Abstract
Poor balance is considered a challenging risk factor for falls in older adults. Therefore, innovative interventions for balance improvement in this population are greatly needed. The aim of this study was to evaluate the effect of a new virtual-reality system (the Balance Rehabilitation Unit [BRU]) on balance, falls, and fear of falling in a population of community-dwelling older subjects with a known history of falls. In this study, 60 community-dwelling older subjects were recruited after being diagnosed with poor balance at the Falls and Fractures Clinic, Nepean Hospital (Penrith, NSW, Australia). Subjects were randomly assigned to either the BRU-training or control groups. Both groups received the usual falls prevention care. The BRU-training group attended balance training (two sessions/week for 6 weeks) using an established protocol. Change in balance parameters was assessed in the BRU-training group at the end of their 6-week training program. Both groups were assessed 9 months after their initial assessment (month 0). Adherence to the BRU-training program was 97%. Balance parameters were significantly improved in the BRU-training group (P < 0.01). This effect was also associated with a significant reduction in falls and lower levels of fear of falling (P < 0.01). Some components of balance that were improved by BRU training showed a decline after 9 months post-training. In conclusion, BRU training is an effective and well-accepted intervention to improve balance, increase confidence, and prevent falls in the elderly.
Introduction
Falls in older persons are associated with fear of falling, lack of confidence, injuries, hospitalizations and, in some cases, death.Citation1 Although broadly implemented, falls prevention programs are a major burden to health care budgets worldwide. This is due to the complexity of the secondary prevention programs and the limited adherence to them in both community and institutional settings.Citation1,Citation2
Older fallers suffering from balance problems constitute one of the most challenging types of patients in clinical practice.Citation3 The only interventions that have demonstrated an effect on balance and falls prevention are vitamin D supplementation, Tai Chi, and exercise.Citation4 A recent meta-analysis by Muir and Montero-OdassoCitation5 reported that vitamin D supplementation has beneficial effects on strength and balance but not on gait. Another recent meta-analysis proposed Tai Chi programs as the most beneficial intervention to improve balance in older adults,Citation6 and a recent Cochrane review concluded that exercise has a statistically significant beneficial effect on balance in the short term, with the strength of the evidence being limited by the short duration of the studies.Citation7 However, despite the evidence demonstrating the effectiveness of these interventions, their implementation in real-life settings has been challenging. Tai Chi requires a considerable amount of motivation and physical endurance.Citation8 And in terms of adherence, exercise programs and vitamin D supplementation have shown variable and frequently discouraging results.Citation7,Citation9,Citation10–Citation12
Overall, due to the important role that balance disorders have in the pathogenesis of falls,Citation3,Citation4 and the limitations of the current interventions to improve balance in older fallers,Citation7–Citation12 the identification of new effective interventions is pivotal. In this study we aimed to evaluate the effect of a new virtual-reality system (the Balance Rehabilitation Unit [BRU]) using virtual reality to assess balance and provide a training system for balance in a population of community-dwelling older subjects with a known history of falls.
