Abstract
COVID-19 pandemic significantly threatens the health and well-being of older adults. Aging-related changes, including multimorbidity, weakened immunity and frailty, may make older people more susceptible to severe infection and place them at higher risk of morbidity and mortality from COVID-19. Various quarantine measures have been implemented to control the spread of COVID-19. Nevertheless, such social distancing has disrupted routine health care practices, such as accessibility of medical services and long-term continuous care services. The medical management of older adults with multimorbidity is significantly afflicted by COVID-19. Older persons with frailty or multiple chronic disease may poorly adapt to the altered health care system, having detrimental consequences on their physical and mental health. COVID-19 pandemic has posed great challenges to the health of older adults. We highlighted the difficulties and obstacles of older adults during this unprecedented time. Also, we provided potential strategies and recommendations for actions to mitigate the COVID-19 pandemic threats. Certain strategies like community primary health care, medication delivery and home care support are adopted by many health facilities and caregivers, whereas other services such as internet hospital and virtual medical care are promoted to be accessible in many regions. However, guidelines and policies based on high-quality data are still needed for better health promotion of older groups with increasing resilience during the COVID-19 pandemic.
Introduction
The ongoing spread of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has posed immense threats to public health worldwide. COVID-19, the highly contagious and infectious disease, has resulted in more than 500 million confirmed cases and over 6.2 million deaths worldwide at the time of writing.Citation1 In the case of COVID-19, the aged population groups, often frail elderly with comorbidities, are significantly vulnerable to such pandemic with devastating morbidity and mortality rates.Citation2–4 It has been estimated that mortality rate of individuals aged 60 and 69 is 8.4%, and almost four times as much for those aged 80 and over, even though the average mortality rate was 3.4% globally.Citation5 According to a nationwide survey in China, the older adults aged over 60 years are comprised 31.2% of the confirmed cases and 81% of the total number of deaths.Citation6 The clinical spectrum of COVID-19 among the older adults is of great heterogeneity, ranging from asymptomatic infection to critical illness with multiple organ failure, and even death. Elderly patients infected with COVID-19 are frequently accompanied with long-term sequelae, including disability, cognitive impairment, and reduced immunity.Citation7,Citation8 Older adults have been significantly impacted by the COVID-19 pandemic. Despite the lockdown and quarantine measures slowing down the spread of SARS-CoV-2 transmission,Citation9 such strict disinfection measures, however, may threaten their physical and psychological well-being, leading to functional decline and low quality of life, which place older adults at particular risk for long-term adverse outcomes.Citation10 Given the vulnerability to SARS-CoV-2 infection and potentially devastating consequences of COVID-19, there are increasing concerns on the health care of the aging population. Social distancing and community containment gradually increase the risk of loneliness and social isolation, and disrupt routine medical activity among older individuals, with the negative consequences of health and function. COVID-19 specifically threatens the physical as well as psychological health of older adults and disrupts their routine health care.Citation11 The health care promotion for older adult during the public health emergency is now being brought to the forefront. Health care providers are obliged to adopt effective and innovative approaches to promote the overall health of older individuals. Several challenges have emerged during this unprecedented time, and the innovative strategies are being developed to overcome them. In this review, we aim to identify biological factors contributing to the increased vulnerability to the COVID-19 pandemic and summarize the geriatric health crisis that impede the older adults to maintain their health during the pandemic. To promote healthy aging, we also provide innovative and practical approach for health care providers to assist the older individuals to improve their multimorbidity management and resilience against COVID-19.
Age-Related Risk Factors for Vulnerability to COVID-19 Among Older Adults
With COVID-19 patients aged 65 and older showing striking trend of age-related increases in death, older age has been identified as a key player for the susceptibility and severity of COVID-19. Older adults are prone to be frail with multiple chronic diseases and reduced immunity, which may be responsible for this high vulnerability and severity of infections.Citation12
Chronic Diseases
In general, all population subsets are susceptible to COVID-19 infection, but aged individuals who suffer from multiple chronic diseases including hypertension, diabetes, obesity, coronary heart disease, chronic obstructive pulmonary disease and cancer, are particularly prone to be infected and hospitalized, and even have fatal outcomes from COVID-19.Citation13 With the prevalence increasing with advancing age, these chronic conditions play a pivotal role in altering immunity activities and driving inflammatory responses, which increase the vulnerability of the elderly to COVID-19 threats.Citation14 Type 2 diabetes mellitus (T2DM) is highly prevalent among older adults, aging patients with T2DM are vulnerable to various infection and developing more severe illness. The polymorphonuclear functions are severely impaired in these diabetic patients, such as chemotaxis, adherence, intracellular killing and altered T lymphocyte function. In addition, there is decreased antiviral response in patients with diminished interferon (IFN) production and pro-inflammatory cytokines.Citation15 The decreased host defense immunity and chronic inflammatory states, as the consequences of diabetic hyperglycemia, make patients more disposed to various infections caused by viruses, bacteria and fungi.Citation16 Notably, for the diabetic patients with COVID-19, poorly controlled glycemia and acute hyperglycemia are significantly associated with longer hospitalization, and increased mortality.Citation17 Hyperglycemia also leads to pathological changes in the lungs, including microangiopathy of alveolar capillaries, loss of elastic recoil and reduction of mucociliary clearance, which aggravate the lung infection.Citation18,Citation19 Cancer and malignant tumor can lead to the dysfunctions of immunity responses, and the corresponding treatment against cancer such as chemotherapy, radiotherapy as well as administration of immune-suppressive drugs, are further involved in immunity exhaustion.Citation20 The presence of cardiovascular diseases (CVD) is confirmed as a predominant risk factor for unfavorable outcomes in COVID-19 patients. The expression of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) entry proteins angiotensin-converting enzyme 2 (ACE-2) and transmembrane protease serine 2 (TMPRSS-2) is highly increased in patients with CVD.Citation21 In the same way, patients with chronic kidney disease (CKD) present heightened expressions of ACE-2 in renal tubular epithelial cells.Citation22 Increased ACE-2 facilitates direct viral invasion, which may possibly account for the high risk of older adults for SARS-CoV-2 infection and developing adverse outcomes from COVID-19. Therefore, SARS-CoV-2 may target many vital organs via attacking cells and provoke fatal damages, which aggravates the severity of primary disease.
