 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
To date, no studies have attempted to estimate body shape biological age using clinical parameters associated with body composition for the purposes of examining a person’s body shape based on their age.
Objective
We examined the relations between clinical parameters associated with body composition and chronological age, and proposed a model for estimating the body shape biological age.
Methods
The study was conducted in 243,778 subjects aged between 20 and 90 years who received a general medical checkup at health promotion centers at university and community hospitals in Korea from 2004 to 2011.
Results
In men, the clinical parameters with the highest correlation to age included the waist- to-hip ratio (r = 0.786, P < 0.001), hip circumference (r = −0.448, P < 0.001), and height (r = −0.377, P < 0.001). In women, the clinical parameters with the highest correlation to age include the waist-to-hip ratio (r = 0.859, P < 0.001), waist circumference (r = 0.580, P < 0.001), and hip circumference (r = 0.520, P < 0.001). To estimate the optimal body shape biological age based on clinical parameters associated with body composition, we performed a multiple regression analysis. In a model estimating the body shape biological age, the coefficient of determination (R2) was 0.71 in men and 0.76 in women.
Conclusion
Our model for estimating body shape biological age might be a novel approach to variation in body shape that is due to aging. We assume that our estimation model would be used as an adjunctive measure in easily predicting differences in body shape with the use of clinical parameters that are commonly used to assess the status of obesity in a clinical setting.
Introduction
Substantial changes in body composition occur over the aging process. Many studies have suggested that over the course of the aging process, the amount of fat tends to increase and is preferentially stored in the abdominal area, while skeletal muscle mass and bone mineral density decline.Citation1–Citation4 Understanding how changes in body composition, especially fat distribution, affect the risk for many chronic diseases such as cardiovascular diseases and type 2 diabetes mellitus, is a primary concern.
It is well known that body mass index (BMI) is one of the most popular clinical parameters for estimating body composition, and it is a reliable indicator for body fat mass percentage (BFM%). It is also an obesity index whose causal relationship with morbidity and mortality has been well established.Citation5–Citation7 Because it can be efficiently used to determine obesity in a large-sized population, BMI is frequently used for the assessment of obesity in a clinical setting. It has been reported, however, that the distribution of body fat rather than its amount is more likely to be associated with health-related risks,Citation8 and that abdominal obesity is an independent risk factor for raising the morbidity and mortality as such.Citation9–Citation11 This has led to an emphasis on the importance of other parameters, including the abdominal obesity index in particular, than BMI in assessing obesity.
Measures for abdominal obesity include waist circumference (WC), waist-to-hip ratio (WHR), and abdominal sagittal diameter. In addition, abdominal obesity is also evaluated by measuring the amount of body fat using ultrasonography, computed tomography, and magnetic resonance imaging. Of the various types of measures that are used to assess obesity, the amount of visceral body fat measured on computed tomography scans is known to best indicate abdominal obesity;Citation12–Citation14 however, its use is somewhat restricted because of the cost and exposure to irradiation. Accordingly, in an actual clinical setting, WC and WHR are mainly used to assess abdominal obesity. According to several previous studies examining various parameters that are commonly used to assess abdominal obesity in a clinical setting, WC was a more reliable parameter than WHR in making a diagnosis of abdominal obesity.Citation15 In addition, these studies have also shown that WC was also the most reliable indicator in predicting the amount of visceral fat.Citation10,Citation16,Citation17
Body fat is redistributed with increasing age, as more of it becomes located in the abdominal cavity.Citation14,Citation18 The reason for this redistribution is not really known, but declining testosterone and growth hormone levels in combination with declining rates of lipolysis of visceral fat associated with aging may play a role in men.Citation19 Low testosterone levels have been shown to be associated with increased visceral fat mass in men.Citation20 In women, the declining estrogen levels after menopause may be a critical factor. While several studies have investigated the relationship between weight change, obesity, and visceral fat with age and the risk of developing lifestyle-related diseases,Citation21–Citation24 the effect of maintaining one’s youthful body shape (in terms of appearance) on reducing such risks has been given significantly less attention.
