Abstract
Background
A key issue in the treatment of obesity in older adults is whether the health benefits of weight loss outweigh the potential risks with respect to musculoskeletal injury.
Objective
To compare change in weight, improvements in metabolic risk factors, and reported musculoskeletal adverse events in middle-aged (50–59 years) and older (65–74 years), obese women.
Materials and methods
Participants completed an initial 6-month lifestyle intervention for weight loss, comprised of weekly group sessions, followed by 12 months of extended care with biweekly contacts. Weight and fasting blood samples were assessed at baseline, month 6, and month 18; data regarding adverse events were collected throughout the duration of the study.
Results
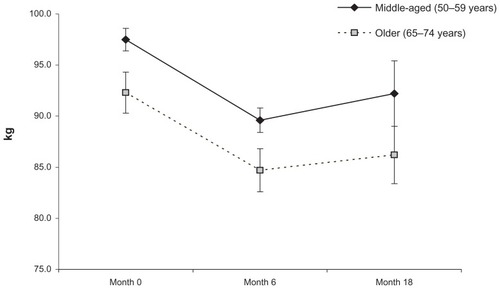
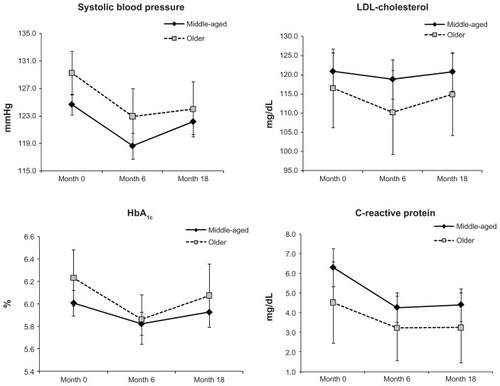
Both middle-aged (n = 162) and older (n = 56) women achieved significant weight reductions from baseline to month 6 (10.1 ± 0.68 kg and 9.3 ± 0.76 kg, respectively) and maintained a large proportion of their losses at month 18 (7.6 ± 0.87 kg and 7.6 ± 1.3 kg, respectively); there were no significant differences between the two groups with respect to weight change. Older women further experienced significant reductions in systolic blood pressure, HbA1c, and C-reactive protein from baseline to month 6 and maintained these improvements at month 18. Despite potential safety concerns, we found that older women were no more likely to experience musculoskeletal adverse events during the intervention as compared with their middle-aged counterparts.
Conclusion
These results suggest that older, obese women can experience significant health benefits from lifestyle treatment for obesity, including weight loss and improvements in disease risk factors. Further investigation of the impact of weight loss on additional health-related parameters and risks (eg, body composition, muscular strength, physical functioning, and injuries) in older adults is needed.
Introduction
According to reports from the National Health and Nutrition Examination Survey (NHANES), the prevalence of obesity in women 60 to 79 years is 42.3% (95% confidence interval [CI]: 38.3%–46.3%), compared with a prevalence of 31.9% (95% CI: 28.6%–35.5%) in women aged 20 to 39;Citation1 as such, obesity among older women represents a serious public health problem. Obesity in this age group is strongly associated with diabetes, hypertension, dyslipidemia, and osteoarthritis,Citation2 although the relation between obesity and all-cause mortality in this age group is inconsistent.Citation3–Citation6 Independent of weight status, age is correlated with greater prevalence and severity of many obesity-related health conditions and metabolic risk factors.Citation7 Additionally, obesity has been associated with significant impairment in health-related quality of life in older individuals.Citation8 However, excess weight in older persons (65 years and older) may also offer protective benefits with respect to bone loss, osteoporosis, and hip fracture.Citation9,Citation10 Further, some have noted the “obesity paradox,” whereby obesity has been found to be protective against mortality due to certain causes such as heart failure or cardiovascular disease.Citation11,Citation12
For middle-aged and young adults who are obese, the benefits of behavioral weight-loss treatment clearly outweigh potential risks. Reviews of randomized trials demonstrate that lifestyle interventions, typically delivered in weekly group sessions over the course of 4 to 6 months, produce average weight losses of 8.5 kg posttreatment (approximately 5%–10% of initial body weight).Citation13–Citation15 Reductions of this magnitude can have beneficial effects on a variety of weight-related health conditions and risk factors.Citation16–Citation18 However, several longitudinal observational studies have demonstrated that weight loss in older adults is related to increased mortality, disability, functional limitation, institutionalization, loss of lean muscle mass and bone mineral density, increased risk of hip fracture, and loss of mobility.Citation19,Citation20 These studies, however, have not controlled for a number of potential confounds, such as intentionality of weight loss, obesity status prior to weight loss, occult disease or pathology, and smoking status.
