Abstract
Meningiomas of the spine are the most common benign intradural extramedullary lesions and account for 25%–46% of all spinal cord tumors in adults. The goal of treatment is complete surgical resection while preserving spinal stability. Usually, these lesions occur in the thoracic region and in middle-aged women. Clinical presentation is usually nonspecific and the symptoms could precede the diagnosis by several months to years, especially in older people, in whom associated age-related diseases can mask the tumor for a long time. We report a series of 30 patients, aged 70 years or more, harboring intradural extramedullary spinal meningiomas. No subjects had major contraindications to surgery. A minimally invasive approach (hemilaminectomy and preservation of the outer dural layer) was used to remove the tumor, while preserving spinal stability and improving the watertight dural closure. We retrospectively compared the outcomes in these patients with those in a control group subjected to laminectomy or laminotomy with different dural management. In our experience, the minimally invasive approach allows the same chances of complete tumor removal, while providing a better postoperative course than in a control group.
Introduction
Spinal meningiomas constitute approximately 25% of all spinal neoplasms.Citation1 There is a female predominance and nearly 80% of these tumors occur in the thoracic spine, followed in frequency by the cervical and lumbar regions.Citation2–Citation6 The majority are benign lesions, classically localized lateral to the spinal cord in an intradural extramedullary position.Citation1,Citation7 These tumors primarily affect middle-aged subjects but, with increasing life expectancy, symptomatic spinal meningiomas are being observed more frequently in elderly patients.Citation8,Citation9 The primary goal of spinal tumor surgery is to decompress the spinal cord and/or the roots involved by radical resection of the lesion, without creating spinal instability or worsening the preoperative neurological status. Choice of optimal surgical route mostly depends on the location and size of the tumor, but also on patient status and surgeon preference.Citation10 Posterior and lateral spinal meningiomas are generally approached via the posterior route, although some reports have demonstrated the feasibility of this route for ventral lesions as well.Citation11–Citation20 Conventional laminectomy provides a good working area, but several drawbacks still exist, including less protection in the event of a hematoma, possible constriction of the dura by epidural scarring, difficulty if a second surgery is required, and a high risk of postoperative spinal deformity.Citation21–Citation27 All these complications could result in a poor outcome, especially in frail elderly patients. This has led some surgeons to perform less invasive approaches, such as laminotomy, laminoplasty, and hemilaminectomy.Citation28
Currently, when applicable, we prefer to perform a hemilaminectomy or par tial hemilaminectomy with an interlaminar approach because it offers some advantages, including a shorter operative time, decreased intraoperative blood loss, and particularly a reduced risk of postoperative spinal instability.Citation29–Citation42 A controversial point in the literature concerns the best management of the dural attachment that is commonly resected or coagulated.Citation43 We have used another technique in our patients, first described by Saito et al in 2001, involving separation of the dura into an outer and inner layer, with the inner layer removed together with the tumor and the outer layer used for primary dural closure.Citation44 Here we review our 5 years of experience with intradural extramedullary spinal meningiomas in older subjects (>70 years) treated by techniques that are less invasive for both bony and dural structures, evaluating the impact of minimally invasive versus conventional approaches for tumor removal and spinal stability.
Materials and methods
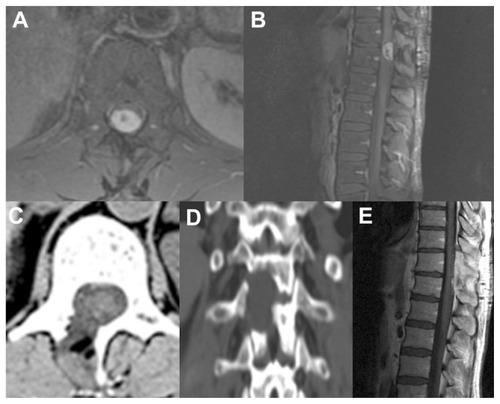
From January 2005 to December 2010, 30 elderly patients harboring spinal intradural extramedullary meningiomas were treated using a minimally invasive approach of hemilaminectomy and dural splitting. Mean age at presentation was 74.6 years. Ten patients were men and 20 were women. The diagnosis was made by contrast-enhanced magnetic resonance imaging (MRI) in 27 subjects and by computed tomography scan due to the presence of a cardiac pacemaker in three patients. No patient had major contraindications to surgery. Laminotomy or laminectomy with a traditional posterior midline approach and dural coagulation/resection was used in another 35 elderly subjects operated for spinal meningioma between January 1998 and December 2004. This latter group of patients was selected because they had characteristics similar to the first ones (). Because of the wide range in follow-up duration, the patients were compared 2 years after surgery. When possible, MRI was the diagnostic test of choice for assessing the extent of resection. If the postoperative course was uneventful and the immediate computed tomography scan was satisfactory, clinical and radiological (MRI) follow-up was performed at 3 and 6 months, and every year thereafter. On the other hand, in the event of suspected postoperative spinal instability, a dynamic x-ray was performed. and show two illustrative cases.