Several recent studies have reported the difference in body shape between men and women, and they have examined age-related differences in body shape using three-dimensional body scans. It has become more and more clinically important to assess body shape based on the pattern of body fat distribution and redistribution, rather than to assess obesity simply based on an increased amount of body fat. Meanwhile, several approaches have been used to objectively assess body shape from this context.Citation25–Citation30 Presumably, the assessment of body shape based on three-dimensional body scans might be unavailable in a clinical setting. Therefore, it might also be mandatory to conduct studies to assess the status of body shape associated with age using clinical parameters that are currently used to assess obesity in a clinical setting.
It remains problematic that in general, anthropometric measures such as BMI or WHR are insufficient for the assessment of this redistribution.Citation31 In addition, anthropometric measures have been mainly used to assess the status of obesity based on body composition up until the present.
Age after birth is a measure of the degree of aging in individual, this is termed as chronological age or calendar age, which is a definition of aging as a function of time. Aging is characterized by a time-related decline in physiological functions and changes in morphology, and is usually assessed by the chronological age, which is defined as time elapsed since birth. Chronological age fails to provide an accurate indicator of the aging process. Because tissues age at different rates and because diseases vary enormously among individuals, humans become increasingly different from one another with age. But, biological age estimates the functional status of an individual in reference to his or her chronological peers on the basis of how well he or she functions in comparison with others of the same chronological age.Citation32,Citation33 Biological age is estimated based on aging biomarkers that are subject to change depending on one’s calendar age. Overall, biological age is a more reliable indicator of the degree of aging and one’s health status as compared to an individual’s calendar age. To date, a variety of models for estimating biological age have therefore been proposed to meet relevant study objectives. To estimate the physical, biochemical, and hormonal biological ages, we have also previously proposed the models for estimating biological ages using relevant biomarkers;Citation34 however, we did not propose a model for estimating body shape biological age using the clinical parameters associated with body composition.
Given this background, we conducted the current study to examine the correlations of age with BMI, BFM%, lean body mass percentage (LBM%), WC, and the WHR using clinical parameters associated with body composition. In addition, by using these parameters, we also proposed a model of body shape biological age that estimated a person’s body shape based on their age. Thus, our estimation model will help people understand the above correlations, and it will promote bidirectional communication between physicians and patients.
Methods
Subjects
The current study was conducted in 243,778 subjects aged between 20 and 90 years; the subjects comprised men and women who received a general medical checkup for health promotion and disease prevention at health promotion centers at university and community hospitals during a period ranging from June 2004 to January 2011. In the current study, exclusion criteria included the presence of uncontrolled hypertension and diabetes, and the subjects taking current medications for cardiovascular, pulmonary, hepatic, pancreatic, or renal diseases. Subjects were also excluded if their reported clinical parameters exceeded the standard deviations of the normal range.
Clinical parameters
To analyze the differences in clinical parameters due to aging, and to minimize the potential confounding effects of diseases or abnormal measurements, we set inclusion criteria considering both the standard deviations of parameters that were collected and the normal range which was established by the American Medical Association. Of these clinical parameters, we excluded those which were not in agreement with the inclusion criteria. Only the screened data were used for the statistical analysis.
For the clinical parameters associated with obesity, we collected data such as height, weight, WC, hip circumference (HC), LBM%, and BFM%. Height and weight were measured using height-measuring equipment and an electronic scale while subjects wore light clothes. As for WC, the thinnest area between the inferior part of the lowest rib and the iliac crest was measured as a unit of cm when subjects were in an upright position. As for HC, the location of the greater trochanter or the widest circumference was measured as a unit of cm. This was followed by the measurement of LBM% and BFM% using multifrequency segmental bioelectrical impedance (Inbody®, Biospace Co, Ltd, Seoul, Korea). BMI was calculated using height and weight as shown below. Then, using the measurements of WC and HC, the WHR was calculated:
Statistical analysis
To identify the correlation between the clinical parameters and chronological age, a Pearson’s correlation analysis was performed. To propose a model for estimating body shape biological age, we performed a stepwise method in multiple regression analysis between the age and clinical parameters that had been selected by the correlation analysis. We employed multiple regression analysis with assigning variance inflation factor to evaluate multicollinearity among the parameters. Statistical analysis was completed using SPSS 12.0 (SPSS Inc, Chicago, IL, USA). Statistical significance was set at P < 0.05.