A small number of clinical trials have been conducted to examine the effects of weight-loss treatment among older, obese adults,Citation21–Citation23 but a recent meta-analysis suggested that high-quality evidence regarding the efficacy of weight-loss interventions among older adults is lacking and that additional studies are needed.Citation23 This meta-analysis also indicated that although obese, older adults are able to achieve significant weight losses, changes in blood pressure, lipid profile, glycemic control, exercise capacity, and quality of life, as a consequence of weight-loss treatment, did not reach statistical significance. Moreover, data on these health outcomes were very limited, and there was substantial heterogeneity across studies.Citation23 Adverse outcomes were not examined in this meta-analysis, though results from the Diabetes Prevention Program indicated that rates of musculoskeletal adverse events were slightly higher among the lifestyle intervention group as compared with the placebo (although authors reported no significant differences by treatment assignment).Citation24 Older participants were more likely to report adverse events as compared with younger participants.Citation24 In a recent randomized controlled clinical trial examining the effectiveness of diet, exercise, or a combination, among adults 65 years of age or older, Villareal et alCitation22 reported that participants in the diet-only arm experienced reductions in lean body mass and bone mineral density, while participants in the exercise arm reported a greater degree of musculoskeletal injuries. This study also reported significant improvements in a variety of weight-related health outcomes.Citation22 However, authors did not report whether these risks and benefits of weight-loss treatment differed by age.
At present, it remains unclear whether the benefits of intentional weight loss in older, obese adults outweigh potential risks of weight-loss treatment, and whether improvements in health or risks associated with treatment are similar across age cohorts. Few studies have examined the effects of behavioral weight-loss treatment in older adults.Citation10,Citation25 Intentional weight loss in older, obese adults could ameliorate weight-related diseases and conditions, such as joint pain, psychological symptoms, and quality of life,Citation10 but could simultaneously present risks with regards to musculoskeletal injury, and bone and muscle loss.
The current study investigated both the health benefits (ie, weight loss, improvements in metabolic risk factors) and adverse consequences of weight-loss treatment in older adults (65–74 years) and examined whether these effects were comparable to those experienced by middle-aged adults (50–59 years). The primary aims of the present study were to determine: (1) if older, obese women experience significant benefits (ie, weight loss) from a lifestyle intervention for weight loss; (2) if behavioral weight-loss treatment is associated with negative outcomes (ie, musculoskeletal injury) for older, obese women; and (3) if weight loss and adverse event outcomes are equivalent in older and middle-aged participants. We hypothesized that positive and adverse outcomes would be similar across age groups. A secondary aim of this study was to describe and compare the responses of older and middle-aged participants with regards to changes in metabolic risk factors, including systolic blood pressure, LDL cholesterol, Hemoglobin A1c, and C-reactive protein.
Materials and methods
This study is a secondary analysis of data collected in the TOURS (Treatment of Obesity in Underserved Rural Settings) trial. TOURS was a randomized, controlled trial of behavioral weight-loss treatment, in six medically underserved rural counties in northern Florida, USA.Citation26
Participants
Participants in the TOURS trial were 298 women (aged 50–75 years), with body mass index (BMI) >30 kg/m2, who resided in rural counties in north-central Florida. Potential participants were excluded if they weighed over 158.8 kg, had a history of heart attack or stroke, metabolic abnormalities, any musculoskeletal conditions that limited walking, any major psychiatric disorders, or experienced significant weight loss (ie, ≥4.5 kg) in the 6 months prior to the study.
Procedure
The University of Florida Institutional Review Board approved all study procedures. Recruitment and study methods have been described previously.Citation26 At months 0, 6, and 18, participants’ weights and blood pressures were assessed, and blood was drawn and analyzed for metabolic profile. Participant height was measured at month 0 but not during the later assessment points.
