Abstract
Background
Incomplete bladder emptying (IBE) is defined as having a postvoid residual (PVR) urine volume greater than 100 mL for 2 consecutive days. IBE is common in stroke patients and could necessitate indwelling or intermittent catheterization. The condition is correlated with urinary tract infections, which could impede rehabilitation progress and increase medical costs. Treatment for patients with IBE includes bladder retraining, biofeedback, medication, and botulinum toxin injection, but none of these interventions are completely effective.
Methods
All patients with acute stroke who were admitted to the rehabilitation ward between August 2010 and April 2011 were included in the study and their PVR urine volume was checked. Electroacupuncture (EA; 1 Hz, 15 minutes) was performed on the acupoints Sanyinjiao (SP6), Ciliao (BL32), and Pangguangshu (BL28) of stroke patients with IBE for a total of ten treatments (five times a week for 2 weeks). Bladder diaries, which included the spontaneous voiding and PVR urine volumes, were recorded during the course of treatment.
Results
The presence of IBE was not related to sex, history of diabetes mellitus, stroke type (hemorrhagic or ischemic), or stroke location (P > 0.05). Among the 49 patients in the study, nine (18%) had IBE, and seven of the stroke patients with IBE were treated with EA. Increased spontaneous voiding volume and decreased PVR urine volume were noted after ten sessions of EA.
Conclusion
EA may have beneficial effects on stroke survivors with IBE, thereby making it a potential safe modality with which to improve urinary function.
Introduction
A high prevalence (44%–69%) of bladder dysfunction has been reported in stroke survivors; this includes urinary retention, incomplete bladder emptying (IBE), detrusor external sphincter dyssynergia, and bladder hyperactivity.Citation1 Urinary retention may occur in approximately 29% of the stroke patients in rehabilitation wards.Citation2 Catheterization is commonly performed to manage episodes of acute urinary retention in stroke survivors. However, indwelling catheters may affect rehabilitation activity or daily living, lead to urinary infection, and interfere with the reestablishment of a normal voiding pattern.Citation3 A significantly higher rate of urinary infection has been observed in individuals with IBE;Citation4 thus, indwelling catheters should be removed as soon as possible. The incidence of IBE is initially 56% in stroke patients, but it decreases to 32% over time.Citation4 The use of α-blockers may increase emptying, but side effects such as orthostatic hypotension may affect patient rehabilitation. Intermittent catheterization is another option for IBE management;Citation5 this procedure, however, is dependent on patient ability and family support.
Several studies on stroke survivors have suggested that acupuncture therapy provides significant benefits for stroke patients.Citation6–Citation11 Animal experiments have demonstrated that electroacupuncture (EA) could improve the bladder emptying function.Citation12,Citation13 Only a few high-quality studies have focused on this subject, and the lack of appropriate inclusion criteria or objective tools to assess the treatment effects of EA has been noted. One randomized trial demonstrated that the stimulation of acupuncture points could improve post-stroke urinary symptoms, but only moxibustion therapy was mentioned in their study.Citation14 Thus, we devised this prospective study to explore the improvement of the bladder emptying function in post-stroke patients after EA treatment.
Materials and methods
Patients
From August 2010 to April 2011, patients who were transferred from the neurology or neurosurgery wards to the rehabilitation ward in the China Medical University Hospital, Taichung, Taiwan, were considered for inclusion if they were diagnosed with infarction or hemorrhagic stroke for the first time and did not suffer from an active urinary tract infection. During the study enrollment period, the patients continued to receive conventional therapy (diet treatment, hypoglycemic agents, insulin, and hypertensive agents). No major changes were made to the prescribed medication during the study.
The specific inclusion criterion at enrollment was the presence of IBE, which was defined as having a postvoid residual (PVR) urine volume greater than 100 mL for 2 consecutive days at the rehabilitation ward.Citation15 Exclusion criteria included dermatitis over the acupuncture points and active urinary tract infection, as well as the prior use of anticholinergic drugs, cholinergic drugs, and α-blockers. All patients gave their informed consent, and the Institutional Review Board of the university approved the study.
