Abstract
Purpose
Rural older adults are more likely to be malnourished than urban older adults, particularly those living in lower-middle-income countries like Vietnam. Therefore, this study aimed to address the prevalence of malnutrition and its association with frailty and health-related quality of life in older rural Vietnamese adults.
Participants and Methods
This cross-sectional study was conducted on community-dwelling older adults (aged ≥ 60 years) living in a rural province in Vietnam. Nutritional status was determined using the Mini Nutritional Assessment Short Form (MNA-SF), and frailty was evaluated using the FRAIL scale. The 36-Item Short Form Survey (SF-36) was used to evaluate health-related quality of life.
Results
Among the 627 participants, 46 (7.3%) were malnourished (MNA-SF score <8), and 315 (50.2%) were at risk of malnutrition (MNA-SF score: 8–11). Individuals with malnutrition had significantly higher rates of impairments in instrumental activities of daily living and activities of daily living than those without malnutrition (47.8% vs 27.4% and 26.1% vs 8.7%, respectively). The prevalence of frailty was 13.5%. Risk of malnutrition and malnutrition were associated with high risks of frailty, with odds ratios of 2.14 (95% confidence interval [CI]: 1.16–3.93) and 4.78 (1.86−12.32), respectively. Furthermore, the MNA-SF score was positively correlated with eight domains of the health-related quality of life among rural older adults.
Conclusion
The prevalence rates of malnutrition, risk of malnutrition, and frailty were high among older adults in Vietnam. A strong association was observed between nutritional status and frailty. Therefore, this study reinforces the importance of screening for malnutrition and risk of malnutrition among older rural individuals. Further studies should explore whether early nutritional intervention reduces the risk of frailty among older adults and increase their health-related quality of life in the Vietnamese population.
Introduction
Nutrition is critical in maintaining health and quality of life among older adults, who are vulnerable to malnutrition due to several contributing factors, including chronic diseases, loss of teeth, and decreasing appetite.Citation1,Citation2 Hence, malnutrition remains a serious public health concern among older adults, particularly those in lower-middle-income countries like Vietnam.Citation3 According to data published by the World Health Organization, the prevalence of malnutrition in older people ranges from 1.3% to 47.8%, and it is much higher in low- and middle-income countries than in high-income countries.Citation4 An Indian study reported that 17.9% of older people had malnutrition and approximately 60% were at risk of malnutrition.Citation5 Another study in MalaysiaCitation6 found that the prevalence rates of malnutrition and risk of malnutrition in older adults were 7.3% and 23.4%, respectively.
Factors contributing to malnutrition in older adults include age-related anorexia, chronic diseases, multimorbidity, polypharmacy, and frailty.Citation7 Another significant aspect of malnutrition in older adults is its adverse consequences, including sarcopenia, frailty, and falls.Citation8 Approximately 70% of malnourished older individuals have frailty.Citation9 Malnutrition and frailty are interrelated. Long-term malnutrition including insufficient protein and energy intake can result in weight loss, exhaustion, slow walking speed, and low physical activity which are components of the frailty phenotype.Citation10,Citation11 Malnutrition plays an important mechanism in frailty pathogenesis and is a target of frailty treatment.Citation12,Citation13 Further, frailty is a major indicator of malnutrition.Citation7 Functional impairment in frail older adults such as impairments in carrying out activities such as shopping, travel, and meal preparation may lead to social isolation, food apathy, and decreased food intake.Citation7,Citation10 Furthermore, malnutrition and frailty have several common pathophysiological pathways such as weight loss, chronic diseases, cognitive and physical risk factors.Citation9 Malnutrition also increases the risks of infection, hospital admission, and mortality.Citation14 In particular, older people with malnutrition have a lower quality of life than those without malnutrition.Citation15
Vietnam is a rapidly aging country facing challenges in maintaining the well-being of older people at risk of multimorbidity, polypharmacy, frailty, functional impairment, and mental health problems.Citation16 Moreover, approximately 75% of the older Vietnamese population resides in rural areas, where they may have a high risk of malnutrition.Citation17 A previous hospital-based studyCitation18 reported that 71.6% of older inpatients were malnourished or at risk of being malnourished, whereas another study found that the prevalence of malnourishment among outpatients with diabetes was 31%.Citation19 However, to our knowledge, there are no previous studies elucidating the nutritional status of community-dwelling older people in rural areas; the problem of malnutrition in this population is often overlooked. This study aimed to address the prevalence of malnutrition and its association with frailty and health-related quality of life among older adults living in a rural province in Vietnam. The findings can inform preventive and interventional strategies for older individuals with malnutrition or at risk of malnutrition, preventing frailty, and improving their quality of life.