Table 1 Preoperative patient features
Figure 1 Illustrative case 1. (A–C) Preoperative axial, sagittal, and coronal magnetic resonance images showing a right upper cervical spine meningioma. (D) Postoperative computed tomography scan showing the unilateral approach. (E and F) Postoperative MRI demonstrating complete removal of the lesion.
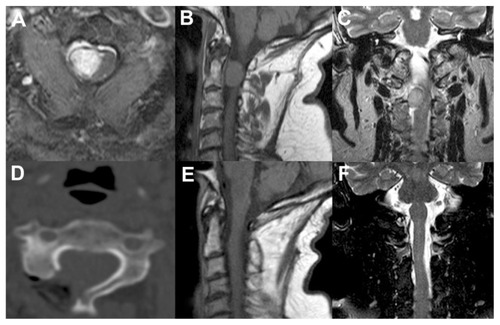
Figure 2 Illustrative case 2. (A and B) Preoperative axial and sagittal magnetic resonance images showing a meningioma of the thoracolumbar junction. (C and D) Postoperative axial and coronal computed tomographic scan demonstrating the minimally invasive unilateral approach. (E) Postoperative magnetic resonance image showing complete tumor resection.
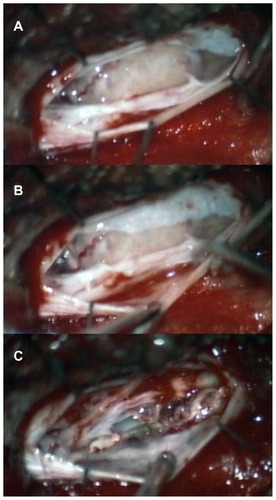
After careful preoperative planning, the patient was placed in the prone position under general anesthesia and a midline skin incision centered on the lesion was made. Somatosensory and transcranial motor evoked potentials along with free running electromyographies were monitored. Unilateral subperiosteal muscle dissection was carried out and the lamina or laminae were exposed. Depending on tumor size, we performed a monosegmental or multisegmental hemilaminectomy above and below the tumor. In the event of smaller lesions, a partial hemilaminectomy of the two contiguous laminae was preferred, using an interlaminar approach. The flavum ligamentum was removed until the contralateral root or dural curve was seen. Partial facetectomy (<50%), undercutting of the base of the spinous processes and contralateral lamina, oblique tilting of the operating table, or an endoscopy-assisted microsurgical technique were sometimes employed to visualize the contralateral side of the spinal canal better. Tumor resection was carried out using the technique described by Saito et al.Citation44 Under microscope vision, a small incision within the outer layer of the dura was made, which was stripped away from the inner layer using microforceps and microdissectors (). The tumor base could then be seen through the inner layer of the dura. After retracting the outer dural layer with stay sutures, a small incision was made with a microscalpel in the inner layer and continued around the tumor base. The lesion was freed from the surrounding dura and then carefully lifted up, using the arachnoid or pia membrane between the meningioma and spinal cord as a dissection plane (). Internal tumor debulking or its piecemeal resection helps the dissection and increase the working space. In the event of a lesion with ventral spreading, the dentate ligament was cut before internal decompression in order to facilitate handling of the spinal cord and avoid excessive mechanical retraction. After removal of the meningioma, the preserved outer dural layer was used to close the dura in a watertight fashion (). Fibrin glue and fat were applied epidurally to reinforce the closure.
