 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Chronic kidney disease (CKD) is recognized worldwide as a public health problem, and its prevalence increases as the population ages. However, the applicability of formulas for estimating the glomerular filtration rate (GFR) based on serum creatinine (SC) levels in elderly Chinese patients with CKD is limited.
Materials and methods
Based on values obtained with the technetium-99m diethylenetriaminepentaacetic acid (99mTc-DTPA) renal dynamic imaging method, 319 elderly Chinese patients with CKD were enrolled in this study. Serum creatinine was determined by the enzymatic method. The GFR was estimated using the Cockroft–Gault (CG) equation, the Modification of Diet in Renal Disease (MDRD) equations, the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, the Jelliffe-1973 equation, and the Hull equation.
Results
The median of difference ranged from −0.3–4.3 mL/min/1.73 m2. The interquartile range (IQR) of differences ranged from 13.9–17.6 mL/min/1.73 m2. Accuracy with a deviation less than 15% ranged from 27.6%–32.9%. Accuracy with a deviation less than 30% ranged from 53.6%–57.7%. Accuracy with a deviation less than 50% ranged from 74.9%–81.5%. None of the equations had accuracy up to the 70% level with a deviation less than 30% from the standard glomerular filtration rate (sGFR). Bland–Altman analysis demonstrated that the mean difference ranged from −3.0–2.4 mL/min/1.73 m2. However, the agreement limits of all the equations, except the CG equation, exceeded the prior acceptable tolerances defined as 60 mL/min/1.73 m2. When the overall performance and accuracy were compared in different stages of CKD, GFR estimated using the CG equation showed promising results.
Conclusions
Our study indicated that none of these equations were suitable for estimating GFR in the elderly Chinese population investigated. At present, based on overall performance, as well as performance in different CKD stages, the CG equation may be the most accurate for estimating GFR in elderly Chinese patients with CKD.
Introduction
Chronic kidney disease (CKD) is a worldwide problem that is in need of particular attention. The prevalence of CKD varies with ageCitation1 and is markedly high in those of the population greater than 64 years old.Citation2,Citation3 In China, the population of those over 60 years old will increase by 16.55% every year; by 2040 this age group will account for 28% of the entire population, which means that China will be considered an ageing society.Citation4 These findings highlight the clinical and public health importance of CKD. The glomerular filtration rate (GFR) is typically considered to be the best way to assess renal function in healthy or diseased states. Direct measurement of GFR by inulin clearance is often impractical. Radioisotopic methods using ethylenediaminetetraacetic acid (51Cr EDTA), 125 iodine iothalamate, and so on provide acceptable alternatives to inulin clearance.Citation5 However, these methods are cumbersome, expensive, and are available to only a few hospitals. Many formulae using serum creatinine (SC) have been established to estimate GFR in adults. The National Kidney Foundation has recommended that the Cockroft–Gault (CG) equation and the Modification of Diet in Renal Disease (MDRD) equations should be used to estimate GFR in adults.Citation6 However, the SC-based equations were not initially developed for elderly people. Additionally, older individuals have decreased lean body mass and often suffer from chronic diseases associated with decreased muscle mass and SC levels,Citation7 thus, when applied to elderly people, the effectiveness of such equations is doubtful.
As previously described,Citation8 GFR estimation equations showed a great deal of bias in elderly Chinese CKD patients. In this study, we increased the sample size and again evaluated the accuracy of various GFR estimation equations in elderly Chinese patients with CKD, comparing them with radionuclide GFRs in a clinical setting.
Research design and methods
The present study was conducted among 319 elderly Chinese CKD patients (121 women; mean ± SD age 70.0 ± 6.8 years; standard GFR (sGFR) measured by 99mTc-DTPA GFR was 39.4 ± 21.8 mL/min per 1.73 m2) from January 2005 through December 2009 at the Third Affiliated Hospital of Sun Yet-sun University, China. The patient exclusion criteria were as previously described.Citation8 None of the subjects were undergoing dialysis during the study period. The CKD patients were assigned to one of five stages based on the National Kidney Foundation (NKF) Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guidelines.Citation9 The causes and stages of CKD, as well as other details, are listed in . For convenience, stages 1 and 2, and stages 4 and 5 were combined. The study was approved by the institutional review board at the Third Affiliated Hospital of Sun Yet-sun University. All patients provided informed consent before participating in the study.