Materials and Methods
Study Design and Participants
We conducted a cross-sectional study in Tra Vinh province, including seven districts and 106 sub-districts with a high proportion of the Khmer people (a minority ethnic group in Vietnam) in Southern Vietnam.Citation20 Tra Vinh is a coastal province in the Mekong Delta with an economy based on agriculture and aquaculture.Citation20 According to the population statistics in 2019, the total population of Tra Vinh was around one million. People aged ≥ 60 years accounted for 12.3% of the total population, 68.2% were people aged 20–59 years, and the remainder were aged < 20 years (30.3%).Citation20 In particular, approximately 90% of Tra Vinh’s population resides in rural areas and most older adults live in the community, where there is no care service or nursing home.Citation20,Citation21
The study was approved by the Institutional Review Board of the University of Medicine and Pharmacy at Ho Chi Minh City (Approval number: 26/HĐĐĐ-ĐHYD), complying with the Declarations of Helsinki.
We used Open Epi version 3.01 to calculate the sample size, with a prevalence of malnutrition in older people of 27%, as specified in a previous study.Citation22 We applied an absolute precision of 5% and a confidence interval of 95%. The primary sample size was 310. Thereafter, a cluster sampling scheme was used; thus, we regarded the effect of intra-cluster correlation (the correlation within the clusters).Citation23 This is called the design effect, a factor used to adjust the required sample size.Citation24 Therefore, the primary sample size was multiplied by two (the design effect) to get the sample size of 620 participants.Citation23 Probability proportional to size sampling with 30 clusters was applied, with 21 individuals in each cluster, and one cluster being equivalent to one sub-district.
The inclusion criteria were as follows: age ≥ 60 years, residence in the community in Tra Vinh province for ≥ 1 year, existence of medical records with a primary care practice, ability to communicate, and the capacity to provide consent for participation in the study. We excluded participants with severe auditory impairment or severe dementia (based on medical records and confirmation by an internal medicine doctor). We did not assess cognition as routine.
Data Collection
The study protocol was explained to eligible participants. Written informed consent was obtained from those who were willing to participate in the study. Trained investigators conducted face-to-face interviews with the participants. Data were collected during a period of 10 months, from December 1st, 2021, to September 30th, 2022. Public health doctors evaluated the eligible participants.
Malnutrition Measurement
We used the Mini-Nutritional Assessment Short Form (MNA-SF), a widely used and validated tool, for evaluating nutrition (www.mna-elderly.com).Citation25–27 It includes six items: food intake, weight loss over the past 3 months, mobility, psychological stress or acute disease in the past 3 months, neuropsychological problems; and body mass index or calf circumference,Citation25 with a total score ranging from 0 to 14 points. A total score of 0–7 is classified as malnutrition, 8–11 as at risk of malnutrition, and 12–14 as no malnutrition.Citation25,Citation28
Frailty Measurement
Frailty was evaluated using the FRAIL scale,Citation29 including five components: (1) fatigue (tiredness during the previous 4 weeks), (2) resistance (difficulty in walking up 10 steps), (3) ambulation (difficulty in walking 300 m unaided), (4) illness (having ≥ 5 illnesses) and (5) loss of weight (≥ 5% of weight within 12 months), with the total score of 5. A score ≥ 3 indicates frailty, 1–2 indicates pre-frailty, and 0 indicates robustness. This scale was translated and validated in Vietnamese and has been reported elsewhere.Citation30
Health-Related Quality of Life Measurement
Health-related quality of life was evaluated using the Short-Form 36 questionnaire (SF-36), which includes 36 items covering eight health domains.Citation31 Physical functioning (10 items), social functioning (two items), role limitations due to physical problems (four items), role limitations due to emotional problems (three items), mental health (five items), energy and vitality (four items), bodily pain (two items), and general perception of health (five items). The total score ranges from 0 to 100, and a higher score indicates a more favorable health status.Citation31 This questionnaire was translated into Vietnamese and validated in a previous study.Citation32
Other Covariates
Data on other variables were also collected, including demographic information (age, sex, educational level, weight, height, body mass index, and perceived income status), functional status (instrumental activities of daily living and activities of daily living), and chronic diseases. Data on chronic diseases were collected from primary care medical records. Musculoskeletal diseases included osteoarthritis, osteoporosis, and gout. Chronic pulmonary diseases included asthma, chronic obstructive pulmonary disease, or bronchiectasis.
