Abstract
Treatment of hypertension in the elderly is expected to become more complex in the coming decades. Based on the current landscape of clinical trials, guideline recommendations remain inconclusive. The present review discusses the latest evidence derived from studies available in 2013 and investigates optimal blood pressure (BP) and preferred treatment substances. Three common archetypes are discussed that hamper the treatment of hypertension in the very elderly. In addition, this paper presents the current recommendations of the NICE 2011, JNC7 2013-update, ESH/ESC 2013, CHEP 2013, JNC8 and ASH/ISH guidelines for elderly patients. Advantages of the six main substance classes, namely diuretics, beta-blockers (BBs), calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and direct renin inhibitors (DRIs) are discussed. Medical and economic implications of drug administration in the very elderly are presented. Avoidance of treatment-related adverse effects has become increasingly relevant. Current substance classes are equally effective, with similar effects on cardiovascular outcomes. Selection of substances should therefore also be based on collateral advantages of drugs that extend beyond BP reduction. The combination of ACEIs and diuretics appears to be favorable in managing systolic/diastolic hypertension. Diuretics are a preferred and cheap combination drug, and the combination with CCBs is recommended for patients with isolated systolic hypertension. ACEIs and CCBs are favorable for patients with dementia, while CCBs and ARBs imply substantial cost savings due to high adherence.
Introduction
In the last decade, life expectancy has increased remarkably in affluent Western societies.Citation1 In the USA, approximately 39 million people (13% of the population) were aged ≥65 years in 2008 and this number is expected to increase to 72 million (20% of the population) in 2030.Citation2 In the European Union, over 30% of the population will be older than 65 years by 2060, and in Germany octogenarians will account for 14% of the population in 2060.Citation3,Citation4 In patients >65 years of age, 78% of older women and 64% of older men have either diagnosed or undiagnosed hypertension. Based on the age-dependent blood pressure (BP) targets currently recommended by the ESH/ESC (European Society of Hypertension/European Society of Cardiology) guidelines,Citation5 it is appropriate to differentiate between the “elderly” and the “very elderly” in this review. The “elderly” comprises the group of patients aged ≥65 years. Patients 80 years and older are considered “very elderly” as described by Gueyffier et al for the Individual Data Analyses Antihypertensive Intervention (INDANA) groupCitation6 and in the Hypertension in the Very Elderly Trial (HYVET).Citation7
Due to improvements in diagnosis and treatment, long-term consequences of arterial hypertension have shifted towards the elderly/very elderly population, but treatment has become more difficult in the light of comorbidities.Citation8 In addition, the tablet burden in octogenarians hampers adherence to medication, and diseases requiring intensified treatment have their highest occurrence in the very elderly.Citation9 The following three archetypes characterize current challenges in high-age patient management.
Discrepancy between required evidence and investment in clinical trials: it is difficult to obtain reliable long-term data because the average life expectancy of patients included in clinical trials is shorter than the duration of these studies. Another problem is that generation of specific evidence in the elderly and very elderly is expensive, while the anticipated revenue for pharmaceutical companies is relatively low. Low evidence leads to guideline ambiguity, subjective treatment decisions, and low target blood pressure attainment (TBPA).Citation10
Eroding goals in treatment: an increasing number of physicians believe in comfortable end-of-life-management with less aggressive treatment.Citation11 In a 2002 survey, 25% of physicians believed that treatment of patients aged ≥85 years implied more risks than benefits,Citation12 and over 58% of physicians only initiate antihypertensive treatment when patients’ systolic blood pressure (SBP) exceeds 160 mmHg. In a Spanish trial, physicians perceived uncontrolled BP in 44.1% of patients as being well controlled.Citation13 This perception is possibly based on the fallacy that BP levels need to be higher in older patients because of atherosclerotic alterations of cerebral vessels.
Attractiveness principle in competing disease areas: polypharmacy in the very elderly is unfortunate because treatment gets prioritized according to the severity of comorbidities and side-effects. As hypertension does not usually affect patient quality of life, other treatments are often favored.
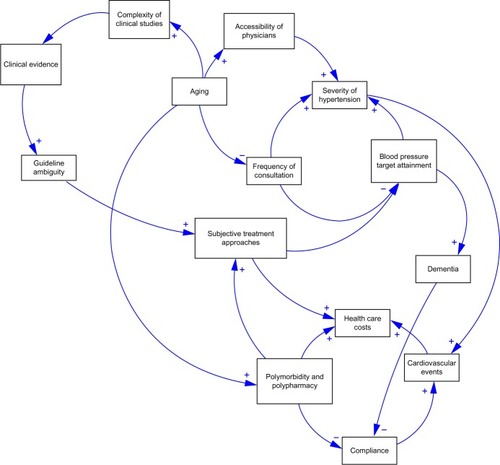
summarizes the challenges in antihypertensive treatment of the elderly and very elderly.
In the last couple of years, several revisions to international guidelines have been undertaken to establish the most appropriate treatment by defining BP goals and recommended substances in the very elderly. Very recently the JNC (Joint National Committee)8 guidelinesCitation14–Citation18 and additionally ASH/ISH (American Society of Hypertension/International Society of Hypertension) practical guidelinesCitation19 were released, with potentially more recommendation in collaboration with American Heart Association (AHA) and American College of Cardiology (ACC) to come by the end of 2014 or early 2015.Citation20 The AHA, ACC, and Centers from Disease Control and Prevention (CDC) had just before published their “science advisory” on effective approaches for managing high blood pressure.Citation21–Citation23
The aims of the present review are as follows:
To present the latest evidence from trials with regard to optimal BP and preferred substances in 2013.
To review the current recommendations of NICE (National Institute for Health and Clinical Excellence) 2011Citation24 and the 2013 updates of the JNC7,Citation25 ESH-ESC,Citation5 CHEP (Canadian Hypertension Education Program),Citation26 JNC8,Citation14 and ASH/ISH practical guidelines.Citation19
To discuss advantages of the six main substance classes, namely diuretics, beta blockers (BBs), calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and direct renin inhibitors (DRIs).
To highlight medical and economic implications of drug administration in the very elderly.
BP levels that establish the diagnosis of hypertension and set targets for therapy
Lowering BP in a timely fashion has been shown to be beneficial with regard to cardiovascular outcome in hypertensive patients aged ≥67 years.Citation27 A recent meta-analysis comparing treatment and placebo groups showed intergroup BP reductions of 27.3/11.1 mmHgCitation28 and significant reductions in all-cause death, cardiovascular death, stroke, and heart failure in patients aged ≥65. Thus, BP lowering is a simple and therapy-independent concept to lower cardiovascular risk.Citation5,Citation29 However, controversy remains regarding when to initiate treatment and what the optimal treatment goals are for this population.