Results
Baseline characteristics
A total of 243,778 subjects participated in the current study, of which there were 132,336 men and 110,042 women. All the clinical parameters associated with obesity are represented in . Mean age was 47.17 ± 10.98 years in men and 46.94 ± 11.96 years in women. In men, mean height and weight were 170.57 ± 5.96 cm and 71.16 ± 9.23 kg, respectively. In women, these values were 157.91 ± 5.63 cm and 56.92 ± 7.64 kg, respectively.
Table 1 Clinical characteristics of study subjects by gender
The correlation between age and the clinical parameters associated with body composition
In men, the clinical parameters with the highest correlation with the age included the WHR (r = 0.786, P < 0.001), HC (r = −0.448, P < 0.001), and height (r = −0.377, P < 0.001). In women, the clinical parameters with the highest correlation with age included the WHR (r = 0.859, P < 0.001), WC (r = 0.580, P < 0.001), and HC (r = 0.520, P < 0.001). All of the collected data surrounding the clinical parameters had a significant correlation with age. In men, however, only the clinical parameters associated with obesity other than BMI (r = 0.005, P = 0.191) had a significant correlation with age ( and ).
Table 2 Correlation coefficients between age and clinical parameters in males
Table 3 Correlation coefficients between age and clinical parameters in females
Estimation of body shape biological age based on clinical parameters associated with body composition
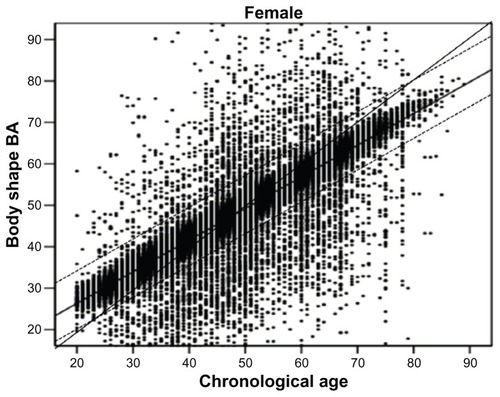
To estimate the optimal body shape biological age based on the clinical parameters associated with body composition, we performed a multiple regression analysis. In a model for estimating body shape biological age in men, the coefficient of determination (R2) was 0.71, and the relevant clinical parameters included the WHR, WC, height, LBM%, and weight. In a model for estimating the body shape biological age in women, the coefficient of determination (R2) was 0.76, and the relevant clinical parameters included the WHR, height, WC, LBM%, and weight ( and ). and illustrate the correlations between biological age and chronological age in a model for estimating body shape biological age in men and women.
Table 4 Body shape biological age prediction model in males (R2 = 0.705)
Table 5 Body shape biological age prediction model in females (R2 = 0.763)
Figure 1 The body shape BA prediction model in males.
Notes: The 45° line represents the theoretical normal aging line in males. The experimental line is the predicted regression line on body shape BA, and both dotted lines mean the range of ± 1 standard deviation (67%). The equation: body shape BA: −16.958 + 281.419 (WHR) − 1.595 (HC) − 0.149 (Ht) − 0.112 (LBM%) − 0.052 (Wt).
Abbreviations: BA, biological age; WHR, waist-to-hip ratio; HC, hip circumference; Ht, height; LBM%, lean body mass percentage; Wt, weight.