Immunosenescence
Aging is an irreversible process with progressive deterioration in a variety of physiological systems, including the dysfunction of immune systems.Citation23 The immune systems generally play an essential role in defending against infection and maintaining the host homeostasis. As human age, their immune systems gradually represent the characteristics of declines in both innate and adaptive immune responses, known as immunosenescence. Immunosenescence in the aging population is significantly associated with increased susceptibility to various infections, reduced vaccination responses as well as raised incidence of autoimmunity, which lead to poor prognosis.Citation24–26 The major alternations of immunosenescence include, but not limited to, thymic involution, DNA damage, imbalance in naive and memory T cells, and dysregulation of immune receptors.Citation27 As a major source of all immune cells, hematopoietic stem cells (HSCs) undergo profound changes during aging, with reduced capabilities of proliferation and differentiation to maintain the appropriate proportions of lineage-specific precursors.Citation28 The senescence of HSCs has drastically impacted on the immune activities and different populations of immune cells.Citation23 T cells play a central role in the adaptive immunity and are highly affected by aging with declines in immune functions, such as orchestrating the responses of immune cells and mediating cytotoxicity toward the infected or damaged cells. In addition to the functional changes, the numbers of T cells show strong alternations with contraction of naive T cells and accumulation of memory T cells, which negatively influence their abilities in response to pathogens and viruses.Citation29 The antibody-producing B cells of aging individuals show low serum levels of immunoglobulin.Citation30 The natural killer cells (NKs) are the pivotal players in the innate immune defense, which undergo various alternations in both function and phenotype in the elderly. Senescent NKs exhibit decreased expression of activating receptors and impairment in cytotoxic activity, which fail to eliminate damaged cells and malignant.Citation23,Citation31 Meanwhile, the numbers of and macrophages and dendritic cells decreased with declined function.Citation32,Citation33
The age-related immune system deterioration induces in the increased susceptibility to SARS-CoV-2 infection. As a novel coronavirus with no prior immune response, SARS-CoV-2 is difficult to be eliminated by senescent immune activities, leading to the widespread transmission to COVID-19 in the geriatric population. Accumulating evidence has demonstrated that lymphocyte counts were remarkably decreased in the elderly patients with COVID-19, and the progressive declines in the number of peripheral blood lymphocytes generally indicate the severity and adverse outcomes of COVID-19 disease.Citation34,Citation35 Moreover, SARS-CoV-2 mainly results in respiratory infections, which can provoke or aggravate the clinical symptoms of other systems and make it more difficult to control development of infection.Citation36 In addition to the lack of immunocompetence, age-dependent defects in immune system also result in the poor vaccination responses. Indeed, the older individuals have decreased capability to response efficiently to antigens with reductions in the level of antibody responses.Citation37 The serum neutralization capacity and IgG or IgA antibody response after vaccination were significantly decreased in the elderly group, especially for individuals over 80 years old.Citation38,Citation39 The cytokines secreted by CD4 T cells, such as interferon-γ and interleukin-2, were much lower in older individuals compared to the healthy young population.Citation38 Taken together, immunosenescence is the key factor that contributes to the vulnerability to COVID-19 in the elderly.
Aging Frailty
Frailty is a common clinical syndrome associated with aging, which is characterized by reduced physiologic function across multiple organ system. Frailty may lead to progressive loss of homeostasis, increased susceptibility, and reduced resilience to minor stress.Citation40 Evidence shows that frailty is highly prevalent in older ages, albeit the variation of identifying frailty methods, the prevalence of frailty among the geriatric population is estimated to be 50%.Citation41,Citation42 Several studies have indicated that frailty is a negative prognostic factor of a range of adverse outcomes, including falling, unplanned hospitalization, disability and death.Citation43,Citation44 Older individuals with frailty are more susceptible to infectious diseases and at higher risk for developing severe consequences.Citation45,Citation46 Substantial evidence suggests that in elderly person, the frailty assessed by clinical frailty scale (CFS), can better predict the outcomes, than by age itself.Citation47,Citation48 The significant association has been further confirmed by a recent meta-analysis with a finding that each one-point increase in CFS was correlated with a 12% increase in mortality.Citation49
Older adults with frailty, who are known as physical inactive, are more predisposed to COVID-19 infection.Citation50 Physical frailty is characterized by weakness and exhaustion, which is associated with loss of muscle strength, decline in physical activity and excessive sedentary behavior. The routine activities of daily living and engagement in formal exercises have been abruptly disrupted among individuals with aging frailty.Citation51 It has been demonstrated that a reduction to 1500 steps per day for 14 days in older adults can lead to loss of approximately 4% leg fat-free mass and around 8% knee extension strength.Citation52,Citation53 In the context of the COVID-19 pandemic, despite positive effects on containing the spread of infection, the model of social isolation and home quarantine may further decrease the activity levels of older individuals. As a consequence, the accompanying adverse events, including exacerbation of muscle wasting, progression of sarcopenia and acceleration of comorbidities, represent an emerging problem.Citation54,Citation55
Frailty makes aging individuals more vulnerable to stressors, including infections, illness and injuries. In addition to physical dysfunction, older adults may simultaneously represent mild cognitive impairment, also known as cognitive frailty. It is the coexistence of physical frailty and shows decline in cognitive function without the presence of dementia.Citation56 Older adults with cognitive frailty have a higher prevalence to experience functional disability and significant cognitive decline, and may be more prone to be affected by “stay-at-home” restrictions.Citation51 Cognitive frailty may lead to alternations in autonomic nervous system activity, involving activation of autonomic nervous system and hypothalamic-pituitary-adrenal axis. The increased levels of norepinephrine and glucocorticoids levels caused by the autonomic unbalance, promoting the development of delirium.Citation57 The likelihood of frailty increases with age, making the older adults more vulnerable to this public health emergency. Aging frailty has been considered as a significantly negative factor for the poor prognosis of patients with COVID-19, independent of age and comorbidity.Citation48 Conversely, this infection disease results in irreversible frailty, which leads to new challenges for older adults to maintain their health.Citation58 Hence, given in the negative impact of frailty on health, the health issue of the aging individuals should be focused during this pandemic, and promotion of geriatric health care is critical to guarantee the health and well-being among the aging population.
Health Crisis of Older Adults During the COVID-19 Pandemic
It is well acknowledged that COVID-19 has drastically disrupted health care system across the globe, posing unprecedented challenges in elders with special need and routine medical care.Citation59 The limited accessibility to medical resources and decline in health care quality may lead to poor management of chronic diseases. Some infection control measures such as lockdown were conducted for the general populations, especially in the geriatric group, those with multiple comorbidities and others who are particularly vulnerable to the COVID-19.Citation60 However, without appropriate support, these measures can negatively affect their physical and psychological well-being, leading to serious clinical consequences.
Interruption to Routine Management of Chronic Diseases
With the rapid growth of aging population, it has been reported that approximately 80% of the older people have two or more chronic diseases, also known as multimorbidity.Citation61 Older patients with multimorbidity require robust health services that can provide continuous and long-term care. To reduce the high burden of chronic diseases, specialists and general practitioners have provided medical supports, such as prescription refills, adjustment of drug dosage, consecutive monitoring and education.Citation62 However, with the implementation of quarantine measures during the pandemic, older adults living with chronic conditions have great difficulties in managing chronic conditions and accessing to health care services.Citation63 Many health facilities have postponed or canceled outpatient visits of those with chronic diseases to reduce the transmission potential of SARS-CoV-2. In addition, many health care providers temporarily scaled down the wide range of health care services, including screenings, monitoring practices and consultations of chronic conditions for older adults.Citation64,Citation65 The poor management may lead to devastating consequence to elders with multimorbidity, particularly those with severe conditions. It has been reported a significant decline in screening and preventive services for the chronic conditions after the outbreak of COVID-19.Citation64 The numbers of in-person visits to outpatient facilities has been dramatically decreased.Citation59 The fear of contracting SARS-CoV-2 for routine follow-up of chronic medical conditions may negatively influence the care-seeking behavior of older persons in the midst of the pandemic.
