevent falls.Citation15,Citation16,Citation23 LiFE facilitates long-term adherence through its timesaving and flexible options to be active at any time and in any place during the day.Citation16,Citation24 Although the execution of LiFE activities is timesaving and due to the renunciation of materials cost-effective for the participants, the training and teaching of LiFE is the opposite. The individual one-to-one teaching of the program over seven home visits is a cost- and time-consuming delivery format from trainers’ perspectiveCitation14,Citation25 which hampers LiFE’s large-scale implementability.Citation14,Citation15,Citation23 Therefore, as part of the LiFE-is-LiFE project, the original LiFE programCitation16 was adapted into a group format (gLiFE) and tested in a pilot studyCitation25 as well as in a randomized trial for its non-inferiority compared to the individually delivered LiFE format in reducing activity-adjusted fall incidence and intervention costs.Citation26
Although the main outcome remained inconclusive, findings’ from the LiFE-is-LiFE trial highlight that gLiFE was associated with lower intervention costs and the increase in walking activity was significantly higher compared to LiFE while at the same time reduction in falls was somewhat lower in gLiFE compared to LiFE. Those results suggest that gLiFE is an attractive alternative from a payer’s and individual perspective and both formats come with important effects and benefits.Citation26 A detailed cost-effectiveness analysis of the LiFE-is-LiFE trial shows that the group program might be cost-effective for increasing PA but was unlikely to be cost-effective for preventing falls in older adults.Citation27
To complement those previous findings, gain a deeper insight into the effectiveness of both LiFE formats and to better understand who could benefit most from the two different formats (gLiFE and LiFE) and why, a detailed dose-response analysis is needed. A dose-response-analysis describes the relationship and magnitude of the response of an organism (functional improvement) to a stimulus (training stimulus) after a certain time.Citation28 To identify the optimal level of exercise required for effective interventions in older adults, investigating the dose-response relationship of exercise on physical functioning is considered important.Citation29 Typical dose parameters are training intensity, frequency, type of exercise (balance or strength activities), and duration.Citation30 Adherence must be distinguished from the training dose as it is typically defined as attendance (ie, does a participant take part in the training session or not).Citation31,Citation32 Since the LiFE program does not contain any repetition or duration information, this cannot be separated clearly. As perceived safety influences adherence in general in older adults when undertaking exercise programs,Citation33 safety can also influence training frequency and intensity and thus influence the dose. Another barrier for being physically active in older adults is a perceived lack of time.Citation34 Integrating LiFE activities into daily routine offers the opportunity to save time. This in combination with the desire of older adults to be able to integrate activities into life,Citation21 influences training adherence in general and hence dose.
To the best of our knowledge, the effects of those training parameters listed below (predictors/dose) on the physical function (response) of older adults have neither been analyzed in general exercise programs nor in the LiFE program, yet.
Therefore, the program content of the two different LiFE formats regarding perceived safety and the acceptance of the LiFE program was evaluated. Furthermore, the objective of this study was to examine the relationship between predictors of training response for the different formats activity frequency, perceived safety during performing the LiFE activities, degree of physical exertion of the activities, and the ability to integrate the LiFE activities into daily routine (dose), and the clinical outcomes in terms of functional improvement in balance, strength and PA (response).
Materials and Methods
Study Design
The LiFE-is-LiFE trial was a multi-center, single-blinded non-inferiority trial at the Network Aging Research (Heidelberg, Germany) and the Robert Bosch Hospital (Stuttgart, Germany). The study protocol was published previously.Citation14 Ethical approval was obtained from the Ethic Review Board of the Faculty of Behavioral and Cultural Studies at Heidelberg University (Schwe2017 2/1–1) and for Stuttgart from the ethics committee at the medical faculty of the Eberhard-Karls-University Tübingen (770/2016BO1). The study was registered on 12 March 2018 at Clinical Trials (Clinicaltrials.gov, NCT03462654) and was in agreement with the Declaration of Helsinki. All participants gave written informed consent at their first screening visit at the respective study site.
Participants
Participant recruitment started in April 2018. Persons 70 years and older were mainly recruited via personalized invitation letters using data from municipal registration offices in Heidelberg and Stuttgart. Interest and eligibility for participation was determined through a structured telephone interview and an on-site screening (details listed in the study protocol).Citation14 To ensure external validity all in- and exclusion criteria were chosen in accordance with previous studies.Citation15,Citation16
German-speaking, community-dwelling older adults aged 70 years and older who were able to walk at least 200m with or without walking aid were included in the study if they had either a) at least one injurious fall within the past 12 months or b) more than one non-injurious fall within the past 12 months or c) described a perceived decline in balance and needed more than 12 seconds for the “Timed Up-and-Go test”.Citation14,Citation35 Exclusion criteria were regular participation in structured exercise more than once a week or moderate to vigorous PA for more than 150 minutes per week in the last three months; moderate to severe cognitive problems (Montreal Cognitive Assessment <23 points);Citation36 current participation in another scientific trial; severe medical conditions (exhaustive list of the inclusion and exclusion criteria in study protocol).
Assessments and Outcome Measures
After determination of eligibility as part of telephone and in-house screenings, participants were assessed at baseline (T1), 6 months ± 2 weeks (T2), and 12 months ± 2 weeks (T3) after the first intervention session. After baseline assessment, participants were randomized into gLiFE or LiFE. Screening and assessments were led by trained assessors blinded towards group allocation. All questions for preparatory content evaluation and data for dose-response analysis were assessed at follow-up after 6 months (T2) retrospectively for the last four weeks’ by questionnaires. Those previously used self-report questionnairesCitation23 were adapted for the group format in the LiFE-is-LiFE non-inferiority trial.