Table 1 Patient characteristics
Glomerular filtration rate, measured by the 99mTc-DTPA renal dynamic imaging method and standardized by body surface area (BSA), was used as the sGFR.Citation10–Citation12 99mTc-DTPA renal dynamic imaging (modified Gate’s method) was measured by Millennium TMMPR SPECT using the General Electric Medical System. 99mTc-DTPA renal imaging showed good agreement with plasma clearance of 51Cr EDTA.Citation13 The 99mTc-DTPA renal dynamic imaging method used was as previously described.Citation8 After image acquisition, the patient’s weight and height were entered into the eNTEGRA Workstation (General Electric Company, Waukesha, WI), on which all imaging data were recorded. The sGFR was automatically calculated, according to Gate’s algorithm.
Estimations of renal function
The results of the CG equation, the Jelliffe-1973 equation, and the Hull equation were standardized for a BSACitation20 of 1.73 m2.
Other measurements
A single serum determination was performed on the same day prior to measurement of GFR using 99mTc-DTPA renal dynamic imaging. The SC levels, serum albumin, and urea were assayed on a Hitachi 7180 autoanalyzer (Hitachi, Tokyo, Japan) with reagents from Roche Diagnostics (Mannheim, Germany). Serum creatinine was determined by the enzymatic method. Sex, age, height, and weight were simultaneously recorded.
Statistical analysis
The sGFR and the estimated GFR (eGFR) were compared using Bland–Altman analysis. The precision was measured as the width between the 95% limits of agreement. A prior acceptable tolerance for the difference between eGFR and sGFR was defined as twice the limit for CKD stages, which is 60 mL/min/1.73 m2.Citation8 The accuracy of GFR estimates was determined as the percentage of results deviating less than 15%, 30%, and 50% from the sGFR. The sensitivity and specificity of all the equations in correctly classified CKD stage 3 (GFR < 60 mL/min/1.73 m2) were based upon the cut points established by the National Kidney FoundationCitation9 and were calculated and compared according to the receiver operating characteristic (ROC) curve approach. In the preliminary analysis,Citation8 the Jelliffe-1973 equation performed better than the other equations. Therefore, we chose eGFR measured by the Jelliffe-1973 equation as the reference against which all comparisons between equations were made. Results were considered to be significant at P < 0.05. All statistical analyses were performed using SPSS software (version 11.0; IBM, Armonk, NY) and Medcalc for Windows (version 9.3.9.0; Medcalc Software, Mariekerke, Belgium).
Results
Overall performance of the equations
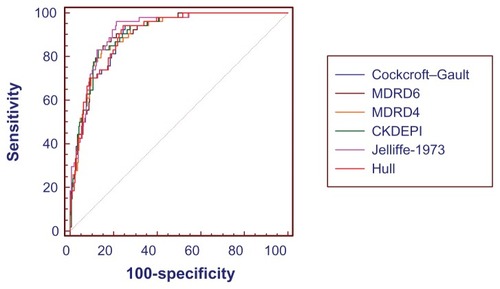
The medians of difference of the four-variable MDRD equation and the six-variable MDRD equation were less than those of the other equations. The interquartile range (IQR) of difference for the CG equation and the Hull equation were smaller. The accuracies with a deviation less than 15% from the sGFR of the Hull equation and the CG equation were higher. The CG equation and the Jelliffe-1973 equation provided better results than the others in accuracies with deviations less than 30% and 50% from the sGFR. However, none of the equations had accuracies that reached 70% while differing less than 30% from the sGFR. Chronic kidney disease stage misclassifications by the four-variable MDRD equation and the Jelliffe-1973 equation were less than that of the other equations. All of the equations had CKD stage misclassification higher than 42% (). We used Bland–Altman plot (see ) analysis to calculate the mean of the difference between eGFR and sGFR and the precision of eGFR. Using this approach, the CKD-EPI equation and the Jelliffe-1973 equation demonstrated less means of the difference than the other equations. The precisions of the GFR estimated by the CG equation and the CKD-EPI equation were better than the other equations. However, the agreement limits of the equations, except for the CG equation, exceeded the prior acceptable tolerances, defined as 60 mL/min/1.73 m2. The ROC curve analysis showed that the maximum diagnostic accuracy of all the equations for the diagnosis of moderate renal failure (GFR < 60 mL/min/1.73 m2) was not statistically significant (P > 0.05 compared with the Jelliffe-1973 GFR). Detailed performances are listed in and , and .