Results
Gross total tumor removal was obtained in 28 patients and was subtotal in two cases in the group treated with hemilaminectomy and dural splitting. Mean operative time was 145 minutes. There was no major postoperative morbidity or mortality. No patient required additional surgery because of progressive spinal instability. Cerebrospinal fluid leak was observed in one patient with spontaneous resolution. The mean duration of hospital stay was 5.83 days. In elderly patients treated with a conventional technique and different dural management, the degree of tumor removal and recovery from neurological deficits was similar to that in the first group of subjects. The main postoperative differences concerned long-term posterior cervical and dorsal pain, radiological instability needing fixation, mean duration of the surgical procedure, length of hospital stay, number of cerebrospinal fluid leaks, and return to normal daily activities (). These results were not statistically significant.
Table 2 Summary of results
Discussion
Treatment of subjects with intradural extramedullary spinal meningioma has changed over the past 20 years. Advances in many disciplines, including neuroradiology, neurosurgery, neuro-oncology, and neuropathology, have contributed substantially to improving outcomes for patients. Despite this, delayed diagnosis still occurs, particularly in elderly patients, because symptoms can be misinterpreted and attributed to pre-existing or age-related diseases, such as degenerative spinal pathology, parkinsonism, and diabetic neuropathy.Citation4,Citation5,Citation15,Citation45,Citation46 The hesitation in performing spinal surgery in aged people may be related to the expectation of higher intraperioperative risk.Citation47 However, various operations, such as hip surgery, transurethral prostate resection, heart valve replacement, and coronary artery bypass surgery, are procedures performed routinely in large numbers of elderly patients.Citation48 Moreover, several clinical studies have demonstrated that spinal meningiomas have a good prognosis regardless of preoperative clinical findings, and even patients with a poor preoperative neurological status can respond favorably to surgery.Citation6,Citation49,Citation50 We are aware of the radiotherapy option, but think that when possible, microsurgical tumor removal still represents the best therapeutic option in older people as well.Citation51,Citation52 Radical removal of the lesion and preservation of spinal stability are the goals of surgery for these benign tumors, but some concerns arise as to what is the best way to do it.
Posterior approach
Tumor location is one of the most important factors affecting the clinical outcome.Citation29 Spinal meningiomas are usually localized lateral to the spinal cord, but 15%–27% of cases are located anteriorly and constitute a surgical challenge.Citation7 Although none of our patients had a purely ventral (anterior to the dentate ligament) meningioma, we believe that in aged subjects, if possible, a posterior approach needs to be used, regardless of tumor location. This route, in association with modern microsurgical and endoscopic techniques, provides adequate exposure to remove the vast majority of lesions safely. The risks related to the anterior approaches, in some patients, are not conterbalanced by benign nature of the tumor and long survival.Citation11,Citation15,Citation17,Citation19,Citation53 Furthermore, as in some of our patients, dentate ligament division, gentle cord rotation, and internal tumor decompression can provide additional space to deal with more anterior tumors.Citation1,Citation11,Citation53 However, in cases of ventral intradural lesions, anterior approaches are necessary, ie, for heavily calcified, densely fibrotic, highly vascular, or en plaque meningiomas with ventral attachment, and should be considered under appropriate circumstances.Citation53
Fortunately, we had only two cases with very dense adhesions (one meningioma was lateral in position and the other one was ventrolateral) and both these patients underwent a posterior unilateral approach with subtotal lesion removal. In fact, the tendency of some psammomatous meningiomas toward pial invasion is well known in the literature.Citation9 Posterior spinal approaches include laminectomy (removal of the spinous process and lamina), laminotomy (removal and subsequent reinsertion of the spinous process and lamina), laminoplasty (hinging of the lamina to allow access or reconstruction of the spinal canal), hemilaminectomy (unilateral removal of the lamina), and percutaneous techniques.Citation28,Citation39,Citation54
Hemilaminectomy