Content Evaluation
For content evaluation of the LiFE activities, the total number of LiFE activities which have been performed per week (divided into balance and strength activities) as well as how often each single LiFE activity was chosen by participants were analyzed descriptively. The frequency of the two activities to increase PA were not assessed.
Ranking of activity preferences of the LiFE activities was documented asking: “Please name your three favorite LiFE activities”. The activity leaning forwards and backwards as well as sideways, stepping over objects forwards and backwards as well as sideways, standing and walking on toes and standing and walking on heels were merged. If fewer than three responses were given or an answer was not assignable to one of the LiFE activities, it was counted as missing. In case of more than three mentioned activities, only the first three were counted. All other variables of content evaluation are listed in .
Table 1 Variables Description of Content Evaluation
Dose-Response Analysis
Dose/Predictors of Response
The dose is a specified quantity or amount of a therapeutic agent, such as a training intervention, prescribed to be taken at stated intervals.Citation37 In addition, we assumed that the safety,Citation33 the degree of physical exertion (training intensity)Citation38 and the integrability of LiFE activities into daily routinesCitation34 have an effect on adherence and thus on the frequency of activity implementation. Therefore, in our analysis the dose and the predictors of response are defined by the parameters listed in .
Table 2 Variables Description of Dose-Response Analysis
Response
For dose-response analysis three clinical outcomes were selected to analyze clinical improvement. Each of the three domains on which the original LiFE program is based – balance, strength and PA - was covered.
The 8 Level Balance Scale (8 LBS)Citation16 was used to assess higher level balance. It is an extended version of the Short Physical Performance Battery (SPPB) balance componentCitation39 to assess hierarchically static balance incorporating challenging tasks at a higher level. Four different standing positions (narrow based, semi-tandem, tandem and one leg stand) should be held for 15 seconds, first with eyes open and then eyes closed. Arms are folded across in front of the chest. The next more challenging position is only taken if the previous position was completed successfully (15 seconds). The last successfully completed level is rated (maximum score: 8 points). In contrast to the version of Clemson et al,Citation16 in the present study the 8th level (“one leg stand with cognitive distracter”) was omitted and in accordance with the other positions the position “semi-tandem stand” was also carried out with eyes closed.
The 30 second chair stand (30 CS)Citation40 was used to assess functional strength. Participants are asked to sit down on a chair without armrest. Arms are folded across in front of their chest. After the start signal, participants get up and sit down again as often as possible within 30 seconds. The response is defined by the number of repetitions within the 30 seconds.
To assess changes in PA “activPAL4™ micro” accelerometers (PAL Technologies Ltd., Glasgow, Scotland) were attached to participants’ central front thigh to continuously measure PA under “free-living” conditions for seven days. The device has shown good to excellent reliability and validity.Citation41 Given that walking activity can be seen as high risk PA when it comes to falling,Citation42 PA was operationalized as mean steps per day in this study.
Intervention
The LiFE program consists of specific principles and activities to improve balance, increase muscle strength of the lower extremities and reduce sedentariness while increasing PA embedded within daily routine.Citation16 Rather than a prescribed set of exercise perform several times a week, the LiFE activities should be done many times during daily routines.Citation16
Both LiFE formats include three different balance principles named 1) “reducing base of support”, 2) “shifting weight and moving to the limits of stability” and 3) “stepping over objects” as well as seven balance activities as strategies to improve balance. Prescribed activities incorporating the first balance principle are tandem stand, tandem walk and one leg stand. Leaning forwards, backwards and from side to side can be assigned to the second balance principle and stepping over objects forwards, backwards and side to side to the third balance principle.Citation16,Citation25 Strategies to increase strength include six strength principles named “increase the number of time using a muscle”, “move slowly”, “use fewer muscles to move the same weight”, “increase the amount of weight”, “increase the range of motion” and “pause shortly during movement” and nine strength activities. These are bend your knees/squatting, sit to stand, standing or walking on toes, standing or walking on heels, stairclimbing, move sideways and tighten muscles (for example move ankles while sitting).Citation16,Citation25 Additionally, there are two more principles to increase PA and reduce sedentariness: “walk more” and “sit less”.Citation16,Citation23,Citation25 Next to the LiFE activities and LiFE principles, the LiFE program includes a behavioral change model for implementing new habits within selected situational contexts that serve as prompts turning intentions into actions.Citation16,Citation24,Citation25,Citation43,Citation44
Trained instructors delivered the same content as in the original LiFE programCitation16 and the previous pilot studyCitation25 based on the LiFE activities and LiFE principles as well as behavior change strategies for habit formation. Like the original LiFE programCitation16 the individual LiFE format (LiFE) was delivered via seven one-to-one home visits at participants’ homes while the group LiFE format (gLiFE) was delivered via seven group sessions with 8–12 participants by two trainers (one main and one co-trainer) per group. At the end of the 7th session, the participants of both formats were to finalize their set of LiFE activities for their individual training program. In both formats, participants received two additional booster phone calls four and ten weeks after the last intervention session.
Statistical Analysis
Descriptive Analysis
Descriptive analysis was conducted for age (in years), sex, number of fallers (fall in the last 6 months before baseline and fall frequency) and cognitive status (Montreal Cognitive Assessment score) at T1. Since all analyses of this paper are secondary analyses of the LiFE-is-LiFE trialCitation26 which was not powered for these secondary analyses no calculation of significance are carried out.
Content Evaluation
All parameters were reported as total number with percentage difference between both formats or mean and standard deviation (SD).
Dose-Response Analysis
The dose-response analysis is presented graphically using radar charts. For the subgroup radar charts, the six-/eight-point Likert scale of the individual items were divided into dichotomous groups by median split.