Table 2 Overall performances of eGFR and sGFR
Table 3 AUCs, sensitivity, and specificity of eGFR for the diagnosis of moderate renal failure (GFR < 60 mL/min/1.73 m2)
Figure 1 Bland–Altman plot of eGFR and sGFR (mL/min/1.73 m2). Solid line represents the mean of difference between methods; dashed lines represent 95% limits of agreement of the mean of difference between methods. (A–F) Represent for the GFR results estimated using Cockcroft–Gault equation, six-variable MDRD equation, four-variable MDRD equation, CKD-EPI equation, Jelliffe-1973 equation, and Hull equation, respectively.
Abbreviations: CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; eGFR, estimated glomerular filtration rate; sGFR, standard glomerular filtration rate; MDRD, Modification of Diet in Renal Disease.
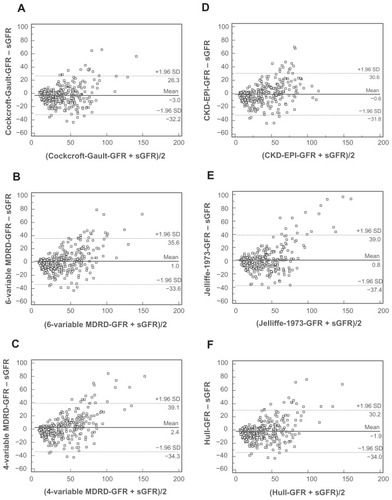
Figure 2 Receiver operating characteristic curves of eGFR for the diagnosis of moderate renal failure (GFR < 60 mL/min/1.73 m2).
Abbreviations: CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; eGFR, estimated glomerular filtration rate; sGFR, standard glomerular filtration rate; MDRD, Modification of Diet in Renal Disease.
Performance of various stages of CKD
In CKD stages 1 and 2, the median of the difference of the Jelliffe-1973 equation was smaller. The IQR of difference for the CKD-EPI equation was smaller. The CKD-EPI equation provided better results than the others in accuracies with deviations less than 15%, 30%, and 50% from the sGFR. In CKD stage 3, the median of the difference of the six-variable MDRD equation was smaller. The IQR of difference for the CG equation was smaller. Accuracy with a deviation less than 15% from the sGFR of the Hull equation was higher. The CG equation provided better results than the others in accuracies with deviations less than 30% and 50% from the sGFR. In CKD stages 4 and 5, the median of the difference for the Jelliffe-1973 equation was smaller. The IQRs of difference for the CG equation and the Jelliffe-1973 equation were smaller. The Jelliffe-1973 equation revealed higher accuracies with deviation less than 15%, 30%, and 50% from the sGFR ().