Total laminectomy is the conventional approach and has been used for surgical removal of spinal cord tumors. It offers some advantages to surgeons, such as familiar exposure and a wide view of the surgical field. However, this technique has some drawbacks that can complicate the postoperative outcome. It can produce spinal instability, epidural fibrosis, and postoperative axial pain.Citation21–Citation27,Citation38 Postlaminectomy kyphosis is well recognized and commonly associated with instability, resulting in anterior compression of the spinal cord that can cause progressive myelopathy.Citation30,Citation41,Citation55 Various alternative procedures were developed to reduce the risk of complications following laminectomy. Some authors have described the advantages of laminoplasty or laminotomy in maintaining postoperative stability and preventing epidural scarring.Citation35,Citation42,Citation56 On the other hand, Asazuma et al reported that extensive laminoplasty, although able to decrease spinal instability and the deformity rate, cannot completely prevent the progressive postoperative deformation of the normal spinal curvature.Citation41 However, these techniques are somewhat difficult, time-consuming, and have a high risk of dural laceration, especially in the elderly where the dura is thinner.Citation57 Although laminectomy, laminoplasty, and laminotomy require different degrees of bone removal, they all involve bilateral surgical stripping and denervation of posterior muscular and ligamentous structures that are essential for maintaining spinal stability.Citation27
Considering these issues, some authors have tried to reduce the surgical trauma by performing hemilaminectomy, which has a lower impact on spinal biomechanics.Citation33–Citation37,Citation58,Citation59 The rationale for hemilaminectomy involves preservation of the contralateral lamina, maintenance of the so-called “tension band”, and maintenance of the integrity of the supraspinous/interspinous ligaments and the contralateral paravertebral musculature.Citation32,Citation60 One possible disadvantage of unilateral hemilaminectomy is the narrow surgical corridor formed by the spinous process and ipsilateral facet joint that could increase the risk of dural tearing, nerve root damage, or incomplete tumor removal. However, undercutting of the base of the spinous process and contralateral lamina, facetectomy limited to <50% ( and ), oblique tilting of the operating table, and an endoscopy-assisted microsurgical technique help the surgeon to control the contralateral side of the spinal cord, thus allowing safer dissection of the tumor.Citation27,Citation61,Citation62 Yeo et al described another way to obtain more surgical space which involves ipsilateral dural tacking and suture with the base of the muscle or fascia near the facet joint, instead of lifting it up or suspending it.Citation38
Although hemilaminectomy proved to be a very promising and versatile procedure in several previous reports and in our patients, we are aware that there may be situations which are not fully manageable using this minimally invasive technique.Citation37 Tumors that involve the contralateral recess, bilateral extradural lesions, huge neoplasms with scalloping of vertebrae, easily bleeding tumors spreading to both sides, lesions with unclear borders, and intramedullary neoplasms may be difficult to manage using this approach.Citation30,Citation31,Citation55
Dural management
Treatment of tumor dural attachment is still a matter of debate. Resection of the dura mater involved (Simpson grade I), coagulation of the dural attachment (Simpson grade II), and peeling off of the inner dural layer from the outer one are three common procedures described in the literature.Citation43,Citation44,Citation63 Grade I Simpson resection is the most radical treatment option for spinal meningioma, although some reports have not confirmed the need for complete resection of the dura involved, and the long-term results of this technique have yet to be validated.Citation1,Citation4,Citation6,Citation15,Citation18,Citation50 Moreover, such aggressive treatment of the dura may increase the risk of cerebrospinal fluid leak.Citation18 Our policy, consistent with the literature, is to perform a grade I Simpson resection in young subjects (<50 years) harboring meningioma with interdural/ extradural extension, heavy calcification, and aggressive behavior (grade II–IV tumors).Citation7,Citation64 Cauterization of the dura mater attachment offers acceptable long-term results in terms of tumor recurrence rates, while the risk of postsurgical cerebrospinal fluid leak is markedly reduced in the event of pure intradural meningioma.Citation11,Citation15,Citation17–Citation19,Citation65 However, we think that excessive coagulation in a very thin and adherent dura, as often found in elderly patients, may cause its perforation or shrinkage and thus jeopardize primary dural closure. In the present series, we used the technique described by Saito et al, consisting of dural splitting into an outer and inner layer with removal of the meningioma en bloc along with the inner dural stratum ().Citation44 We have chosen this method to deal with the dural implant because of the advanced age of our patients, tumor features, and the possibility of obtaining a primary watertight dural closure using the preserved outer dural layer.