Aging individuals with multiple comorbidities require integrated care involving social support, lifestyle modification, self-care and optimal medication to control diseases. For those patients with chronic diseases, the community practices for seeking adequate knowledge from general practitioners, such as exercise, nutrition and how to administrate medications (eg, the type of insulin, pump instructions), have been greatly affected during the current pandemic. For those patients requiring complex therapeutic regimens, the failure of regular monitoring and adjustment of prescription may increase the risk of presenting new symptoms and worsen current health conditions among older adults.Citation66 The lockdown measures affected visits to health facilities for medical care and life-saving treatment related to chronic diseases. Substantial evidence has indicated that the vulnerable groups are confronted with challenge in getting access to health care, obtaining consecutive follow-up visits and experiencing deteriorating pre-existing conditions due to fear of COVID-19 and restrictions.Citation67
The disruption in management of chronic diseases may also negatively influence medical adherence, which is essential for maintaining health conditions for the older adults.Citation68 However, the practice of medication adherence for the aging groups is challenging due to the widespread of COVID-19. Regional lockdown, social isolation, low income, and long travel distances to health care facilities, collectively leading to the limited access to medications.Citation69–71 To minimize the negative impact of COVID-19, several clinics have shifted the in-person visits to telemedicine; however, geriatric patients often have visual and hearing deficits, who may have difficulty in using electronic devices, making the implementation of telehealth challenging.Citation72 The poor adaptation to quarantine measures may impede their ability to obtain medications, and many older patients may self-manage or stop their medications for chronic diseases, which may ultimately lead to adverse health outcomes.Citation66,Citation73 Given in the disruption in chronic disease management and shortage of healthcare resources, a real concern over the long-term impacts of COVID-19 pandemic on the medical care of elders may become a nonnegligible threat to well-being of older adults.
Physical Inactivity
Considering that older adults are the most vulnerable population for serious illness and death, they are advised or even forced to stay at home to protect themselves from catching the virus. However, social exclusion has disrupted their daily routines lifestyles, such as reduced physical activities and increased sedentary behaviors. The decreased opportunities for either the incidental or intended physical activities can ultimately impair the function of skeletal muscle and lead to loss of intrinsic capacity. In this scenario, the sarcopenia, decline in physical function and low quality of life may likely be the consequences of the reduced levels of physical exercise for elders in response to COVID-19 pandemic.Citation74
Malnutrition
The altered dietary habit has also become a detrimental factor for malnutrition among older adults. Malnutrition is a common and serious condition which is influenced by several factors, such as living conditions, socioeconomic status, and physical environment.Citation75 Unemployment, soaring food prices and reduced external assistance restrict their access to adequate and nutritious food. Substantial evidence indicated that social isolation is an independent risk factor for malnutrition.Citation76–78 Due to the absence of support, a high proportion of elderly community dwellers would have trouble with instrumental activities of daily life, such as purchase of food and preparation of meals. Without social interaction, home confinement would lead to inadequate diet for the aging vulnerable group. Evidence indicated that food consumption and diet pattern were unhealthier during this pandemic, which placed them at high risk for poor nutritional status.Citation79 In addition, home-stay model decreased the time that older adults spent outside the door. Insufficient sunlight exposure contributes to vitamin D deficiency,Citation80 which predominantly aggravates the development of osteoporosis and other degenerative diseases among older adults. Furthermore, the overall mortality is increased.Citation81
Mental Disorders
COVID-19 has dramatically impacted the health of older adults, including their psychological well-being.Citation82 Despite efficacy of vaccinations, the rates of infection remain high due to incomplete protection afforded by vaccine,Citation83 social isolation is still considered to be the most effective approach to contain the spread of the new coronavirus. However, the isolative strategy may severely worsen the mental health conditions of older adults. Older adults make up one of the most vulnerable groups. It has been estimated that approximately 15% of the aging populations are struggling with psychiatric disorders or cognitive impairments.Citation84 Stay-at-home measures such as single and separated status are associated with the absence of social support, which ultimately leads to feelings of loneliness, anger and depression.Citation85–87 It has been reported that the time people are confined at home is coordinated with the high incidence of mental disorders.Citation88 In particular, the prolonged stress and sadness may increase the vulnerability for those living with mental disorders and precipitate the pre-existing psychiatric conditions.Citation89,Citation90 Furthermore, social disconnection places the elderly at higher risk of cognitive impairments with increasing trend of mortality.Citation91 Conversely, the mental disorders and cognitive impairments may aggravate the symptoms related to COVID-19 via increasing circulating pro-inflammatory cytokines.Citation85,Citation92 Extreme stress and insecurity due to isolation can also result in elevated level of corticosteroids and amplify the susceptibility to viral infections,Citation93 which have dramatically negative impacts on the health among older adults.
Strategies for Promoting Geriatric Health Care During the COVID-19 Pandemic
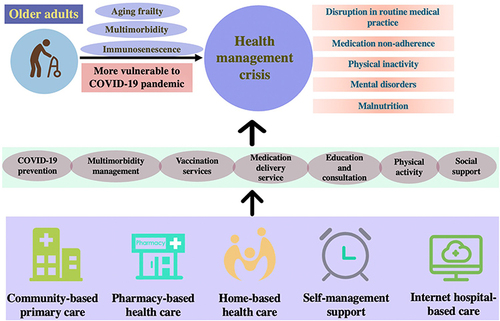
The COVID-19 crisis has brought unprecedented challenges to health care systems worldwide with a surge in medical care demands. As a highly contagious infectious disease, the COVID-19 has profoundly affected the well-being of individuals worldwide, leading to the exacerbation of demand for health care. With the vulnerable characteristics, the aging individuals are at higher risk from COVID-19 compared with the general persons. In the period of COVID-19 pandemic, the disruptions in health care delivery and shortages of medical resources have posed a significant challenge in elders who required routine medical care.Citation59,Citation94 Accumulating risks for suspension of routine medical practices, such as preventive services, routine monitoring and treatment would be significant over time. With the huge increase in healthcare demand for geriatric health service, the expansion of efforts is required to manage the demand, such as improving health care accessibilities and resources. Effective strategies that could mitigate long-term consequences related to COVID-19 pandemic has been recommended ().
Figure 1 The vulnerability of older adults during the COVID-19 pandemic: risk factors, health management crisis, effective and innovative strategies to promote geriatric health care.
Community-Based Primary Care
In the context of COVID-19, restriction policies to mitigate the virus transmission has hindered access to health services among the aging individuals. As hospital-based care was overwhelmed, the novel coronavirus pandemic highlighted the importance of community-based primary health care, which generally plays a pivotal role in promoting health and well-being. During this pandemic, primary health care has undertaken dual responsibilities to provide continuity of health service as well as respond to acute health system demand. As the “front door” of the health system, primary health care plays a crucial role in responding to health emergency management. Primary care professionals have been involved in initiatively screening the patients who visited primary health care facilities and tracking of COVID-19 contact in the community. The quick action would inevitably prevent COVID-19 transmission and protect the older vulnerable adults from infection.
