 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
To analyze the relationship between N-terminal pro-brain natriuretic peptide (NT-proBNP) and renal function, and compare the ability and cut-off thresholds of NT-proBNP to detect chronic heart failure (CHF) and predict mortality in elderly Chinese coronary artery disease (CAD) patients with and without chronic kidney disease (CKD).
Methods
The study included 999 CAD patients older than 60 years. The endpoint was all-cause mortality over a mean follow-up period of 417 days.
Results
The median age was 86 years (range: 60–104 years), and the median NT-proBNP level was 409.8 pg/mL. CKD was present in 358 patients. Three hundred and six patients were positive for CHF. One hundred and ten CKD patients and 105 non-CKD patients died. Not only CKD, but also estimated glomerular filtration rate independently affected NT-proBNP. NT-proBNP detected CHF with a cut-off value of 298.4 pg/mL in non-CKD patients and a cut-off value of 435.7 pg/mL in CKD patients. NT-proBNP predicted death with a cut-off value of 369.5 pg/mL in non-CKD patients and a cut-off value of 2584.1 pg/mL in CKD patients. The NT-proBNP level was significantly related to the prevalence of CHF and all-cause mortality in CAD patients with and without CKD; this effect persisted after adjustment. The crude and multiple adjusted hazard ratios of NT-proBNP to detect CHF and predict mortality were significantly higher in patients with CKD compared with the remainder of the population. The addition of NT-proBNP to the three-variable and six-variable models generated a significant increase in the C-statistic.
Conclusion
Amongst elderly Chinese CAD patients, there was an independently inverse association between NT-proBNP and renal function. With the higher cutoff points, NT-proBNP better detected CHF and better predicted mortality in CKD patients than in non-CKD patients.
Introduction
N-terminal pro-brain natriuretic peptide (NT-proBNP) is a well-known biomarker for cardiovascular diseases, including heart failure (HF) and coronary artery disease (CAD), and may facilitate the early diagnosis of acute HF (AHF) and stratification of cardiac risk.Citation1 Chronic kidney disease (CKD) is a common comorbidity that affects a significant portion of patients with cardiovascular diseases.Citation2,Citation3 Similarly, CKD patients are at increased risk of suffering from cardiovascular complications.Citation4–Citation6 Therefore, patients with known or suspected CAD and HF, as well as CKD patients, are potential candidates for NT-proBNP testing. Understanding the influence of renal function on the NT-proBNP level is thus highly relevant for clinical application. As the NT-proBNP level is more frequently utilized, there has been much debate over the interpretation and significance of the NT-proBNP level in CKD patients.Citation1 Indeed, although several studies have provided clear and convincing evidence of the diagnostic value of NT-proBNP for AHF,Citation1 the ability of NT-proBNP to detect patients with chronic HF (CHF) and the appropriate cutoff values have not been tested in a sufficient number of CAD patients with and without CKD.Citation7 In addition, previous studies have examined the prognostic usefulness of NT-proBNP in HF patients with and without CKD,Citation8,Citation9 but studies focusing on the prognostic impact in CAD patients with concomitant CKD are limited. Moreover, in elderly patients, data illustrating the relationship between renal function and NT-proBNP level and relating the detecting and prognostic role of NT-proBNP level to renal function is scarce, especially in the People’s Republic of China. To be of clinical value, NT-proBNP measurements need to be evaluated within the context of renal function in elderly patients. Thus, the current study attempted to investigate the serum NT-proBNP levels of patients with varying levels of renal function, and compare the roles and cutoff values of NT-proBNP to detect CHF and predict mortality in elderly Chinese CAD patients with and without CKD.
Methods
Study population
Initially, this prospective study included 1050 CAD inpatients older than 60 years from October 11, 2007 to July 2, 2011. The Chinese PLA General Hospital was their designated hospital and had the integrated long-term medical and final death records of the patients, which made it easier for us to follow-up effectively and judge endpoints accurately. The diagnosis of CAD was supported by history, symptoms of typical angina, cardiac markers, and specific cardiac examinations, such as electrocardiogram (resting/exercise), echocardiography, radionuclide imaging, computed tomography, and coronary angiography, as established by chief physicians on the basis of the American College of Cardiology (ACC)/American Heart Association (AHA) or European Society of Cardiology (ESC) guidelines.Citation10–Citation12 Serum NT-proBNP was not obtained in a total of 51 patients. Thus, 999 patients were eligible for analysis.