On the one hand, the HYVET landmark trialCitation30 demonstrated substantial reduction in fatal and non-fatal stroke, all-cause mortality, and cardiovascular disease in octogenarians treated who had a sustained SBP ≤160 mmHg. On the other hand, another meta-analysisCitation31 showed only reduction of stroke risk, cardiovascular events, and heart failure, while all-cause mortality remained high. Even more surprisingly, all-cause mortality was lowest in trials with the least BP reductions and the lowest therapy intensity. The difference between the two analyses may derive from the fact that in frail, elderly subjects with a diversity of comorbidities the potential benefit of antihypertensive treatment may be blunted by competing risks. Also, the expected protective effect of BP lowering seems to become progressively smaller with increasing age.Citation32 As the average age in the HYVET trial was 84 years, there are few data available for the very elderly. Despite this problem, the results of HYVET have been implemented in the new ESH/ESC guidelines: BP should be reduced in patients >80 years and with initial SBP >160 mmHg to values between 140 mmHg and 150 mmHg, provided that octogenarians are in good physical and mental condition. In physically fit hypertensive patients <80 years old with SBP >140 mmHg, BP values <140 mmHg may be considered, but in the fragile elderly population SBP should be adapted to individual tolerability. If patients live to >80 years of age they should continue their antihypertensive treatment if well tolerated.Citation5 The newly relased JNC8Citation14,Citation15 guidelines are mostly in line with the ESH/ESC guidelines. In patients ≥60 years, JNC8 recommends lowering BP below 150/90 mmHg. In the ASH/ISH guidelines,Citation19,Citation20 age thresholds of BP ≥150/90 mmHg apply to patients ≥80 years. With regard to the ASH/ISH guidelines, the scientific community argues that they were not developed according to the guideline process and thus should rather be considered as an “opinion piece”.Citation20 In general, BP target recommendations should mitigate any effect potentially associated with the “J-curve effect” discussed by Banach and Aronow.Citation33
Recent late-outcome trials with more aggressive BP control have observed the J-curve effect in hypertensive patients, in patients with coronary artery disease, diabetes mellitus and left ventricular hypertrophy, and in elderly patients.Citation34 When BP was lowered below a specific nadir, risk of coronary events (but not stroke) increased. Lowering diastolic BP (DBP) can lead to a critically reduced perfusion of the coronary arteries during the diastolic phase of the cardiac cycle. In healthy subjects, coronary pressure autoregulation provides a relatively constant perfusion to the myocardium over a fairly wide perfusion pressure ranging from 45 mmHg to 125 mmHg. In patients with coronary heart disease, hypertension, and left ventricular hypertrophy, the autoregulation is no longer functional and the fractional flow reserve will be compromised and may lead to myocardial ischemia and myocardial infarction.Citation35 The human brain is the organ that depends mostly on SBP. Cerebral blood flow autoregulation can operate at a mean arterial pressure between 60 mmHg and 150 mmHg. Still, it seems that the heart is more vulnerable to BP changes than the brain, which has a much wider BP autoregulatory range.
In a secondary analysis of the INVEST (the INternational VErapamil SR/Trandolapril STudy) trial,Citation36 hypertensive patients (≥50 years of age) with coronary artery disease were treated with two different regimens. Grouped in 10-year increments, the adjusted hazard ratio for primary outcomes (all-cause death, non-fatal myocardial infarction, or non-fatal stroke) revealed a J-shape relationship between treatment SBP and DBP. Although all age groups showed a J-shaped curve, there was a progressive increase in SBP with increasing age. In very old patients (≥80 years) the systolic pressure hazard ratio nadir was 140 mmHg,Citation37 compared with the nadir of 110 mmHg for patients <60 years. However, the hazard ratio nadir for DBP was only marginally lower for those ≥80 years (70 mmHg) than for their younger counterparts (75 mmHg). Overall, the incidence of stroke was much less than myocardial infarction and correlated with low SBP, whereas the incidence of myocardial infarction was correlated with low DBP.
In a Japanese trial, PATE-Hypertension II (Practitioner’s trial on the efficacy of antihypertensive treatment in elderly patients with hypertension II), excessive SBP reduction to less than 120 mmHg (in patients ≥75 years) appeared to be harmful, leading to higher cardiovascular/cerebrovascular morbidity and mortality than in patients with a SBP of 120–139 mmHg.Citation38
Even though the J-curve phenomenon has been shown in many trials, its physiological correlation is not yet understood. As a result, this issue should be studied in a correctly designed trial comparable to the HOT (Hypertension Optimal Treatment) trial.Citation39 The SPRINT (Systolic Blood Pressure Intervention Trial) trialCitation40 will hopefully clarify if a SBP of <120 mmHg will demonstrate lower cardiovascular disease event rates than a SBP of 140 mmHg. The trial will randomize approximately 9,250 patients ≥50 years of age with a SBP of ≥130 mmHg and with at least one additional cardiovascular disease risk factor, and will run until late 2018.
The ESH-CHL-SHOT (European Society of Hypertension and Chinese Hypotension League Stroke in Hypertension Optimal Treatment) trial will randomize 7,500 patients aged ≥65 years with SBP ≥140 mmHg and history of previous stroke or transient ischemic attack (TIA). Patients will be randomly allocated into one of three different sitting SBP targets: <145–135 mmHg, <135–125 mmHg, and <125 mmHg. The endpoint will be collected after approximately 4–5 years and will include recurrent stroke, major cardiovascular events, cognitive impairment, and dementia.Citation41
Ambulatory BP measurement: improved understanding of BP variability in the elderly
BP variability in the elderly is high due to baroreflex failure and increased arterial stiffness, with periods of hyper- and hypotension throughout the day. White-coat hypertension, an increase in 24-hour pulse pressure and the prevalence of 24-hour isolated systolic hypertension, exaggerated ambulatory BP variability, morning BP surge, disrupted diurnal BP variation (non-dipping), and postural and postprandial hypotension are more common in the elderly and need to be considered so that treatment can be tailored appropriately.Citation42 Twenty-four-hour SBP is more closely related to outcome (fatal or non-fatal cardiovascular events and/or total mortality) than office BP. Twenty-four-hour ambulatory pulse pressure demonstrates a greater association with stroke than with coronary artery disease (CAD). Outcome worsening will also be observed in non-dippers and in patients with nocturnal hypertension and with an exaggerated morning BP surge. Disruption of the circadian BP variation is also associated with orthostatic BP dysregulation. Postural and postprandial hypotension can be exaggerated by antihypertensive drugs (diuretics, alpha-blockers, neuroleptics, antidepressants) and is best diagnosed by ambulatory BP monitoring.
Pharmacological treatment in the light of an aging organism
Although oral absorption of drugs is not significantly affected by aging, drug distribution can be influenced by lean body mass and decreased proportion of body water. Drug half-life time and excretion can be disturbed by liver and kidney functional deterioration. Also, pharmacodynamic effects become relevant due to changes in end-organ responsiveness (decreased baroreceptor sensitivity leading to orthostatic hypotension) and may limit the use of vasodilators. A recent analysis of 61,661 elderly Japanese patientsCitation43 showed that the risk of adverse drug interactions in hypertensive patients increased with age and rose dramatically per 10,000 person-days from 2.0 (monotherapy) to 5.1 (co-medication), and up to 8.6 (polypharmacy). Further risk occurs with hyperglycemia induced by diuretics. BBs may cause acute cardiac decompensation in elderly patients with congestive heart failure, intermittent claudication in patients with peripheral vascular disease, and bronchoconstriction in patients with chronic obstructive pulmonary disease. Agents that increase the antihypertensive effect of BBs and calcium antagonists (CCBs), including cimetidine, antifungals, and grapefruit juice (cytochrome P4503A), should be considered with care. Non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, erythropoietin, amphetamines, ergotamine, and anabolic steroids may further increase BP in elderly patients.
Are there BP sex differences in the elderly?
Both the prevalence and severity of hypertension are greater in elderly women than in elderly men. It is more difficult to achieve BP control in elderly women than in elderly men, and there seem to be differences in antihypertensive treatment patterns between them. Reasons for these differences are difficult to decipher, but could be due to inadequate treatment intensity, inappropriate drug choices, lack of compliance, treatment resistance because of biological factors, or to other factors (eg, central obesity, and so on).
Is there a “right” drug for treatment of hypertension in the elderly?
The question of the “right drug” in the very elderly has caused endless debate in various societies and guideline committees. One hundred and forty-seven randomized trials involving 464,000 patients have shown that all classes of BP-lowering drugs have similar effects in reducing events and stroke for a given reduction in BP.Citation44 Therefore, no drug has been consistently superior across all important outcomes.Citation45 Only BBs (atenolol) and alpha-blockers (see alpha and beta-blocker section) should not be first-choice drugs as they are not superior to any other drug class for any outcome.
Another recent meta-analysisCitation28 included 18 clinical studies and examined 55,569 hypertensive patients and 59,285 controls. The study compared all commonly used antihypertensive therapies with each other (baseline BP 157/86 mmHg; BP reduction to less than 140/80 mmHg) and found that a similar BP reduction resulted in equivalent risk reduction for the substances compared.
A third prospective meta-analysis comparing younger and older hypertensives (≥65 years) treated with different antihypertensive drugs substantiated previous results and found similar drug-class efficacy in younger and older patients.Citation46 Hence, all these investigations show limited evidence of pivotal differences between various drug classes; treatment success is dependent on which collateral outcome is preferred.