In this era of restricted movement, the capability of community health care in responding to COVID-19 is relatively limited. WONCA, the global organization of family medicine, has advocated the ways in which the frontline primary care can coordinate with public health to deliver care during emergencies.Citation95 In the rural areas, the government should issue decisions on strengthening health care network and define the specific functions and tasks of primary health workers with clear guides.Citation96 In addition, they also collaborate with non-government organization to perform community-based health education, such as tracing, testing and treatment, which can help boost the performance of primary health care in managing the pandemic. Community service providers, especially the medical students, also play a pivotal role in supporting health communication programs and delivering education to the elderly at agencies, schools, and localities.Citation97 Of note, as the vaccination against SARS-CoV-2 is an effective approach to stop viral spread and control the pandemic, community health professionals have readiness to implement vaccination programs and provide vaccination services to older persons.Citation98 Also, annual influenza vaccinations are recommended to stimulate the immune system of older individuals and improve their capability to fight against infection.Citation10 During the pandemic, the primary care should also pay more attention to the non-COVID-19 care of older individuals isolated at home. For the older patients, the fear of visiting medical facilities and decline in health and definitively impede their health care seeking. Worse still, restriction on family visits may cut back on home support, so it is essential for physicians to take the initiative to inquire about their functional and social needs.Citation99 In addition, to provide the continuity of care for older dwellers, the primary care professionals have operated clinics and teleconsultation services designed for management of chronic diseases.Citation100,Citation101 In many countries, access to medicine was maintained through delivery services and health volunteers.Citation102 COVID-19 has strained the already weak health care system and almost stretched them beyond their capacity. Older adults are more vulnerable during the pandemic, and they are at higher risk of developing severe conditions. It is vital for primary care providers to assess an older adult’s health status and their resiliency in time. Regular follow-up visits in person or by phone, video and web-based communication are easily conducted by health care providers. Application of screening tools can improve the capability to identify the common signs of health condition and identify health care needs of the older adults during the COVID-19 pandemic (see ).
Table 1 Screening Tools to Evaluate the Health Conditions of Older Adults
In addition to routine practice of monitoring chronic conditions, the front-line care workers are forced to involve in identifying suspected COVID-19 patients and provide facilitators to pandemic response.Citation103,Citation104 As homebound individuals or suspected patients are lacking guidance on medications, health caregivers can provide professional instructions for them. Moreover, health care workers also provide emotional support for the community-dwelling older adults living alone. Moreover, primary care professionals also provide medical education, resources and social support to older adults. They can optimize the nutrition and consume protein to decrease the risk of malnutrition, sarcopenia and frailty.Citation105 Community social workers can facilitate operating local food delivery services to provide healthier food in line with dietary guidelines. Recommendations regarding sleep and physical activities should also be given to older adults to improve their well-being.Citation10 Community social workers may refer them to digital resources and assist them to engage in community virtual programs.Citation106 The utilization of technology and social media may be a useful strategy to strengthen the social connection and reduce loneliness of older adults.
Pharmacy-Based Health Care
Community pharmacies are mainly located in community health service centers in many countries. As an essential part in primary care system, community pharmacies involve in dispensing prescription medication and over-the-counter medication as well as health-related products. During the COVID-19 pandemic, the infectious disease has provoked a surge in demand for community pharmacy-based care. The scope of community pharmacies services has expanded from dispensing medication to pandemic prevention and control.Citation107 Community pharmacists exert a positive function as a bridge connecting primary care and community-dwellers to a certain extent. In accordance with guidance for pharmacists during the COVID-19 pandemic, community pharmacies play a key role in keeping adequate supply of daily medications and nutrients as well as providing pharmaceutical care to patients.Citation108 For homebound patients, home delivery services were offered by collaborating with social workers and drug companies so that older patients get adequate of their daily medications. Pharmacists also emphasize the significance of taking medications on time to make sure patients’ compliance.Citation109 They can ensure medication supply by sharing real-time information of drug availabilities and drug purchase on online platforms, which can effectively address medication nonadherence for caring older patients with chronic diseases.
As healthcare professionals, community pharmacists are highly responded to the pandemic. To promote the pandemic control, they provide reliable information and essential COVID-19 preventive products, such as masks, disinfectants and testing kits. In addition, pharmacies can provide services of screening body temperature to identify the suspected patients. In the time of that the aging individuals have limited approaches to acquire information on the scientific prevention and maintaining well-being, pharmacists provide consulting services, such as basic information on scientific prevention and various symptoms of COVID-19 to community-dwellers.Citation110 It is also notable that pharmacists should be professionally trained to improve quality of care and promote pandemic control.
Home Health Care
Community-dwelling older adults, particularly those who live alone, are highly prone to medication errors like discontinuation of medications or incorrected administration with over dosage. Illness-related barriers, including cognitive impairment, and functional deficits and mental disorders along with lack of access to facilities, have threatened the health of the elderly.Citation111,Citation112 Home-based care plays an essential role in providing health services to older individuals with comorbidities, which allows patients receive health care in their homes and maintain optimal health.Citation113 With the implementation of restriction policies, it is evident that the vulnerability of the older individuals is partially related to the absence of social support, but home-based health care can eliminate social isolation through bridging the gap between homebound older individuals and community.Citation113 In many countries, home-based care is provided by the care staffs, such as personal care providers, health care workers, nursing aides, who can provide medical information and heighten medication management and assist daily living activities. During the pandemic, there are alternations in the model of home care.
In the time of COVID-19, home care is prone to be performed via using telephone and videoconference, which can effectively mitigate the influence of COVID-19 infection on caregivers.Citation114 The utilization of telehealth is effective in multiple care procedures, such as reminding prescription, or evaluating conditions via queries, which is beneficial in severing the aging population presenting with complex chronic conditions.Citation103 Moreover, telehealth saves time and eliminates expenses of home caregivers in travel.Citation115 Nevertheless, for many community-dwelling older adults, lack of access to technological devices and scarce knowledge of artificial intelligence still pose challenge to the use of telehealth in home care.Citation116
Self-Management Support
The widespread of COVID-19 accelerates development of self-management among older persons. Older individuals with chronic conditions can provide routine medical self-care via utilization of telehealth and guidance with professional physicians to reduce the impact of disease on health status.Citation117,Citation118 The daily tasks that older patients undertake include measuring their blood pressure, monitoring blood glucose and maintaining insulin regimen, etc. Moreover, it is essential for them to self-manage their daily health behaviors, including healthy diet, physical activities, mental health state, weight control, and so forth. However, lack of knowledge, poor social support and ineffective physician communication may make many older patients have difficulties in self-managing their chronic conditions.Citation119 With the development of telehealth, older adults with chronic diseases can access health services, grasp health management skills and enhance communication with health care providers. A wide range of digital health programs are applied to support self-management, which include self-monitoring and professional evaluations, decision support, 24-hour access lines, education programs, digital depression intervention and rehabilitation support. With the rapid increase in the utilization of technologies, e-health care may exert a significant effect on managing health in the future.Citation120
As regard to physical activity, it is appropriate for homebound older adults to perform at home. As is well known, proper physical activity is essential for maintaining well-being and physical function for older adults. A line of evidence indicates that people living sedentary lifestyles have elevated mortality of mortality and hospitalization from infections.Citation121 However, during the COVID-19 pandemic, quarantine policies including social distancing, stay-at-home model, have fostered the decondition of physical inactivity for older individuals. Therefore, it is significant to encourage appropriate physical activity to assist with management of the chronic diseases and increase the immune responses to combat the SARS-COV-2 infection and fight against physical and mental consequences of COVID-19.Citation122,Citation123 It has been recommended that the multicomponent exercise program including aerobic, resistance, balance, coordination and mobility training exercises is appropriate for older people confined at home.Citation122,Citation124,Citation125 The guidelines recommend 5 to 7 days per week of physical exercises to compensate for the decline in the levels of daily activity in this quarantine situation. To be more specific, a minimum of 150 to 300 min per week of aerobic exercise and twice resistance training program per week are required to maintain health. In mobility training exercise, balance and coordination should be distributed among the training days.