Due to the special approach of the LiFE program, integrating the LiFE activities into everyday life and training is not structured, for example in sets of 30/45/60 minutes Clemson et alCitation16 assumed that 0–3 days per week performing LiFE activities correspond to 0–1 days of training in a structured training program. In this way, it can be substantiated why participants who performed the LiFE balance/strength activities less than 4 days per week, are classified as non-to-low (balance-/strength-) performers. Accordingly, participants who performed the LiFE balance/strength activities for 4–7 days per week can be compared with people who carry out a structured training program at 2–3 days per week and considered medium-to-high (balance-/strength) performers.Citation16
All participants who felt “very safe” (1), “safe” (2) or “slightly safe” (3) during LiFE activities at home were considered as safe performers. All other participants were considered as unsafe-performers (“slightly unsafe” (4), “unsafe” (5) or “very unsafe” (6)). All participants who found the LiFE activities “very easy” (1), “easy” (2) or “slightly easy” (3) to perform/to integrate into daily routine were considered as not-exhausted-performers/performers with an easy integration. All other participants were considered as exhausted-performers/performers struggling with integration (“slightly exhausting/hard” (4), “exhausting/hard” (5) or “very exhausting/hard” (6)).
For comparing the values by radar charts, data were z-transformed in SPSS. All statistics and outcome analyses were performed using SPSS Version 23 (IBM Corporation, 2016, Armonk, NY, USA). Radar charts were created in Microsoft Excel (Version 2010).
Results
Descriptive Analysis
In total n= 310 participants were recruited and n= 309 participants completed the baseline assessment (T1). Before T2, n= 25 participants withdrew in gLiFE, n= 19 in LiFE. Two gLiFE participants and eleven LiFE participants did not complete the questionnaire analyzed in this study and were excluded from analysis. In total, n= 252 participants (gLiFE n= 126, LiFE n= 126) with a mean age of 78.6 years (range 69–95 years) were included in this analysis. Participants’ baseline characteristics are listed in .
Table 3 Participants’ Baseline Characteristics
Content Evaluation
The descriptive results of the content evaluation regarding chosen LiFE activities are listed in and .
Table 4 Content Evaluation – Frequency of the Chosen Balance and Strength Activities
Table 5 Content Evaluation – Safety of the LiFE Activities and Format, Degree of Physical Exertion, Ability to Integrate the LiFE Activities into Daily Routine and Acceptance of Both LiFE Formats
In total, participants had the opportunity to perform 16 LiFE activities - seven balance and nine strength activities. On average, gLiFE participants performed 11.18 (3.97) LiFE activities per week and LiFE participants 11.20 (3.62) LiFE activities per week. In gLiFE, the most frequently performed balance activities were the one leg stand and the tandem stand (). Likewise, LiFE participants performed the one leg stand and the leaning forwards/backwards most often. Regarding strength, stairclimbing was the most common LiFE activity in both formats (). There was no percentage difference > 10% between the formats based on the frequency of the chosen single activities except for tandem stand. 15.1% more gLiFE participants performed the tandem stand than LiFE participants ().
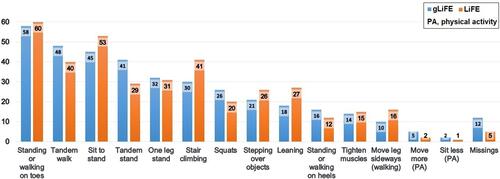
Activity preferences documented by the question: “Please name your three favorite LiFE activities” of the LiFE activities are presented in .
Standing or walking on toes (strength LiFE activity) was rated as the favourite LiFE activity in both formats. Tandem walk was the favourite balance LiFE activity in both formats. It was ranked 2nd for gLiFE and 4th for LiFE participants. Sit to stand was ranked 3rd for gLiFE and 2nd for LiFE. The activities to increase PA were located on the last two places in both formats ().
Mean and SD for the items on content evaluation regarding perceived safety during LiFE activities, perceived degree of physical exertion of the LiFE activities (intensity) and the ability to integrate the LiFE activities into daily routine as well as perceived safety and acceptance of the LiFE program are displayed in . The majority of the participants in both groups reported they felt “safe (2)” while performing the LiFE activities on their own. gLiFE and LiFE participants classified the LiFE activities between “slightly physically exhausting (4)” and “slightly easy (3)”. Participants of both groups reported that it was “slightly easy (3)” to incorporate the LiFE activities into their everyday life. The safety of the LiFE program was reported as “safe (2)” by participants of both formats. Moreover, the acceptability of the LiFE program was rated as “very good (1)” to “good (2)” by gLiFE and LiFE participants. (). On average LiFE participants felt marginally safer while performing the LiFE activities both on their own and during home visits. Additionally, for LiFE participants it was marginally easier to incorporate LiFE activities into their daily routine and the LiFE activities were less physically exhausting ().
Dose-Response Analysis
In the clinical responses for balance, strength and PA are listed.
Table 6 Dose-Response Analysis – Difference in Clinical Response Between gLiFE and LiFE
There is a functional improvement in all three domains in both groups, except for 8 LBS score in the LiFE group ().
shows the functional change regarding the selected balance, strength, and PA parameters (response) in relation to the dose/predictors of response parameters of both LiFE formats.
Figure 2 Radar charts of dose/predictors of response and response.