Guideline recommendations
The latest ESH/ESC guidelinesCitation5 recommend antihypertensive treatment classes that appeared beneficial in reducing cardiovascular risk in randomized clincial trials. All hypertensive agents are recommended (), but diuretics and CCBs may be preferred in patients with isolated systolic hypertension (ISH). Former US guidelines (JNC7) favored thiazide-type-diruetics when commencing antihypertensive therapy in patients without other compelling indications.Citation25 JNC8Citation14 lately backs away from the JNC7 recommendation that thiazide-type diuretics should be initial therapy in most patients, suggesting ACEIs, ARBs, CCBs, or thiazide-type diuretics are reasonable choices in nonblacks. In black patients, thiazide-type diuretics and CCBs are recommended as first-line therapy for hypertension. The ASH/ISH guidelinesCitation19 recommend different drugs for the initial therapy, depending on patients’ age, race, and blood pressure levels. They mention ACEIs or ARBs for nonblack patients under the age of 60 and a CCB or thiazide in nonblack patients over the age of 60. The most recent Canadian guideline update strongly emphasizes ISH as a special entity rather than simply acknowledging “age” alone, and recommends thiazides, ARBs, and CCBs.Citation26 In contrast, NICE 2011 is fairly rigid with regard to treatment recommendations and does not recommend different treatment approaches for patients below and above 80 years of age.Citation24
Table 1 Comparison of recommended target blood pressure goals and substance classes in the elderly
Since ACCOMPLISH (Avoiding Cardiovascular events through COMbination therapy in Patients Living with Systolic Hypertension),Citation47 the ACEI/CCB combination has shown substantial benefits in the overall population and in patients >70 years. These results were reflected 2 years later in the 2011 NICE recommmendations. An overview of the most recent JNC7, ESH/ESC, CHEP and NICE guidelines is presented in . A comparison between the latest JNC8 and ASH/ISH is given in .
Table 2 Comparison of latest divergent guideline-recommendations of ASH/ISH 2013 and JNC8 2014
Pharmacological treatment with different drug classes
Diuretics
Thiazide diuretics (hydrochlorothiazide [HCTZ], chlorthalidone, and indapamide [thiazide-like]) are recommended for initiating therapy and are generally well tolerated. Diuretics control hypertension by inhibiting reabsorption of sodium and chloride ions from the tubules in the kidney. They lead to an early reduction of intravascular volume and peripheral vascular resistance, causing a reduction in BP. The thiazide-associated decrease in peripheral vascular resistance could be the result of a direct vasodilatory effect, perhaps separately from the diuretic effect of HCTZ. One proposed effect of HCTZ is its direct vascular relaxant effects via opening of the calcium-activated potassium (KCa) channel. Another hypothesis is that HCTZ inhibits carbonic anhydrase so that the KCa channel gets activated by the increased intracellular pH. Further potential mechanisms of the direct and indirect vasodilatory effects of HCTZ are described by Duarte and Cooper-DeHoff.Citation48 A number of clinical studies in the elderly have shown reduced incidence of cardiovascular events with thiazide (mean age ALLHAT [Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial]: 67 years, SHEP [the Systolic Hypertension in the Elderly Program]: 72 years, HYVET: 84 years, EWPHE [European Working Party on High blood pressure in the Elderly study]: 72 years).
However, at the same time, elderly patients run a higher risk of hypovolemia and are more prone to orthostatic hypotension due to reduced baroreceptor sensitivity.
Chlorthalidone differs pharmacokinetically from HCTZ due to its longer action. However, whether chlorthalidone really exhibits stronger potency has to be evaluated in future trials. In recent retrospective studies, no statistical difference in the primary outcome (composite of mortality and hospitalization for cardiovascular events) could be observed between chlorthalidone and HCTZ. On the contrary, chlorthalidone was associated with greater incidence of electrolyte abnormalities in older adults compared to HCTZ.Citation49
Although thiazides had been considered first-line therapy in hypertension some controversy exists with regard to antihypertensive efficacy, effect on morbidity and mortality, and adverse drug reactions of this substance in the elderly.Citation50
After a 1-year follow-up, only 39% of all patients remained on diuretic therapy. According to statistics on adverse drug reactions leading to hospitalization, diuretics are among the five leading drug classes. Finally, thiazide diuretics, as compared to thiazide-like diuretics (indapamide), increase uric acid, potentially expediting the development of gout through volume contraction and competition with uric acid for renal tubular secretion. All diuretics cause electrolyte disturbances; in conjunction with left ventricular hypertrophy this can provoke ventricular arrhythmias and sudden death. Thiazides are also diabetogenic, can cause dyslipidemia, and can reduce lithium excretion and precipitate lithium toxicity. In combination with BBs, thiazides have the potential to increase fatigue and glucose levels. While NSAIDs hamper the potency of thiazides, potassium and renal function need to be monitored carefully in light of renal insufficiency and the danger of hyperkalemia.
Beta-blockers
BBs should be used in combination therapy, usually with diuretics in elderly patients who have additional cardiovascular conditions, such as coronary heart disease (CHD), particularly in individuals with a history of myocardial infarction (MI), systolic heart failure, or arrhythmias. The inhibition of catecholamine-mediated cardiotoxic effects and hyperactivity of the sympathetic system play a role in younger patients, whereas the mechanism for lowering BP is based on a decrease of cardiac output, inhibition of renin release, decrease of angiotensin II (AII) production, and blockade of presynaptic adrenoceptors that decrease central vasomotor activity.Citation51 In several large studies and meta-analyses, BBs have failed to provide benefits as a first-line antihypertensive drug compared to other therapies.Citation52,Citation53 BBs only show modest reductions in cardiovascular events and no significant effects on mortality.Citation51,Citation54 Reasons for the negligible cardiovascular protection include their inability to lower central aortic pressure (pseudo-antihypertensive efficacy), unfavorable metabolic effects, and their lack of regressive effects on left ventricular hypertrophy and endothelial dysfunction.
In ISH patients, BBs lead to a compensatory increase in stroke volume due to their negative chronotropic effect. Subsequently, this leads to a further elevation in SBP and a decrease in DBP, which exacerbates pulse pressure even more. Although it was thought that lowering heart rate is associated with a positive effect on outcome, this assumption has not held true.Citation55
There can also be differences between various sub-types of BBs. The newer BBs, such as nebivolol and carvedilol, which have vasodilatory properties, may provide better morbidity and mortality outcomes and safety profile. A definitive answer would have to come from prospective randomized controlled trials. Overall, BB tolerability is poor, indicated by substantial drop-out rates in clinical trials. Drowsiness, lethargy, sleep disturbance, visual hallucinations, and depression are side-effects that hamper life quality, even more so in elderly and very elderly patients.