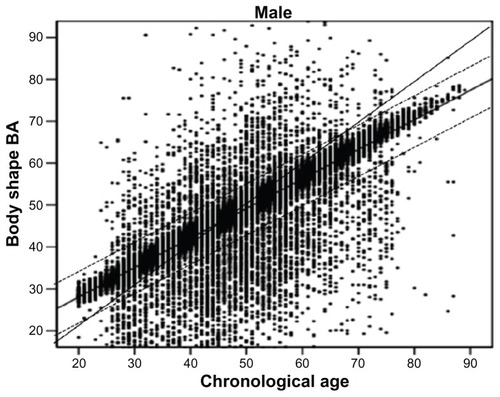
Figure 2 The body shape and BA prediction model in females.
Abbreviations: BA, biological age; WHR, waist-to-hip ratio; Ht, height; HC, hip circumference; LBM%, lean body mass percentage; WC, waist circumference.
Discussion
As shown in the current study, a model for estimating body shape biological age was effective in predicting the age-related changes that occur in body shape based on clinical parameters associated with body composition (WHR, WC, height, LBM%, weight, and HC) in approximately 71% of men and approximately 76% of women. Regarding the correlation between age and the clinical parameters associated with body composition, seven parameters other than BMI for men, and all of the eight parameters for women had a significant correlation with age. Of the clinical parameters that had a significant correlation with age. Of the clinical parameters that had a significant correlation with age in men, height, weight, LBM%, and HC had a negative correlation with age, while BFM%, WC, and the WHR had a positive correlation. In women, height and LBM% had a negative correlation with age, while weight, BMI, BFM%, WC, HC, and the WHR had a positive correlation.
Previous studies have shown that both men and women have experienced a decrease in height due to increased age, and this was more notable in women.Citation35–Citation43 A decrease in height due to increased age mainly originates from changes in the vertebrae (eg, vertebral fracture, weakening of the paravertebral muscles, changes in posture, degenerative changes in the intervertebral disc, vertebral deformity, and kyphosis). In addition, its onset begins at the age of 45 years or so, and then it continues with increased age.Citation36,Citation37,Citation43,Citation44 It is therefore known that a decrease in height due to increased age is associated with osteoporotic fractures, and it is also an indicator of the prediction of vertebral fractures and risks of developing femoral fractures in the elderly.Citation45,Citation46 In the current study, there was also a significant correlation between a decrease in height and increased age. In a model for estimating body shape biological age, the degree of the correlation between the two parameters was significantly higher in women than men.
BMI is widely used for nutritional assessment, obesity classification, and as a prognostic variable for mortality; however, there are many limitations. First, BMI could potentially produce an inaccurate diagnosis of “overweight” and “obese” in some special populations such as athletes, body builders, and elderly patients. Second, BMI-associated mortality in specific situations is controversial.Citation47
In a model for estimating the body shape biological age, we included the height and weight of men and only the height of women rather than the BMI. In addition, the correlation between BMI and age reached statistical significance only in women.
As shown in the current results, both men and women demonstrated a positive correlation between BFM% and age, and a negative correlation between age and LBM%. In addition, we included only the LBM% in a model for estimating biological age. Previous studies have established that BFM% was increased and LBM% was decreased with increased age.Citation48,Citation49 An increase in BFM% due to increased age originated from a decrease in LBM%, rather than from an increase in BFM% in men. It has been reported that an increase in BFM% rather than a decrease in LBM% might play a key role in causing an increase body fat due to aging in women.Citation50,Citation51
Regarding the distribution of body fat depending on body shape, it has been reported that abdominal obesity is a notable, independent risk factor for raising morbidity and mortality rates.Citation9–Citation11 Therefore, the clinical significance of weight, BMI, and the BFM% would greatly vary depending on the types of abdominal obesity, (ie, android or gynoid type). Previous studies have shown that WC is the most reliable indicator for reflecting the amount of visceral fat in the assessment of abdominal obesity.Citation10,Citation15–Citation17 As shown in the current results, both men and women had a positive correlation between increased age and both WC and the WHR; however, HC had a negative correlation with age in men and a positive correlation with in women. According to previous studies, the WHR was increased until the age of 55–64 years, and then it decreased thereafter in men, though it continually increased with increased age in women.Citation52,Citation53 These authors noted that these findings occurred because of the redistribution of body fat due to changes in sex hormones in both men and women aged between 45 and 54 years.Citation52,Citation53 Other studies have also shown that hormone therapy reduced the WHR, thus providing more evidence for the redistribution of body fat because of hormonal changes.Citation54,Citation55 As shown in the current results, the WHR was included in a model for estimating body shape biological age in both men and women. In addition, HC was included in this model for men, and both HC and WC were included for women. In particular, in estimating the body shape biological age, both men and women showed that the WHR was the most powerful factor. Previous studies have shown that WC is a more reliable indicator of predicting abdominal obesity. From a perspective that considers the differences in body shape due to aging, however, the WHR is a more powerful factor, and it better reflects differences in body shape.