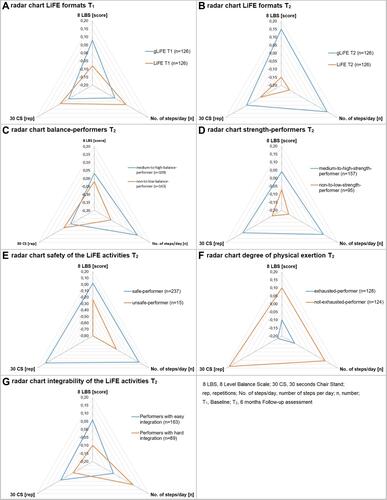
Medium-to-high-balance-performers (practicing balance activities on ≥ 4 days per week) performed better in the balance and PA domain compared to non-to-low-balance-performers (practicing balance activities on less than 4 days per week) (). Medium-to-high-strength-performers (practicing strength activities on ≥ 4 days per week) performed better in all three domains compared to non-to-low-strength-performers (practicing strength activities on less than 4 days per week) (). Participants who rated the activities as safe performed also better in all three domains compared to those participants who rated the activities as not safe (). Additionally, participants who classified the activities as not exhausting performed better in all three domains (). Participants who had no difficulty to integrate the activities into their lives performed better in the balance and strength domain compared to those who had difficulties ().
Discussion
Within the LiFE-is-LiFE projectCitation14,Citation26 the evidenced-based LiFE program was adapted from an individually-delivered home exercise program to a group-based format. The present study is a supplementary analysis to the main results.Citation26 Analyses of intervention content regarding LiFE activity frequency, perceived safety during LiFE program and activities, perceived degree of physical exertion (intensity) of the LiFE activities, potential for integration into daily routine as well as acceptance of both LiFE formats and subsequent changes in selected clinical outcomes like balance (8 LBS), strength (30 CS) and PA (steps/day) were carried out. To the best of our knowledge, this is the first in-depth analysis of the LiFE program content in particular but also for lifestyle-integrated prevention programs for older adults in general. It is also the first analysis of the relationship between predictors of training response for the different LiFE formats and the clinical outcomes in terms of functional improvement in balance, strength and PA (dose-response analysis).
Content Evaluation
Although the focus of fall prevention regularly lies on activities to improve balance,Citation45 LiFE focus more on strength activities. Accordingly, LiFE provide seven balance activities compared to nine strength activities. Regardless of the number of provided activities participants of the present study had the choice how many and which of the LiFE activities they would try to integrate permanently into their lives. Participants of both formats chose mostly strength instead of balance activities. In a previous pilot study, participants reported that strength activities were “easy to integrate into everyday life”.Citation23 This could be one reason why strength activities were chosen more frequently compared to balance activities. In addition, most frequently performed strength activities are activities that are usually carried out in everyday life (stair climbing and sit to stand), suggesting participants could just continue with their daily routine but perform those movements more consciously.
Considering the total number of LiFE activities selected, it is noticeable that more than two thirds of the available LiFE activities were actually performed and reported by the participants in both formats, suggesting that the activities of the LiFE program seem appropriate for the age and target group in both formats. Participants of both formats performed on average 11.2 out of 16 LiFE activities per week, which is in line with pilot results from another study.Citation23 The structure of both LiFE formats scheduled the integration of two out of four LiFE activities in the first three training sessions plus two more with each session until session six. In this way, 12 out of 18 LiFE activities (including two activities to increase PA) were tried to integrate after seven sessions. Hence, study participants of both formats have nearly maintained the number of different LiFE activities integrated after seven sessions (11 weeks) over the six-month period.
Assuming that the participants have not only performed the LiFE activities in the last four weeks as reported in the questionnaire, but already regularly since the seventh session, the activities were performed over a period of more than three months (> 90 days). According to Lally et al,Citation46 it takes on average 66 days (18–254 days) to form a new habit.Citation46 It is possible that in our study, gLiFE and LiFE participants may have performed the LiFE activities habitually, at least to a certain extent. The formation of habits depends on various factors, including intra-personal characteristics, the desired behavior and the external circumstances.Citation46 Previous studies on habit formation found that missing a chance to perform the desired behavior does not have a direct negative effect on the habit formation process.Citation46 So, if gLiFE and LiFE participants forgot to do a LiFE activity as planned in a certain situation once, habit formation might not have been disrupted. Other studies on basis of the LiFE-is-LiFE trial explore the issue of habit formation in the LiFE intervention in more detail.Citation47
Frequency of execution of the activities was nearly similar in both formats. For the balance component, gLiFE participants selected tandem stand and one leg stand most frequently. The tandem stand was actually selected more often (+15.1%) by gLiFE participants than LiFE participants. The more frequent selection in gLiFE may be based on group dynamics. One gLiFE participant chooses the tandem stand, which is one of the most plagiaristic LiFE activities, and reports about it in the group. As a result, other gLiFE participants decide to do this exercise as well. LiFE participants in turn chose leaning forwards/backwards/sideways and one leg stand most often. One leg stand and tandem stand are static balance activities, which were reported by the participants of two pilot studies as “easy to incorporate into everyday life”.Citation23,Citation48 Activities that can be easily incorporated into everyday life were perceived as most beneficialCitation48 and were therefore probably selected most frequently in this study. For the strength component, stair climbing and sit to stand were performed most often in both groups. Overall, the distribution of frequencies is generally very evenly spread over all LiFE activities, suggesting that all LiFE activities are considered feasible and useful from the target population in both formats and therefore still performed after six months.