Measurements and definitions
Serum NT-proBNP was measured by the NT-proBNP Flex Reagent Cartridge (PBNP/LPBN) produced by Siemens Healthcare Diagnostics Inc (Deerfield, IL, USA) on the Dimension RxL Max (analytical measurement range: 10–30,000 pg/mL; Siemens Healthcare Global, Erlangen, Germany). Body mass index (BMI) was defined as weight in kilograms divided by the square of height in meters. Mean systolic blood pressure (MSBP) and mean diastolic blood pressure (MDBP) were taken as the average of five separate measurements. Conventional echocardiogram was performed and the ejection fraction (EF) was obtained. Estimated glomerular filtration rate (eGFR) was calculated by a modified Modification of Diet in Renal Disease (MDRD) equation based on data from Chinese CKD patients:Citation13
CKD was defined as eGFR < 60 mL/minute/1.73 m2 on the basis of the Kidney Disease Outcomes Quality Initiative (KDOQI) Working Group definition.Citation14 Atrial fibrillation (AF) and CHF were diagnosed by chief physicians according to the ACC/AHA/ESC guidelines for AFCitation15 and the ESC guidelines for CHF.Citation16 Patients with a MSBP ≥ 140 mmHg, MDBP ≥ 90 mmHg or patients receiving medication for treatment of hypertension (HTN) were defined as having HTN. Patients with a fasting glucose concentration ≥ 7 mmol/L or receiving treatment with an oral hypoglycemic agent/insulin were defined as having diabetes mellitus (DM). If the hemoglobin level was lower than 120 g/L in males or 110 g/L in females, the diagnosis of anemia was established. Hypoalbuminemia was considered to be present if patients had a serum albumin < 30 g/L. The diagnosis of hyperuricemia was made if the patients met the following criterion: uric acid > 420 umol/L for males or >350 umol/L for females.
Traditional prognostic models
In spite of many models predicting renal replacement therapy, there are few models to forecast mortality for patients with CKD. The most basic and simple risk assessment model of CKD consists of age, gender, and eGFR (three-variable model). Meanwhile, the six-variable model includes age, gender, eGFR, DM, HTN, and anemia, and has been reported to have a greater ability to estimate CKD mortality.Citation17
End point
Given the high incidence of multiple organ failure in the elderly as well as the priority of all-cause mortality in outcome studies, the primary endpoint assessed in the current study was all-cause death. The study population had a mean follow-up period of 417 days (median: 317 days; 75% range: 185–557 days). No patient was dropped during the study period. Follow-up data was obtained from medical records and telephone contact. Death was ascertained from death record; a legal document including time, site, and other information.
Statistical methods
Continuous variables were described using mean and standard deviation for data with a normal distribution, and median and 75% range for non-normally distributed variables. Categorical data were expressed as a percentage of the total. The correlation between the NT-proBNP level and other variables was determined by Spearman rank correlation coefficients. The NT-proBNP level was logarithmically transformed to meet the multinormality assumption. The multiple linear regression model with NT-proBNP as the dependent variable was used to determine independent determinants of NT-proBNP. Receiver-operating characteristic curves and area under the curve (C statistics) were used to assess the usefulness of NT-proBNP to identify CHF or predict death. The added predictive abilities of NT-proBNP to CKD risk assessment models regarding mortality were investigated by comparison of C-statistics between models and models + NT-proBNP. The Z-statistic was used to compare the C-statistics. To examine the ability of NT-proBNP in detecting CHF, the multivariate logistic regression model with CHF as a dependent variable was developed. To test prognostic values of NT-proBNP for mortality, the multivariate Cox regression model with death as the dependent variable was used. Differences in hazard ratios (HRs) between patients with CKD and without CKD were checked with interaction analysis. Survival curves were generated by means of Kaplan–Meier estimates. A two-tailed P-value of less than 0.05 was considered to be statistically significant. There was little missing data; in the cases where date was missing, the missing values were calculated by multiple imputations and the results were pooled to minimize bias.Citation18 All information on the characteristics of patients was entered into the database by trained abstractors and checked by other independent abstractors. SPSS 17 (SPSS Inc., Chicago, IL, USA) and MedCalc 9.6 for Windows (MedCalc Software bvba, Ostend, Belgium) were used as the statistical systems.