Our experience
The present study has some limitations due to the small number of patients, the short follow-up duration in some subjects, and the retrospective nature of our observations. However, our minimally invasive approach (hemilaminectomy and dural splitting) is relatively simple and straightforward, allowing good results in terms of total resection and postoperative quality of life. Compared with the group treated conventionally, our elderly subjects, who underwent a minimally invasive technique, experienced reduced intraoperative blood loss, a briefer surgical procedure, a shortened hospital stay, less cerebrospinal fluid leak, improved wound healing, faster recovery, and less disabling cervical and/or dorsal pain. All these benefits allow for earlier ambulation and rehabilitation, which are the major targets for good postoperative quality of life in patients, particularly elderly ones. We did not identify any disadvantages of hemilaminectomy in our patients, but if the surgeon feels unable to remove the tumor by this technique, the unilateral approach can be easily and quickly converted to a conventional laminectomy.
Conclusion
A minimally invasive approach and primary dural closure associated with good neuroanesthesia along with excellent preoperative postoperative care should be, in our opinion, the preferred way to manage elderly patients with spinal meningioma. The message of this paper is three-fold. The first relates to the preservation of spinal stability as a result of hemilaminectomy. The second emphasizes the importance of primary dural closure. The third concerns the posterior approach as the route of choice, whenever possible. All these issues have led us to tailor our surgical treatment to the individual patient, aiming to achieve the best possible result both in terms of tumor removal and functional outcome.
Disclosure
The authors report no conflicts of interest in this work.
References
- VoulgarisSAlexiouGAMihosEPosterior approach to ventrally located spinal meningiomasEur Spine J20101971195119920127494
- HirabayashiHTakahashiJKatoHEbaraSTakahashiHSurgical resection without dural reconstruction of a lumbar meningioma in an elderly womanEur Spine J200918Suppl 223223519219468
- HelsethAMørkSJPrimary intraspinal neoplasms in Norway, 1955 to 1986. A population-based survey of 467 patientsJ Neurosurg19897168428452585075
- LevyWJJrBayJDohnDSpinal cord meningiomaJ Neurosurg19825768048127143063
- RouxFXNatafFPinaudeauMBorneGDevauxBMederJFIntraspinal meningiomas: review of 54 cases with discussion of poor prognosis factors and modern therapeutic managementSurg Neurol19964654584648874546
- SoleroCLFornariMGiombiniSSpinal meningiomas: review of 174 operated casesNeurosurgery19892521531602671779
- Cohen-GadolAAZikelOMKochCAScheithauerBWKraussWESpinal meningiomas in patients younger than 50 years of age: a 21-year experienceJ Neurosurg200398Suppl 325826312691381
- MorandiXHaegelenCRiffaudLAmlashiSAdnMBrassierGResults in the operative treatment of elderly patients with spinal meningiomasSpine (Phila Pa 1976)200429192191219415454715
- SchallerBSpinal meningioma: relationship between histological subtypes and surgical outcome?J Neurooncol200575215716116132511
- PayerMRadovanovicIJostGResection of thoracic dumbbell neurinomas: single postero-lateral approach or combined posterior and transthoracic approach?J Clin Neurosci200613669069316797989
- KimCHChungCKSurgical outcome of a posterior approach for large ventral intradural extramedullary spinal cord tumorsSpine (Phila Pa 1976)2011368E53153721178841
- BeallDPGoogeDJEmeryRLExtramedullary intradural spinal tumors: a pictorial reviewCurr Probl Diagn Radiol200736518519817765798