The ranking of the favorite LiFE activities was nearly equal in gLiFE and LiFE but differs largely from the ranking in a previous pilot study.Citation23 Standing or walking on toes, which was the favorite LiFE activity in both formats in our study, was rated 12th or 15th place in the pilot study. On the other hand, in the pilot study, the one leg stand was on first place but was rated fifth place in both formats in our study. Only the second place of the pilot study (stairclimbing) also landed relatively far ahead in our ranking.Citation23 Those differences could be due to differences between samples, for example age group and different daily routine due to age, gender or cultural aspects as participants of the pilot study were compared to this study sample on average about 12 years younger.Citation23 The one leg stand is a very demanding LiFE activity and could therefore have ended up further behind in the ranking even if it was selected most (LiFE) or second most frequently (gLiFE) by participants. Standing and walking on toes is a strength activity that is relatively easy to perform, which in turn may have demanded too little from the younger target group of the pilot studyCitation23 but better fit to this study sample. Considering the ranking of the LiFE activities, it is also noticeable that the ranking did not necessarily correspond to the actual selected and performed activities. One reason for the difference between the ranking and the actual selected and performed activities could be that participants consider activities as helpful and performance-enhancing because the activities are more challenging (for example one leg stand) but those for the same reason are not among their favorite activities. Participants may have performed those LiFE activities just for anticipated health benefits.Citation49 Another reason could be the order of introduction of the LiFE activities in the seven sessions. The tandem stand, which is performed most frequently by the gLiFE participants as a balance activity, is taught during the first session. The participants therefore have a lot of time to integrate the tandem stand into their everyday life and to receive feedback during following sessions compared to activities which were introduced in later sessions. For example, the one leg stand is introduced in the fifth session. Therefore, participants have less time to incorporate this balance activity into their everyday life under supervision of trainers compared to the tandem stand. However, this activity is performed most frequently by the LiFE participants. This in turn could indicate that activities, which are introduced towards the end of the seven sessions, are more likely to be remembered and are therefore carried out more frequently. Ultimately, no clear connection between the order of introduction and activity frequency can be derived. Further reasons could be the feeling of safety while performing the individual activities or the integrability into everyday life. However, these two factors were not analyzed based on individual activities in the present study.
Even if the participants of both formats generally felt safe during the intervention sessions and when performing the LiFE activities independently, LiFE participants felt marginally “safer” in performing the LiFE activities in both situations compared to gLiFE participants. This difference between the formats may be due to direct one-to-one delivery during home visits.
Participants of both formats rated the intensity of the LiFE activities as “slightly easy/physically exhausting”. On the one hand, this suggests that the activities were explained well to the participants and on adequate level of difficulty. On the other hand, this could also indicate that the participants performed the activities at a difficulty level that was too low for them. Consequently, participants might not have exploited the potential of the LiFE program fully due to a too low training stimulus. This assumption is also supported by a focus group analysis of a previous pilot studyCitation48 in which participants stated that the intensity “was slightly too low” and that the strength activities could be “a bit more challenging”.
Additionally, participants of both formats rated the LiFE activities in general as “slightly easy to integrate into everyday life”, thereby the LiFE program meets older adults’ need for embeddable activities into daily routine.Citation21 LiFE participants rated the LiFE activities marginally more often as “easy to integrate” compared to gLiFE participants. This could be because the LiFE participants performed the activities directly in their own home environment during home visits and did not have to imagine and visualize the implementation of the activities in their everyday lives at home like gLiFE participants had to.
Moreover, the participants of both LiFE formats graded the LiFE program as “good”, indicating that both formats were highly accepted by participants. Thus, the statement of the participants of two previous pilot studies, who would recommend the LiFE program to a friendCitation23 and the positive attitude towards both LiFE formatsCitation48 can be confirmed.
Recapitulatory the content evaluation support the results of the non-inferiority analysisCitation26 and show that both LiFE formats are nearly similar.
Dose-Response Analysis
Regarding the results of Baseline (T1) and Follow-up assessment (T2), participants of both formats could improve in all three domains expect LiFE participants in the balance domain presented by the 8 LBS. These results suggest that participants from both formats have benefited from the LiFE program. On average, the LiFE participants were able to maintain their starting value in the 8 LBS over a period of 6 months, which can be regarded as a success in this age group.Citation50,Citation51
In line with literature,Citation52,Citation53 medium-to-high-balance performers (n= 109) scored better in balance and PA domain compared to those who performed the balance activities less frequently (n=143). It is assumed that an impaired balance leads to avoidance of activities and results in a low habitual PA level and a sedentary behavior.Citation54 Conversely, it can be assumed that balance training and improved balance leads to more PA. The strength activities are not only selected more frequently compared to balance activities, but also performed by more participants on more than four days per week (n= 157 vs n=95) for the same reason that was already mentioned above – they were “easy to integrate into everyday life”.Citation23 Several studies prove that older adults could realize several physiological benefits by undertaking strength training.Citation55,Citation56 Accordingly, the more frequent conduct of strength activities for the lower extremities leads to more muscle strength and thus a better result in the 30 CS test. There is also evidence in the literature that strength training in older adults not only enhances strength but also improves balanceCitation57 and physical activity.Citation58,Citation59
The majority of the participants (n= 237) felt confident performing the activities, which indicates good acceptance and introduction of the LiFE activities by the trainers. Additionally those participants who felt “rather unsafe” (n= 15) in performing the LiFE activities on their own performed worse in all three domains than the participants who felt “safe”. One possible explanation for this could be training inside their “comfort zone”. Subjects who felt “unsafe” may have trained at a less demanding level of difficulty because they were slowed down by their insecurity (for example balance training without support of the hands) and hampered by fear (for example fear of falling), thus had a lower exercise self-efficacy and therefore could not set any effective training stimulus to challenge their strength and balance enough.Citation60 Trainers should encourage participants to push themselves to their limits and challenge themselves. They should explain to the participants that progress can only be achieved through challenging training on a regular basis. About half of all participants rate the activities as exhausting (n= 128) and half as not exhausting (n=124), which is in line with a previous study.Citation23 This suggests that the LiFE activities are appropriate for the target population in terms of difficulty. However, when tailoring the program, care should be taken to ensure that all participants are able to adapt the activities to their individual level of difficulty and training progress. The facts that those participants who found the LiFE activities rather “not exhausting”, performed better in all three domains could be explained by the fact that those participants had a higher level at the beginning of the study and could keep this training level. It is also possible, that they already improved their motor capacity within the 6 months and then at reassessment (T2) the activities were classified as “not exhausting” anymore. The participants who did not improve that much until T2, however, possibly found the activities rather “exhausting”.