Calcium channel blockers
Three sub-classes of CCBs block the influx of calcium ions into the cells of vascular smooth-muscle and myocardial tissue: phenylalkylamines (verapamil), benzothiazepines (diltiazem), and dihydropyridines (eg, nifedipine, amlodipine, and nitrendipine). CCBs inhibit the contraction of coronary and peripheral arterial smooth-muscle cells that are considerably more dependent on external calcium than the heart and skeletal muscle. As a result, CCBs dilate coronary and peripheral arteries without jeopardizing the heart or muscle contractibility. In addition, they influence the sinus node function, atrioventricular conduction, and coronary circulation. A special attribute of dihydropyridines is the decrease of cytosolic free calcium, leading to a lower vasomotor tone (especially at the arteriolar level), and thus lower peripheral resistance. With this mode of action, CCBs are particularly suited for the treatment of stiffening arteries, angina, and supraventricular arrhythmias. Side-effects of dihydropyridines are ankle edema, headache, and postural hypotension. Verapamil and diltiazem may cause heart block in elderly patients. The first generation of CCBs (nifedipine, verapamil, and diltiazem) should be avoided in patients with left ventricular systolic dysfunction. A variety of studies have shown dihydropyridines to be beneficial in patients with ISH, high age, diabetes, atherosclerosis, stroke,Citation56 and dementia.Citation57 One meta-analysis involving 9,138 patientsCitation58 demonstrated that CCBs attenuate the rate of progression of carotid intima–media thickening. Further benefits in favor of dihydropyridines have been reported in the CAFÉ (Conduit Artery Function Evaluation) studyCitation59 where the combination of CCB/ACEI yielded a higher central BP-lowering effect than the ACEI/diuretic combination. Interestingly, no difference has been reported for brachial BP. The CAFÉ study provides a plausible explanation, at least in part, for the better clinical outcome in patients treated with amlodipine/perindopril. The ACCOMPLISH trial has substantiated these findings. Benazepril/amlodipine was shown to be superior, with a 20% lower incidence of cardiovascular mortality and a 17% lower rate of cardiovascular events than HCTZ/benazepril, independent of age and the presence of CAD.Citation60 On the other hand, a recent meta- analysis of 31 randomized controlled trials involving 273,543 participants showed that CCBs were not different to ACEIs and diureticsCitation61 for lowering stroke rates. In analogy to the ACCOMPLISH trial,Citation60 the COLM (Combination of OLMesartan and CCB or Low Dose Diuretics in High Risk Elderly Hypertensive Patients) study compares combination therapy using an ARB (olmesartan) and a CCB with the combination of an ARB and a diuretic in high-risk elderly (65–84 years) hypertensive patients.Citation62 A total of more than 4,000 patients were recruited and were followed up for at least 3 years. The study has been completed, but the results are still outstanding.Citation62 In the NICE guidelines,Citation24 CCBs are recommended as initial therapy for all patients older than 55 years of age. This recommendation is based on the low withdrawal rates with CCBs found in the ASCOT (Anglo-Scandinavian Cardiac Outcome Trial),Citation63 as well as the low association between CCB medication and fewer revascularization procedures leading to a combined medico–economic rationale. Also, the JNC7, JNC8, ASH/ISH (>60 years of age), and ESH/ESC guidelines have CCBs included in their initial drug therapy ( and ).
Drugs that influence the renin angiotensin aldosterone system
Angiotensin-converting enzyme inhibitors
ACEIs block the conversion from angiotensin I to the vasoconstrictor AII, leading to a systematic decrease in blood-vessel tension and blood volume, without affecting heart rate via reflex stimulation. AII damages the endothelium by increasing oxidative stress while reducing nitric oxide bioavailability that provokes vascular remodeling, atherosclerosis, and arterial stiffening. Multiple clinical trials (ALLHAT,Citation86 STOP-2 [The Second Swedish Trial in Old Patients with Hypertension-2],Citation64 and HOPE [The Heart Outcomes Prevention Evaluation Study]Citation65) found that ACEIs lowered BP equally effectively compared to other drugsCitation66 and demonstrated lower morbidity and mortality in the elderly.Citation53 ACEIs seem to be most effective in patients with comorbidities, such as left ventricular hypertrophy, congestive heart failure and diabetes, to reduce cardiovascular death, stroke, and myocardial infarction,Citation67 although ACEIs appear to be inferior to CCBs with regard to stroke risk reduction;Citation68 centrally acting ACEIs that cross the blood–brain barrier may do so by inhibiting the brain’s ACE-driven degradation of amyloid-beta protein. In elderly diabetic patients, the use of ACEIs to preclude and slow the progression of renal disease and to prevent kidney failure still has to be proven in large-scale clinical trials. In a sub-study of HOPECitation69 involving diabetic patients (mean age 65 years), the primary endpoints (myocardial infarction, stroke, and cardiovascular death) and secondary endpoints (total mortality, heart failure, and TIA) were significantly lowered. Elsewise, evidence can only be extrapolated from middle-aged patients who have been treated with ARBs.Citation70 Notwithstanding the results of a recent meta-analysisCitation71 in elderly patients, the benefits of an ACEI or an ARB therapy (see the next section) should not be denied, but continuous monitoring of renal function and electrolytes (especially potassium) and avoidance of NSAIDs and potassium in the diet (eg, potassium-sparing diuretics, potassium supplements, and potassium-rich food) are recommended and will help to diminish the risks associated with this therapy.
Angiotensin-receptor blockers
ARBs block the activation of AII AT1 (Angiotensin-II-Receptor-Subtype-1) receptors. As ARBs trigger fewer side-effects, they are alternatives when adverse events of ACEIs are not tolerable. This applies specifically to ACEI-induced coughing. Improved or similar outcome with ARBs compared with other drugs has been demonstrated in several trials (LIFE [Losartan Intervention for Endpoint Reduction], VALUE [Valsartan Antihypertensive Long-Term-Use Evaluation]).Citation72,Citation73 ARBs are effective in reducing microalbuminuria levels and end-stage renal disease rates in patients with diabetic nephropathy. However, optimal BP thresholds and targets in elderly chronic kidney disease (CKD) patients still remain to be determined.Citation71 ARBs exhibit beneficial effects in elderly patients with stroke and heart failure (SCOPE [Study on COgnition and Prognosis in the Elderly], MOSES [Morbidity and Mortality after Stroke, Eprosartan Compared with Nitrendipine for Secondary Prevention], ACCESS [Acute Candesartan Cilexetil Therapy in Stroke Survivors], ValHeft [Valsartan Heart Failure Trial], and CHARM [Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity]).Citation74–Citation78 In CKD and heart-failure patients, the combination of ACEIs and ARBs should be avoided. Evidence has been provided that there is an increased risk of renal dysfunction and hyperkalemia, with limited additive efficacy.Citation79 In a recent meta-analysis, all-cause mortality reduction in hypertensive patients was driven primarily by ACEIs compared to ARBs.Citation80 Relevant side effects are displayed in .
Table 3 Most common drug-related side-effects of the main substance classes
ACEIs or ARBs are recommended only in patients younger than 55 years in the NICE guidelines.Citation24 All other guidelines (JNC7, JNC8 ESH/ESC, CHEP) do recommend ACEI and ARBs as first line therapy for nonblack patients.
Direct renin inhibitors
Aliskiren appears to be as effective as ARBs and ACEIs in lowering BP in the elderly.Citation81 In the AGELESS (aliskiren for geriatric lowering of systolic hypertension: a randomized controlled trial) trial,Citation82 the drug was found to be more effective and better tolerated than ramipril in patients with ISH. The major side-effect is mild diarrhea, which usually does not lead to discontinuation. In patients with type II diabetes or in patients with glomerular filtration rate (GFR) below 60 mL/minute/1.73m2, the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) do not recommend the combined use of aliskiren and blockers of the renin angiotensin aldosterone system (RAAS). This decision is based on results from the interrupted ALTITUDE (Aliskiren Trial In Type 2 Diabetes Using Cardio-Renal Endpoints) trial,Citation83 in which the incidence of primary endpoints (cardiovascular and renal events) was not improved, but more adverse events were observed in the combination arm (hyperkalemia). In the ASTRONAUT (The Aliskiren Trial on Acute Heart Failure Outcomes) trial,Citation83 the combination of aliskiren and an ARB also did not show an improvement in post-discharge mortality and heart failure readmissions, although significant decreases in N-terminal pro-brain natriuretic peptide (NT-proBNP) were observed. Patients on aliskiren on top of standard therapy displayed a significantly higher rate of hyperkalemia, worsening renal function, and hypotension. The final results of the ATMOSPHERE (the Aliskiren Trial of Minimizing OutcomeS for Patients with HEart failure) studyCitation84 (patients with chronic heart failure treated with the combination of aliskiren and enalapril) still need to be reported before final conclusions can be drawn, especially for the elderly population.Citation85 JNC8Citation19 guidelines do not recommend direct renin inhibitors as there have been no studies demonstrating their benefits on kidney or cardiovascular outcomes.
Other agents
Adrenergic blockers (eg, doxazosin) and centrally acting antihypertensive drugs (eg, clonidine, methyldopa, and reserpine) are not recommended for the treatment of hypertension in the elderly as their efficacy/adverse-effect profile is not beneficial.Citation53
Alpha-adrenergic blockers dilate the arterial wall by blocking the vasoconstrictive effects of alpha-adrenergic receptors. Although alpha-blockers are very effective in lowering BP, they often cause adverse events, such as postural hypotension, especially in patients receiving other vasodilators or diuretics. Since in the ALLHAT studyCitation86 the doxazosin arm demonstrated a 25% increase in cardiovascular endpoints and tripled the risk of congestive heart failure compared to chlorthalidone, alpha-blockers are no longer used in treatment combinations or just as third- or fourth-line agents, for example in isolated hypertension.