Instrumental activities of daily living (IADL) were evaluated using the Lawton-Brody scale, which includes eight activities: the ability to use the telephone, ability to go shopping, ability to prepare food, ability to engage in housekeeping, ability to do the laundry, mode of transportation, responsibility for own medications, and ability to handle finances,Citation33 with a total score ranging from 0 to 8, and a higher score indicating a higher level of independence.Citation33 Scores below 8 indicated IADL impairment.Citation33 Activities of daily living (ADL) were evaluated using the Katz Index, including six activities: dressing, bathing, toileting, transferring, feeding, and incontinence.Citation34 Similarly, the total ADL score ranges from 0 to 6, with a higher score indicating a higher level of independence. ADL impairment was defined as a total score of < 6.Citation34
Data Analysis
Categorical variables were expressed as the number of participants (percentage), and quantitative variables were expressed as mean ± standard deviation (SD). We used chi-squared or Fisher’s exact tests to compare categorical variables and one-way analysis of variance or t-test to compare continuous variables with normal distribution. The correlation between the SF-36, including eight scales and two summary measures, and the MNA-SF was determined using Pearson’s coefficient.
The association between nutritional status and frailty, adjusting for age, sex, ADL, and IADL, was examined by the multinomial logistic regression analysis and expressed as odds ratio (OR) and confidence interval (CI). All statistical analyses were performed using the Stata version 14.0 software (STATA Corp, College Station, Texas). Statistical significance was set at p <0.05.
Results
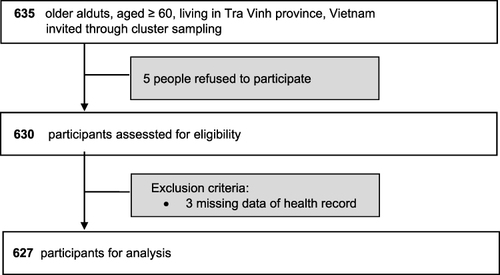
We approached 635 eligible older adults for participation in the study; however, five of them refused to participate and three were excluded due to missing data (). Finally, the study included 627 participants with a mean age of 69 ± 7 years; and 63.6% were female. Kinh and Khmer were the two most popular ethnicities (67.4% and 31.9%, respectively). Buddhism was the most popular religion (64.8%). In particular, most of the participants had low educational attainment (preschool and primary school-educated participants accounted for 78.4%), and one-fourth were former farmers (25.4%). Most of the older adults (89.5%) lived with their family members.
Prevalence of Malnutrition
The prevalence of malnutrition was 7.3% (n = 46); however, 50.2% of the study participants (n = 315) were at risk of malnutrition. In particular, the number of malnourished individuals increased with age, with more than 30% (30.4%) aged ≥ 80 years. As shown in , participants with malnutrition had a lower mean body mass index than those without malnutrition (18.9 ± 3.0 vs 25.6 ± 2.7, p <0.001). In particular, ADL and IADL impairment rates in the malnourished group were significantly higher than those in the non-malnourished group (26.1% vs 8.7% and 47.8% vs 27.4%, respectively).
Table 1 Characteristics of Rural Older Adults in Vietnam Classified by Nutritional Status (N = 627)
Association of Malnutrition and Frailty
shows the relationship between nutritional status according to the MNA-SF and frailty status. Based on the FRAIL scale, 13.6% (n = 85) of participants were classified as frail, 53.4% (n = 335) as pre-frail, and 33% (n = 207) as non-frail. The frail group’s malnutrition rate was twice as high as that of the non-frail group (17% vs 6.3%, p <0.001). Moreover, the proportions of participants whose food intake had declined over the past 3 months and who experienced involuntary weight loss were also significantly greater in the frail group than in the non-frail group (45.9% vs 24.7% and 36.5% vs 20.8%, respectively). In particular, 20 participants who met the criteria of weight loss belonged to both the groups of malnutrition (20/46, 43.5%) and frailty (20/85, 23.5%). The results also showed that the rate of psychological stress or acute disease in the past 3 months was three times higher in frail individuals than in non-frail individuals (52.9% vs 17.9%, p <0.001).