The probability that the activities were carried out more frequently, more consistently and possibly more precisely is high if they were classified as “easy to integrate into everyday life”. Almost two thirds of the participants state that the activities can be easily integrated into everyday life (n= 163). Those participants who found it “hard to integrate the activities into everyday life” (n= 89) walked more steps per day (PA domain) compared to the participants who rated the LiFE activities as “easy to integrate into everyday life”. This could be because participants who had difficulties integrating balance and strength activities into daily routine focused on being more physically active instead. If those participants, for example, went shopping by foot instead of by car, as recommended in the LiFE program, PA can be integrated into daily life without requiring much additional time.Citation23
Limitations
One limitation is that the frequency of the performed LiFE activities was analyzed at one time point (T2) and retrospectively for the last four weeks. As behaviors that occur frequently, such as the LiFE activities, are unlikely to be specifically present in memory in the long termCitation61 precise tracking of which LiFE activity were carried out each week over the 6-month period is prone to errors. In addition, it is a self-reported, non-validated questionnaire and the participants may have been influenced by the social desirability of the answers.Citation55 Participants may have reported more activities than they actually performed and the number of reported days per week on which the LiFE activities were performed may differ from the actual days. An average value for the last four weeks was requested and individual implementation of the activities could differ greatly in the individual weeks and vary due to illness or pain, for example. No monitoring was carried out to check whether the participants actually performed the activities at home as indicated. Statements on the frequency of the activities to increase PA could not be made, as these were not reported in the questionnaire. Only the average number of steps per day at the two time points T1 and T2 could be evaluated here. Since the results in this paper are secondary analyses and the LiFE-is-LiFE trial was only powered for main analysis, no statements about statistical significance can be made in this paper.
Conclusion
This paper provides important insights beyond the primary outcomes of the LiFE-is-LiFE trial, that is, what are predictors and which training dose is necessary to achieve the measured functional improvements in balance, strength and PA. The participants succeeded in safely integrating the LiFE activities into their everyday lives. They appreciated the LiFE program, which was found to be slightly exhausting on average. As there are similar results for gLiFE and LiFE in terms of functional response, individual preferences based on delivery format should be taken into account in order to convey the program with the highest possible motivation. In order to achieve the best possible results in the areas of balance, strength and PA, the LiFE activities should be provided in such a way that the participants feel confident and safe while performing those activities. For participants with balance deficits and limited PA, the focus should also be on performing balance activities on four days or more per week in addition to strength training. Moreover, trainers should enable participants to push themselves to their limits and challenge themselves. This could make the program even more specific to peoples’ training level and possibly increase positive training effects.
Abbreviations
LiFE, Lifestyle integrated Functional Exercise; gLiFE, group LiFE; LiFE, individual delivered LiFE; PA, physical activity; 8 LBS, 8 Level balance scale; 30 CS, 30 seconds chair stand.
Data Sharing Statement
The datasets of the non-inferiority trial is published elsewhereCitation26,Citation27 and are together with the datasets used and/or analyzed during the current study available from the LiFE-is-LiFE consortium upon reasonable request.
Ethics Approval and Consent to Participate
The randomized non-inferiority trial of the LiFE-is-LiFE project was evaluated and approved by the ethical committees in Heidelberg (document number Schwe2017 2/1–1), and Tübingen (document number 723/2017BO2) and is in agreement with the Declaration of Helsinki. All participants gave written informed consent.
Consent for Publication
The manuscript does not contain any images, videos or recordings which require approval.
Author Contributions
CN, FKG, CPJ, SL, JK, CB and MS were responsible for the study concept and design. CN, FKG, CPJ, SL were also responsible for the study organization and execution, recruitment and data collection. CN performed the statistical analysis and drafted the manuscript. All authors critically revised and reviewed the manuscript and gave important intellectual content. All authors agreed on the journal to which the article will be submitted and read and approved the final manuscript. They agree with the order of presentation of the authors and take responsibility for the content of the manuscript.
Acknowledgments
This research would not have been possible without the contributions of LiFE-is-LiFE participants. We are grateful for their insights, time, and engagement in the research project. We also thank all colleagues who supported and contributed to the conduct of this study: the trainers and assessors at our study centers Mona Baer, Malte Liebl-Wachsmuth, Martin Bongartz, Annette Lohmann (Network Aging Research, Heidelberg University), Christoph Endress, Anna Kroog, Carolin Barz, Julia Gugenhan and Rebekka Leonhardt (Department of Clinical Gerontology and Geriatric Rehabilitation, Robert Bosch Hospital, Stuttgart, Germany). A specially thank you goes to the advisory board: Prof. Lindy Clemson, Prof Lena Fleig, Prof Frank Oswald, and Prof Chris Todd as well as to Birgit Och and Sarah Enderle for our database management.
Disclosure
The authors declare that they have no financial or non-financial competing interests.