Methods
Subjects
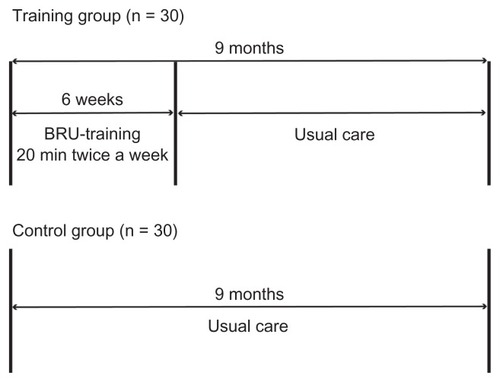
The study design is summarized in . Participants (65 years and older) were recruited at the Falls and Fractures Clinic, Nepean Hospital in Penrith (NSW, Australia). Subjects attended the clinic after suffering at least one fall within 6 months prior to the assessment. All subjects were included in the study after showing poor performance in their balance, which was assessed using the accepted parameters of normality reported by the posturography component of the BRU.Citation13–Citation15 These parameters included limits of stability (LOS), interpreted as the maximum sway on the platform before losing stability, and area of the ellipse of confidence (CE) for the center of pressure (COP) at six different conditions: open eyes and eyes closed on hard surface, eyes closed on foam, and several different visual stimuli (saccadic condition combined with optokinetic bars in four different directions and visual-vestibular conditions) using the 3D virtual-reality goggles. Inclusion criteria were: LOS lower than 170 cm2 and COP > 20 cm2 in at least three of six different conditions. Exclusion criteria were: (a) severe visual impairment, (b) inability to ambulate independently with a cane or walker, (c) inability to stand unaided for 60 seconds, (d) score of <22/30 in the Mini-Mental State Examination,Citation16 (e) Parkinson’s disease or any neuromuscular conditions, (f) Geriatric Depression Scale (GDS) > 8/15,Citation17 and (g) inability to understand or answer the study questionnaires. After agreeing to be part of the study and after informed consent was obtained, participants went through a comprehensive assessment that included structured questionnaires, information about chronic diseases, physical examination and anthropometric measurements. Subjects were then randomly assigned to either BRU-training or control groups. The study was conducted in accordance with the ethical standards set forth in the Declaration of Helsinki (1983). The local ethics committee at Nepean Blue Mountains Local Health District approved the project.
Postural assessment
BRU is a recently validated and reliable method that combines variable somatosensory, visual and vestibular conditions, which are used to assess and train balance.Citation14,Citation15,Citation18–Citation20 The assessment component of the BRU (posturography) evaluates postural control responses to different types of visual and visual-vestibular stimulation on standing surfaces of different firmness. The posturography report is automatically generated by the software integrated in the BRU system and includes LOS and COP under several different conditions. The assessment takes about 30 minutes to perform. To avoid any bias in the assessment, a physiotherapist performed all the posturography assessments at time 0, at week 6 in the BRU-training group, and at month 9 in both groups. The same physiotherapist was responsible for asking the subjects about new falls and assisting them to perform the fear of falling questionnaires.
Definition of falls
Falls were defined as “an unexpected event in which the participants come to rest on the ground, floor, or lower level.”Citation21 The occurrence of falls was retrospectively assessed by asking the participant (1) whether they have suffered a fall and, (2) the number of falls during the 6 months prior to the assessment.
Gait assessment
A GAIT Rite® (CIR Systems Inc, Havertown, PA, USA) instrumented walkway (810 cm × 89 cm × 0.625 cm, sample rate = 80 Hz) was positioned along a straight section of the walkway to record spatiotemporal gait data.
Grip strength
Grip strength was measured following the Groningen Elderly Test using a Smedley Hand Dynamometer (Stoelting, Wood Dale, IL, USA).Citation22 The best of three attempts (with 30 seconds rest between them) was recorded.
Serum measurements
Venous blood was collected from resting subjects for the measurement of serum 25(OH)D3, parathyroid hormone (PTH), calcium, creatinine, and albumin. Serum 25(OH)D3 concentration was measured by chemiluminescence using the Elecsys 25(OH)D3 assay (Roche, Mannheim, Germany). Distributor is correct. The intra- and interassay precisions were 7.5% and 10.6%, respectively (normal range = 10–132 nmol/l). Intact PTH was measured by immunochemoluminometric assay (Immulite 2000 Siemens, Erlander, Germany; normal range = 12–72 pg/mL). The intra- and interassay precisions were 7% and 5%, respectively. Serum calcium, albumin, and creatinine were determined using automated standard laboratory methods. Because of the high prevalence of hypoalbuminemia in older adults, the serum concentration of albumin and calcium were used to correct the calcium value (calcium-corrected value = Ca + 0.8 [40 − albumin]). The calcium-corrected value was used in the subsequent analysis. The clearance of creatinine was calculated from the Cockcroft formula ([(140 – age in years) × weight (kg)/ 72 × creatinine mol/L]). All measurements were performed at the Nepean Hospital, Penrith, Australia.