Internet Hospital-Based Care
With the rapid development of technologies and increasing popularity of artificial intelligence products, telemedicine care model has been made accessible to the public.
Internet hospital is an online platform that links the complex network of medical consulting clinics, primary health centers, secondary and tertiary hospitals, and large pharmacy stores.Citation126 During the COVID-19 crisis, internet hospital is well developed and greatly popularized by the public, because it not only allows older patients to access real-time information, specialists and treatments but also empowers specialists to practice prescriptions, recommendations to patients without distance barriers. Internet hospital is a promising avenue to connect doctors and patients due to the convenience and ubiquity of technology.Citation127 During the widespread of COVID-19, internet hospital also serves multiple significant functions in epidemic counselees, provide medical supports and enhance self-protection of individuals.Citation128 The widespread of this model can help to reduce viral transmission and maintain the health of older patients with chronic diseases.
Conclusions
The COVID-19 pandemic is placing an unprecedented strain on health care systems worldwide, leading to the negligence of care on aging populations whose management has become worsening with the pandemic. Increased incidence of chronic diseases, immunosenescence, and frailty, presenting as the characteristics of aging individuals, may decrease their resilience to COVID-19 and make them vulnerable to the potential threats from social distancing, which may exacerbate negative long-term impacts on their physical and psychological health outcomes. It is an urgent time for health care providers to pay attention to their non-COVID-19 care. In this scenario, the contribution of primary health care professionals and pharmacists in managing multimorbidity and promoting continuous care at the frontline is the cornerstone to alleviate the heavy burden on health systems. Home care can be conducted by skilled caregivers to provide essential support for vulnerable older individuals. In particular, exploring innovative strategies such as integrating internet hospital into health-care services is also critical to ensuring continuous care of older adults. With the uncertain continuation of this pandemic, more effective guidelines and strategies that help to avoid threats of COVID-19 and promote overall geriatric health are needed.
Disclosure
The authors declare no conflicts of interest in this work.
Additional information
Funding
References
- World Health Organization. WHO coronavirus (COVID-19) dashboard; 2022.
- Gao YD, Ding M, Dong X, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76(2):428–455. doi:10.1111/all.14657
- Zhang JJ, Cao YY, Tan G, et al. Clinical, radiological, and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients. Allergy. 2021;76(2):533–550. doi:10.1111/all.14496
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi:10.1001/jama.2020.6775
- Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi:10.1016/s0140-6736(20)30627-9
- CDC Weekly C; The Novel Coronavirus Pneumonia Emergency Response Epidemiology T. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) - China, 2020. China CDC Wkly. 2020;2(8):113–122. doi:10.46234/ccdcw2020.032
- Lithander FE, Neumann S, Tenison E, et al. COVID-19 in older people: a rapid clinical review. Age Ageing. 2020;49(4):501–515. doi:10.1093/ageing/afaa093
- Chen Y, Klein SL, Garibaldi BT, et al. Aging in COVID-19: vulnerability, immunity and intervention. Ageing Res Rev. 2021;65:101205. doi:10.1016/j.arr.2020.101205
- Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2). doi:10.1093/jtm/taaa020
- Batsis JA, Daniel K, Eckstrom E, et al. Promoting healthy aging during COVID-19. J Am Geriatr Soc. 2021;69(3):572–580. doi:10.1111/jgs.17035
- Beckman AL, Mechanic RE, Shah TB, Figueroa JF. Accountable Care Organizations during Covid-19: routine care for older adults with multiple chronic conditions. Healthc. 2021;9(1):100511. doi:10.1016/j.hjdsi.2020.100511
- Promislow DEL. A geroscience perspective on COVID-19 mortality. J Gerontol a Biol Sci Med Sci. 2020;75(9):e30–e33. doi:10.1093/gerona/glaa094
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
- Ajebli M, Amssayef A, Akdad M, et al. Chronic Diseases and COVID-19: a Review. Endocr Metab Immune Disord Drug Targets. 2021;21(10):1781–1803. doi:10.2174/1871530320666201201110148
- Summers KL, Marleau AM, Mahon JL, McManus R, Hramiak I, Singh B. Reduced IFN-alpha secretion by blood dendritic cells in human diabetes. Clin Immunol. 2006;121(1):81–89. doi:10.1016/j.clim.2006.05.015
- van Crevel R, van de Vijver S, Moore DAJ. The global diabetes epidemic: what does it mean for infectious diseases in tropical countries? Lancet Diabetes Endocrinol. 2017;5(6):457–468. doi:10.1016/s2213-8587(16)30081-x
- Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31(6):1068–1077.e3. doi:10.1016/j.cmet.2020.04.021
- Kolahian S, Leiss V, Nürnberg B. Diabetic lung disease: fact or fiction? Rev Endocr Metab Disord. 2019;20(3):303–319. doi:10.1007/s11154-019-09516-w
- Rajpal A, Rahimi L, Ismail-Beigi F. Factors leading to high morbidity and mortality of COVID-19 in patients with type 2 diabetes. J Diabetes. 2020;12(12):895–908. doi:10.1111/1753-0407.13085
- Russell B, Moss C, George G, et al. Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence. Ecancermedicalscience. 2020;14:1022. doi:10.3332/ecancer.2020.1022
- Chung MK, Zidar DA, Bristow MR, et al. COVID-19 and cardiovascular disease: from bench to bedside. Circ Res. 2021;128(8):1214–1236. doi:10.1161/circresaha.121.317997
- Lely AT, Hamming I, van Goor H, Navis GJ. Renal ACE2 expression in human kidney disease. J Pathol. 2004;204(5):587–593. doi:10.1002/path.1670
- Borgoni S, Kudryashova KS, Burka K, de Magalhães JP. Targeting immune dysfunction in aging. Ageing Res Rev. 2021;70:101410. doi:10.1016/j.arr.2021.101410
- McElhaney JE. Influenza vaccine responses in older adults. Ageing Res Rev. 2011;10(3):379–388. doi:10.1016/j.arr.2010.10.008
- Dock JN, Effros RB. Role of CD8 T cell replicative senescence in human aging and in HIV-mediated immunosenescence. Aging Dis. 2011;2(5):382–397.