Identification of acupuncture points
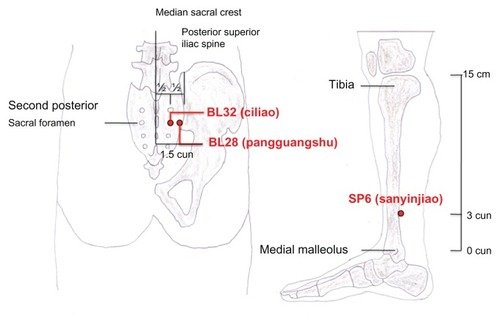
Three acupuncture points, namely Sanyinjiao (SP6), Ciliao (BL32), and Pangguangshu (BL28),Citation16 were selected for the treatment of IBE according to traditional Chinese medicine theories. In this study, the acupuncture points were identified by an experienced licensed acupuncturist, and the three acupuncture points were marked for subsequent study by the same acupuncturist using “cun”. Cun is the unit of measurement used for locating acupuncture points. One cun is equal to the space between the distal interphalangeal joint and the proximal interphalangeal joint on the middle finger. SP6 is located 3 cun above the tip of the medial malleolus. BL32 is located in the second posterior sacral foramen which in the depression, midway between the posterior superior iliac spine and the spinous process of the second sacral vertebra. BL28 is located at the same level, 1.5 cun lateral to the median sacral crest ().
Figure 1 Locations of acupuncture points based on the WHO standards for the Western Pacific region.Citation16 Redrawn by Yu and Chou.
Treatment procedures
The acupuncturist who had initially identified the acupuncture points likewise performed all the subsequent treatment procedures. Patients underwent treatment in a comfortable side-lying position. Prior to insertion of the acupuncture needle, the skin over the marked acupuncture point was cleaned with alcohol. Disposable acupuncture needles (Yuguang Industrial Co, Ltd, Taipei, Taiwan) (size #30; 0.28 mm in diameter) with a length of 1 inch (25.4 mm) or 1.5 inches (37 mm) were used for each patient. Six of the bilateral acupuncture points, specifically the pairs of SP6, BL32, and BL28, were connected to an electrostimulator (Ching Ming model-05B, Ching Ming Medical Device, Taipei, Taiwan) that produced biphasic square-shaped pulses at a low frequency (1 Hz, 3 mA to 60 mA) for 15 minutes. The treatment sessions were performed 5 days a week for 2 weeks.
Measurement of treatment outcomes
The basic clinical data of all patients were collected, including their age, sex, history of diabetes mellitus, stroke type, and stroke location. Bladder diaries were kept for each patient, which monitored parameters such as the spontaneous voiding and PVR urine volumes. These values were measured by a portable ultrasonic bladder scanner or by intermittent catheterization during the 10-day EA treatment.Citation17
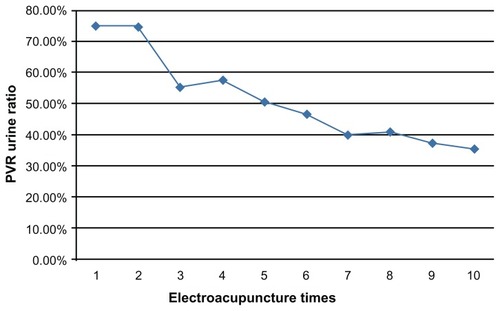
Effects of the EA treatment were presented in terms of the daily PVR urine ratio. This ratio was computed using the following equation: daily PVR urine ratio = (daily PVR urine volume/[daily PVR urine volume + spontaneous voiding volume]).
Statistical analyses
The arithmetic means of all values were used for the statistical methods in this study. All analyses were performed using the SPSS version 15 software (IBM Corporation, Armonk, NY). The categorical variables were analyzed using the χ2-test and Fisher’s exact test. Comparisons of numerical variables between patient groups were performed using the independent t-test. Values with P < 0.05 were considered statistically significant.