- Slin’koEIAl-QashqishIIIntradural ventral and ventrolateral tumors of the spinal cord: surgical treatment and resultsNeurosurg Focus2004171ECP2
- ContiPPansiniGMouchatyHCapuanoCContiRSpinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literatureSurg Neurol2004611344414706374
- KlekampJSamiiMSurgical results for spinal meningiomasSurg Neurol199952655256210660020
- ArnautovićKIAl-MeftyOHusainMVentral foramen magnum meningiomasJ Neurosurg200092Suppl 1718010616061
- BassiouniHNtoukasVAsgariSSandalciogluEIStolkeDSeifertVForamen magnum meningiomas: clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approachNeurosurgery20065961177118717277680
- BoströmABürgelUReinacherPA less invasive surgical concept for the resection of spinal meningiomasActa Neurochir (Wien)2008150655155618421413
- SetzerMVatterHMarquardtGSeifertVVrionisFDManagement of spinal meningiomas: surgical results and a review of the literatureNeurosurg Focus2007234E1417961038
- SteckJCDietzeDDFesslerRGPosterolateral approach to intradural extramedullary thoracic tumorsJ Neurosurg19948122022058027802
- JönssonBAnnertzMSjöbergCStrömqvistBA prospective and consecutive study of surgically treated lumbar spinal stenosis. Part II: five years follow-up by an independent observerSpine (Phila Pa 1976)19972224293829449431630
- IidaYKataokaOShoTPostoperative lumbar spinal instability occurring or progressing secondary to laminectomySpine (Phila Pa 1976)19901511118611892148439
- LonsteinJEPostlaminectomy spinal deformityLonsteinJEBradfordDSWinterRBOgilvieJWMoe’s Textbook of Scoliosis and Other Spinal Deformities3rd edPhiladelphia, PAWB Saunders1995
- MayfieldFHComplications of laminectomyClin Neurosurg197623435439975694
- WinterRBHallJEKyphosis in childhood and adolescenceSpine (Phila Pa 1976)197834285308741235
- YasuokaSPetersonHAMacCartyCSIncidence of spinal column deformity after multilevel laminectomy in children and adultsJ Neurosurg19825744414457108592
- YaşargilMGTranmerBIAdamsonTERothPUnilateral partial hemi-laminectomy for the removal of extra- and intramedullary tumours and AVMsAdv Tech Stand Neurosurg1991181131321930371
- YucesoyKSonntagVKTerminology confusion in spinal surgery: laminotomy, laminoplasty, laminectomyJ Neurosurg200092237110659036
- CanbaySHasturkAEBasmaciMErtenFHarmanFManagement of thoracal and lumbar schwannomas using a unilateral approach without instability: an analysis of 15 casesAsian Spine J201;61434922164313
- BertalanffyHMitaniSOtaniMIchikizakiKToyaSUsefulness of hemilaminectomy for microsurgical management of intraspinal lesionsKeio J Med199241276791619851
- NaganawaTMiyamotoKHosoeHSuzukiNShimizuKHemilaminectomy for removal of extramedullary or extradural spinal cord tumors: medium to long-term clinical outcomesYonsei Med J201152112112921155044
- SunCXMengXLXieSNYuYYangHJWuBUnilateral hemilaminectomy for patients with intradural extramedullary tumorsJ Zhejiang Univ Sci B201112757558121726065
- TaylorASUnilateral laminectomyAnn Surg191051452953317862515
- PanjabiMMWhiteAA3rdBasic biomechanics of the spineNeurosurgery19807176937413053
- OktemISAkdemirHKurtsoyAKoçRKMenküATucerBHemilaminectomy for the removal of the spinal lesionsSpinal Cord2000382929610762181
- OgdenATBresnahanLSmithJSNatarajanRFesslerRGBiomechanical comparison of traditional and minimally invasive intradural tumor exposures using finite element analysisClin Biomech (Bristol, Avon)2009242143147
- ChiouSMEggertHRLabordeGSeegerWMicrosurgical unilateral approaches for spinal tumor surgery: eight years’ experience in 256 primary operated patientsActa Neurochir (Wien)19891003–41271332589118
- YeoDKImSBParkKWShinDSKimBTShinWHProfiles of spinal cord tumors removed through a unilateral hemilaminectomyJ Korean Neurosurg Soc201150319520022102948