Results
Independent impact of cardiac factors and renal function on the NT-proBNP level
At baseline, the median age of the study patients was 86 years (range: 60–104 years) and the median NT-proBNP level was 409.8 pg/mL (158.4–1783.8 pg/mL). displays descriptive statistics of the study population. CKD was present in 358 patients (35.8%), who had a significantly higher NT-proBNP concentration (median NT-proBNP level: 1027.5 pg/mL [267.3–3660.5 pg/mL]) than patients without CKD (median NT-proBNP level: 298.6 pg/mL [129.1–950.2 pg/mL]) (P < 0.001). There were even significant distinctions in NT-proBNP level between patients in different stages of CKD (eGFR 45–60 mL/minute/1.73 m2: 526.3 pg/mL [174.9–1915.4 pg/mL]; eGFR 30–45 mL/minute/1.73 m2: 1531.0 pg/mL [518.6–3755.6 pg/mL]; eGFR < 30 mL/minute/1.73 m2: 4734.7 pg/mL [1357.0– 19163.0 pg/mL]; all P < 0.001). The NT-proBNP levels in all of the patients had a strong inverse association with eGFR (correlation coefficient, −0.319, P < 0.001). After adjusting for age; gender; BMI; acute myocardial infarction (AMI); CHF; HTN; DM; AF; anemia; hypoalbuminemia; hyperuricemia; MSBP; heart rate; EF < 40%; serum Na+, Ka+, and Ca2+ levels; and diuretic use, not only CKD and eGFR < 45 mL/minute/1.73 m2, but also the eGFR level as a continuous variable (all P < 0.001) had an independent influence on the NT-proBNP level. Other independently associated factors were age, BMI, AMI, CHF, AF, anemia, hypoalbuminemia, heart rate, EF < 40%, and serum Ka+ and Ca2+ levels (all P < 0.05). BMI and serum Ca2+ had a negative correlation with NT-proBNP level; all other factors had a positive correlation with NT-proBNP level. The impact of CKD on the NT-proBNP level (β value: 0.135) was less than the impact of cardiac factors (CHF, AMI, AF, and EF < 40%) and anemia, whereas the impact of eGFR < 45 mL/minute/1.73 m2 on the NT-proBNP level (β value: 0.228) was higher than these factors. No significant correlation was noted between the NT-proBNP level and gender, HTN, DM, hyperuricemia, MSBP, serum Na+ level, and diuretic use (all P > 0.05).
Table 1 Baseline characteristics of study population
Superior ability of NT-proBNP to detect CHF in CKD patients
Of 999 eligible patients, 306 (30.6%) were positive for CHF. The NT-proBNP level was significantly related to the prevalence of CHF in CAD patients with CKD (crude HR: 1.728, 95% confidence interval [CI]: 1.487–2.007, P < 0.001) and without CKD (crude HR: 1.727, 95% CI: 1.510–1.977, P < 0.001), and the significance persisted after adjusting for age; gender; BMI; AMI; HTN; DM; AF; anemia; hypoalbuminemia; hyperuricemia; MSBP; heart rate; EF < 40%; serum Na+, Ka+, and Ca2+ levels; and diuretic use (with CKD: adjusted HR: 1.707, 95% CI: 1.415–2.061, P < 0.001; without CKD: adjusted HR: 1.474, 95% CI: 1.202–1.806, P < 0.001). By interaction analysis, the crude HR values (1.728 versus 1.727, P < 0.001) and multiple adjusted HR values (1.707 versus 1.474, P = 0.002) of NT-proBNP were significantly higher in patients with CKD compared with the remainder of the population.