- Ostan R, Bucci L, Capri M, et al. Immunosenescence and immunogenetics of human longevity. Neuroimmunomodulation. 2008;15(4–6):224–240. doi:10.1159/000156466
- Mittelbrunn M, Kroemer G. Hallmarks of T cell aging. Nat Immunol. 2021;22(6):687–698. doi:10.1038/s41590-021-00927-z
- Pang WW, Price EA, Sahoo D, et al. Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age. Proc Natl Acad Sci USA. 2011;108(50):20012–20017. doi:10.1073/pnas.1116110108
- Quinn KM, Fox A, Harland KL, et al. Age-related decline in primary CD8(+) T cell responses is associated with the development of senescence in virtual memory CD8(+) T cells. Cell Rep. 2018;23(12):3512–3524. doi:10.1016/j.celrep.2018.05.057
- Han S, Yang K, Ozen Z, et al. Enhanced differentiation of splenic plasma cells but diminished long-lived high-affinity bone marrow plasma cells in aged mice. J Immunol. 2003;170(3):1267–1273. doi:10.4049/jimmunol.170.3.1267
- Camous X, Pera A, Solana R, Larbi A. NK cells in healthy aging and age-associated diseases. J Biomed Biotechnol. 2012;2012:195956. doi:10.1155/2012/195956
- Stout RD, Suttles J. Immunosenescence and macrophage functional plasticity: dysregulation of macrophage function by age-associated microenvironmental changes. Immunol Rev. 2005;205:60–71. doi:10.1111/j.0105-2896.2005.00260.x
- Uyemura K, Castle SC, Makinodan T. The frail elderly: role of dendritic cells in the susceptibility of infection. Mech Ageing Dev. 2002;123(8):955–962. doi:10.1016/s0047-6374(02)00033-7
- Li X, Marmar T, Xu Q, et al. Predictive indicators of severe COVID-19 independent of comorbidities and advanced age: a nested case-control study. Epidemiol Infect. 2020;148:e255. doi:10.1017/s0950268820002502
- Zhou Z, Zhang M, Wang Y, et al. Clinical characteristics of older and younger patients infected with SARS-CoV-2. Aging. 2020;12(12):11296–11305. doi:10.18632/aging.103535
- Chen Q, Wang L, Yu W, et al. Recommendations for the prevention and treatment of the novel coronavirus pneumonia in the elderly in China. Aging Med. 2020;3(2):66–73. doi:10.1002/agm2.12113
- Ciabattini A, Nardini C, Santoro F, Garagnani P, Franceschi C, Medaglini D. Vaccination in the elderly: the challenge of immune changes with aging. Semin Immunol. 2018;40:83–94. doi:10.1016/j.smim.2018.10.010
- Collier DA, Ferreira I, Kotagiri P, et al. Age-related immune response heterogeneity to SARS-CoV-2 vaccine BNT162b2. Nature. 2021;596(7872):417–422. doi:10.1038/s41586-021-03739-1
- Li J, Hui A, Zhang X, et al. Safety and immunogenicity of the SARS-CoV-2 BNT162b1 mRNA vaccine in younger and older Chinese adults: a randomized, placebo-controlled, double-blind Phase 1 study. Nat Med. 2021;27(6):1062–1070. doi:10.1038/s41591-021-01330-9
- Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. doi:10.1016/s0140-6736(19)31785-4
- Hoogendijk EO, Suanet B, Dent E, Deeg DJ, Aartsen MJ. Adverse effects of frailty on social functioning in older adults: results from the Longitudinal Aging Study Amsterdam. Maturitas. 2016;83:45–50. doi:10.1016/j.maturitas.2015.09.002
- Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. 2018;3(7):e323–e332. doi:10.1016/s2468-2667(18)30091-4
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–56. doi:10.1093/gerona/56.3.m146
- Walston J, Robinson TN, Zieman S, et al. Integrating frailty research into the medical specialties-report from a U13 conference. J Am Geriatr Soc. 2017;65(10):2134–2139. doi:10.1111/jgs.14902
- Vetrano DL, Triolo F, Maggi S, et al. Fostering healthy aging: the interdependency of infections, immunity and frailty. Ageing Res Rev. 2021;69:101351. doi:10.1016/j.arr.2021.101351
- Kundi H, Wadhera RK, Strom JB, et al. Association of frailty with 30-day outcomes for acute myocardial infarction, heart failure, and pneumonia among elderly adults. JAMA Cardiol. 2019;4(11):1084–1091. doi:10.1001/jamacardio.2019.3511
- Prendki V, Tiseo G, Falcone M. Caring for older adults during the COVID-19 pandemic. Clin Microbiol Infect. 2022;28:785–791. doi:10.1016/j.cmi.2022.02.040
- Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5(8):e444–e451. doi:10.1016/s2468-2667(20)30146-8
- Pranata R, Henrina J, Lim MA, et al. Clinical frailty scale and mortality in COVID-19: a systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2021;93:104324. doi:10.1016/j.archger.2020.104324
- Roschel H, Artioli GG, Gualano B. Risk of increased physical inactivity during COVID-19 outbreak in older people: a call for actions. J Am Geriatr Soc. 2020;68(6):1126–1128. doi:10.1111/jgs.16550
- Murukesu RR, Singh DKA, Shahar S, Subramaniam P. Physical activity patterns, psychosocial well-being and coping strategies among older persons with cognitive frailty of the ”WE-RISE” trial throughout the COVID-19 movement control order. Clin Interv Aging. 2021;16:415–429. doi:10.2147/cia.S290851
- Breen L, Stokes KA, Churchward-Venne TA, et al. Two weeks of reduced activity decreases leg lean mass and induces ”anabolic resistance” of myofibrillar protein synthesis in healthy elderly. J Clin Endocrinol Metab. 2013;98(6):2604–2612. doi:10.1210/jc.2013-1502
- Reidy PT, McKenzie AI, Mahmassani Z, et al. Skeletal muscle ceramides and relationship with insulin sensitivity after 2 weeks of simulated sedentary behaviour and recovery in healthy older adults. J Physiol. 2018;596(21):5217–5236. doi:10.1113/jp276798
- Wall BT, Dirks ML, van Loon LJ. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12(4):898–906. doi:10.1016/j.arr.2013.07.003
- Hartley P, Costello P, Fenner R, et al. Change in skeletal muscle associated with unplanned hospital admissions in adult patients: a systematic review and meta-analysis. PLoS One. 2019;14(1):e0210186. doi:10.1371/journal.pone.0210186
- Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging. 2013;17(9):726–734. doi:10.1007/s12603-013-0367-2
- Boccardi M, Boccardi V. Silent cognitive frailty at the interplay between delirium and COVID-19. Asian J Psychiatr. 2021;57:102565. doi:10.1016/j.ajp.2021.102565
- Franceschi C, Capri M, Monti D, et al. Inflammaging and anti-inflammaging: a systemic perspective on aging and longevity emerged from studies in humans. Mech Ageing Dev. 2007;128(1):92–105. doi:10.1016/j.mad.2006.11.016
- Baum A, Kaboli PJ, Schwartz MD. Reduced In-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129–131. doi:10.7326/m20-3026
- Roy J, Jain R, Golamari R, Vunnam R, Sahu N. COVID-19 in the geriatric population. Int J Geriatr Psychiatry. 2020;35(12):1437–1441. doi:10.1002/gps.5389
- Kramer BJ, Cleary JF, Mahoney JE. Enhancing palliative care for low-income elders with chronic disease: feasibility of a hospice consultation model. J Soc Work End Life Palliat Care. 2014;10(4):356–377. doi:10.1080/15524256.2014.975088