Additional information
Funding
References
- Grimmer M, Riener R, Walsh CJ, Seyfarth A. Mobility related physical and functional losses due to aging and disease - a motivation for lower limb exoskeletons. J NeuroEngineering Rehabil. 2019;16(1):2. doi:10.1186/s12984-018-0458-8
- Böhm K, Mardorf S, Nöthen M, et al. Gesundheit und Krankheit im Alter. Robert Koch-Institut; 2009. doi:10.25646/3145
- Park J, Yim J. A new approach to improve cognition, muscle strength, and postural balance in community-dwelling elderly with a 3-D virtual reality kayak program. Tohoku J Exp Med. 2016;238(1):1–8. doi:10.1620/tjem.238.1
- Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17(1):25–46. doi:10.1146/annurev.pu.17.050196.000325
- Gordt K, Mikolaizak AS, Taraldsen K, et al. Creating and validating a shortened version of the community balance and mobility scale for application in people who are 61 to 70 years of age. Phys Ther. 2020;100(1):180–191. doi:10.1093/ptj/pzz132
- Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health Rev Can Sante Publique. 1992;83(Suppl 2):S7–11.
- Rechel B, McKee M, Haas M, et al. Public reporting on quality, waiting times and patient experience in 11 high-income countries. Health Policy Amst Neth. 2016;120(4):377–383. doi:10.1016/j.healthpol.2016.02.008
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–2243. doi:10.1111/j.1532-5415.2008.02014.x
- Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. doi:10.1002/14651858.CD012424.pub2
- Vieira ER, Palmer RC, Chaves PHM. Prevention of falls in older people living in the community. BMJ. 2016;353:i1419. doi:10.1136/bmj.i1419
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9). doi:10.1002/14651858.CD007146.pub3
- Chou CH, Hwang CL, Wu YT. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil. 2012;93(2):237–244. doi:10.1016/j.apmr.2011.08.042
- Liu CJ, Shiroy DM, Jones LY, Clark DO. Systematic review of functional training on muscle strength, physical functioning, and activities of daily living in older adults. Eur Rev Aging Phys Act. 2014;11(2):95–106. doi:10.1007/s11556-014-0144-1
- Jansen CP, Nerz C, Kramer F, et al. Comparison of a group-delivered and individually delivered lifestyle-integrated functional exercise (LiFE) program in older persons: a randomized noninferiority trial. BMC Geriatr. 2018;18(1):267. doi:10.1186/s12877-018-0953-6
- Taraldsen K, Mikolaizak AS, Maier AB, et al. Protocol for the PreventIT feasibility randomised controlled trial of a lifestyle-integrated exercise intervention in young older adults. BMJ Open. 2019;9(3):e023526. doi:10.1136/bmjopen-2018-023526
- Clemson L, Singh MAF, Bundy A, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ. 2012;345:47. doi:10.1136/bmj.e4547
- Weber M, Belala N, Clemson L, et al. Feasibility and effectiveness of intervention programmes integrating functional exercise into daily life of older adults: a systematic review. Gerontology. 2018;64(2):172–187. doi:10.1159/000479965
- Hill KD, Hunter SW, Batchelor FA, Cavalheri V, Burton E. Individualized home-based exercise programs for older people to reduce falls and improve physical performance: a systematic review and meta-analysis. Maturitas. 2015;82(1):72–84. doi:10.1016/j.maturitas.2015.04.005
- Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. The Gerontologist. 2016;56(Suppl_2):S268–S280. doi:10.1093/geront/gnw031
- Merom D, Pye V, Macniven R, et al. Prevalence and correlates of participation in fall prevention exercise/physical activity by older adults. Prev Med. 2012;55(6):613–617. doi:10.1016/j.ypmed.2012.10.001
- Burton NW, Khan A, Brown WJ. How, where and with whom? Physical activity context preferences of three adult groups at risk of inactivity. Br J Sports Med. 2012;46(16):1125–1131. doi:10.1136/bjsports-2011-090554
- Franco MR, Howard K, Sherrington C, et al. Eliciting older people’s preferences for exercise programs: a best-worst scaling choice experiment. J Physiother. 2015;61(1):34–41. doi:10.1016/j.jphys.2014.11.001
- Schwenk M, Bergquist R, Boulton E, et al. The adapted lifestyle-integrated functional exercise program for preventing functional decline in young seniors: development and initial evaluation. Gerontology. 2019;65(4):362–374. doi:10.1159/000499962
- Boulton E, Hawley-Hague H, French DP, et al. Implementing behaviour change theory and techniques to increase physical activity and prevent functional decline among adults aged 61–70: the PreventIT project. Prog Cardiovasc Dis. 2019;62(2):47–156. doi:10.1016/j.pcad.2019.01.003
- Kramer F, Labudek S, Jansen CP, et al. Development of a conceptual framework for a group-based format of the Lifestyle-integrated Functional Exercise (gLiFE) programme and its initial feasibility testing. Pilot Feasibility Stud. 2020;6:6. doi:10.1186/s40814-019-0539-x
- Jansen CP, Nerz C, Labudek S, et al. Lifestyle-integrated functional exercise to prevent falls and promote physical activity: results from the LiFE-is-LiFE randomized non-inferiority trial. Int J Behav Nutr Phys Act. 2021;18(1):115. doi:10.1186/s12966-021-01190-z
- Gottschalk S, König HH, Schwenk M, et al. Cost-effectiveness of a group vs individually delivered exercise program in community-dwelling persons aged ≥70 years. J Am Med Dir Assoc. 2021. doi:10.1016/j.jamda.2021.08.041
- Crump KS, Hoel DG, Langley CH, Peto R. Fundamental carcinogenic processes and their implications for low dose risk assessment. Cancer Res. 1976;36(9pt.1):2973–2979.