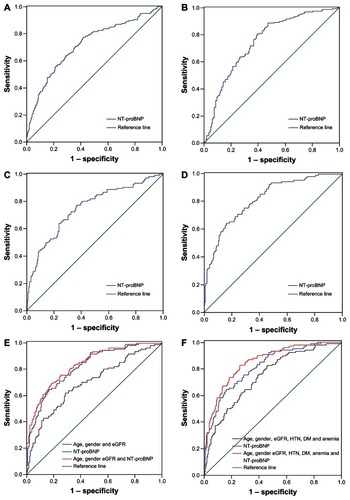
In patients without CKD, NT-proBNP detected CHF with a C-statistic of 0.720 (95% CI: 0.671–0.769, P < 0.001) and a cutoff value of 298.4 pg/mL (). In patients with CKD, NT-proBNP detected CHF with a C-statistic of 0.749 (95% CI: 0.689–0.799, P < 0.001) and a cutoff value of 435.7 pg/mL (). The C-statistic for NT-proBNP in detecting CHF in patients with CKD was higher (but not significant) than in patients without CKD (0.749 versus 0.720, P = 0.421). In patients without CKD, CHF was more common in patients with a NT-proBNP level > 298.4 pg/mL in comparison to patients with a NT-proBNP level < 298.4 pg/mL (HR: 4.790, 95% CI: 3.126–7.338, P < 0.001). In CKD patients, the likelihood of CHF was significantly higher in patients with a NT-proBNP level > 435.7 pg/mL in comparison to patients with a NT-proBNP level < 435.7 pg/mL (HR: 8.750, 95% CI: 4.978–15.380, P < 0.001).
Figure 1 (A) Non-CKD patients (n = 641): ROC curve analysis for NT-proBNP identifying CHF. (B) CKD patients (n = 358): ROC curve analysis for NT-proBNP identifying CHF. (C) non-CKD patients (n = 641): ROC curve analysis for NT-proBNP predicting death. (D) CKD patients (n = 358): ROC curve analysis for NT-proBNP predicting death. (E) CKD patients (n = 358): comparison of ROC curve predicting death between NT-proBNP and the three-variable model. (F) CKD patients (n = 358): comparison of ROC curve predicting death between NT-proBNP and the six-variable model.
Superior independent and compensated prognostic ability of NT-proBNP in CKD patients
One hundred and ten patients (30.7%) with CKD and 105 patients (16.4%) without CKD died during the follow-up period. The NT-proBNP level was significantly related to all-cause death in CAD patients with CKD (crude HR: 1.766, 95% CI: 1.574–1.983, P < 0.001) and without CKD (crude HR: 1.691, 95% CI: 1.504–1.901, P < 0.001), and the significance persisted after adjusting for age; gender; BMI; AMI; CHF; HTN; DM; AF; anemia; hypoalbuminemia; hyperuricemia; MSBP; heart rate; EF < 40%; serum Na+, Ka+, and Ca2+ levels; and diuretic use (with CKD: adjusted HR: 1.542, 95% CI: 1.324–1.795, P < 0.001; without CKD: adjusted HR: 1.384, 95% CI: 1.190–1.609, P < 0.001). By interaction analysis, the crude HR values (1.766 versus 1.691, P < 0.001) and multiple adjusted HR values (1.542 versus 1.384, P = 0.008) of NT-proBNP were significantly higher in patients with CKD compared with the remainder of the population. Meanwhile, patients with different stages of CKD were analyzed separately. With the deterioration of CKD, the crude HRs (eGFR > 45 mL/minute/1.73 m2: HR: 2.051, 95% CI: 1.609–2.615; eGFR 30–45 mL/minute/1.73 m2: HR: 1.716; 95% CI: 1.340–2.198; eGFR < 30 mL/minute/1.73 m2: HR: 1.574; 95% CI: 1.253–1.978; all P < 0.001) and multiple adjusted HRs (eGFR > 45 mL/minute/1.73 m2: HR: 2.075, 95% CI: 1.462–2.945; eGFR 30–45 mL/minute/1.73 m2: HR: 1.922; 95% CI: 1.288–2.870; eGFR < 30 mL/minute/1.73 m2: HR: 1.729; 95% CI: 1.189–2.515; all P < 0.05) of NT-proBNP decreased. Of note, regardless of the stage of CKD, NT-proBNP was an independent predictor of all-cause mortality in these patients. The crude and multiple adjusted influences of NT-proBNP on mortality are listed in .