- Syed ST, Sharp LK, Kim Y, et al. Relationship between medication adherence and distance to dispensing pharmacies and prescribers among an urban Medicaid population with diabetes mellitus. Pharmacotherapy. 2016;36(6):590–597. doi:10.1002/phar.1757
- Chan EYY, Kim JH, Lo ESK, et al. What happened to people with non-communicable diseases during COVID-19: implications of H-EDRM policies. Int J Environ Res Public Health. 2020;17(15):5588. doi:10.3390/ijerph17155588
- Wright A, Salazar A, Mirica M, Volk LA, Schiff GD. The invisible epidemic: neglected chronic disease management during COVID-19. J Gen Intern Med. 2020;35(9):2816–2817. doi:10.1007/s11606-020-06025-4
- Hartmann-Boyce J, Morris E, Goyder C, et al. Diabetes and COVID-19: risks, management, and learnings from other national disasters. Diabetes Care. 2020;43(8):1695–1703. doi:10.2337/dc20-1192
- Palmer K, Monaco A, Kivipelto M, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32(7):1189–1194. doi:10.1007/s40520-020-01601-4
- Singh K, Kondal D, Mohan S, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021;21(1):685. doi:10.1186/s12889-021-10708-w
- Kretchy IA, Asiedu-Danso M, Kretchy JP. Medication management and adherence during the COVID-19 pandemic: perspectives and experiences from low-and middle-income countries. Res Social Adm Pharm. 2021;17(1):2023–2026. doi:10.1016/j.sapharm.2020.04.007
- Karter AJ, Parker MM, Moffet HH, et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care. 2004;42(2):110–115. doi:10.1097/01.mlr.0000109023.64650.73
- Schectman JM, Schorling JB, Voss JD. Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med. 2008;23(10):1685–1687. doi:10.1007/s11606-008-0747-1
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi:10.1007/s10900-013-9681-1
- Gruss J, Smith CH. Demonstrating the vital role of physiatry throughout the health care continuum: lessons learned from the impacts of the COVID-19 pandemic on skilled nursing facilities. Pm r. 2021;13(6):563–571. doi:10.1002/pmrj.12609
- Nguyen HL, Tran OT, Ha DA, et al. Impact of the COVID-19 pandemic on clinical research activities: survey of study participants and health care workers participating in a hypertension trial in Vietnam. PLoS One. 2021;16(7):e0253664. doi:10.1371/journal.pone.0253664
- Machado CLF, Pinto RS, Brusco CM, Cadore EL, Radaelli R. COVID-19 pandemic is an urgent time for older people to practice resistance exercise at home. Exp Gerontol. 2020;141:111101. doi:10.1016/j.exger.2020.111101
- Jensen GL, McGee M, Binkley J. Nutrition in the elderly. Gastroenterol Clin North Am. 2001;30(2):313–334. doi:10.1016/s0889-8553(05)70184-9
- Kalousova L. Social isolation as a risk factor for inadequate diet of older Eastern Europeans. Int J Public Health. 2014;59(5):707–714. doi:10.1007/s00038-014-0582-6
- Boulos C, Salameh P, Barberger-Gateau P. Social isolation and risk for malnutrition among older people. Geriatr Gerontol Int. 2017;17(2):286–294. doi:10.1111/ggi.12711
- Delerue Matos A, Barbosa F, Cunha C, Voss G, Correia F. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults. BMC Public Health. 2021;21(1):924. doi:10.1186/s12889-021-10956-w
- Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. doi:10.3390/nu12061583
- Palaniswamy S, Hyppönen E, Williams DM, et al. Potential determinants of vitamin D in Finnish adults: a cross-sectional study from the Northern Finland birth cohort 1966. BMJ Open. 2017;7(3):e013161. doi:10.1136/bmjopen-2016-013161
- Wei J, Zhu A, Ji JS, Comparison A. Study of Vitamin D deficiency among older adults in China and the United States. Sci Rep. 2019;9(1):19713. doi:10.1038/s41598-019-56297-y
- Sutton E, Catling J, Segaert K, Veldhuijzen van Zanten J. cognitive health worries, reduced physical activity and fewer social interactions negatively impact psychological wellbeing in older adults during the COVID-19 pandemic. Front Psychol. 2022;13:823089. doi:10.3389/fpsyg.2022.823089
- Schmidt AL, Labaki C, Hsu CY, et al. COVID-19 vaccination and breakthrough infections in patients with cancer. Ann Oncol. 2022;33(3):340–346. doi:10.1016/j.annonc.2021.12.006
- Reed PG, Boyd M, Buckwalter KC. Mental health of older adults. West J Nurs Res. 1989;11(2):143–163. doi:10.1177/019394598901100202
- Grolli RE, Mingoti MED, Bertollo AG, et al. Impact of COVID-19 in the mental health in elderly: psychological and biological updates. Mol Neurobiol. 2021;58(5):1905–1916. doi:10.1007/s12035-020-02249-x
- Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi:10.1016/s2215-0366(20)30046-8
- Wang C, Tee M, Roy AE, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16(2):e0246824. doi:10.1371/journal.pone.0246824
- Yang XY, Peng S, Yang T, Cottrell RR. Changing trends of mental and behavioral responses and associations during the COVID-19 epidemic in China: a panel study. Health Educ Res. 2021;36(2):151–158. doi:10.1093/her/cyab012
- Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi:10.1016/s2215-0366(20)30090-0
- Russell G, Lightman S. The human stress response. Nat Rev Endocrinol. 2019;15(9):525–534. doi:10.1038/s41574-019-0228-0
- Friedler B, Crapser J, McCullough L. One is the deadliest number: the detrimental effects of social isolation on cerebrovascular diseases and cognition. Acta Neuropathol. 2015;129(4):493–509. doi:10.1007/s00401-014-1377-9
- Parisi V, Leosco D. Precision medicine in COVID-19: IL-1β a potential target. JACC Basic Transl Sci. 2020;5(5):543–544. doi:10.1016/j.jacbts.2020.04.006
- Yan C, Luo Z, Li W, et al. Disturbed Yin-Yang balance: stress increases the susceptibility to primary and recurrent infections of herpes simplex virus type 1. Acta Pharm Sin B. 2020;10(3):383–398. doi:10.1016/j.apsb.2019.06.005
- Ismail H, Marshall VD, Patel M, Tariq M, Mohammad RA. The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J Am Pharm Assoc. 2021. doi:10.1016/j.japh.2021.11.013
- de Lusignan S, Correa A, Smith GE, et al. RCGP research and surveillance centre: 50 years’ surveillance of influenza, infections, and respiratory conditions. Br J Gen Pract. 2017;67(663):440–441. doi:10.3399/bjgp17X692645
- Tran BX, Phan HT, Nguyen TPT, et al. Reaching further by Village Health Collaborators: the informal health taskforce of Vietnam for COVID-19 responses. J Glob Health. 2020;10(1):010354. doi:10.7189/jogh.10.010354
- Le HT, Mai HT, Pham HQ, et al. Feasibility of intersectoral collaboration in epidemic preparedness and response at grassroots levels in the threat of COVID-19 pandemic in Vietnam. Front Public Health. 2020;8:589437. doi:10.3389/fpubh.2020.589437