Table 2 MNA-SF Item Results Classified by Frailty Status Among Rural Older People in Vietnam (N = 627)® Société des Produits Nestlé SA, Trademark Owners.
In the multinomial logistic regression model assessing the association between nutritional status and frailty, malnutrition, and risk of malnutrition status were independently associated with frailty (). Individuals at risk of malnutrition had a 2.14 higher odds of frailty (OR = 2.14, 95% CI: 1.16–3.93), which increased to 4.78 (OR = 4.78, 95% CI: 1.86–12.32) in those with malnutrition after adjusting for age, sex, ADL, and IADL. In particular, those with psychological stress or acute disease in the past 3 months had a significantly higher odds ratio of frailty (OR = 5.45, 95% CI: 3.05–9.72) than their counterparts.
Table 3 Multinomial Logistic Regression Analysis of the Nutritional Status and MNA-SF Items Associated with Pre-Frailty/Frailty Among Rural Older Adults in Vietnam (N=627)
Association of Nutritional Status and Health-Related Quality of Life
presents the correlation between the MNA-SF and SF-36 scores. Eight domains of the health-related quality of life were positively correlated with the MNA-SF score; two domains, including physical functioning and general health, had a slightly higher correlation with the MNA-SF score than the other domains.
Table 4 Correlation Between MNA-SF Score and Health-Related Quality of Life Measured by SF-36 Among Rural Older Adults in Vietnam (N = 627)
Discussion
Prevalence of Malnutrition
This study aimed to determine the prevalence of malnutrition and its association with frailty and health-related quality of life among older rural adults in Vietnam. Although 7.3% of rural older adults were malnourished, approximately half (50.2%) were at risk of malnutrition. In particular, the prevalence of malnutrition increased with age, with approximately 30% of individuals aged ≥ 80 years experiencing malnutrition. These results indicate that poor nutrition is an alarming issue for older rural Vietnamese adults. Further, the prevalence of malnutrition in our study was similar to that in a Malaysian studyCitation6 (7.3% vs 7.5%). However, the prevalence of risk of malnutrition was significantly higher in our study than in the Malaysian study (50.5% vs 23.5%). The prevalence of malnutrition in our study was seven times higher than that reported in a Korean study (7.3% vs 0.8%), whereas the prevalence of risk of malnutrition was nearly four times higher (50.2% vs 13.5%).Citation36 The differences in the prevalence rates may be due to the differences in the socioeconomic status among the countries. First, Vietnamese people, particularly those living in rural areas, have lower incomes than Malaysians and Koreans.Citation37 Meanwhile, income level has been proven to be a strong determinant of nutritional status in older adults. Participants with low income are more likely to be malnourished or at risk of malnutrition.Citation38 Indeed, in our study, approximately 25% of malnourished individuals perceived their financial status as “poverty” or “pro-poverty”. Second, the majority of participants in our study (78.9%) had low educational attainment (preschool/primary school), which was much higher than that in the Korean study (50.9%). Previous studies revealed that older adults with low educational attainment tended to have worse nutritional status due to insufficient knowledge of healthy food selection and a lack of cooking skills.Citation39,Citation40 Furthermore, our study participants lived in a rural community, which is also a determinant of malnutrition or risk of malnutrition status. Several reports have shown that the prevalence of malnutrition in rural communities is approximately double that in urban communities because rural older adults have less access to healthcare services, family support, and diverse food options.Citation41,Citation42 Therefore, our results indicate the need for screening and early interventions for malnutrition and the risk of malnutrition among rural older Vietnamese adults.