Clinical assessment
Depression was assessed using the Geriatric Depression Scale (GDS). Height was measured with a digital stadiometer. Nutritional assessment was performed by body mass index (BMI) calculation and by completing the Mini-Nutritional Assessment (MNA) tool.
Fear of falling
The Survey of Activities and Fear of Falling in the Elderly (SAFFE)Citation23 was used to assess fear of falling. To facilitate the analysis, a total SAFFE fear-of-falling score was generated as described previously.Citation24 This method, which is based on a 5-point Likert (0–4 item) response format with higher scores indicating a greater fear of falling, has demonstrated an internal consistency of 0.70.Citation24
BRU-training protocol
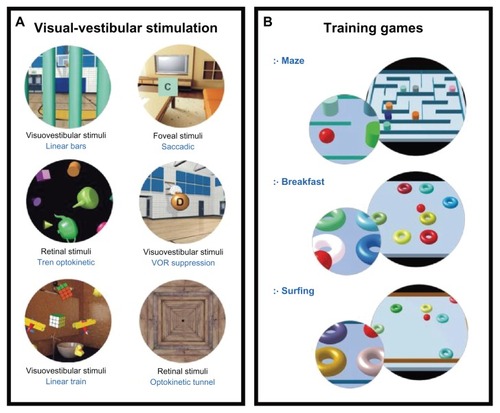
The components of the BRU-training protocol are described in detail in . Participants in the BRU-training group were scheduled for two sessions of balance training per week for 6 weeks under the guidance of a physiotherapist other than the one performing the assessments. Each training session lasted 30 minutes and consisted of a combination of visual-vestibular rehabilitation () and postural training virtual reality exercises ().Citation14 The rehabilitation exercises included saccadic, optokinetic stimulation, vestibular optokinetic and vestibular-ocular reflex exercises performed while standing. In addition, postural training virtual reality exercises were also used to improve balance (). These exercises consisted of three different postural training games with increasing levels of complexity (maximum of 15 levels), with the goal of reaching at least level 10 in every game by the end of the training period. The levels of complexity were progressively increased as the individual reported higher confidence and demonstrated learning of the correct postural control techniques required to pass to a higher level. After completing their 6 weeks of BRU training, our assessment physiotherapist obtained a new posturography report, which was then compared with the initial report (time 0).
Figure 2 Components of the BRU-training protocol. Each training session lasted 30 minutes and consisted of a combination of visual-vestibular rehabilitation (A) and postural training virtual reality exercises (B). The rehabilitation exercises (A) included saccadic and optokinetic stimulation. Postural training exercises (B) consisted of three different games (maze, breakfast and surfing) with increasing levels of complexity (maximum of 15 levels).Citation33
Falls prevention recommendations and interventions (usual care)
After their initial assessment, all participants were given general recommendations and an evidence-based care plan on falls prevention (usual care).Citation25 This usual care included an invitation to join an exercise program (following the Otago protocol),Citation26 medication review, home visit by an occupational therapist (if more than 60% of the falls occurred at home), hearing and visual assessment, nutritional supplements (when nutritional risk was identified by the MNA tool), vitamin D supplementation (1,000 IU/day independently of their serum levels), and education materials on falls prevention.
Sample size calculation
The LOS measure was selected for calculation of sample size, based on our previous preliminary results.Citation15 Expecting a post-training improvement of 10%, a sample size of 30 participants per group was required (80% power, alpha of 0.05). This sample size was also considered sufficient when data from other balance measures (COP, CEs) were used.
Statistical analysis
Values are expressed as the mean of the standard deviations (SD). The baseline characteristics of the groups were compared using Student’s unpaired t-test. We compared balance parameters within the BRU-training group at time 0 and after completing treatment (6 weeks) as well as between both groups at time 0 and 9 months using two-way analysis of repeated measures (ANOVA). When the ANOVA interaction was significant, means were compared by the Newman– Keuls method. Statistical significance was set at P < 0.05. Statistics were performed using SPSS software (v. 20; IBM, Armonk, NY, USA).