- Akbar MA, Juniarti N, Yamin A. The roles of community health nurses’ in covid-19 management in Indonesia: a qualitative study. Int J Community Based Nurs Midwifery. 2022;10(2):96–109. doi:10.30476/ijcbnm.2021.90884.1739
- Steinman MA, Perry L, Perissinotto CM. Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern Med. 2020;180(6):819–820. doi:10.1001/jamainternmed.2020.1661
- Mistry SK, Ali A, Akther F, Yadav UN, Harris MF. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Global Health. 2021;17(1):47. doi:10.1186/s12992-021-00698-0
- Gummidi B, John O, Jha V. Continuum of care for non-communicable diseases during COVID-19 pandemic in rural India: a mixed methods study. J Family Med Prim Care. 2020;9(12):6012–6017. doi:10.4103/jfmpc.jfmpc_1805_20
- Yadav UN, Mistry SK, Ghimire S, et al. Recognizing the roles of primary health care in addressing non-communicable diseases in low- and middle-income countries: lesson from COVID-19, implications for the future. J Glob Health. 2021;11:03120. doi:10.7189/jogh.11.03120
- Ruíz-Fernández MD, Fernández-Medina IM, Gálvez Ramírez F, Granero-Molina J, Fernández-Sola C, Hernández-Padilla JM. Experiences of home care nurses during the COVID-19 pandemic. Nurs Res. 2022;71(2):111–118. doi:10.1097/nnr.0000000000000566
- García JMM, Izquierdo JA, Pérez MIG. [COVID-19 in Spain, how did we get here?] COVID-19 en España, ¿cómo hemos llegado hasta aquí? Aten Primaria. 2020;52(10):676–679. Spanish. doi:10.1016/j.aprim.2020.10.003
- Visser M, Schaap LA, Wijnhoven HAH. Self-reported impact of the COVID-19 pandemic on nutrition and physical activity behaviour in Dutch older adults living independently. Nutrients. 2020;12(12):3708. doi:10.3390/nu12123708
- Berg-Weger M, Morley JE. Editorial: loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging. 2020;24(5):456–458. doi:10.1007/s12603-020-1366-8
- Zheng SQ, Yang L, Zhou PX, Li HB, Liu F, Zhao RS. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: a China perspective. Res Social Adm Pharm. 2021;17(1):1819–1824. doi:10.1016/j.sapharm.2020.03.012
- Aruru M, Truong HA, Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Social Adm Pharm. 2021;17(1):1967–1977. doi:10.1016/j.sapharm.2020.04.002
- Visacri MB, Figueiredo IV, Lima TM. Role of pharmacist during the COVID-19 pandemic: a scoping review. Res Social Adm Pharm. 2021;17(1):1799–1806. doi:10.1016/j.sapharm.2020.07.003
- Kambayashi D, Manabe T, Kawade Y, Hirohara M. Knowledge, attitudes, and practices regarding COVID-19 among pharmacists partnering with community residents: a national survey in Japan. PLoS One. 2021;16(10):e0258805. doi:10.1371/journal.pone.0258805
- Thiruchselvam T, Naglie G, Moineddin R, et al. Risk factors for medication nonadherence in older adults with cognitive impairment who live alone. Int J Geriatr Psychiatry. 2012;27(12):1275–1282. doi:10.1002/gps.3778
- Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. doi:10.1016/j.amjopharm.2011.02.004
- Westra BL, Paitich N, Ekstrom D, et al. Getting on with living life: experiences of older adults after home care. Home Healthc Nurse. 2013;31(9):493–501. doi:10.1097/NHH.0b013e3182a87654
- Osakwe ZT. Home care and use of telehealth amidst the COVID-19 pandemic. Home Healthc Now. 2020;38(4):229–230. doi:10.1097/nhh.0000000000000900
- Hickey S, Gomez J, Meller B, et al. Interactive home telehealth and burns: a pilot study. Burns. 2017;43(6):1318–1321. doi:10.1016/j.burns.2016.11.013
- Hirko KA, Kerver JM, Ford S, et al. Telehealth in response to the COVID-19 pandemic: implications for rural health disparities. J Am Med Inform Assoc. 2020;27(11):1816–1818. doi:10.1093/jamia/ocaa156
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–187. doi:10.1016/s0738-3991(02)00032-0
- Guo Y, Albright D. The effectiveness of telehealth on self-management for older adults with a chronic condition: a comprehensive narrative review of the literature. J Telemed Telecare. 2018;24(6):392–403. doi:10.1177/1357633x17706285
- Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Educ Couns. 2005;57(3):300–307. doi:10.1016/j.pec.2004.08.004
- Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID-19 Pandemic: scoping review. J Med Internet Res. 2020;22(12):e24087. doi:10.2196/24087
- Hudson GM, Sprow K. Promoting physical activity during the COVID-19 pandemic: implications for obesity and chronic disease management. J Phys Act Health. 2020;17(7):685–687. doi:10.1123/jpah.2020-0318
- Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis. 2020;63(3):386–388. doi:10.1016/j.pcad.2020.03.009
- Laddu DR, Lavie CJ, Phillips SA, Arena R. Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic. Prog Cardiovasc Dis. 2021;64:102–104. doi:10.1016/j.pcad.2020.04.006
- Cadore EL, Sáez de Asteasu ML, Izquierdo M. Multicomponent exercise and the hallmarks of frailty: considerations on cognitive impairment and acute hospitalization. Exp Gerontol. 2019;122:10–14. doi:10.1016/j.exger.2019.04.007
- Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, et al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med. 2019;179(1):28–36. doi:10.1001/jamainternmed.2018.4869
- Tu J, Wang C, Wu S. The internet hospital: an emerging innovation in China. Lancet Glob Health. 2015;3(8):e445–e446. doi:10.1016/s2214-109x(15)00042-x
- Ding L, She Q, Chen F, et al. The internet hospital plus drug delivery platform for health management during the COVID-19 pandemic: observational study. J Med Internet Res. 2020;22(8):e19678. doi:10.2196/19678
- Gong K, Xu Z, Cai Z, Chen Y, Wang Z. Internet hospitals help prevent and control the epidemic of COVID-19 in China: multicenter user profiling study. J Med Internet Res. 2020;22(4):e18908. doi:10.2196/18908
- Cleland C, Ferguson S, Ellis G, Hunter RF. Validity of the International Physical Activity Questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behaviour of older adults in the United Kingdom. BMC Med Res Methodol. 2018;18(1):176. doi:10.1186/s12874-018-0642-3
- Radbruch L, Sabatowski R, Elsner F, Everts J, Mendoza T, Cleeland C. Validation of the German version of the brief fatigue inventory. J Pain Symptom Manage. 2003;25(5):449–458. doi:10.1016/s0885-3924(03)00073-3
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi:10.1001/jama.282.18.1737
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
- Gago CM, Lopez-Cepero A, O’Neill J, et al. Association of a single-item self-rated diet construct with diet quality measured with the alternate healthy eating index. Front Nutr. 2021;8:646694. doi:10.3389/fnut.2021.646694
- Folstein MF, Folstein SE, McHugh PR. ”Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