Results
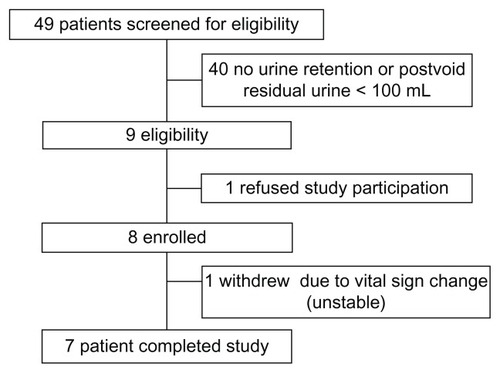
All patients with acute stroke who were admitted to the rehabilitation ward between August 2010 and April 2011 were included in this study. IBE occurred in 9 out of 49 patients (18%). The flow diagram of the study is shown in . For EA treatment, 7 out of the 9 eligible patients were enrolled and completed the study; their data were included in the analysis. One patient with IBE refused to participate; another withdrew due to pneumonia and was transferred to the intensive care unit.
The baseline patient characteristics are shown in and . Overall, the study population had a mean age of 65.67 years, and the majority of the participants were male. No significant associations were observed between the presence of IBE and each of the following parameters: sex, history of diabetes mellitus, stroke type (hemorrhagic or ischemic), and stroke location (P > 0.05).
Table 1 Demographic information of IBE and non-IBE patients
Table 2 Basic data of IBE patients who complete clinical trial
The arithmetic means of the daily PVR urine ratio of all patients during the 10 day EA treatment are presented in . The PVR urine ratio had the tendency to decrease as an effect of EA. IBE persisted in two of the patients after the EA treatment. A significant difference (P < 0.05) in the PVR urine volume of each patient was noted after the ten EA sessions.
Discussion
Effect of EA on urinary function
An increase in the spontaneous voiding volume and a decrease in the PVR urine volume were noted after the EA treatment. Thus, EA may have beneficial effects on stroke survivors with IBE and could be a safe modality for the improvement of urinary function.
Stroke and IBE
The two major and distinct functions of the bladder are urine storage and voiding. Burney et al reported that 28 out of 60 patients (47%) had urinary retention within 72 hours after stroke onset.Citation18 This high incidence rate was not surprising because the present study was performed during the acute stroke stage. The detrusor function gradually improves with time after the patient’s condition has stabilized.Citation19,Citation20 Kong and Young reported that urinary retention was present in 29% of patients at the subacute stage, which was observed after their admission to the rehabilitation ward within 4 weeks after stroke onset.Citation2
In our study, 18% (9 out of 49) of the stroke patients who were admitted to our rehabilitation ward had IBE. After the ten EA sessions, IBE persisted in only 28% (2 out of 7) of the patients. In a previous study, Garrett found that 58% (28 out of 48) of stroke patients who were admitted to a rehabilitation ward had sustained IBE at the time of discharge.Citation4 Another study on ischemic stroke patients showed that 17% of patients had sustained IBE at the time of discharge.Citation2 In the present study, all ischemic stroke patients could void without IBE after the 10-day treatment course of EA.
IBE management
For stroke survivors with urinary retention, catheterization is the most common treatment to relieve pain and distention. However, indwelling catheters may increase urinary tract infection rates or affect rehabilitation and daily living activities.Citation3 Thus, indwelling catheters should be removed as soon as possible. Intermittent catheterization is an alternative solution that could improve the vesical defense mechanisms and decrease the incidence of bacteriuria.Citation21 Moreover, intermittent catheterization could provide information on PVR urine. The actual determination of PVR urine volume after catheterization could aid in the prescription of a rational program for clean intermittent catheterization (CIC). However, a CIC program proves ineffective if the attendants and family members are unable to perform it. Other problems that were encountered with CIC included urethral trauma and occasional bladder stone formation.