Measures
Primary aims
Percent weight change
Weight was measured to the nearest 0.1 kilogram using a calibrated and certified balance beam scale. Participants were measured in light indoor clothing with shoes removed. Change in body weight was calculated by subtracting participants’ 6 and 18 month weights from their baseline values. Participant height was measured, without shoes, to the nearest 1.0 cm using a portable stadiometer. Height and weight were used to calculate BMI.
Musculoskeletal adverse events
Participants were asked to report all adverse events experienced throughout the duration of the study. Adverse events were categorized for review by a local Institutional Review Board and by a specially constituted Data Safety and Monitoring Board. Additionally, all events were separately recoded, as representing a musculoskeletal injury or other type of adverse event. Musculoskeletal adverse events were chosen because research has demonstrated a slight increase risk of this type of injury with lifestyle treatment.Citation24
Secondary aim
Metabolic risk factors
Resting blood pressure was measured by a Registered Nurse (RN), using a standardized protocol.Citation27 In the present study, only systolic blood pressure was examined due to its relation to cardiovascular disease risk.Citation28 Similarly, lipid profile was measured using low density lipoprotein (LDL)-cholesterol due to its strong association with cardiovascular disease risk.Citation29 Glycemic control, which is highly related to diabetic risk,Citation30 was assessed via Hemoglobin A1c (HbA1c), which is a more durable measure of glycemic control than fasting glucose.Citation31 C-reactive protein is a marker of inflammation, which is associated with atherosclerosis and cardiovascular disease, and was also measured.Citation32 Blood samples were drawn by the study RN and analyzed by Quest Diagnostics Clinical Laboratories (Quest Diagnostics Inc, Madison, NJ, USA) for lipid and metabolic profile.
TOURS intervention
All participants received a 6-month lifestyle intervention (Phase I) carried out through Cooperative Extension Service offices in six rural counties in North Florida. Phase I of the TOURS trial included 24 weekly group behavioral treatment sessions. The program was designed to decrease caloric intake (to 1200 kcal per day) and increase moderate-intensity physical activity to reach a 10,000 per day step average or attain at least 3000 steps greater than baseline levels. No liquid meal supplements were utilized in the trial. At the conclusion of Phase I, these women were randomized to one of three year-long follow-up programs with biweekly contacts (Phase II): a face-to-face counseling program, a telephone counseling program, or a mail-only education “control” condition.
Change in caloric intake and physical activity
Change in caloric intake was assessed using the Block Food Frequency Questionnaire (Block FFQ).Citation33 This self-report questionnaire asks participants to record the frequency at which they consumed 106 different foods over the preceding year. This questionnaire probes participants for the portion size of foods consumed, along with composition (eg, low- vs high-fat cuts of meat) and added condiments (eg, butter or jam added to toast). Estimates from the Block FFQ have been demonstrated to correlate 0.45 with estimated “true” dietary intake using 24-hour recalls.Citation34
Physical activity was measured using the CHAMPS Physical activity questionnaire for older adults.Citation35 This 40-item questionnaire was specifically designed to assess types of physical activity that are appropriate for older adults. The CHAMPS has been validated against other physical activity measures, with correlations of 0.73 for moderate-intensity activities (which were the focus of the current intervention), and 0.55 for all specified activities.Citation35
Statistical analyses
The data analyses were performed using both a per-protocol and an intent-to-treat approach. All randomized participants were included in the intent-to-treat analyses. For this approach, multiple imputation was used to handle missing weights for individuals who dropped out after baseline; values were imputed assuming weight was regained back at a rate of 0.3 kg per month.Citation36,Citation37 The variance of this distribution was chosen as the variance of the residual from regressing 6-month (or 18-month) weights on baseline weight among those individuals without missing weights; this essentially corresponds to the variance under an assumption of missing at random (MAR). Use of this scenario is consistent with the findings from long-term studies of weight loss that show a reliable return to baseline weights over time and was used in the primary analysis of TOURS.Citation26,Citation38,Citation39 For the metabolic risk factors, a similar multiple imputation approach was used, with means corresponding to the baseline value of the risk factor. For the equivalence tests, only treatment completers were used (a per-protocol approach). Use of only treatment completers is consistent with a recent Consolidated Standards of Reporting Trials (CONSORT) group statement regarding the appropriate use of equivalence testing.Citation40 Use of intent-to-treat analyses in equivalence testing can increase the risk of type I error, as it suppresses observed mean differences between groups. Statistical analyses were conducted using SPSS (v17.0 for Windows; IBM, Armonk, NY, USA) and SAS (v9.1.2 for Windows; SAS Institute Inc, Cary, NC, USA) software programs.