Summary of treatment per disease condition
The recent ESH/ESC guidelines suggest a condition–drug correlation.Citation87 As there is no evidence that different drugs should be used according to age and sex, the guideline allocations may also be applied to elderly patients ().
Table 4 Comparison of recommended substance classes in special situations in hypertension management
The comorbidity of dementia
Elderly patients have an increased risk of hypertension-induced dementia and cognitive dysfunction. High BP is also a predictor of stroke and vascular brain lesions.Citation88
Vascular dementia is a consequence of cognitive impairment caused by hypertensive angiopathy.Citation89 The underlying mechanism seems to be the elongation and tortation of blood vessels leading to an increase in BP in order to maintain blood flow; blood vessel wall thickness, and subsequent rigidity increase.Citation90 Subcortical white matter is damaged through blood flow impairment, hypoperfusions, and micro-ruptures of cerebral blood vessels.Citation91
However, to date there is no hard evidence regarding whether or not antihypertensive therapy has an impact on cognitive decline and dementia and if white-matter lesions can be prevented with antihypertensive therapy. This ambiguity is caused by several studies that revealed a curvilinear relationship between BP and cognitive function, in that low BP in late life is associated with a higher incidence of dementia.Citation92 Another finding comes from a recent French cohort study, which showed that BP variability and not mean BP was associated with an increased risk of incident dementia.Citation93 The MIND sub-study of the SPRINT trial (SPRINT Memory and cognition IN Decreased hypertension: SPRINT-MIND) may provide more insights on cognitive function by assessing the Mini Mental State results of elderly people with SBPs of 100 mmHg, 120 mmHg, and 180 mmHg.Citation94
Thus, to date it remains unclear whether benefits in the prevention of cognitive impairment are derived from lowering BP or from the choice of a particular drug class. The comprehensive PROGRESS (Perindopril Protection Against Recurrent Stroke Study) sub-studyCitation95 will hopefully address this issue by assessing the protective effects of perindopril and indapamide. Even though the underlying mechanisms are unknown, it is assumed that blockage of the cerebral ACE system and facilitating cholinergic activation can prevent cognitive decline.Citation96 Also, telmisartan is assumed to interplay with the hippocampal brain-derived neurotrophic factor/tropomyosin-related kinase B.Citation97 In the smaller Honululu-Asia Aging study, BBs seemed to be associated with a lower risk of developing cognitive impairment,Citation98 and a recent Spanish reviewCitation99 highlights the advantages of CCBs. Nitrendipine and lercanidipin in particular seem to have specific neuroprotective effects. The latter is responsible for substantial and long-acting vasodilation, and may therefore be indicated to reduce vascular dementia. In light of conflicting evidence, CCBs and ACEIs may be recommended for preventive use in elderly and very elderly patients with dementia ().
Changes in hypertension treatment through the aging process
Primarily, reduction of BP is more important than the agent used to reach that goal. Thus, the four basic drug classes, namely ACEIs, ARBs, CCBs, and diuretics, are all suitable as first-line therapy to treat arterial hypertension in both elderly (≥65 years) and very elderly patients (≥80 years). BBs should be administered cautiously, with the exception of prior myocardial infarction, heart failure, and arrhythmia. The choice of antihypertensive agent should be individually adjusted according to the tolerability of the corresponding drugs and underlying comorbidities. A successful antihypertensive treatment without side-effects should be principally maintained when patients become older, but modified according to the stage of aging in order to maintain the SBP goals of <140 mmHg in patients <80 years and 140–150 mmHg in patients ≥80 years, as recommended in the current ESH/ESC guidelines.Citation5 In a recent review on SBP targets for the elderly by Denker and CohenCitation100 and as elucidated by Paul James: ‘[…] if you gotten someone’s [systolic] BP to 140 or 135 mmHg on medicine and they are doing well then you need to take them off medicine and get their BP closer to 150 mmHg.’Citation15 Data suggest that the activity of the RAAS system, including plasma renin activity, is remarkably lower in the elderly.Citation101 Thus, drugs targeting the RAAS might become less effective and patients should be monitored more intensively.
Medical rationale for single-pill combinations in the elderly
Only 20% of patients ≥65 years show good adherence to medication.Citation102 As a result, treatment success is often impaired. Overall, utilization of multiple antihypertensive drugs in the elderly has been observed, with 38% of patients receiving three or more antihypertensive drugs.Citation103 A study found that non-vascular comorbidities are also negatively correlated with antihypertensive drug use in the elderly.Citation104 Approximately 50% of patients discontinue their treatment within only 1-year,Citation105 and a high percentage of drug-related admissions to hospitals are caused by non-adherence to medication.
An older but nicely designed systematic review on the association between dose and medication compliance indicated that compliance dropped from 79%±14% with one daily drug to 51%±20% with four daily drugs.Citation107 Decreasing the number of tablets can therefore improve adherence to treatment.Citation108 In addition, prescription of single-pill combinations (SPCs) appears to be useful in reducing side-effects and bringing more patients to goal.Citation109 Combined therapies can increase responder rates up to 70%Citation110 and reduce side-effects by neutralizing counter-regulatory mechanisms. In a survey conducted in Thuringia, 85.1% of physicians treated their hypertensive patients early on with combination therapy.Citation111 ESH/ESC guidelinesCitation5 recommend to start combination therapy with marked BP elevation and/or high/very high CV risk. JNC8 guidelinesCitation14 leave it to the physicians’ diligence, which of the 3 strategies described to adopt, and tailor the therapy according to the individual circumstances, clinician and patient preferences, and drug tolerability ().
A focus on compliance: looking beyond mode of application
Compliance problems are not caused exclusively by mode of application. The composition of prescribed drugs and patient sex also influence compliance behavior. Highest adherence has been found in patients taking CCBs and ARBs, while BBs and diuretics have been associated with low adherence.Citation112 A cohort study of 2,194 patients identified the most prominent factors of low adherence in the elderly to be high body mass index in men, dissatisfaction with communication of the health care provider, and depression in women.Citation113 Furthermore, consultation of multiple doctors has been shown to be associated with a lower likelihood of achieving target BP in patients aged >80 years.Citation114 A Swiss study indicated that older physicians in rural areas showed more hesitation concerning the use of SPCs in elderly patients.Citation10 It is likely that SPCs are perceived as impractical when medication adjustments need to be performed frequently. In addition, it must be mentioned that cortical dementia, for example, also increases the risk of non-adherence to medication. Thus, physicians may believe that in a twice-daily scheme the probability of taking at least one dosage/day is higher than with a SPC where the forgiveness factor is low. Based on the fact that approximately 18% of octogenarians show an impairment of cortical function or dementia, the prescription of SPCs must be evaluated carefully. Furthermore, it must not be forgotten that the initial use of a SPC can result in a substantial drop in BP.
Early detection of cardiovascular disease
Hypertension in the elderly is a very common biomarker to detect developing cardiovascular disease early and reliably. Changes in hypertension levels reflect subtle perturbations and provide the opportunity for prevention or regression at an early and potentially modifiable disease stage. Heart failure, arrhythmias, valvular heart disease, and CHD are highly prevalent among octogenarians. Because treatment variation is more restricted in the elderly due to limitations pertaining to homeostatic and adaptive capacity, aggravation of existing diseases should be prevented. The currently applied methodologies (eg, electrocardiography and echocardiography) do not have high detection sensitivity and cannot always be used in routine assessment (ie, they are costly and time-consuming). For example, the diagnosis of left ventricular hypertrophy (LVH) has been demonstrated to be predictive of major cardiovascular events, including stroke and all-cause mortality, independent of BP. Conversely, patients who achieve LVH regression during follow-up are much less likely to experience morbid events than those with persistence of LVH.Citation115 Also, NT-pro-BNP/BNP and cardiac troponins are related to structural and functional abnormalities that may progress to symptomatic heart disease, eg, LVH and LV systolic and diastolic dysfunction.Citation116 Results from high-sensitivity cardiac troponin (hs-cTn) assays were also strongly related to cardiac abnormalities, namely LV systolic dysfunction and increased LV mass and LV dimensions portending mortality and heart failure hospitalization. Shown in three different large population-based cohort studies strong and graded associations were seen linking hypertension, diabetes, and CKD with higher cTn levels.Citation116 Combining information derived from NT-pro-BNP/BNP and/or cTn may provide complementary utility to risk-stratify subjects to different categories beyond traditional risk factors.Citation117 Combined with clinical information (eg, LVH), biomarker testing may allow identification of patients with a malignant subphenotype of LVH with a high risk for progression to heart failure and CV deathCitation118 or may in combination with electrocardiography lead to a similar sensitivity as echocardiography with a tenth of the costs.Citation119 However, to date, studies have shown considerable heterogeneity due to different thresholds (cut-offs) used and varying prevalence of the abnormalities screened and concomitant cardiovascular diagnoses. Furthermore, the biomarker results may be confounded by several non-cardiac conditions, such as age, sex, renal function, and metabolic status. Results suggest that risk (heart failure, CVD death) associated with higher cTn levels can be dynamic. If therapies or lifestyle factors can be identified that can prevent further troponin increase, or, better yet, reduce troponin levels assessed in serial measurement, then heart failure risk may also be modifiable. There are currently no studies evaluating the effectiveness of a biomarker based treatment intervention on hard outcomes in either a general or an old population with subclinical but potentially modifiable cardiorenal organ damage stages.