Association of Malnutrition and Frailty
Consistent with previous studies, our study confirms that nutrition is significantly associated with frailty.Citation10,Citation36 We found that older adults with malnutrition and risk of malnutrition had 4.78 and 2.14 higher odds of frailty, respectively, than those without malnutrition. Similarly, previous studies in Korea and China reported that older individuals with poor nutritional status had 3.3 and 3.38 higher odds of frailty, respectively, than those with good nutritional status.Citation10,Citation36 This result may be explained by the fact that long-term malnutrition may result in fatigue, weight loss, and reduced activity which are components of frailty.Citation29 One interesting finding in our study is that older adults with psychological stress or acute disease in the past 3 months had 5.45 higher odds of frailty than those without psychological stress and acute disease. These two conditions directly impact mental health and frailty, leading to decreased food intake, reduced mobility and physical activity, and a lack of engagement in social relationships.Citation43 Therefore, older people with acute disease or psychological stress should be recognized as high-risk individuals for frailty.
Association of Nutritional Status and Health-Related Quality of Life
Health-related quality of life is an essential measure of health outcomes in older adults.Citation44 In our study, the MNA-SF score was positively correlated with eight domains of health-related quality of life measured by SF-36, particularly physical functioning and general health. Older individuals with good nutritional status had a higher quality of life. These results align with those of previous studies, which suggested that malnutrition predicted declining quality of life among older adults.Citation45,Citation46 A possible explanation for this is that food intake and nutrition are related to cultural and social aspects of eating and life satisfaction, a part of the quality of life.Citation45 Therefore, older adults with good nutritional status are expected to experience a better quality of life than those with poor nutrition. This result emphasizes the need to improve the nutritional status of older rural adults to improve their quality of life.
To the best of our knowledge, this is the first study addressing nutritional status among rural older adults living in a community in Vietnam. It provides a clear understanding of malnutrition and risk of malnutrition status and their association with frailty and quality of life among older people in a lower-middle-income country. However, our study has some limitations. First, this was a cross-sectional study; hence, it could not identify the causal relationship between malnutrition and frailty and health-related quality of life. Second, the data may not be nationally representative because our study was limited to a rural province in Vietnam and we may have a selection bias because we did not recruit participants who did not register to primary care. These would be fruitful areas for future research with larger sample sizes and diverse populations in Vietnam. Moreover, our study used overlapping diagnostic criteria for malnutrition (based on MNA-SF) and frailty (based on the FRAIL scale). Approximately 45% of the malnourished individuals had weight loss, accounting for 25% of the frail group. Therefore, our study may have overestimated the association between malnutrition and frailty.
Conclusion
Malnutrition and the risk of malnutrition were significantly higher among older adults living in the community, particularly in those aged ≥ 80 years in an agricultural province in Vietnam. Older individuals with malnutrition had approximately five-fold higher odds of frailty than those without malnutrition. Those with psychological stress or acute disease in the past 3 months had a greater risk of frailty than those without. Furthermore, nutritional status was positively correlated with the health-related quality of life among older rural Vietnamese adults. Therefore, there is a need for screening older rural adults for malnutrition and risk of malnutrition since they lack access to health services, and as nutrition may receive little attention from healthcare providers. In particular, further interventional studies are needed to explore whether early nutritional interventions may reduce the risk of frailty and increase the quality of life among older adults in rural areas.
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board of the University of Medicine and Pharmacy at Ho Chi Minh City (Approval number: 26/HĐĐĐ-ĐHYD). Written informed consent was obtained from the participants in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- Rasheed S, Woods RT. Malnutrition and quality of life in older people: a systematic review and meta-analysis. Ageing Res Rev. 2013;12(2):561–566. doi:10.1016/j.arr.2012.11.003
- Jung SE, Kim S, Bishop A, et al. Poor nutritional status among low-income older adults: examining the interconnection between self-care capacity, food insecurity, and depression. J Acad Nutr Diet. 2019;119(10):1687–1694. doi:10.1016/j.jand.2018.04.009
- Damayanthi H, Prabani KIP. Nutritional determinants and COVID-19 outcomes of older patients with COVID-19: a systematic review. Arch Gerontol Geriatr. 2021;95:104411. doi:10.1016/j.archger.2021.104411
- World Health Organization. Evidence profile: malnutrition. Integrated care for older people (ICOPE); 2017:1–31. Available from: https://www.who.int/ageing/health-systems/icope/evidence-centre/ICOPE-evidence-profile-malnutrition.pdf?ua=1#:~:text=Undernutrition%20is%20common%20among%20older,%2Dincome%20countries%20(6). Accessed February 22, 2022.