Primary aims: weight loss and adverse events
To determine if older, obese women experience significant benefits from a lifestyle intervention for weight loss, we fit multivariate normal regression models, controlling for race/ethnicity, to examine changes in weight from month 0 to month 6 and month 18 using SAS Proc Mixed. Bonferroni corrections were applied to adjust for multiple comparisons.
To assess whether weight change and number of adverse events were equivalent between middle-aged and older obese women, we used equivalence tests. Margins of equivalence (Δ) for weight and the proportion of each group (older women and middle-aged women) reporting a musculoskeletal adverse event were set a priori, based on the smallest value that would represent a clinically significant difference. Weight outcomes for older and middle-aged participants were regarded as equivalent if the difference between group means (using a 95% CI of the difference) was less than or equal to 2.5 kg. Similarly, the proportions of each group reporting a musculoskeletal adverse event were regarded as equivalent if the 95% CI of the difference was contained within ±Δ (±0.04). The mean difference in weight change between older and middle-aged groups was obtained using multivariate normal regression. CIs of the difference in proportions of older and middle-aged women reporting a musculoskeletal adverse event were calculated using methods described by Newcombe.Citation41
Secondary aims: metabolic risk factors
Multivariate normal regression models fit using SAS Proc Mixed were used to compare older and middle-aged participants with regards to changes in metabolic risk factors over time. Criterion variables included systolic blood pressure, LDL-cholesterol, HbA1c, and C-reactive protein. To adjust for multiple comparisons, Bonferroni corrections were applied.
Results
Baseline characteristics by age
The mean age of participants in the TOURS study was 59.3 ± 6.2 years. The present study included 56 older women (65–74 years) and 162 middle-aged women (50–59 years) drawn from the total sample. Among all 298 participants, 75.5% classified their race/ethnicity as Caucasian, 20.5% as African American, 1.7% as Hispanic American, 2.0% as American Indian, and 0.3% as Pacific Islander. The mean pretreatment weight was 96.5 ± 14.9 kg, and mean baseline BMI was 36.8 ± 5.0 kg/m2. The majority of the sample (64.4%) had completed at least 12 years of education, with 43.3% reporting at least trade, vocational, or associate training. The majority of participants were married (72.5%), and nearly half of the women were employed full or part time (47.3%). Over two-thirds of the sample (67.9%) reported a total household income of less than $50,000.
Older women (ie, women 60–74 years; n = 56) in this study were more likely to be Caucasian, χ2 (1) = 4.6, P < 0.05, and less likely to be employed, χ2 (1) = 57.2, P < 0.001, than middle-aged women (ie, women 50–59 years; n = 162). Older women weighed significantly less than middle-aged women at baseline, t(216) = 2.3, P < 0.025, but this difference was not clinically significant, and both groups fell in the Class II obesity range (BMI 35.0 to 39.9 kg/m2) at pretreatment. Older women did not differ from middle-aged women on any metabolic risk factor at pretreatment, with the exception of systolic blood pressure, which was higher in the older group, t(216) = −3.6, P < 0.001. Baseline characteristics by age are displayed in .
Table 1 Baseline demographic characteristics of older and middle-aged participants
Previous analyses of the TOURS data have suggested that Caucasian women and African-American women respond differently to treatment in terms of magnitude of weight loss, changes in metabolic risk factors, and a number of behavioral variables.Citation42 The older age group was comprised of a significantly greater proportion of Caucasian women, thus equivalence testing was conducted separately for Caucasian and African American women. However, given that the older age group contained only seven African American women, we did not have enough power to perform formal tests of equivalence with this subsample. Thus, only descriptive statistics are provided.