Economic aspects of antihypertensive treatment in the elderly
Antihypertensive treatment has a huge economic impact on health systems. In general, two factors impact on treatment costs: 1) duration of treatment, and 2) mode of application. Data have shown that patients treated for longer than 10 years are more cost-intensive.Citation117 This may be due to resistance to change to alternative and cheaper combinations once treatment is successful. In Switzerland, fewer SPCs are prescribed in the very elderly than in younger patients,Citation10 which impacts therapy costs. Thus, daily therapy costs were found to be higher in patients aged 65–79 and >80 years than in patients aged >65 years.
In many markets, treatment costs are higher for ARBs than for ACEIs. However, it must be noted that despite nominally higher daily treatment costs, the antihypertensive effect and adverse side-effect profile for ARBs are more favorable than for older drugs, such as diuretics or BBs. Increased compliance with ARBs resulting in substantial cost savingsCitation118 may therefore justify higher daily treatment costs. Despite the findings of an Italian investigation reporting diuretics and BBs to be highly cost-effective, blood pressure control rates remained low with these drugs.Citation119 Data from another Swiss survey indicated an exceedingly high use of diuretics in primary careCitation120 as diuretics are often perceived to be the preferred approach for initial treatment of mild to moderate hypertension.Citation121 Considering the increased costs for potential new-onset diabetes of USD $549 per patient, the use of diuretics/BBs has been shown to be economically and medically unpropitious.Citation122 This finding can be backed with data from an analysis showing substantial savings in Great Britain and Sweden with respect to new-onset diabetes by using CCBs instead of BBs.Citation122
Conclusion
The increasing number of elderly (≥65 and <80 years) and very elderly (≥80 years) patients, plus restricted evidence from randomized controlled trials consolidated in different guidelines, means that antihypertensive treatment remains challenging in this patient population. It is therefore the physician’s responsibility to individualize treatment, taking important aspects such as the J-curve effect, age, comorbidities, and co-medication into consideration. The central questions remain: whom to treat with which drug class, when to initiate treatment, and what should be optimal goals in this population. Furthermore, other modifiable cardiovascular risk factors, such as diabetes mellitus and chronic kidney disease, also need to be integrated into the treatment strategy. The principle to start low and go slow will probably help primarily in patients with orthostatic hypotensive problems and kidney insufficiency. BP measurement should also be conducted in a standing position, and 24-hour ambulatory BP measurements are recommended. The newly started studies, SPRINT and ESH-CHL-SHOT, should help us to define optimum BP values for elderly patients more accurately. Future studies should also include 24-hour ambulatory BP measurement to gain more insight into an optimal treatment algorithm for the individual characteristics of a BP profile. Care should also be improved by accelerating adoption and implementation of standardized treatment approaches nationwide.Citation21,Citation23 Novel non-pharmacological interventions, namely renal sympathetic denervation and carotid baroreceptor stimulation, should also be assessed to provide further armamentarium in managing the ever-increasing number of hypertensive elderly patients.
Disclosure
Kaiser E and Schäfer H work for Roche Diagnostics and are former employees of Novartis Pharma Germany/Switzerland. The authors report no other conflicts of interest in this work.
References
- SimpsonFOLong-term cost and life-expectancy consequences of hypertensionJ Hypertens1998168109911009794710
- PimentaEOparilSManagement of hypertension in the elderlyNat Rev Cardiol20129528629622411292
- Statistisches BundesamtBevölkerung Deutschlands bis 2060 12 koordinierte Bevölkerungsvorausberechnung [German population up to 2060 12 Coordinated population projection]2009 Available from https://www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/Vorausberech-nungBevoelkerung/BevoelkerungDeutschland2060Presse5124204099004.pdf?__blob=publicationFileAccessed February 20, 2014
- AronowWSFlegJLPepineCJACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of HypertensionJ Am Soc Hypertens20115425935221771565
- ManciaGFagardRNarkiewiczKTask Force Members2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)J Hypertens20133171281135723817082
- GueyffierFBulpittCBoisselJPAntihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDANA GroupLancet1999353915579379610459960
- PetersRBeckettNPoulterRKidney function in the very elderly with hypertension: data from the hypertension in the very elderly (HYVET) trialAge Ageing201342225325822910302
- MutasingwaDRGeHUpshurREHow applicable are clinical practice guidelines to elderly patients with comorbidities?Can Fam Physician2011577e253e26221753084
- GhaliJKKadakiaSCooperRFerlinzJPrecipitating factors leading to decompensation of heart failure. Traits among urban blacksArch Intern Med19881489201320163046541
- SchäferHHSudanoITheusGRZillaPNollGBurnierMBlood pressure target attainment in the background of guidelines: the very elderly in Swiss primary careFam Pract201229551152022379186
- BorzeckiAMOliveriaSABerlowitzDRBarriers to hypertension controlAm Heart J2005149578579415894958
- HajjarIMillerKHirthVAge-related bias in the management of hypertension: a national survey of physicians’ opinions on hypertension in elderly adultsJ Gerontol A Biol Sci Med Sci2002578M487M49112145360
- Rodriguez-RocaGCLlisterriJLPrieto-DiazMABlood pressure control and management of very elderly patients with hypertension in primary care settings in SpainHypertens Res201437216617124089262
- JamesPAOparilSCarterBL2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (JNC 8)JAMA2014311550752024352797
- WoodSJNC 8 at Last! Guidelines Ease Up on BP Thresholds, Drug ChoicesHeartwire2013 http://www.medscape.com/viewarticle/817991Accessed February 17, 2014
- SoxHCAssessing the trustworthiness of the guideline for management of high blood pressure in adultsJAMA2014311547247424352688
- BauchnerHFontanarosaPBGolubRMUpdated guidelines for management of high blood pressure: recommendations, review, and responsibilityJAMA2014311547747824352759
- PetersonEDGazianoJGreenlandPRecommendations for treating hypertension: What are the right goals and purposes?JAMA2013
- WeberMASchiffrinELWhiteWBClinical Practice Guidelines for the Management of Hypertension in the CommunityThe Journal of Clinical Hypertension2014161142624341872
- WoodSHypertension Guidelines: But Wait, There’s MoreHeartwire2014 http://www.medscape.com/viewarticle/818652Accessed February 17, 2014
- GoASBaumanMKingSMCAn Effective Approach to High Blood Pressure Control: A Science Advisory From the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and PreventionHypertension Epub11152013
- O’RiordanMAHA/ACC/CDC Issue ‘Science Advisory’ on Treating BPHeartwire2013 http://content.onlinejacc.org/article.aspx?articleid=1778408Accessed February 17, 2014
- FriedenTRKingSWrightJSProtocol-based treatment of hypertension: A critical step on the pathway to progressJAMA20143111212224231925
- National Institute for Health and Clinical ExcellenceNICE clinical guideline 127. Hypertension: clinical management of primary hypertension in adultsLondonNational Institute for Health and Clinical Excellence2011 Available from: http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdfAccessed February 13, 2014
- ChobanianAVBakrisGLBlackHRNational Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJAMA2003289192560257212748199
- HouleSKPadwalRTsuyukiRTThe 2012–2013 Canadian Hypertension Education Program (CHEP) guidelines for pharmacists: An updateCan Pharm J (Ott)2013146314615023795198