Table 2 Hazard ratios of NT-proBNP in elderly Chinese coronary artery disease patients with and without CKD
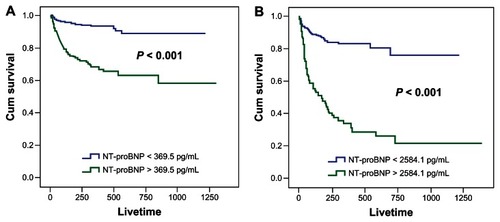
NT-proBNP predicted death with a C-statistic of 0.751 (95% CI: 0.698–0.805, P < 0.001) in patients without CKD () and a C statistic of 0.818 (95% CI: 0.772–0.864, P < 0.001) in patients with CKD (). The C-statistic for NT-proBNP in predicting death in patients with CKD was higher (but not significant) than in patients without CKD (0.818 versus 0.751, P = 0.064). The cutoff value of NT-proBNP that best distinguished the deaths versus the survivors amongst patients with CKD (2584.1 pg/mL) was approximately six times higher than the NT-proBNP cutoff value amongst patients without CKD (369.5 pg/mL). In addition, there was a significantly worse prognosis in patients with a NT-proBNP level greater than the cutoff value compared with patients with a NT-proBNP level less than cutoff value (with CKD: HR: 5.304, 95% CI: 3.582–7.853; without CKD: HR: 5.152, 95% CI: 3.264–8.130; all P < 0.001). Kaplan– Meier analyses based on the two cutoff values provided better descriptions ().
Figure 2 (A) Non-CKD patients (n = 641): Kaplan–Meier estimate of survival according to the cutoff point of NT-proBNP (369.5 pg/mL). (B) CKD patients (n = 358): Kaplan–Meier estimate of survival according to the cutoff point of NT-proBNP (2584.1 pg/mL).
The analyses of the compensated predictive roles of NT-proBNP to the risk assessment models of CKD were confined to patients with CKD. The C-statistic of the NT-proBNP level in predicting death in patients with CKD was statistically greater than the three-variable (0.818 versus 0.694, P < 0.001) and six-variable models (0.818 versus 0.744, P = 0.035) (, ). The addition of the NT-proBNP level to the three-variable (0.836 versus 0.694, P < 0.001) and six-variable models (0.853 versus 0.744, P < 0.001) generated a significant increase in the C-statistic ().
Table 3 Prognostic value of NT-proBNP and other models in elderly Chinese patients with both coronary artery disease and chronic kidney disease
Discussion
Independent impact of cardiac factors and renal function on the NT-proBNP level
The current study showed an inverse, significant, and independent correlation between the NT-proBNP level and eGFR in elderly CAD patients with and without CKD. This finding corroborated recent observational studies that indicated a relationship between NT-proBNP and eGFR in patients with stable ischemic heart disease,Citation19 peripheral artery disease,Citation20 HF,Citation21 and acute dyspnea,Citation1 and in patients with various stages of renal function;Citation4,Citation22 this finding was in contrast to pooled data which suggested that there was no interdependence between renal impairment and increased NT-proBNP concentration.Citation23 The correlation coefficients between NT-proBNP and eGFR typically ranged from −0.3 to −0.5, which were in agreement with our result (−0.319). The current study illustrated that the cause of an elevated NT-proBNP level was multifactorial and reflected the changes in cardiac and renal function. To what extent the increase in the NT-proBNP level was due to decreased renal clearance versus increased cardiac production is controversial. Previous assessments have tempered the enthusiasm to conclude that cardiac pathology is the primary etiology of an increase in NT-proBNP level. For example, van Kimmenade et al proposed that an increased NT-proBNP level was predominantly related to, and a result of, the presence and extent of cardiac pathology rather than impaired renal clearance.Citation24 The current study showed that when eGFR was between 45–60 mL/minute/1.73 m2, the NT-proBNP level was most strongly dependent on cardiovascular diseases, such as CHF, AMI, and AF, as well as cardiac function (EF) rather than renal function, which was in agreement with previous reports. But when eGFR was < 45 mL/minute/1.73 m2, renal function was crucial for the change in the NT-proBNP level, rather than cardiac function and cardiovascular diseases.