- Krishnamoorthy Y, Vijayageetha M, Kumar SG, et al. Prevalence of malnutrition and its associated factors among elderly population in rural Puducherry using mini-nutritional assessment questionnaire. J Family Med Prim Care. 2018;7(6):1429–1433. doi:10.4103/jfmpc.jfmpc_22_18
- Ahmad MH, Salleh R, Siew Man C, et al. Malnutrition among the elderly in Malaysia and its associated factors: findings from the national health and morbidity survey 2018. J Nutr Metab. 2021;2021:6639935. doi:10.1155/2021/6639935
- Evans C. Malnutrition in the elderly: a multifactorial failure to thrive. Perm J. 2005;9(3):38–41. doi:10.7812/TPP/05-056
- Laur CV, McNicholl T, Valaitis R, et al. Malnutrition or frailty? Overlap and evidence gaps in the diagnosis and treatment of frailty and malnutrition. Appl Physiol Nutr Metabol. 2017;42(5):449–458. doi:10.1139/apnm-2016-0652
- Verlaan S, Ligthart-Melis GC, Wijers SLJ, et al. High prevalence of physical frailty among community-dwelling malnourished older adults-a systematic review and meta-analysis. J Am Med Dir Assoc. 2017;18(5):374–382. doi:10.1016/j.jamda.2016.12.074
- Liang H, Li X, Lin X, et al. The correlation between nutrition and frailty and the receiver operating characteristic curve of different nutritional indexes for frailty. BMC Geriatr. 2021;21(1):619. doi:10.1186/s12877-021-02580-5
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. doi:10.1093/gerona/56.3.M146
- Fried LP, Cohen AA, Xue Q-L, et al. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1(1):36–46. doi:10.1038/s43587-020-00017-z
- Wei K, Nyunt MS, Gao Q, et al. Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults: results from the Singapore longitudinal aging study 1. JAMA Netw Open. 2018;1(3):e180650. doi:10.1001/jamanetworkopen.2018.0650
- Holmes S. The effects of undernutrition in hospitalised patients. Nurs Standard. 2007;22(12):35–38. doi:10.7748/ns2007.11.22.12.35.c6242
- Volkert D, Beck AM, Cederholm T, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. 2019;38(1):10–47. doi:10.1016/j.clnu.2018.05.024
- World Health Organization. Ageing and health in viet nam. aging and health; 2016. Available from: https://www.who.int/vietnam/health-topics/ageing-and-health. Accessed February 23, 2022.
- Help Age Global Network. Vietnam age watch report card ageing population in Vietnam; 2019. Available from: https://ageingasia.org/ageing-population-vietnam/#:~:text=The%20number%20of%20older%20people%3A%20Vietnam%20is%20one%20of%20the,third%20of%20the%20total%20population.&text=The%20majority%20of%20older%20people,in%20rural%20and%20mountainous%20areas. Accessed February 23, 2022.
- Tran TP, Nguyen LT, Hirose K, et al. Malnutrition is associated with dysphagia in Vietnamese older adult inpatients. Asia Pac J Clin Nutr. 2021;30(4):588–594. doi:10.6133/apjcn.202112_30(4).0005
- Nguyen TTH, Vu HTT, Nguyen TN, et al. Assessment of nutritional status in older diabetic outpatients and related factors in Hanoi, Vietnam. J Multidiscip Healthc. 2019;12:601–606. doi:10.2147/JMDH.S194155
- City Population. Trà Vinh province in Vietnam. Provincial division; 2019. Available from: http://citypopulation.de/en/vietnam/prov/admin/84__tr%C3%A0_vinh/. Accessed February 23, 2022.
- Bank TW. Population, total - Vietnam. Population; 2022. Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=VN. Accessed March 10, 2023.
- Abate T, Mengistu B, Atnafu A, et al. Malnutrition and its determinants among older adults people in Addis Ababa, Ethiopia. BMC Geriatr. 2020;20(1):498. doi:10.1186/s12877-020-01917-w
- Carlin JB, Hocking J. Design of cross-sectional surveys using cluster sampling: an overview with Australian case studies. Aust N Z J Public Health. 1999;23(5):546–551. doi:10.1111/j.1467-842X.1999.tb01317.x
- Alimohamadi Y, Sepandi M. Considering the design effect in cluster sampling. J Cardiovasc Thorac Res. 2019;11:78. doi:10.15171/jcvtr.2019.14
- Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–788. doi:10.1007/s12603-009-0214-7
- Vellas B, Villars H, Abellan G, et al. Overview of the MNA--its history and challenges. J Nutr Health Aging. 2006;10(6):456–463;discussion 463–455.