- Kaushal N, Desjardins-Crépeau L, Langlois F, Bherer L. The effects of multi-component exercise training on cognitive functioning and health-related quality of life in older adults. Int J Behav Med. 2018;25(6):617–625. doi:10.1007/s12529-018-9733-0
- Herold F, Müller P, Gronwald T, Müller NG. Dose-response matters! - A perspective on the exercise prescription in exercise-cognition research. Front Psychol. 2019;10:2338. doi:10.3389/fpsyg.2019.02338
- Fairman CM, Nilsen TS, Newton RU, et al. Reporting of resistance training dose, adherence, and tolerance in exercise oncology. Med Sci Sports Exerc. 2020;52(2):315–322. doi:10.1249/MSS.0000000000002127
- Nilsen TS, Scott JM, Michalski M, et al. Novel methods for reporting of exercise dose and adherence: an exploratory analysis. Med Sci Sports Exerc. 2018;50(6):1134–1141. doi:10.1249/MSS.0000000000001545
- Bethancourt HJ, Rosenberg DE, Beatty T, Arterburn DE. Barriers to and facilitators of physical activity program use among older adults. Clin Med Res. 2014;12(1–2):10–20. doi:10.3121/cmr.2013.1171
- Craighead DH, Heinbockel TC, Hamilton MN, et al. Time-efficient physical training for enhancing cardiovascular function in midlife and older adults: promise and current research gaps. J Appl Physiol. 2019;127(5):1427–1440. doi:10.1152/japplphysiol.00381.2019
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi:10.1111/j.1532-5415.2005.53221.x
- Company HMHP. The American Heritage Dictionary entry: dose. Available from: https://www.ahdictionary.com/word/search.html?q=dose. Accessed August 5, 2021.
- Wasfy M, Baggish AL. Exercise dose in clinical practice. Circulation. 2016;133(23):2297–2313. doi:10.1161/CIRCULATIONAHA.116.018093
- Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi:10.1093/geronj/49.2.m85
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi:10.1080/02701367.1999.10608028
- Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40(9):779–784. doi:10.1136/bjsm.2006.027276
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi:10.1056/NEJM198812293192604
- Clemson L, Singh MF, Bundy A, et al. LiFE Pilot Study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Aust Occup Ther J. 2010;57(1):42–50. doi:10.1111/j.1440-1630.2009.00848.x
- Clemson L, Munro J, Fiatarone Singh M. Lifestyle-Integrated Functional Exercise (LiFE) program to prevent falls [Trainer’s Manual]. Sydney University Press; 2014. Available from: https://sydneyuniversitypress.com.au/products/78838. Accessed August 5, 2021.
- Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758. doi:10.1136/bjsports-2016-096547
- Lally P, van Jaarsveld CHM, Potts HWW, Wardle J. How are habits formed: modelling habit formation in the real world. Eur J Soc Psychol. 2010;40(6):998–1009. doi:10.1002/ejsp.674
- Labudek S, Fleig L, Jansen CP, et al. Changes in psychological determinants of behavior change after individual vs. group-based lifestyle-integrated fall prevention: Results from the LiFE-is-LiFE trial. Gerontology. 2022. In Press.
- Reicherzer L, Kramer-Gmeiner F, Labudek S, et al. Group or individual lifestyle-integrated functional exercise (LiFE)? A qualitative analysis of acceptability. BMC Geriatr. 2021;21(1):93. doi:10.1186/s12877-020-01991-0
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJH. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89–112. doi:10.1080/17437199.2015.1082146
- Downs S, Marquez J, Chiarelli P. Normative scores on the Berg Balance Scale decline after age 70 years in healthy community-dwelling people: a systematic review. J Physiother. 2014;60(2):85–89. doi:10.1016/j.jphys.2014.01.002
- da Silva Borges EG, de Souza Vale RG, Cader SA, et al. Postural balance and falls in elderly nursing home residents enrolled in a ballroom dancing program. Arch Gerontol Geriatr. 2014;59(2):312–316. doi:10.1016/j.archger.2014.03.013
- Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports Med Auckl NZ. 2015;45(12):1721–1738. doi:10.1007/s40279-015-0375-y
- Dohrn IM, Hagströmer M, Hellénius ML, Ståhle A. Short- and long-term effects of balance training on physical activity in older adults with osteoporosis: a randomized controlled trial. J Geriatr Phys Ther. 2017;40(2):102–111. doi:10.1519/JPT.0000000000000077
- Delbaere K. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33(4):368–373. doi:10.1093/ageing/afh106
- Izquierdo M, Häkkinen K, Ibañez J, et al. Effects of strength training on muscle power and serum hormones in middle-aged and older men. J Appl Physiol. 2001;90(4):1497–1507. doi:10.1152/jappl.2001.90.4.1497
- Häkkinen A, Sokka T, Kotaniemi A, Hannonen P. A randomized two-year study of the effects of dynamic strength training on muscle strength, disease activity, functional capacity, and bone mineral density in early rheumatoid arthritis. Arthritis Rheum. 2001;44(3):515–522. doi:10.1002/1529-0131(200103)44:3<515::AID-ANR98>3.0.CO;2-5
- Lee IH, Park SY. Balance improvement by strength training for the elderly. J Phys Ther Sci. 2013;25(12):1591–1593. doi:10.1589/jpts.25.1591
- Hunter GR, Fisher G, Bryan DR, Zuckerman PA. Weight loss and exercise training effect on oxygen uptake and heart rate response to locomotion. J Strength Cond Res. 2012;26(5):1366–1373. doi:10.1519/JSC.0b013e31824f236c
- Seguin RA, Eldridge G, Lynch W, Paul LC. Strength training improves body image and physical activity behaviors among midlife and older rural women. J Ext. 2013;51(4):4FEA2.
- Ponzano M, Gibbs JC, Adachi JD, et al. Exploring fear of falling and exercise self-efficacy in older women with vertebral fractures. J Aging Phys Act. 2020;29(2):219–224. doi:10.1123/japa.2019-0485
- Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health-Syst Pharm. 2008;65(23):2276–2284. doi:10.2146/ajhp070364