Weight change
Using a per-protocol analysis (ie, treatment completers only) we fit a multivariate normal regression to examine within-group changes in weight, while controlling for race/ethnicity. The proportion of older women who completed the study was not significantly different from the proportion of middle-aged women, χ2 (1) = 0.58, P = 0.466. Similarly, there were no significant differences between the proportion of older and middle-aged women who returned for assessment at month 6 or month 18, (P = 0.948 and 0.467, respectively). There were also no significant differences between groups in reported caloric change from month 0 to month 6 for older and middle-aged women (−438.7 kcal/day vs −504.7 kcal/day, P = 0.645), although both groups experienced significant decreases in reported caloric intake over this time, t(51) = 4.5, P < 0.0001, and t(145) = 6.5, P < 0.0001, respectively. With respect to changes in reported physical functioning, while both older and middle-aged women significantly increased their average distance walked from month 0 to month 6 (65.9 feet vs 71.8 feet, t[50] = 3.46, P < 0.001 and t[140] = 5.39, P < 0.0001, respectively), there was no significant difference between groups in this change, P = 0.812.
Older women evidenced a significant reduction in weight from month 0 to month 6, mean ± standard error (SE) = 9.3 ± 0.76 kg, P < 0.001. This weight loss was largely maintained at month 18, at 7.6 ± 1.3 kg, P < 0.001. Similarly, middle-aged women experienced a significant within-group weight loss from month 0 to month 6, mean ± SE = 10.1 ± 0.68 kg, and this loss was largely maintained at month 18, mean ± SE = 7.6 ± 0.86 kg. Changes in weight over time among treatment completers are displayed in . Using an intent-to-treat approach produced similar results ().
Table 2 Changes in weight and metabolic risk factors in older and middle-aged women (per-protocol analysis)
With respect to clinically significant weight loss (ie, weight loss ≥ 5% of baseline weight), there were no further differences by age group over time. At 6 months, 78.8% of older adults achieved a ≥5% weight loss compared with 75.0% of middle-aged adults, χ2(1) = 0.312, P = 0.576; at 18 months, 57.1% of older women maintained a clinically significant weight loss compared with 51.1% of middle-aged women, χ2(1) = 0.530, P = 0.467.
Equivalence testing
Weight change
Among treatment completers, older Caucasian women (n = 47) lost a mean ± SE of 9.6 ± 0.83 kg from month 0 to month 6, which was not significantly different from the 11.0 ± 0.55 kg weight loss achieved by middle-aged Caucasian women (n = 112). The 95% CI of the difference (−3.4 to 0.55) was not contained within the margin of equivalence (2.5 kg), thus, statistical equivalence could not be established. At long-term follow up, older women had lost a mean of 7.6 ± 1.3 kg body weight; again, this was not significantly different from the 7.4 ± 0.76 kg weight loss evidenced by middle-aged women. The groups were not equivalent with respect to weight loss at month 18, as the 95% CI of the difference exceeded the margin of equivalence (95% CI: −2.8 to 3.2, respectively).
Older African American women (n = 7) lost a mean of 5.9 ± 3.0 kg of body weight from month 0 to month 6, as compared with 6.7 ± 4.3 kg for the middle-aged African American women (n = 42). At long-term follow-up, older African American women had lost 6.1 ± 5.1 kg of body weight as compared with 5.0 ± 7.7 kg for the middle-aged women.
Adverse events
Point-biserial correlations indicated that there was no relationship between age (as a continuous variable) and the report of injury at 6 or 18 months (r = 0.05, P = 0.400, and r = 0.03, P = 0.630, respectively). During initial treatment (month 0 to 6), 23% of older Caucasian women reported at least one musculoskeletal adverse event, as compared with 18% of middle-aged Caucasian women. The 95% CI of the difference in proportions, calculated according to the methods described by Newcombe,Citation41 was −20.6% to 7.2%, well outside the margin of equivalence (4%). The proportion of older women reporting a musculoskeletal adverse event over the course of the entire study (month 0 to 18) was 47%, as compared with 36% of middle-aged Caucasian women, χ2 (1) = 1.7, P = 0.19. Again, the 95% CI of the difference in proportions fell outside the margin of equivalence (95% CI: −27.3 to 5.2).
To further investigate the risk of musculoskeletal injury, we divided all participants into ad hoc 5-year age cohorts. Although the sample of women over 70 years of age was not large enough to conduct a formal significance test (n = 16), 56% of Caucasian participants over 70 years of age reported at least one adverse event over the course of the study as compared with 37% of Caucasian women ages 50 to 69 years (n = 209).