- KjeldsenSEJuliusSHypertension mega-trials with cardiovascular end points: effect of angiotensin-converting enzyme inhibitors and angiotensin receptor blockersAm Heart J2004148574775415523303
- BriasoulisAAgarwalVTousoulisDStefanadisCEffects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studiesHeart2014100431732323813846
- BanachMAronowWSHypertension therapy in the older adults-do we know the answers to all the questions? The status after publication of the ACCF/AHA 2011 expert consensus document on hypertension in the elderlyJ Hum Hypertens2012261164164322513754
- BeckettNSPetersRFletcherAEHYVET Study GroupTreatment of hypertension in patients 80 years of age or olderN Engl J Med2008358181887189818378519
- Bejan-AngoulvantTSaadatian-ElahiMWrightJMTreatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trialsJ Hypertens20102871366137220574244
- ReboldiGGentileGAngeliFVerdecchiaPBlood pressure lowering in the oldest oldJ Hypertens20102871373137620574245
- BanachMAronowWSBlood pressure j-curve: current conceptsCurr Hypertens Rep201214655656623054894
- PanjrathGSChaudhariSMesserliFHThe j-point phenomenon in aggressive therapy of hypertension: new insightsCurr Atheroscler Rep201214212412922396196
- ChrysantSGCurrent status of aggressive blood pressure controlWorld J Cardiol201133657121499494
- PepineCJHandbergEMCooper-DeHoffRMINVEST InvestigatorsA calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trialJAMA2003290212805281614657064
- DenardoSJGongYNicholsWWBlood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudyAm J Med2010123871972620670726
- OgiharaTMatsuokaHRakugiHPractitioner’s trial on the efficacy of antihypertensive treatment in elderly patients with hypertension II (PATE-hypertension II study) in JapanGeriatr Gerontol Int201111441442121410854
- HanssonLZanchettiACarruthersSGEffects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study GroupLancet19983519118175517629635947
- Wake Forest Baptist HospitalSystolic Blood Pressure Intervention Trial (SPRINT) Available form: http://clinicaltrials.gov/ct2/show/NCT1206062 NLM identifier: NCT1206062Accessed November 2, 2013
- Istituto Auxologico ItalianoEuropean Society of Hypertension and Chinese Hypertension League Stroke in Hypertension Optimal Treatment Trial (ESH-CHL-SHOT) Available from: http://clinicaltrials.gov/ct2/show/NCT1563731. NLM identifier: NCT1563731Accessed November 2, 2013
- O’BrienEParatiGStergiouGEuropean Society of Hypertension Working Group on Blood Pressure MonitoringEuropean society of hypertension position paper on ambulatory blood pressure monitoringJ Hypertens20133191731176824029863
- SatoIAkazawaMPolypharmacy and adverse drug reactions in Japanese elderly taking antihypertensives: a retrospective database studyDrug Healthc Patient Saf2013514315023843704
- LawMRMorrisJKWaldNJUse of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studiesBMJ2009338b166519454737
- OpiyoNShepperdSMusilaNEnglishMFretheimAThe “Child Health Evidence Week” and GRADE grid may aid transparency in the deliberative process of guideline developmentJ Clin Epidemiol201265996296922742914
- TurnbullFNealBNinomiyaTBlood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trialsBMJ200833676531121112318480116
- KjeldsenSEWeberMOparilSJamersonKACombining RAAS and calcium channel blockade: ACCOMPLISH in perspectiveBlood Press2008175–626026919061055
- DuarteJDCooper-DeHoffRMMechanisms for blood pressure lowering and metabolic effects of thiazide and thiazide-like diureticsExpert Rev Cardiovasc Ther20108679380220528637
- DhallaIAGomesTYaoZChlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort studyAnn Intern Med2013158644745523552325
- WehlingMMorbus diureticus in the elderly: epidemic overuse of a widely applied group of drugsJ Am Med Dir Assoc201314643744223510827
- De CaterinaARLeoneAMWhy beta-blockers should not be used as first choice in uncomplicated hypertensionAm J Cardiol2010105101433143820451690
- MesserliFHGrossmanEGoldbourtUAre beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic reviewJAMA199827923190319079634263
- FlegJLAronowWSFrishmanWHCardiovascular drug therapy in the elderly: benefits and challengesNat Rev Cardiol201181132820978470
- WiysongeCSBradleyHAVolminkJMayosiBMMbewuAOpieLHBeta-blockers for hypertension [review]Cochrane Database Syst Rev201211CD00200323152211
- BangaloreSSawhneySMesserliFHRelation of beta-blocker-induced heart rate lowering and cardioprotection in hypertensionJ Am Coll Cardiol200852181482148919017516
- CostanzoPPerrone-FilardiPPetrettaMCalcium channel blockers and cardiovascular outcomes: a meta-analysis of 175,634 patientsJ Hypertens20092761136115119451836
- CocaAHypertension and vascular dementia in the elderly: the potential role of anti-hypertensive agentsCurr Med Res Opin20132991045105423745517
- WangJGStaessenJALiYCarotid intima-media thickness and antihypertensive treatment: a meta-analysis of randomized controlled trialsStroke20063771933194016763185
- WilliamsBLacyPSThomSMCAFE InvestigatorsAnglo-Scandinavian Cardiac Outcomes Trial InvestigatorsCAFE Steering Committee and Writing CommitteeDifferential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) studyCirculation200611391213122516476843
- JamersonKWeberMABakrisGLACCOMPLISH Trial InvestigatorsBenazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patientsN Engl J Med2008359232417242819052124
- ChenGJYangMSThe effects of calcium channel blockers in the prevention of stroke in adults with hypertension: a meta-analysis of data from 273,543 participants in 31 randomized controlled trialsPLoS One201383e5785423483932
- COLM Study Research OrganizationCombination of OLMesartan and CCB or Low Dose Diuretics in High Risk Elderly Hypertensive Patients Study (COLM-Study) Available from: http://clinicaltrials.gov/show/NCT0454662. NLM identifier: NCT0454662Accessed November 2, 2013
- MeurinPThe ASCOT trial: clarifying the role of ACE inhibition in the reduction of cardiovascular events in patients with hypertensionAm J Cardiovasc Drugs20066532733417083267
- HanssonLLindholmLHEkbomTRandomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 studyLancet199935491921751175610577635
- YusufSSleightPPogueJBoschJDaviesRDagenaisGEffects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study InvestigatorsN Engl J Med2000342314515310639539
- GoschMThe role of ACE inhibitors in the treatment of hypertensive elderly patientsZ Gerontol Geriatr200033643343711201013
- FretheimAOdgaard-JensenJBrørsOComparative effectiveness of antihypertensive medication for primary prevention of cardiovascular disease: systematic review and multiple treatments meta-analysisBMC Med2012103322480336
- FretheimAWitterSLindahlAKOlsenITPerformance-based financing in low- and middle-income countries: still more questions than answersBull World Health Organ2012908559559A22893735
- PappoeLSWinkelmayerWCACE inhibitor and angiotensin II type 1 receptor antagonist therapies in elderly patients with diabetes mellitus: are they underutilized?Drugs Aging2010272879420104936
- Levi MarpillatNMacquin-MavierITropeanoAIBachoud-LeviACMaisonPAntihypertensive classes, cognitive decline and incidence of dementia: a network meta-analysisJ Hypertens20133161073108223552124
- WeirMRRolfeMPotassium homeostasis and renin-angiotensin-aldosterone system inhibitorsClin J Am Soc Nephrol20105353154820150448
- DahlöfBDevereuxRde FaireUThe Losartan Intervention For Endpoint reduction (LIFE) in Hypertension study: rationale, design, and methods. The LIFE Study GroupAm J Hypertens1997107 Pt 17057139234823
- MannJJuliusSThe Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial of cardiovascular events in hypertension. Rationale and designBlood Press1998731761839758088
- LithellHHanssonLSkoogISCOPE Study GroupThe Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trialJ Hypertens200321587588612714861