Results
Time 0: Before BRU training (both groups)
Both groups showed similar demographic, anthropometric, and health characteristics at the beginning of the study. In addition, baseline balance and gait parameters were not significantly different between the two groups ().
Table 1 Baseline characteristics of the subjects
Week 6 post-BRU training
Adherence
Of the 30 subjects in the BRU-training group, only two withdrew from the program before completing their 6 weeks of BRU training due to logistics problems to attend the sessions, which indicates a 97% adherence to the BRU-training program.
Balance parameters
Most of the participants (91%) reached at least 10 out of 15 possible levels in every group of virtual exercises. We identified a significant improvement in balance parameters after 6 weeks of BRU training (). This improvement included a significant increase in LOS (~31%; P < 0.01) and significantly smaller elliptical areas of the eyes closed on hard surface (~−33%; P < 0.01), eyes closed on foam (~−52%; P < 0.01), optokinetic stimuli (~25%; P < 0.01), and vertical (~50%; P < 0.01) and horizontal (~33%; P < 0.01) VVC.
Figure 3 (A) Comparison of limits of stability and mean ellipse of confidence areas before and after 6 weeks of Balance Rehabilitation Unit (BRU) training (in the BRU-training group) and after 9 months of the initial assessment in both BRU-training and control groups. (B and C) Both groups showed a reduction in the number of falls at month 9 postassessment. BRU training induced a significant reduction in number of falls per subject (B) and fear of falling (C) in the BRU-training group compared with the untrained control group.
Abbreviations: BRU, Balance Rehabilitation Unit; SAFFE, Survey of Activities and Fear of Falling in the Elderly.
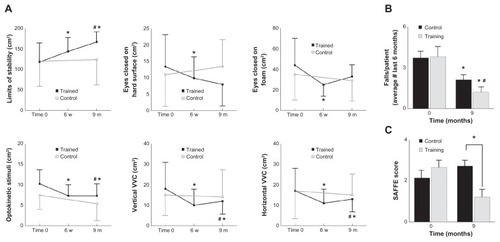
Month 9: BRU-training and control groups
Anthropometric, functional and biochemical characteristics of the participants were similar in both groups (data not shown). At month 9 post-initial assessments, both BRU-training and control groups showed the same proportion of subjects attending an exercise program (2%), taking nutritional supplements (3%) and vitamin D supplementation (48%), and reporting changes in their medications following the clinic’s recommendations (11%). As compared with the usual care group, the BRU-training group showed significantly higher level of LOS, and significantly smaller COP areas in the optokinetic stimuli and both vertical and horizontal VVC (P < 0.01). In contrast, elliptical areas for both eyes closed conditions (on hard surface and on foam) returned to the pre BRU-training levels.
Falls and fear of falling
As shown in , both groups showed a significant reduction in the incidence of falls (P < 0.05). However, BRU-training subjects reported a significantly lower number of falls as compared with the untrained controls (1.1 ± 0.7 in the BRU-training vs 2 ± 0.2 in the control group; P < 0.01). Finally, BRU-training subjects reported lower levels of fear of falling as demonstrated by a significantly lower SAFFE score in the BRU-training group compared with the control group (; P < 0.01).
Discussion
In this study, we have assessed the effectiveness of a new virtual reality training system on balance, falls, and fear of falling in a population of community-dwelling older fallers. Our system was expected to stress their balance and visio-vestibular pathways while offering them a safe and closely supervised environment, which involves less physical effort than the usual balance exercise programs. An additional advantage of this system was a higher adherence that could be due to the level of physical effort involved and to the simplicity of the BRU-training protocol, which includes easy-to-follow instructions and a closer interaction between the health professional and the subject.
After completing their BRU-training protocol, participants showed a significant improvement in their LOS and COP. In addition, 9 months after their initial assessment, the BRU-training group showed a significant reduction in both the incidence of falls and in their levels of fear of falling. As expected, the subjects in the usual-care group showed a reduction in the number of falls; however, this reduction was significantly higher in the BRU-training group, which indicates an additive and beneficial effect of this intervention on fall prevention in this population. Interestingly, the positive effects of BRU training on balance seem to reduce with time as indicated by the results of our assessment at month 9. Nevertheless, long-term studies looking at the maintenance of the beneficial effect of BRU training on these parameters are still required.