During initial treatment, 11% of older African-American women reported a musculoskeletal adverse event, as compared with 26% of middle-aged women. At long-term follow up, 42% of middle-aged African-American women had reported at least one adverse event, as compared with only 11% of older African-American women. There was a trend for older African-American women to be less likely to report a musculoskeletal adverse event overall than middle-aged African-American women, χ2 (1) = 3.1, P = 0.078, again a difference that may have reached significance with a larger sample size.
Secondary aims: metabolic risk factors
Using a per-protocol approach, older women experienced significant reductions in systolic blood pressure from month 0 to month 6, mean ± SE = 7.3 ± 1.77, P < 0.001, and maintained these improvements at month 18, mean change ± SE month 0 to 18 = 5.9 ± 1.8, P < 0.01. Changes in LDL cholesterol were not significant over time. HbA1c was significantly reduced from month 0 to months 6, 0.32 ± 0.01, P < 0.001; and from month 0 to month 18, 0.25 ± 0.09, P < 0.01. C-reactive protein was also significantly reduced from month 0 to month 6, 2.1 ± 0.63, P < 0.001; these changes were maintained at month 18, −2.0 ± 0.70, P < 0.01. Changes in metabolic risk factors over time can be seen in . Using an intent-to-treat approach, a similar pattern of results emerged ().
Discussion
The present study examined both the benefits (ie, weight loss and improvements in metabolic risk factors) and adverse outcomes of a lifestyle intervention for weight loss in a sample of older and middle-aged adults, and compared these outcomes between age groups. Older women achieved significant reductions in weight during treatment and at long-term follow up. Among treatment completers, older Caucasian women had lost a mean of 9.6 kg of body weight at 6 months, which was not statistically different from the 11.0 kg of weight loss achieved by middle-aged Caucasian women. At 18 months, the difference between older and middle-aged participants exceeded the margin of equivalence (7.5 vs 8.5 k g; 95% CI: −2.4 to 4.4), possibly due to the small sample size of older adults. A comparison of middle-aged and older African-American women revealed a trend for older women to lose more weight than middle-aged women from baseline to month 18 (6.1 kg of body weight as compared with 5.0 kg).
With regards to adverse outcomes, 23% of older Caucasian women reported at least one musculoskeletal injury during initial treatment, and 47% reported this type of adverse event over the course of the 18-month intervention. These proportions were not significantly different from the 18% of middle-aged women reporting an injury during initial treatment and the 36% reporting an injury throughout the 18 month study. The Diabetes Prevention Program Research Group described a similar pattern of results for participants in the “lifestyle” condition, by which participants between 60 and 85 years of age reported 28 musculoskeletal adverse events per 100 person-years, in contrast to 25 to 40 year old participants, who reported 20 musculoskeletal adverse events per 100 person-years, a nonsignificant difference.Citation24
The proportions of middle-aged and older women reporting a musculoskeletal adverse event during initial treatment and over the course of the entire study were not equivalent. Post hoc power analyses suggested we would have needed over 800 participants per group to determine equivalence, even if we had used a wider 10% margin. Beyond rejecting our hypothesis that older and middle-aged women experience comparable rates of injury, it appears that older Caucasian women may be at greater risk for injury than middle-aged Caucasian women. When we further categorized the sample into 5-year age increments, 56% of Caucasian women over 70 years of age reported at least one musculoskeletal injury throughout the 18 months, as compared with only 37% of Caucasian participants 50 to 69 years of age. Given that only 16 women fell into the above 70-year age range, we did not have enough power to examine differences in the proportion of women over 70 reporting a musculoskeletal injury, as compared with younger age groups. This discrepancy warrants further investigation regarding the safety of behavioral weight-loss treatment for older adults, with a larger sample. A related finding deserving of further investigation is the potential trend for older African-American women to report fewer adverse events than their younger counterparts. Future research with larger samples of racial and ethnic subpopulations should examine these potential differences.