In cross-sectional studies, the prevalence of high body weight or obesity (BMI > 30 kg/m2) increases with age up to about age 60 and then declines.Citation56 Although this does not indicate that the excessive accumulation of body fat rarely occurs in the elderly, this does suggest that visceral obesity increasingly occurs because of the redistribution of body fat due to increased age, and this leads to changes in body shape.Citation25–Citation30,Citation56 Accordingly, considering variation in body shape due to aging, it would be more appropriate for clinical evaluation to be based on body shape due to the increased occurrence of visceral obesity, rather than the consistent application of clinical parameters for assessing obesity.
We propose that a model for estimating body shape biological age be appropriate for assessing differences in body shape due to increased age with the application of clinical parameters associated with body composition. Moreover, by presenting the clinical parameters for assessing obesity that are commonly used in a clinical setting – and thereby comparing the results with those obtained from age-matched controls – our estimation model would be used to perform an overall analysis of the differences in body shape due to aging. Furthermore, by comparing one’s current body shape biological age with their calendar age (thereby expressing whether the body shape biological age is older or younger than one’s calendar age), our estimation model would be easily accepted by people, and it would also be of help for facilitating communication between physicians and patients. In addition, it would also be of help for providing the motives to improve the status of obesity, and for setting personal goals. In a model for assessing body shape biological age, however, we did not include the factors that might affect the clinical parameters associated with obesity, including the amount of physical activity, eating habits such as nutritional intake, and socioeconomic status, and we excluded the data of some subjects who were suspected of having diseases or conditions based on certain criteria. There were also limitations in the current study in that we did not perform a detailed analysis of the participants’ medical history such as a present illness, a past history, and a family history.
Conclusion
Our model for estimating body shape biological age might be a novel approach to variation in body shape that is due to aging despite several limitations. We assume that our estimation model would be used as an adjunctive measure in easily predicting differences in body shape with the use of clinical parameters that are commonly used to assess the status of obesity in a clinical setting. Our results will provide baseline data for further studies to examine not only the effects of changes in body shape due to the aging process on the degree of aging in individuals, the rate of aging progression, and life expectancy, but they will also provide information surrounding correlations between body shape, disease, morbidity, and mortality.
Disclosure
The authors report no conflicts of interest in this work.