The use of α-blockers may increase bladder emptying. However, the side effect of orthostatic hypotension may affect patient rehabilitation. The oral forms of these cholinergic agents have not been proven effective at levels that could be tolerated by patients.Citation22 Thus, EA could be an alternative method in the management of IBE.
Possible mechanisms of urinary retention via acupuncture treatment
Acupuncture is a safe form of treatment,Citation23 and several studies have suggested its beneficial effects on the treatment of stroke survivors.Citation24,Citation25 One study provided evidence that acupuncture may be clinically useful for improving bladder function in diabetics.Citation26 However, only a few high-quality studies have focused on IBE in stroke survivors. Moreover, the lack of appropriate inclusion criteria or objective tools to assess the treatment effects has been noted. Each acupuncture point has its distinct therapeutic actions. The acupuncture points used for EA treatment in this study, namely SP6, BL32, and BL28, improved the urinary function of patients.
Acupuncture could improve the voiding function by regulating the peripheral afferent nerve system. The locations of the two acupoints, BL28 and BL32, are similarly distributed along the S2–S4 dermatomes. The reflex voiding center lies at the S2 to S4 levels of the sacral spinal cord. BL28 and BL32 were stimulated by acupuncture to directly increase the excitability of the pelvic nerve, which consequently innervates the detrusor muscle. In addition, SP6 indirectly increases the excitability of the pelvic nerve.Citation27,Citation28 The increased detrusor pressure was previously observed after acupuncture treatment in animal experiments.Citation28 The improvement in voiding function as an effect of acupuncture treatment has been proven by clinical studies.Citation26,Citation28–Citation30
Either the mechanical action of an acupuncture needle or electrical point stimulation could achieve the appropriate stimulation of these acupuncture points.Citation31
Limitations of the study
The present study was only a preliminary study with several limitations. First, the small sample size limited the statistical power for subgroup analyses. Second, no patient follow-up was conducted for an extended time period to observe whether the effects of EA treatment are sustained. Finally, there was no randomized control group with which to compare the natural course of bladder function improvement. Control groups are very important for comparisons among patients and for the assessment of treatment modalities. The limited case numbers and ethical considerations required the use of the pre-treatment conditions of patients as the controls, which were subsequently compared with their posttreatment conditions. Further studies with larger sample sizes and longer follow-up periods are required to confirm the findings of this preliminary study.
Conclusion
In our study, the effects of EA treatment on the subjective symptoms as well as the objective PVR urine conditions provided evidence that EA may be clinically useful in the management of post-stroke IBE. Further studies with larger sample sizes are required to confirm the findings of this study and to determine the sustainability of the effects of EA treatment.
Disclosure
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article. This study was supported by a grant from of the China Medical University Hospital (DMR-100-107) and supported in part by Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH101-TD-B-111-004).
References
- BrittainKRPeetSMPotterJFCastledenCMPrevalence and management of urinary incontinence in stroke survivorsAge Ageing199928650951110604500
- KongKHYoungSIncidence and outcome of poststroke urinary retention: a prospective studyArch Phys Med Rehabil200081111464146711083349
- FronteraWRDeLisa’s Physical Medicine and Rehabilitation5th edPhiladelphiaLippincott Williams & Wilkins2011chapter 23569
- GarrettVEScottJACostichJAubreyDLGrossJBladder emptying assessment in stroke patientsArch Phys Med Rehabil198970141432916918
- FowlerCJNeurological disorders of micturition and their treatmentBrain1999122Pt 71213123110388789
- HopwoodVLewithGTDoes acupuncture help stroke patients become more independent?J Altern Complement Med200511117517715750379
- WuHTangJLinXAcupuncture for Stroke RehabilitationStroke132008 [Epub ahead of print.]