With respect to our secondary aims, older women experienced a significant reduction in systolic blood pressure from pre- to posttreatment and largely maintained this decrease at 18 months. Additionally, older women showed significant reductions in HbA1c and C-reactive protein from month 0 to month 6, and from month 0 to month 18. There was no significant within-group change over time in LDL-cholesterol levels. Overall, the current results support the hypothesis that older women experience a number of benefits from lifestyle interventions for weight loss. However, the present study did not measure additional health-related parameters, such as medication use or changes in body composition, muscular strength, or physical functioning. While outcomes from weight loss in older adults hold both potential risks and benefits,Citation43 further investigation of these variables is warranted.
There are several limitations to the present study. First, we had a relatively small sample of older women, offering limited power to detect small differences in a variety of outcomes. A second limitation was the lack of an untreated control group of older women. Although there appeared to be a slight increase in risk of musculoskeletal injury for older women, we cannot determine if this increase was related to participation in the study or the consequence of aging. Future research should compare the rate of musculoskeletal injury in older women not undergoing weight-loss treatment with those participating in the lifestyle program, to clarify if this type of treatment is associated with greater risk of injury in older adults.
Additionally, individuals with serious health conditions (eg, uncontrolled diabetes or hypertension) were excluded from the study. Given that the severity of weight-related risk factors and diseases is typically compounded with age, the exclusion of older women with serious health conditions at baseline may have resulted in a sample that is not representative of the larger population of women over 65 years of age. Generalizability is also limited by the exclusion of younger age groups as well as the underrepresentation of older racial/ethnic minority participants.
This study has several important implications with regards to the safety and efficacy of behavioral weight-loss interventions for older adults. We found that older women (those over 65 years of age) experienced significant benefits from a lifestyle intervention for weight loss. However, results also indicated that older women might be at greater risk for musculoskeletal adverse events during participation in a lifestyle intervention for weight loss as compared with their middle-aged counterparts. Subsequently, lifestyle interventions including older adults should take particular precautions to educate participants about safe ways to achieve exercise goals and avoid injury (eg, including several supervised exercise sessions at initiation of treatment). Future research should further explore potential negative outcomes of weight-loss treatment for older, obese adults, particularly with respect to musculoskeletal injury, and bone and muscle loss.
Acknowledgment
This research was supported by grant R18HL73326 from the National Heart, Lung and Blood Institute. Publication of this article was funded in part by the University of Florida Open Access Publishing Fund.
Disclosure
The authors report no conflicts of interest in this work.
References
- FlegalKMCarrollMDKitBKOgdenCLPrevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010JAMA2012307549149722253363
- MustASpadanoJCoakleyEHFieldAEColditzGDietzWHThe disease burden associated with overweight and obesityJAMA1999282161523152910546691
- CorradaMMKawasCHMozaffarFPaganini-HillAAssociation of body mass index and weight change with all-cause mortality in the elderlyAm J Epidemiol20061631093894916641311
- FlegalKMGraubardBIWilliamsonDFGailMHExcess deaths associated with underweight, overweight, and obesityJAMA2005293151861186715840860
- LocherJLRothDLRitchieCSBody mass index, weight loss, and mortality in community-dwelling older adultsJ Geront A Biol Sci Med Sci2007621213891392
- MansonJEWillettWCStampferMJBody weight and mortality among womenN Engl J Med1995333116776857637744
- VillarealDTApovianCMKushnerRFKleinSfor the American Society for Nutrition; NAASO, The Obesity SocietyObesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity SocietyAm J Clin Nutr200582592393416280421
- VillarealDTBanksMSienerCSinacoreDRKleinSPhysical frailty and body composition in obese elderly men and womenObes Res200412691392015229329
- FelsonDTZhangYHannanMTAndersonJJEffects of weight and body mass index on bone mineral density in men and women: the Framingham studyJ Bone Miner Res1993855675738511983
- RössnerSObesity in the elderly–a future matter of concern?Obes Rev20012318318812120103