Table 4 Performances of eGFR and sGFR in the different stages of CKD
Discussion
A report from the Dialysis and Transplantation Registration Group of the Chinese Society of Nephrology revealed that in 1999, the population undergoing maintenance dialysis numbered 41,755.Citation21 Liu and his colleagues found that, in China, about 14.82% of the 13,383 hospitalized patients investigated were diagnosed as having CKD.Citation22 They also found that the prevalence of CKD increases dramatically in older people. Therefore, in the elderly population, the evaluation of renal function is critically important in clinical practice, since it has a great impact on diagnosis and medical treatment requiring adjustment in drug dosages in the elderly. The changes in renal function that accompany aging present a decrease in GFR – more than 1 mL/min/1.73 m2/year in those over the age of 40 years.Citation23 However, this change can vary. Gault and CockcroftCitation24 found that the variability of creatinine clearance also increased with increasing age. This was accordant with a recent report from the Baltimore Longitudinal Study of Aging, which demonstrated that variability, such as decrease, increase, or no change, in creatinine clearance emerged in 254 healthy individuals followed up for as long as 23 years.Citation23 This variability causes additional difficulties in the estimation of GFR. The American Diabetes Association recommended estimation of GFR using prediction equations based on SC determinations.Citation25 However, this has still not been validated in elderly populations.
Application of SC-based GFR prediction equations to elderly patients with CKD is limited. Bevc et alCitation26 found that both the MDRD equations and the CKD-EPI equation lacked precision, and the accuracy within 30% of estimated 51Cr EDTA clearance values differs according to the stage of CKD. Burkhardt et alCitation27 demonstrated that the accuracies and precisions of the CG equation and the MDRD equations were low, and that there was an underestimation of actual GFR. A cross-sectional study in a French hospital with mostly Caucasian patientsCitation28 also found that the CG equation seemed to be the most accurate and appropriate formula. The present study revealed that none of the equations had acceptable accuracy to exactly predict GFR in an elderly population. A new equation is still needed to provide a more accurate estimation of GFR in elderly patients.
Age and body mass are important sources of bias in the prediction. All the equations in our study are based on the SC value. The generation of creatinine is determined primarily by muscle mass and dietary intake. Muscle mass is considered a constant part of total body weight. However, elderly people often have decreased lean body mass and suffer from many chronic diseases associated with decreased muscle mass and SC levels.Citation7 Additionally, elderly patients are often malnourished and Compan et al found that patients classified as malnourished account for 25% of the hospitalized elderly.Citation29 Older and malnourished patients are particularly at risk of having decreased GFR even with normal SC levels.Citation30,Citation31 All of these factors could influence the accuracy of application of the equations. Recent research finds that applying the CG equation corrected by BSA may be more precise than the MDRD equations in patients with malnutrition or inflammation. In the present study, the CG equation had higher accuracy than the other equations; however, it still did not provide acceptable accuracy.
In these prediction equations, the subjects enrolled did not adequately represent subjects older than 70 years of age. The MDRD equation had not been initially validated in older people, and the mean age was 50.6 ± 12.7 years.Citation16 The CG equation was originally established with 249 patients aged 18 to 92 years. Among the patients, only 59 (23%) were over the age of 70 years and women accounted for only 4% of the patients,Citation14 yet when a study was applied in an elderly population to calculate creatinine clearance, most of the subjects were female. A correction factor of 0.85 was proposed for females, according to data from earlier studies, but in Cockcroft and Gault’s own study, data on females were extremely limited, so this figure must be considered pure speculation.Citation32 Special attention must be given to the application of equations extended to populations not represented in the original study.
The large percentage of diabetic patients in the present study is also a source of bias. Related investigations found that many of the diabetic patients had a supernormal GFR before the onset of overt clinical diabetic nephropathy and progressive renal insufficiency.Citation33,Citation34 A surrogate marker based on SC cannot effectively detect emerging hyperfiltration in the early phase of diabetic nephropathies.Citation27 In our study, diabetic patients make up 35.7% of the patients, so the remarkable underestimation of actual GFR by formula estimators is, in part, on account of an undetectable hyperfiltration in patients with diabetes; this is consistent with previous results.Citation35,Citation36 Considering the number of elderly patients with diabetes, it is understandable that our results underestimated the actual GFRs.