References
- PoehlmanETTothMJFishmanPSSarcopenia in aging humans: the impact of menopause and diseaseJ Gerontol A Biol Sci Med Sci199550Spec No73777493223
- BaumgartnerRNStauberPMMcHughDKoehlerKMGarryPJCross-sectional age differences in body composition in persons 60+ years of ageJ Gerontol A Biol Sci Med Sci1995506M3073167583802
- ChristmasCO’ConnorKGHarmanSMGrowth hormone and sex steroid effects on bone metabolism and bone mineral density in healthy aged women and menJ Gerontol A Biol Sci Med Sci2002571M121811773207
- EvansWJCampbellWWSarcopenia and age-related changes in body composition and functional capacityJ Nutr1993123Suppl 24654688429405
- WelbornTAKnuimanMWVuHTBody mass index and alternative indices of obesity in relation to height, triceps skinfold and subsequent mortality: the Busselton health studyInt J Obes Relat Metab Disord200024110811510702759
- StrainGWZumoffBThe relationship of weight-height indices of obesity to body fat contentJ Am Coll Nutr19921167157181460187
- WhitlockGLewingtonSSherlikerPfor Prospective Studies CollaborationBody-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studiesLancet200937396691083109619299006
- DesprésJPLemieuxIPrud’hommeDTreatment of obesity: need to focus on high risk abdominally obese patientsBMJ2001322728871672011264213
- ReederBASenthilselvanADesprésJThe association of cardiovascular disease risk factors with abdominal obesity in Canada. Canadian Heart Health Surveys Research GroupCMAJ1997157Suppl 1S39459220953
- PerryACApplegateEBAllisonMLMillerPCSignorileJFRelation between anthropometric measures of fat distribution and cardiovascular risk factors in overweight pre- and postmenopausal womenAm J Clin Nutr19976648298369322557
- SeidellJCHanTSFeskensEJLeanMENarrow hips and broad waist circumferences independently contribute to increased risk of non-insulin-dependent diabetes mellitusJ Intern Med199724254014069408070
- DesprésJPNadeauATremblayARole of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese womenDiabetes19893833043092645187
- FujiokaSMatsuzawaYTokunagaKTaruiSContribution of intraabdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesityMetabolism198736154593796297
- SeidellJCOosterleeADeurenbergPHautvastJGRuijsJHAbdominal fat depots measured with computed tomography: effects of degree of obesity, sex, and ageEur J Clin Nutr19884298058153181112
- PouliotMCDesprésJPLemieuxSWaist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and womenAm J Cardiol19947374604688141087
- WeiMGaskillSPHaffnerSMSternMPWaist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans – a 7-year prospective studyObes Res19975116239061711
- KimSMKimSSYounSJWhat is the best simple anthropometric indexes of abdominal visceral fat in obese patients?The Korean Journal of Obesity199872157168 [Korean]
- BorkanGAHultsDEGerzofSGRobbinsAHComparison of body composition in middle-aged and elderly males using computed tomographyAm J Phys Anthropol20056632892953985138
- ÖstmanJEfendićSArnerPCatecholamines and metabolism of human adipose tissueActa Med Scand19691861–62412464314050
- SeidellJCBjörntorpPSjöströmLKvistHSannerstedtRVisceral fat accumulation in men is positively associated with insulin, glucose, and C-peptide levels, but negatively with testosterone levelsMetabolism19903998979012202881
- WillettWCMansonJEStampferMJWeight, weight change, and coronary heart disease in women: risk within the “normal” weight rangeObstet Gynecol Surv1995507525528
- HuangZWillettWCMansonJEBody weight, weight change, and risk for hypertension in womenAnn Intern Med1998128281889441586
- JacobsEJNewtonCCWangYWaist circumference and all-cause mortality in a large US cohortArch Intern Med2010170151293130120696950
- OnatAHergencGSariIKarabulutACanGElevated LDL- cholesterol level predicts diabetes in centrally obese women but not men: relative roles of insulin resistance and central obesityCirc J20077191463146717721029
- WellsJCSexual dimorphism of body compositionBest Pract Res Clin Endocrinol Metab200721341543017875489
- WellsJCColeTJBrunerDTreleavenPBody shape in American and British adults: between-country and inter-ethnic comparisonsInt J Obes (Lond)200832115215917667912
- WellsJCColeTJTreleavenPAge-variability in body shape associated with excess weight: the UK National Sizing SurveyObesity (Silver Spring)200816243544118239656