- LavieCJMilaniRVVenturaHOObesity and cardiovascular disease: risk factor, paradox, and impact of weight lossJ Am Coll Cardiol200953211925193219460605
- UretskySMesserliFHBangaloreSObesity paradox in patients with hypertension and coronary artery diseaseAm J Med20071201086387017904457
- JefferyRWDrewnowskiAEpsteinLHLong-term maintenance of weight loss: current statusHealth Psychol200019Suppl 1S5S16
- WaddenTACrerandCEBrockJBehavioral treatment of obesityPsychiatr Clin North Am200528115117015733617
- PerriMGFullerPRSuccess and failure in the treatment of obesity: Where do we go from here?Med Exer Nutr Health19954255272
- National Institutes of HealthClinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults – The Evidence ReportObes Res19986Suppl 2S51S209
- WingRRVendittiEJakicicJMPolleyBALangWLifestyle intervention in overweight individuals with a family history of diabetesDiabetes Care19982133503599540015
- MaggioCAPi-SunyerFXThe prevention and treatment of obesity: Application to type 2 diabetesDiabetes Care19972011174417669353619
- ThomasDRWeight loss in older adultsRev Endocr Metab Disord20056212913615843884
- WallaceJISchwartzRSEpidemiology of weight loss in humans with special reference to wasting in the elderlyInt J Cardiol2002851152112163206
- BalesCWBuhrGIs obesity bad for older persons? A systematic review of the pros and cons of weight reduction in later lifeJ Am Med Dir Assoc20089530231218519110
- VillarealDTChodeSParimiNWeight loss, exercise, or both and physical function in obese older adultsN Engl J Med2011364131218122921449785
- WithamMDAvenellAInterventions to achieve long-term weight loss in obese older people: a systematic review and meta-analysisAge Ageing201039217618420083615
- Diabetes Prevention Program Research GroupCrandallJSchadeDMaYThe influence of age and the effects of lifestyle modification and metformin in prevention of diabetesJ Gerontol2006611010751081
- ZamboniMMazzaliGZoicoEHealth consequences of obesity in the elderly: a review of four unresolved questionsInt J Obes (Lond)20052991011102915925957
- PerriMGLimacherMCDurningPEExtended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trialArch Intern Med2008168212347235419029500
- ChobanianAVBakrisGLBlackHRfor the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute:National High Blood Pressure Education Program Coordinating CommitteeSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034261206125214656957
- Prospective Studies CollaborationAge-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet200236093491903191312493255
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in AdultsExecutive summary of the third report of the National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III)JAMA2001285192486249711368702
- American Diabetes AssociationImplications of the United Kingdom Prospective Diabetes StudyDiabetes Care200225Suppl 1S27S31
- Centers for Disease Control and PreventionTeam Care: Comprehensive Lifetime Management for DiabetesAtlantaCenters for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion2001
- LibbyPRidkerPMMaseriAInflammation and atherosclerosisCirculation200210591135114311877368
- BlockGHartmanAMDresserCMCarrollMDGannonJGardnerLA data-based approach to diet questionnaire design and testingAm J Epidemiol198612434534693740045
- SubarAFThompsonFEKipnisVComparative validation of the Block, Willet, and National Cancer Institute Food Frequency Questionnaires: the Eating at America’s Table StudyAm J Epidemiol2001154121089109911744511
- StewartALMillsKMKingACHaskellWLGillisDRitterPLCHAMPS physical activity questionnaire for older adults: outcomes for interventionsMed Sci Sports Exerc20013371126114111445760
- WaddenTABerkowitzRIWombleLGRandomized trial of lifestyle modification and pharmacotherapy for obesityN Engl J Med2005353202111212016291981
- WingRRTateDFGorinAARavnorHAFavaJLA self-regulation program for maintenance of weight lossNew Engl J Med2006355151563157117035649
- KramerFMJefferyRWForsterJLSnellMKLong-term follow-up of behavioral treatment for obesity: patterns of weight regain among men and womenInt J Obes19891321231362663745
- StalonasPMPerriMGKerznerABDo behavioral treatments of obesity last? A five-year follow-up investigationAddict Behav1984921751836741677
- PiaggioGElbourneDRAltmanDGPocockSJEvansSJfor the CONSORT GroupReporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statementJAMA2006295101152116016522836
- NewcombeRGTwo-sided confidence intervals for the single proportion: comparison of seven methodsStat Med19981788578729595616
- RickelKAMilsomVARossKMHooverVJPetersonNDPerriMGDifferential response of African American and Caucasian women to extended-care programs for obesity managementEthn Dis Spring201121217017521749020
- HoustonDKNicklasBJZizzaCAWeighty concerns: the growing prevalence of obesity among older adultsJ Am Diet Assoc2009109111886189519857630