- BoulangerJMHillMDMorbidity and mortality after stroke--eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES)Stroke2006372335356 author reply 33816397169
- CareyRMLoganAGAcute candesartan cilexetil therapy in stroke survivorsCurr Hypertens Rep20046211411615010014
- CohnJNTognoniGValsartan Heart Failure Trial InvestigatorsA randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failureN Engl J Med2001345231667167511759645
- SwedbergKPfefferMGrangerCCandesartan in heart failure--assessment of reduction in mortality and morbidity (CHARM): rationale and design. Charm-Programme InvestigatorsJ Card Fail19995327628210496201
- MakaniHBangaloreSDesouzaKAShahAMesserliFHEfficacy and safety of dual blockade of the renin-angiotensin system: meta-analysis of randomised trialsBMJ2013346f36023358488
- van VarkLCBertrandMAkkerhuisKMAngiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patientsEur Heart J201233162088209722511654
- VerdecchiaPCalvoCMöckelVKeelingLSatlinASafety and efficacy of the oral direct renin inhibitor aliskiren in elderly patients with hypertensionBlood Press200716638139118058456
- DuprezDAMungerMABothaJKeefeDLCharneyANAliskiren for geriatric lowering of systolic hypertension: a randomized controlled trialJ Hum Hypertens201024960060820033075
- FriedrichSSchmiederREReview of direct renin inhibition by aliskirenJ Renin Angiotensin Aldosterone Syst201314319319623873285
- McMurrayJJAbrahamWTDicksteinKKøberLMassieBMKrumHAliskiren, ALTITUDE, and the implications for ATMOSPHEREEur J Heart Fail201214434134322431404
- KrumHMassieBAbrahamWTATMOSPHERE InvestigatorsDirect renin inhibition in addition to or as an alternative to angiotensin converting enzyme inhibition in patients with chronic systolic heart failure: rationale and design of the Aliskiren Trial to Minimize OutcomeS in Patients with HEart failuRE (ATMOSPHERE) studyEur J Heart Fail201113110711421169387
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research GroupThe Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)JAMA2002288232981299712479763
- ManciaGFagardRNarkiewiczKTask Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)J Hypertens20133171281135723817082
- VermeerSELongstrethWTKoudstaalPJSilent brain infarcts: a systematic reviewLancet Neurol20076761161917582361
- NinomiyaTOharaTHirakawaYMidlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama studyHypertension2011581222821555680
- FletcherAEBulpittCJHow far should blood pressure be lowered?N Engl J Med199232642512541727978
- RománGCTatemichiTKErkinjunttiTVascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International WorkshopNeurology19934322502608094895
- ChaudhryKNChavezPGasowskiJGrodzickiTMesserliFHHypertension in the elderly: some practical considerationsCleve Clin J Med2012791069470423027728
- AlpérovitchABlachierMSoumaréABlood pressure variability and risk of dementia in an elderly cohort, the Three-City StudyAlzheimers Dement Epub2013814
- MorrisMCScherrPAHebertLEAssociation between blood pressure and cognitive function in a biracial community population of older personsNeuroepidemiology200221312313012006775
- RatnasabapathyYLawesCMAndersonCSThe Perindopril Protection Against Recurrent Stroke Study (PROGRESS): clinical implications for older patients with cerebrovascular diseaseDrugs Aging200320424125112641480
- YamadaKHoritaTTakayamaMEffect of a centrally active angiotensin converting enzyme inhibitor, perindopril, on cognitive performance in chronic cerebral hypo-perfusion ratsBrain Res2011142111012021981801
- KishiTHirookaYSunagawaKTelmisartan reduces mortality and left ventricular hypertrophy with sympathoinhibition in rats with hypertension and heart failureAm J Hypertens201427226026724096926
- GelberRPRossGWPetrovitchHMasakiKHLaunerLJWhiteLRAntihypertensive medication use and risk of cognitive impairment: the Honolulu-Asia Aging StudyNeurology2013811088889523911753
- WatfaGRossignolPKearney-SchwartzAUse of calcium channel blockers is associated with better cognitive performance in older hypertensive patients with subjective memory complaintsJ Hypertens201028122485249320739903
- DenkerMGCohenDLWhat is an appropriate blood pressure goal for the elderly: review of recent studies and practical recommendationsClin Interv Aging201381505151724255596
- BauerJHAge-related changes in the renin-aldosterone system. Physiological effects and clinical implicationsDrugs Aging1993332382458324299
- MonaneMBohnRLGurwitzJHGlynnRJLevinRAvornJCompliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and raceAm J Public Health19968612180518089003143
- ThoenesMSpirkDBöhmMMahfoudFThevathasanLBramlagePTreatment of hypertension in the elderly: data from an international cohort of hypertensives treated by cardiologistsJ Hum Hypertens201327213113722258208
- WangPSAvornJBrookhartMAEffects of noncardiovascular comorbidities on antihypertensive use in elderly hypertensivesHypertension200546227327915983239
- ChrostowskaMNarkiewiczKImproving patient compliance with hypertension treatment: mission possible?Curr Vasc Pharmacol20108680480720626345
- LaFleurJOderdaGMMethods to measure patient compliance with medication regimensJ Pain Palliat Care Pharmacother2004183818715364635
- ClaxtonAJCramerJPierceCA systematic review of the associations between dose regimens and medication complianceClin Ther20012381296131011558866
- SherrillBHalpernMKhanSZhangJPanjabiSSingle-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherenceJ Clin Hypertens (Greenwich)2011131289890922142349
- HillemanDERyschonKLMohiuddinSMWurdemanRLFixed-dose combination vs monotherapy in hypertension: a meta-analysis evaluationJ Hum Hypertens199913747748310449213
- MesserliFHOparilSFengZComparison of efficacy and side effects of combination therapy of angiotensin-converting enzyme inhibitor (benazepril) with calcium antagonist (either nifedipine or amlodipine) versus high-dose calcium antagonist monotherapy for systemic hypertensionAm J Cardiol200086111182118711090788
- HermannRRauMMarxCWolfGArterial hypertension: guideline acceptance and implementation in workaday life of internists and general practitioners in ThuringiaDtsch Med Wochenschr201313825–2613471352 German23761056
- RizzoJASimonsWRVariations in compliance among hypertensive patients by drug class: implications for health care costsClin Ther199719614461457 discussion 1424–14259444452
- HoltEJoyceCDornellesASex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adultsJ Am Geriatr Soc201361455856423528003
- ChowdhuryEKOwenAKrumHSecond Australian National Blood Pressure Study Management Committee. Barriers to achieving blood pressure treatment targets in elderly hypertensive individualsJ Hum Hypertens201327954555123448846
- VolpeMBattistoniATocciGCardiovascular risk assessment beyond Systemic Coronary Risk Estimation: a role for organ damage markersJ Hypertens20123061056106422573072
- EggersKMVengePUtility of B-type natriuretic peptides and cardiac troponins for population screening regarding cardiac abnormalitiesPathology201244212913822198250
- SchäferHHScheunertUCosts of current antihypertensive therapy in Switzerland: an economic evaluation of 3,489 patients in primary careSwiss Med Wkly2013143w1385424163048
- BramlagePHasfordJBlood pressure reduction, persistence and costs in the evaluation of antihypertensive drug treatment – a reviewCardiovasc Diabetol200981819327149
- AmbrosioniEPharmacoeconomic challenges in disease management of hypertensionJ Hypertens Suppl2001193S33S4011713849
- SchäferHHde VilliersJDSudanoIManagement of hypertension in patients with diabetes mellitus and metabolic syndrome in Swiss primary careInt J Clin Pract201266111125112623067037
- RochefortCMMorlecJTamblynRMWhat differentiates primary care physicians who predominantly prescribe diuretics for treating mild to moderate hypertension from those who do not? A comparative qualitative studyBMC Fam Pract201213922375684
- GrimmCKöberleinJWiosnaWKresimonJKienckePRychlikRNew-onset diabetes and antihypertensive treatmentGMS Health Technol Assess20106 Doc03