Superior ability of NT-proBNP to detect CHF in CKD patients
Several studies have provided clear and convincing evidence of the diagnostic value of NT-proBNP for AHF,Citation1 but there was a lack of clear recommendations regarding its relationship with CHF and CKD. The issue of how to differentially interpret the CHF detecting utilities of the NT-proBNP level within the context of renal function has received considerable attention and has been tested in a small population but remains incompletely resolved from a clinical perspective.Citation7 When comparing the detecting ability of the NT-proBNP level in individuals with and without deteriorating renal function, previous studies reported that only mildly diminished accuracy was observed in renal disease as long as a modestly increased optimal cutoff value was used for NT-proBNP.Citation25 The current study, which focused on elderly patients with CAD, showed that the usefulness of NT-proBNP in detecting CHF in the presence of CKD might be improved to some extent rather than compromised after adopting a higher cutoff value.
Superior independent and compensated prognostic ability of NT-proBNP in CKD patients
NT-proBNP has been reported to be a significant predictor of mortality for cardiovascular diseases such as HF and CAD.Citation26,Citation27 The prognoses of CKD patients based on the NT-proBNP level have not been thoroughly studied; indeed, only small series have shown the ability of NT-proBNP to independently predict adverse outcomes.Citation8 Previous studies have shown that NT-proBNP provides independent and similar prognostic information in the entire CHF cohort, as well as in subgroups with and without CKD.Citation8,Citation9 Given the increasing number of patients affected by both CAD and CKD, the effect of CKD on the application of NT-proBNP in risk stratification of CAD patients is of particular importance. However, there has been no study definitively answering the question of whether or not the NT-proBNP level has an important prognostic role in the CAD population with and without CKD, especially in elderly patients. The current study confirmed the superior independent predictive performance of NT-proBNP in elderly CAD patients with CKD in comparison to patients without CKD. Moreover, when suitable cutoff points of NT-proBNP were used, low- and high-risk subpopulations could easily be identified in both patients with CKD and patients without CKD. Nevertheless, there was an obviously higher cutoff value in the CKD patients than in the non-CKD patients. Currently most institutions continue to use the NT-proBNP diagnostic and prognostic cutoff levels without taking renal function into account. Our data emphasizes that the cutoff values of NT-proBNP must be evaluated in conjunction with the overall status of patients, particularly the level of renal function. Additionally, the current study described the additive effects of NT-proBNP on CKD risk assessment models, ie, the compensated predictive ability of NT-proBNP.
The current study had several limitations. Firstly, due to the shortage of noninvasive methods and unified standards in evaluating blood volume, there was no other invasive data about blood volume except for blood pressure in our study. In addition, the sample size of our study is relatively small, and there is need of large studies to confirm our study results.
The following conclusions about elderly Chinese patients could been drawn from the current study: (1) a significantly and independently inverse association between NT-proBNP level and renal function was evident, with higher NT-proBNP level observed as eGFR declined; (2) NT-proBNP was shown to have a better ability to detect CHF and predict mortality in CKD patients than in non-CKD patients; (3) CKD patients had higher cutoff points for NT-proBNP in detecting CHF or predicting death than non-CKD patients; and (4) NT-proBNP added important information to CKD risk assessment models in patients with CAD.
Acknowledgment
This study was supported by the Central Health Special Foundation (grant number B2009B108) and The National Key Basic Research Project (973) (grant number CB517503) (Beijing, People’s Republic of China).
Disclosure
The authors report no conflicts of interest in this work.