Although virtual reality has been used to rehabilitate subjects suffering from stroke,Citation27 cerebral palsy,Citation28 and brain injury,Citation29 the use of this technology in falls prevention has been limited. Indeed, apart from the studies using the BRU in younger populations,Citation18–Citation20 there are no reports in the literature of the use of virtual reality to train balance and prevent falls in older subjects. The only related evidence came from a recent study that tested the Nintendo Wii™ Fit Plus in 26 young participants (aged 43 ± 14 years) suffering from balance impairment.Citation30 Participants interacted with a television screen and no virtual reality was used. Although no data on change in balance parameters was provided, trained participants reported more enjoyment and motivation than usual physiotherapy, which coincides with the findings of the present study.
Our study has some strengths and limitations. The major strength of this study is that this is the first demonstration of the beneficial effect of balance training on balance parameters and falls in older adults using a novel, accurate, safe and effective virtual reality method. In terms of cost, with the exception of the initial investment on the BRU equipment and software, this intervention involves similar costing to any other falls prevention intervention that requires regular physiotherapy sessions. Another strength is the use of computerized posturography to document changes in balance parameters, which could be performed using the same BRU system. Although this method has the same sensitivity and specificity as the usual clinical balance tests,Citation31,Citation32 computerized posturography has major advantages such as a more precise determination of changes in balance parameters, no additional effort from the participant, and a more accurate inter- and intrarater reliability.Citation31,Citation32
In terms of the weaknesses of this study, performing a double-blind, controlled trial to test this system is clearly unfeasible, therefore we decided to use an open approach in which both the participants at the medical team were aware of the interventions. However, to prevent any assessment bias, different physiotherapists with no access to the subjects’ data were specifically assigned to perform either assessment or training. Furthermore, the evidence that both groups are similar is provided in and is demonstrated by similar involvement of the participants in our usual-care program.
Another potential limitation of the study is the use of self-reports for the falls data episodes, which could be inaccurate. However, excluding subjects with reported cognitive impairment could partially solve this limitation. Nevertheless, and although this study was not powered to assess its effect on falls prevention due to the small sample and the use of self-report, our finding that BRU training had a significantly higher effect on falls prevention deserves further exploration in future clinical trials.
A final limitation of this study could be that the control group was not exposed to the BRU equipment as often as the trained group, which could affect their performance at their second assessment. This is a very unlikely possibility since the posturography assessment, which is clearly different from the training component of BRU, is a very objective measurement that is independent of the subject’s familiarity with the system.
In conclusion, we have successfully demonstrated that the novel BRU training is an effective method to offer balance training to community-dwelling older fallers. Although it is not intended to replace, but rather to complement, other falls prevention intervention programs, BRU training offers a safe and well-accepted intervention with high levels of effectiveness and adherence that could become a successful treatment for falls prevention in older adults in the near future.