The methods used to measure SC were different in each study. In the original MDRD study, SC was measured by the CX3 Beckman method.Citation15,Citation16 In the CKD-EPI equation,Citation17 SC was determined by the enzymatic method. The other equations in our study were published long ago, and the methods used for SC measurement have not been available until now.Citation36 In our study, SC was measured using the enzymatic method, different from that in the MDRD study. Several studies have proven that calibration of SC assays can influence the accuracy of MDRD.Citation37,Citation38 Variability among clinical laboratories in the calibration of SC assays results in bias in the estimation of GFR.
In conclusion, our data indicated that when SC was measured by the enzymatic method, none of the equations considered were suitable for use in the elderly Chinese population invested in our study. Further improved formulae are needed to assess GFR in elderly Chinese CKD patients. At present, based on both overall performance and performance in different CKD stages, the CG equation may be the most accurate for use in elderly Chinese patients with CKD.
Authors’ contributions
Contributions of each author: XL, CGS, ZJC, and TQL, planning of the project; XL, HT, and ZCY, performed the experimental work; XL, MHC, CW, JXC, and CLC, intellectual analysis of the data; XL, writing of the paper.
Acknowledgments
Project 81070612 was supported by the National Natural Science Foundation of China. This work was also supported by the China Postdoctoral Science Foundation (Grant No 201104335), the Guangdong Science and Technology Plan (Grant No 2011B031800084), and the Fundamental Research Funds for the Central Universities (Grant No 11ykpy38).
We would also like to thank the patients involved in this study for their cooperation.
Disclosure
The authors report no conflicts of interest in this work.
References
- ZhangQLRothenbacherDPrevalence of chronic kidney disease in population-based studies: systematic reviewBMC Public Health2008811718405348
- GargAXPapaioannouAFerkoNCampbellGClarkeJARayJGEstimating the prevalence of renal insufficiency in seniors requiring long-term careKidney Int200465264965314717937
- WasénEIsoahoRMattilaKVahlbergTKiveläSLIrjalaKEstimation of glomerular filtration rate in the elderly: a comparison of creatinine-based formulae with serum cystatin CJ Intern Med20042561707815189368
- China News AgencyAccording to the Chinese Academy of Social Sciences, aging degree of China will become the highest by the year 20302012 In Chinese. Available from: http://www.chinanews.com/gn/2010/09-10/2526415.shtmlAccessed September 12, 2012
- StevensLACoreshJGreeneTLeveyASAssessing kidney function – measured and estimated glomerular filtration rateN Engl J Med2006354232473248316760447
- LeveyASCoreshJBalkENational Kidney FoundationNational Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAnn Intern Med2003139213714712859163
- CarnevaleVPastoreLCamaioniMEstimate of renal function in oldest old inpatients by MDRD study equation, Mayo Clinic equation and creatinine clearanceJ Nephrol201023330631320155719
- XunLChengWHuaTAssessing glomerular filtration rate (GFR) in elderly Chinese patients with chronic kidney disease (CKD): a comparison of various predictive equationsArch Gerontol Geriatr2010511132019615764
- National Kidney FoundationK/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAm J Kidney Dis2002392 Suppl 1S1S26611904577
- LiJTXunCCuiCLRelative performance of two equations for estimation of glomerular filtration rate in a Chinese population having chronic kidney diseaseChin Med J (Engl)2012125459960322490481
- DUXLiuLHuBIs the Chronic Kidney Disease Epidemiology Collaboration four-level race equation better than the cystatin C equation?Nephrology (Carlton)201217440741422257305
- DuXHuBJiangLImplication of CKD-EPI equation to estimate glomerular filtration rate in Chinese patients with chronic kidney diseaseRen Fail201133985986521851197