- MannionRJNowitzkeAMEfendyJWoodMJSafety and efficacy of intradural extramedullary spinal tumor removal using a minimally invasive approachNeurosurgery201168Suppl Operative 120821621206315
- YuYZhangXHuFXieTGuYMinimally invasive microsurgical treatment of cervical intraspinal extramedullary tumorsJ Clin Neurosci20111891168117321763145
- AsazumaTNakamuraMMatsumotoMChiboKToyamaYPostoperative changes of spinal curvature and range of motion in adult patients with cervical spinal cord tumors: analysis of 51 cases and review of the literatureJ Spinal Disord Tech200417317818215167332
- BalakNUnilateral partial hemilaminectomy in the removal of a large spinal ependymomaSpine J2008861030103617938003
- YamamuroKSeichiAKimuraAHistological investigation of resected dura mater attached to spinal meningiomaSpine (Phila Pa 1976)20123722E1398140122805341
- SaitoTArizonoTMaedaTTeradaKIwamotoYA novel technique for surgical resection of spinal meningiomaSpine (Phila Pa 1976)200126161805180811493855
- HuangCYMathesonJSpinal cord tumors in the elderlyAust N Z J Med197995538541294909
- KhodadadGCommon errors in the diagnosis of spinal meningiomasGeriatrics19732811431454683088
- DrippsRDLamontAEckenhoffJEThe role of anesthesia in surgical mortalityJAMA196117826126613887881
- McIntyreABBallengerJFKingATCoronary artery bypass surgery in the elderlyJ S C Med Assoc19908684354392214680
- GezenFKakrahamSCanakciZBedükAReview of 36 cases of spinal cord meningiomasSpine (Phila Pa 1976)200025672773110752106
- GottfriedONGlufWQuinones-HinojosaAKanPSchmidtMHSpinal meningiomas: surgical management and outcomeNeurosurg Focus2003146e215669787
- SachdeySDoddRLChangSDStereotactic radiosurgery yields long-term control for benign intradural, extramedullary spinal tumorsNeurosurgery201169353353921832967
- PostalciLTugcuBGungorAGucluGSpinal meningiomas: recurrence in ventrally located individuals on long-term follow-up; a review of 46 operated casesTurk Neurosurg201121444945322194098
- AngevinePDKellnerCHaqueRMMcCormickPCSurgical management of ventral intradural spinal lesionsJ Neurosurg Spine2011151283721495815
- LuDCDhallSSMummaneniPVThe transspinous mini-open approach for resection of intradural spinal neoplasms: cadaveric feasibility study and report of 3 clinical casesWorld Neurosurg201074119519921300013
- OzawaHKokubunSAizawaTHoshikawaTKawaharaCSpinal dumbbell tumors: an analysis of a series of 118 casesJ Neurosurg Spine20077658759318074682
- SongYKJahngTAThe usefulness of laminoplasty in cervical spinal cord tumor surgeryJ Korean Neurosurg Soc2004353261266
- ParkinsonDReplacement laminotomySurg Neurol197784277279898005
- AbbottRFeldsteinNWisoffNEpsteinFJOsteoplastic laminotomy in childrenPediatr Neurosurg19921831531561457375
- EggertHRScheremetRSeegerWGaitzschJUnilateral microsurgical approaches to extramedullary spinal tumors. Operative technique and resultsActa Neurochir1983673–4245253
- HottaHAn experimental study on stability of human spine, especially the role of the lumbar ligamentsJ Jpn Orthop Assoc197650114
- TredwayTLSantiagoPHrubesMRSongJKChristieSDFesslerRGMinimally invasive resection of intradural-extramedullary spinal neoplasmsNeurosurgery200658Suppl 1ONS525816479629
- ZdeblickTAZouDWardenKEMcCabeRKunzDVanderbyRCervical stability after foraminotomyJ Bone Joint Surg Am199274122271734010
- AhnDKParkHSChoiDJKimKSKimTWParkSYThe surgical treatment for spinal intradural extramedullary tumorsClin Orthop Surg20091316517219885053
- NakamuraMTsujiOFujiyoshiKLong-term surgical outcomes of spinal meningiomasSpine (Phila Pa 1976)20123710E61762322146282
- SchickUMarquardtGLorenzRRecurrence of benign spinal neoplasmsNeurosurg Rev2001241202511339463