Acknowledgments
This study was supported by a research grant from the Nepean Medical Research Foundation and by the Department of Geriatric Medicine at Nepean Hospital. Dr Demontiero holds a scholarship from The Rebecca Cooper Medical Research Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
- CloseJCLordSRFall assessment in older peopleBMJ2011343d515321917828
- NymanSRVictorCROlder people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic reviewAge Ageing201140443043621502163
- WetmoreSJEiblingDEGoebelJAChallenges and opportunities in managing the dizzy older adultOtolaryngol Head Neck Surg2011144565165621493351
- RandDMillerWCYiuJInterventions for addressing low balance confidence in older adults: a systematic review and meta-analysisAge Ageing201140329730621508204
- MuirSWMontero-OdassoMEffect of vitamin d supplementation on muscle strength, gait and balance in older adults: a systematic review and meta-analysisJ Am Geriatr Soc201159122291230022188076
- LiuHFrankATai chi as a balance improvement exercise for older adults: a systematic reviewJ Geriatr Phys Ther201033310310921155504
- HoweTERochesterLJacksonAExercise for improving balance in older peopleCochrane Database Syst Rev20074CD00496317943831
- WangCColletJPLauJThe effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic reviewArch Intern Med2004164549350115006825
- PhillipsEMSchneiderJCMercerGRMotivating elders to initiate and maintain exerciseArch Phys Med Rehabil2004857 Suppl 35257
- SjöstenNMSalonojaMPiirtolaMA multifactorial fall prevention program in the community-dwelling aged: predictors of adherenceEur J Public Health200717446447017208952
- TangBMEslickGDNowsonCUse of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysisLancet2007370958865766217720017
- GrantAMAvenellACampbellMKOral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trialLancet200536594711621162815885294
- BarattoLMorassoPGReCSpadaGA new look at posturographic analysis in the clinical context: sway-density versus other parameterization techniquesMotor Control20026324627012122219
- SuarezHGeisingerDFerreiraEDBalance in Parkinson’s disease patients changing the visual inputBraz J Otorhinolaryngol201177565165522030976
- BoersmaDDemontieroOMohtasham-AmiriZVitamin D status in relation to postural stability in the elderlyJ Nutr Health Aging201216327027522456785
- FolsteinMFFolsteinSEMcHughPR“Mini-mental state”: A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res19751231891981202204
- WancataJAlexandrowiczRMarquartBWeissMFriedrichFThe criterion validity of the Geriatric Depression Scale: a systematic reviewActa Psychiatr Scand2006114639841017087788
- SuarezHMusePSuarezAPostural behavior responses to visual stimulation in patients with vestibular disordersActa Otolaryngol2000120216817211603765
- SuarezHGeisingerDSuarezAPostural control and sensory perception in patients with Parkinson’s diseaseActa Otolaryngol2009129435436019021071
- SuárezHSuárezALavinskyLPostural adaptation in elderly patients with instability and risk of falling after balance training using a virtual-reality systemInt Tinnitus J2006121414417147038
- LambSEJørstad-SteinECHauerKPrevention of Falls Network Europe and Outcomes Consensus GroupDevelopment of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensusJ Am Geriatr Soc20055391618162216137297
- SoerRvan der SchansCPGeertzenJHNormative values for a functional capacity evaluationArch Phys Med Rehabil200990101785179419801072
- LachmanMEHowlandJTennstedtSFear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE)J Gerontol B Psychol Sci Soc Sci1998531P43P509469171
- LiFFisherKJHarmerPFear of falling in elderly persons: association with falls, functional ability, and quality of lifeJ Gerontol B Psychol Sci Soc Sci2003585P283P29014507935
- MicahelYLWhitlockEPLinJSPrimary care–relevant interventions to prevent falling in older adults: a systematic evidence review for the US Preventive Services Task ForceAnn Int Med20101531281588221173416
- YangXJHillKMooreKEffectiveness of a targeted exercise intervention in reversing older people’s mild balance dysfunction: a randomized controlled trialPhys Ther2012921243721979272
- LaverKEGeorgeSThomasSVirtual reality for stroke rehabilitationCochrane Database Syst Rev20119CD00834921901720
- BrienMSveistrupHAn intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsyPediatr Phys Ther201123325826621829120
- Gil-GómezJALlorénsRAlcañizMEffectiveness of a Wii balance board-based system (eBaViR) for balance rehabilitation: a pilot randomized clinical trial in patients with acquired brain injuryJ Neuroeng Rehabil201123830
- MeldrumDGlennonAHerdmanSVirtual reality rehabilitation of balance: assessment of the usability of the Nintendo Wii(®) Fit PlusDisabil Rehabil Assist Technol20127320521022117107
- BrowneJO’HareNDevelopment of a novel method for assessing balance: the quantitative posturography systemPhysiol Meas200021452553411110250
- BrowneJO’HareGFinnAColinJClinical Assessment of the Quantitative Posturography System (QPS)Physiotherapy2002884217233
- http://www.medicaa.com/index2.php?option=com_docman&task=doc_view&gid=2&Itemid=43. Visited on: 11 February 2013