- Rubenstein LZ, Harker JO, Salvà A, et al. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol a Biol Sci Med Sci. 2001;56(6):M366–372. doi:10.1093/gerona/56.6.M366
- Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature--what does it tell us? J Nutr Health Aging. 2006;10(6):466–485;discussion 485–467.
- Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
- Anh D, Nguyen T, Nguyen T, Nguyen TV. The validity of the FRAIL scale in frailty screening among Vietnamese older people. Aging Med Healthc. 2022;13:87–92. doi:10.33879/AMH.132.2021.07060
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi:10.1097/00005650-199206000-00002
- Khoa VT, Khue NT. Translation, cultural adaptation and preliminary validity of the Vietnamese Short Form 36 (SF-36). Hội Nội Tiết và Đái Tháo Đường miền Trung. 2016;19:154.
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi:10.1093/geront/9.3_Part_1.179
- Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–727. doi:10.1111/j.1532-5415.1983.tb03391.x
- Nestlé Nutrition Institute. Mini Nutritional Assessment MNA®. https://www.mna-elderly.com: https://www.mna-elderly.com/sites/default/files/2021-10/mna-mini-english.pdf.%20www.mna-elderly.com. Available from:
- Kim J, Lee Y, Won CW, et al. Nutritional status and frailty in community-dwelling older Korean adults: the Korean frailty and aging cohort study. J Nutr Health Aging. 2018;22(7):774–778. doi:10.1007/s12603-018-1005-9
- CEIC. Vietnam household income per capita. Vietnam; 2021; Available from: https://www.ceicdata.com/en/indicator/vietnam/annual-household-income-per-capita#:~:text=Vietnam%20Annual%20Household%20Income%20per,averaged%20value%20of%20813.323%20USD. Accessed January 11, 2023.
- Maseda A, Diego-Diez C, Lorenzo-López L, et al. Quality of life, functional impairment and social factors as determinants of nutritional status in older adults: the VERISAÚDE study. Clin Nutr. 2018;37(3):993–999. doi:10.1016/j.clnu.2017.04.009
- Donini LM, Scardella P, Piombo L, et al. Malnutrition in elderly: social and economic determinants. J Nutr Health Aging. 2013;17(1):9–15. doi:10.1007/s12603-012-0374-8
- Hoogendijk EO, Flores Ruano T, Martínez-Reig M, et al. Socioeconomic position and malnutrition among older adults: results from the FRADEA study. J Nutr Health Aging. 2018;22(9):1086–1091. doi:10.1007/s12603-018-1061-1
- Crichton M, Craven D, Mackay H, et al. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: associations with geographical region and sex. Age Ageing. 2019;48(1):38–48. doi:10.1093/ageing/afy144
- Ferede YM, Derso T, Sisay M. Prevalence of malnutrition and associated factors among older adults from urban and rural residences of Metu district, Southwest Ethiopia. BMC Nutr. 2022;8(1):52. doi:10.1186/s40795-022-00532-9
- Navarro-Pardo E, Facal D, Campos-Magdaleno M, et al. Prevalence of cognitive frailty, do psychosocial-related factors matter? Brain Sci. 2020;10(12):968. doi:10.3390/brainsci10120968
- MacLeod S, Schwebke K, Hawkins K, et al. Need for comprehensive health care quality measures for older adults. Popul Health Manag. 2017;21(4):296–302. doi:10.1089/pop.2017.0109
- Keller HH, Østbye T, Goy R. Nutritional risk predicts quality of life in elderly community-living Canadians. J Gerontol A Biol Sci Med Sci. 2004;59(1):68–74. doi:10.1093/gerona/59.1.M68
- Keshavarzi S, Ahmadi SM, Lankarani KB. The impact of depression and malnutrition on health-related quality of life among the elderly Iranians. Glob J Health Sci. 2014;7(3):161–170. doi:10.5539/gjhs.v7n3p161