- LingZLin-baoGLian-fangCClinical study on early acupuncture for acuteischemic strokeJournal of Acupuncture and Tuina Science20086222226
- LiuSYHsiehCLWeiTSLiuPTChangYJLiTCAcupuncture stimulation improves balance function in stroke patients: a single-blinded controlled, randomized studyAm J Chin Med200937348349419606509
- ZhaoJGCaoCHLiuCZEffect of acupuncture treatment on spastic states of stroke patientsJ Neurol Sci20092761–214314718973910
- TangY-YLinC-HYuTYClinical evaluation in stroke patients for acupuncture and chinese manipulation combine with rehabilitation therapyJournal of Chinese Medicine2010211–25361
- BenHZuYYeYThe effect of electroacupuncture on the function of the partially denervated bladder in rabbitsZhen Ci Yan Jiu19931816872 (Chinese)8082284
- WangJHChenBGYinJWangGZouWGLuoXJEffect of electroacupuncture of different acupoints on the excitability of detrusor muscle and the expression of BDNF and TrkB in the spinal cord of rats with urinary retention due to spinal cord injuryZhen Ci Yan Jiu200934638739220209974
- YunSPJungWSParkSUEffects of moxibustion on the recovery of post-stroke urinary symptomsAm J Chin Med200735694795418186581
- MengNHLoSFChouLWYangPYChangCHChouECIncomplete bladder emptying in patients with stroke: is detrusor external sphincter dyssynergia a potential cause?Arch Phys Med Rehabil20109171105110920599050
- WHO Regional Office for the Western PacificWHO Standard Acupuncture Point Locations in the Western Pacific RegionManilaWorld Health Organization200872113115
- IretonRCKriegerJNCardenasDDBladder volume determination using a dedicated, portable ultrasound scannerJ Urol199014359099112184254
- BurneyTLSenapatiMDesaiSChoudharySTBadlaniGHAcute cerebrovascular accident and lower urinary tract dysfunction: a prospective correlation of the site of brain injury with urodynamic findingsJ Urol19961565174817508863586
- MaruACystometry and urethral pressure profilometry after cerebral strokeNihon Hinyokika Gakkai Zasshi1980712171183 (Japanese)7382230
- ArunabhMBadlaniUrologic problems in cerebrovascular accidentsProblems in Urology1993714153
- OrikasaSImaiYIgariDUrethral indwelling catheter, intermittent self-catheterization and urinary infectionNihon Hinyokika Gakkai Zasshi1991821118071816 (Japanese)1762270
- FinkbeinerAEIs bethanechol chloride clinically effective in promoting bladder emptying? A literature reviewJ Urol198513434434492863391
- LaoLSafety issues in acupunctureJ Altern Complement Med19962127319395638
- KjendahlASällströmSOstenPEStanghelleJKBorchgrevinkCFA one year follow-up study on the effects of acupuncture in the treatment of stroke patients in the subacute stage: a randomized, controlled studyClin Rehabil19971131922009360031
- LeeSYBaekYHParkSUIntradermal acupuncture on shen-men and nei-kuan acupoints improves insomnia in stroke patients by reducing the sympathetic nervous activity: a randomized clinical trialAm J Chin Med20093761013102119938212
- TongYJiaQSunYHouZWangYAcupuncture in the treatment of diabetic bladder dysfunctionJ Altern Complement Med200915890590919678782
- SatoASatoYSuzukiAMechanism of the reflex inhibition of micturition contractions of the urinary bladder elicited by acupuncture-like stimulation in anesthetized ratsNeurosci Res19921531891981336832
- Yue-laiCLeiZProgress of study on neural mechanism in acupuncture regulation of vesical functionsActa Universitatis Traditionis Medicalis Sinensis Pharmacologiaeque Shanghai2002166365
- YangDLAcupuncture therapy in 49 cases of postpartum urinary retentionJ Tradit Chin Med198551263849626
- ChengPTWongMKChangPLA therapeutic trial of acupuncture in neurogenic bladder of spinal cord injured patients – a preliminary reportSpinal Cord19983674764809670383
- HurtakJJAn overview of acupuncture medicineJ Altern Complement Med20028553553812470432