- CarlsenOThe gamma camera as an absolute measurement device: determination of glomerular filtration rate in 99mTc-DTPA renography using a dual head gamma cameraNucl Med Commun200425101021102915381870
- CockcroftDWGaultMHPrediction of creatinine clearance from serum creatinineNephron197616131411244564
- LeveyASGreeneTKusekJWBeckGJGroupMSA simplified equation to predict glomerular filtration rate from serum creatinineJ Am Soc Nephrol200011SupplA0828
- LeveyASBoschJPLewisJBGreeneTRogersNRothDA more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study GroupAnn Intern Med1999130646147010075613
- LeveyASStevensLASchmidCHCKD-EPI (Chronic Kidney Disease Epidemiology Collaboration)A New Equation to Estimate Glomerular Filtration RateAnn Intern Med2009150960461219414839
- JelliffeRWLetter: Creatinine clearance: bedside estimateAnn Intern Med19737946046054748282
- HullJHHakLJKochGGWarginWAChiSLMattocksAMInfluence of range of renal function and liver disease on predictability of creatinine clearanceClin Pharmacol Ther19812945165217471619
- Du BoisDDu BoisEFA formula to estimate the approximate surface area if height and weight be known. 1916Nutrition1989553033112520314
- Dialysis and Transplantation Registration Group of Chinese Society of Nephrology of Chinese Medical AssociationThe report about the registration of dialysis and transplantation in China 1999Clin J Am Soc Nephrol20011727778
- LiuBCWuXCWangYLInvestigation of the prevalence of CKD in 13,383 Chinese hospitalised adult patientsClin Chim Acta20083871–212813218028892
- LindemanRDTobinJShockNWLongitudinal studies on the rate of decline in renal function with ageJ Am Geriatr Soc19853342782853989190
- GaultMHCockcroftDWLetter: Creatinine clearance and ageLancet19752793561261351444
- American Diabetes AssociationStandards of medical care in diabetes – 2010Diabetes Care201033Suppl 1S11S6120042772
- BevcSHojsREkartRGorenjakMPuklavecLSimple cystatin C formula compared to sophisticated CKD-EPI formulas for estimation of glomerular filtration rate in the elderlyTher Apher Dial201115326126821624073
- BurkhardtHHahnTGretzNGladischRBedside estimation of the glomerular filtration rate in hospitalized elderly patientsNephron Clin Pract20051011c1c815886493
- FabreEERaynaud-SimonAGolmardJLGourgouillonNBeaudeuxJLNivet-AntoineVInterest and limits of glomerular filtration rate (GFR) estimation with formulae using creatinine or cystatin C in the malnourished elderly populationArch Gerontol Geriatr2010503e55e5819552970
- CompanBdi CastriAPlazeJMArnaud-BattandierFEpidemiological study of malnutrition in elderly patients in acute, sub-acute and long-term care using the MNAJ Nutr Health Aging19993314615110823981
- LindemanRDAssessment of renal function in the old. Special considerationsClin Lab Med19931312692778462266
- GargAXBlakePGClarkWFClaseCMHaynesRBMoistLMAssociation between renal insufficiency and malnutrition in older adults: results from the NHANES IIIKidney Int20016051867187411703605
- GoldbergTHFinkelsteinMSDifficulties in estimating glomerular filtration rate in the elderlyArch Intern Med19871478143014333453695
- DonBRSchambelanMDiabetes, dietary protein and glomerular hyperfiltrationWest J Med198714744494552891223
- MogensenCERenal function changes in diabetesDiabetes197625Suppl 2872879971791
- NielsenSRehlingMSchmitzAMogensenCEValidity of rapid estimation of glomerular filtration rate in type 2 diabetic patients with normal renal functionNephrol Dial Transplant199914361561910193808
- MussapMDalla VestraMFiorettoPCystatin C is a more sensitive marker than creatinine for the estimation of GFR in type 2 diabetic patientsKidney Int20026141453146111918752
- LeveyASCoreshJGreeneTChronic Kidney Disease Epidemiology CollaborationUsing standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rateAnn Intern Med2006145424725416908915
- Van BiesenWVanholderRVeysNThe importance of standardization of creatinine in the implementation of guidelines and recommendations for CKD: implications for CKD management programmesNephrol Dial Transplant2006211778316221704