- WellsJCGriffinLTreleavenPIndependent changes in female body shape with parity and age: A life-history approach to female adiposityAm J Hum Biol201022445646220035547
- WellsJCTreleavenPColeTJBMI compared with 3-dimensional body shape: the UK National Sizing SurveyAm J Clin Nutr200785241942517284738
- WellsJCCharoensiriwathSTreleavenPReproduction, aging, and body shape by three-dimensional photonic scanning in Thai men and womenAm J Hum Biol201123329129821387458
- BaumgartnerRNBody composition in healthy agingAnn N Y Acad Sci200090443744810865787
- FinkelDWhitfieldKMcGueMGenetic and environmental influences on functional age: a twin studyJ Gerontol B Psychol Sci Soc Sci1995502P1041137757832
- BorkanGANorrisAHAssessment of biological age using a profile of physical parametersJ Gerontol19803521771846967883
- BaeCYKangYGKimSDevelopment of models for predicting biological age (BA) with physical, biochemical, and hormonal parametersArch Gerontol Geriatr200847225326517889950
- van LeerEMvan NoordPASeidellJCComponents of adult height and height loss. Secular trend and effects of aging in women in the DOM projectAnn Epidemiol1992256116151342312
- GallowayAEstimating actual height in the older individualJ Forensic Sci19883311261363351449
- ClineMGMeredithKEBoyerJTBurrowsBDecline of height with age in adults in a general population sample: estimating maximum height and distinguishing birth cohort effects from actual loss of stature with agingHum Biol19896134154252807265
- AlbrightFSmithPHRichardsonAMPostmenopausal osteoporosisJ Am Med Assoc19411162224652474
- AdamsPDaviesGTSweetnamPOsteoporosis and the effects of ageing on bone mass in elderly men and womenQ J Med1970391566016154250827
- MiallWEAshcroftMTLovellHGMooreFA longitudinal study of the decline of adult height with age in two Welsh communitiesHum Biol19673944454546078969
- TrotterMGleserGThe effect of ageing on statureAm J Phys Anthropol19519331132414885427
- GsellOLongitudinal gerontological research over 10 years (Basel studies 1955–1965Gerontol Clin (Basel)19679267806055292
- BorkanGAHultsDEGlynnRJRole of longitudinal change and secular trend in age differences in male body dimensionsHum Biol19835536296416642483
- RibotCTremollieresFPouillesJMRisk factors for hip fracture. MEDOS study: results of the Toulouse CentreBone199314Suppl 1S77808110526
- BriotKLegrandEPouchainDMonnierSRouxCAccuracy of patient-reported height loss and risk factors for height loss among postmenopausal womenCMAJ2010182655856220308271
- HannanMTBroeKECupplesLADufourABRockwellMKielDPHeight loss predicts subsequent hip fracture in men and women of the Framingham StudyJ Bone Miner Res Epub November 9, 2011
- ChittawatanaratKPruenglampooSKongsawasdiSThe variations of body mass index and body fat in adult Thai people across the age spectrum measured by bioelectrical impedance analysisClin Interv Aging2011628529422162644
- BartaliBBenvenutiECorsiAMChanges in anthropometric measures in men and women across the life-span: findings from the InCHIANTI studySoz Praventivmed200247533634812512227
- BroadwinJGoodman-GruenDSlymenDAbility of fat and fat-free mass percentages to predict functional disability in older men and womenJ Am Geriatr Soc200149121641164511843997
- ShonCMKimJHShinSYChaKCA study of age-related patterns in body composition by segmental bioelectrical impedance analysis for KoreansJournal of the Korean Dietetic Association200172153158 [Korean]
- FalcigliaGO’ConnorJGedlingEUpper arm anthropometric norms in elderly white subjectsJ Am Diet Assoc19888855695743367013
- LeyCJLeesBStevensonJCSex- and menopause-associated changes in body-fat distributionAm J Clin Nutr19925559509541570802
- CouillardCGagnonJBergeronJContribution of body fatness and adipose tissue distribution to the age variation in plasma steroid hormone concentrations in men: the HERITAGE Family StudyJ Clin Endocrinol Metab20008531026103110720034
- HaarboJMarslewUGotfredsenAChristiansenCPostmenopausal hormone replacement therapy prevents central distribution of body fat after menopauseMetabolism19914012132313261961129
- TroisiRJWolfAMMasonJEKlinglerKMColditzGARelation of body fat distribution to reproductive factors in pre- and postmenopausal womenObes Res1995321431517719960
- SeidellJCVisscherTLBody weight and weight change and their health implications for the elderlyEur J Clin Nutr200054Suppl 3S333911041073