References
- JanuzziJLJrCamargoCAAnwaruddinSThe N-terminal Pro- BNP Investigation of Dyspnea in the Emergency department (PRIDE) studyAm J Cardiol200595894895415820160
- AnavekarNSMcMurrayJJVelazquezEJRelation between renal dysfunction and cardiovascular outcomes after myocardial infarctionN Engl J Med2004351131285129515385655
- McAlisterFAEzekowitzJTonelliMArmstrongPWRenal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort studyCirculation200410981004100914769700
- DeFilippiCvan KimmenadeRRPintoYMAmino-terminal pro- B-type natriuretic peptide testing in renal diseaseAm J Cardiol20081013A828818243865
- VargheseKCherianGAbrahamUTHayatNJJohnyKVPredictors of coronary disease in patients with end stage renal diseaseRen Fail200123679780611777319
- BaigentCBurburyKWheelerDPremature cardiovascular disease in chronic renal failureLancet2000356922414715210963260
- GardnerRSChongKSO’MearaEJardineAFordIMcDonaghTARenal dysfunction, as measured by the modification of diet in renal disease equations, and outcome in patients with advanced heart failureEur Heart J200728243027303317967819
- BruchCFischerCSindermannJStypmannJBreithardtGGradausRComparison of the prognostic usefulness of n-terminal pro–brain natriuretic peptide in patients with heart failure with versus without chronic kidney diseaseAm J Cardiol2008102446947418678308
- HartmannFPackerMCoatsAJPrognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure: a substudy of the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) TrialCirculation2004110131780178615381643
- BraunwaldEAntmanEMBeasleyJWACC/AHA guidelines for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina)J Am Coll Cardiol2000363970106210987629
- RyanTJAntmanEMBrooksNH1999 Update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction)J Am Coll Cardiol199934389091110483976
- FoxKGarciaMAArdissinoDTask Force on the Management of Stable Angina Pectoris of the European Society of Cardiology; ESC Committee for Practice Guidelines (CPG)Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of CardiologyEur Heart J200627111341138116735367
- MaYCZuoLChenJHModified glomerular filtration rate estimating equation for Chinese patients with chronic kidney diseaseJ Am Soc Nephrol200617102937294416988059
- National Kidney FoundationK/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAm J Kidney Dis2002392 Suppl 1S1S26611904577
- FusterVRydénLECannomDSAmerican College of Cardiology/American Heart Association Task Force on Practice Guidelines; European Society of Cardiology Committee for Practice Guidelines; European Heart Rhythm Association; Heart Rhythm SocietyACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm SocietyCirculation20061147e257e35416908781
- DicksteinKCohen-SolalAFilippatosGESC Committee for Practice Guidelines (CPG)ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008Eur Heart J200829192388244218799522
- JohnsonESThorpMLYangXCharansonneyOLSmithDHPredicting renal replacement therapy and mortality in CKDAm J Kidney Dis200750455956517900455
- SPSS IncSPSS Missing Values™ 17.0ArmonkIBM Corporation2007
- RichardsMNichollsMGEspinerEAChristchurch Cardioendocrine Research Group; Australia-New Zealand Heart Failure GroupComparison of B-type natriuretic peptides for assessment of cardiac function and prognosis in table ischemic heart diseaseJ Am Coll Cardiol2006471526016386664
- GoeiDSchoutenOBoersmaEInfluence of renal function on the usefulness of N-terminal pro-B-type natriuretic peptide as a prognostic cardiac risk marker in patients undergoing noncardiac vascular surgeryAm J Cardiol2008101112212618157978
- PfisterRDiedrichsHSchiedermairAPrognostic impact of NT-proBNP and renal function in comparison to contemporary multimarker risk scores in heart failure patientsEur J Heart Fail200810331532018304872
- DasSRAbdullahSMLeonardDAssociation between renal function and circulating levels of natriuretic peptides (from the Dallas Heart Study)Am J Cardiol2008102101394139818993162
- HerrmannZUhlWSteinbergHWDworschackRThe influence of renal function on NT-proBNP levels in various disease groupsClin Lab20034911–1264965614651336
- van KimmenadeRRJanuzziJLJrBakkerJARenal clearance of B-type natriuretic peptide and amino terminal pro-B-type natriuretic peptide: a mechanistic study in hypertensive subjectsJ Am Coll Cardiol2009531088489019264247
- LeeJEChoiSYHuhWN-terminal pro-brain natriuretic peptide levels predict left ventricular systolic function in patients with chronic kidney diseaseJ Korean Med Sci200924Suppl 1S63S6819194564
- KragelundCGrønningBKøberLHildebrandtPSteffensenRN-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart diseaseN Engl J Med2005352766667515716560
- JamesSKLindahlBSiegbahnAN-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: a Global Utilization of Strategies To Open occluded arteries (GUSTO)-IV substudyCirculation2003108327528112847065