Abstract
Background
Falls are a significant issue in people with diabetic peripheral neuropathy. Balance interventions have been broadly administered in individuals with diabetic peripheral neuropathy, but the effects on static and dynamic balance in those who are at risk of falling have not yet been comprehensively reviewed.
Objective
To provide a synthesis of the literature regarding the effectiveness of physical rehabilitation interventions to improve balance in people with diabetic peripheral neuropathy who are at risk of falling.
Methods
Four databases (PubMed, Embase, the Cochrane Central Register of Controlled Trials, Cumulated Index in Nursing and Allied Health Literature) were systematically searched from inception to July 2022. Articles meeting the eligibility criteria (ie, participants with diabetic peripheral neuropathy and at risk of falling based on validated fall balance outcome risk cut off scores; inclusion of physical rehabilitation intervention) underwent a quality assessment using the Physiotherapy Evidence Database scale. Data regarding fall risk was extracted.
Results
Sixteen studies met the eligibility criteria. Participants in six studies improved balance such that their fall risk was reduced from a moderate-high risk of falls to no or low risk of falls from pre- to post-intervention. Interventions within these six studies were variable and included balance exercise, gait training, endurance, tai-chi with mental imagery, proprioceptive training, aerobic training, and yoga. Participants in seven of the remaining studies showed no improvement and participants in three studies showed mixed results regarding improved balance and reduced fall risk status by post-intervention.
Conclusion
While physical rehabilitation is sufficient to improve balance in individuals with diabetic peripheral neuropathy who are at risk of falling, few interventions led to improved balance and reduced fall risk. Interventions involving intentional weight shifting, manipulation of the base of support, and displacement of the center of mass such as tai-chi and yoga appear to provide the most consistent results in terms of decreasing fall risk. To better understand the effectiveness of rehabilitation on balance and fall risk, future studies should examine the impact of physical interventions on prospective fall rates.
Introduction
Diabetic peripheral neuropathy (DPN) is a common, chronic complication of diabetes that negatively impacts balance and gait.Citation1–3 Among neurological populations, people with peripheral neuropathy report the third highest rate of falls.Citation4 DPN results in loss of proprioception, cutaneous sensation, and muscle stretch reflexes in the lower limbs, which are essential for recognizing that balance has been perturbed and for triggering balance-correcting responses.Citation5,Citation6 Therefore, loss of these sensory functions results in delayed balance responses, increasing the risk of falls and fall-related injuries.Citation7–10 People with DPN are also 15 times more likely to report injury and feel significantly less safe during standing and walking compared to healthy age-matched controls.Citation11 Consequently, balance training and fall prevention are essential elements of any rehabilitation program for people with DPN.
To improve balance and reduce falls in people with DPN, several physical rehabilitative interventions have been investigated and reported beneficial effects on balance control. Such interventions include walking activities, balance training, strengthening, and aerobic exercise.Citation12–14 A 2011 review of physical therapy balance interventions in people with DPN concluded that interventions focusing on lower limb strengthening presented the greatest evidence for improvements in balance, with little evidence supporting the use of passive interventions such as vibrating insoles and monochromatic infrared energy.Citation14 However, the conclusions in this review were limited by the inclusion of lower quality studies owing to the lack of higher-level evidence available at the time. A subsequent review in 2014 determined that balance training was superior to strengthening or combined strength and endurance training with respect to improved balance in people with peripheral neuropathy.Citation13 However, the results of this review were not specific to DPN and included other causes of neuropathy. This is significant as the pattern of sensory loss differs depending on the cause. Therefore, the subsequent balance impairments may be different as well. A more recent review in 2017 investigating the effects of falls prevention exercises in muscle strength, balance, and fall risk factors determined that a focused multicomponent intervention is optimal for the improvement of gait, balance, and function in people with DPN.Citation12 Nevertheless, it is essential to note that in this review, half of the studies included participants with only minimally impaired balance at the start of the intervention, as indicated by balance test scores that were above validated fall risk cut-off scores. Understanding the effectiveness of interventions in individuals across the spectrum of balance impairment severity is crucial for informing tailored treatment approaches that cater to the diverse needs of the DPN population. In DPN, demands for sensory integration and motor planning during balance challenges are increased as sensory impairments worsen. Thus, it is critical to determine whether more impaired individuals with DPN can learn to draw upon and train these compensatory centrally driven mechanisms to improve balance to the extent that fall risk is reduced. Moreover, an understanding of whether fall prevention interventions lead to a reduction in prospective falls is lacking. Since there remains insufficient data regarding long term prospective fall rates following balance rehabilitation in DPN, established fall risk cut off scores based on validated balance outcomes may be used as a proxy for fall risk.
The objective of this systematic review was to provide a synthesis of the literature regarding the effectiveness of physical rehabilitation interventions to improve balance in people with DPN who are identified as being at risk of falling. Secondarily, we aimed to determine whether any improvements in balance also led to a reduction in fall risk based on validated fall risk cut off scores and minimal clinically important differences. Ultimately, advancing our understanding of effective rehabilitation strategies for DPN-specific impairments holds the potential to mitigate fall-related morbidity and enhance overall quality of life in this population.
Materials and Methods
Search Strategies
This systematic review was registered in the PROSPERO international prospective register of systematic reviews (ID: CRD42021245702). PubMed (1809-present), Embase (embase.com, 1974-present), Cochrane Central Register of Controlled Trials (Wiley), and CINAHL (EBSCO) were searched on February 26, 2022, by a qualified librarian. All searches were performed in English. A total of 2369 articles were retrieved from the database searches. Following the removal of duplicates, 1849 articles remained. Keywords included “peripheral neuropathy” or ‘peripheral nervous system disease’ or ‘peripheral nerve disease’ or “diabetic neuropathy” AND ‘fall’ or ‘balance’ or ‘postural stability’ or ‘postural control’ or ‘postural balance’ or ‘accidental falls’ AND ‘intervention’ or ‘rehabilitation’ or ‘physical therapy’ or ‘exercise’ or ‘exercise therapy’ or ‘exercise training’ or ‘program’ or ‘manage’ or ‘risk’ or ‘rate’ or ‘prevent’ or ‘reduce’.
Study Selection
The search strategy retrieved a total of 1605 articles from inception to July 2022 in PubMed, 671 in Embase, 162 from the Cochrane Central Register of Controlled Trials (Wiley), and 271 from CINAHL. All non-English manuscripts and duplicates were removed. Remaining articles then underwent screening and assessment for quality and eligibility.
Studies were assessed for eligibility by two independent reviewers (NA, KW) using the software Covidence. When these two reviewers were unable to reach a consensus, a third reviewer (LZ) was consulted. Studies were included in the review if they aimed to investigate the effects of a physical rehabilitation intervention on balance outcomes in people with DPN. Physical rehabilitation interventions were defined as any rehabilitation program involving active participation, such as balance activities, strengthening exercises, gait training, sensorimotor training, aerobic exercise, or tai chi. Studies involving passive (non-physical) rehabilitation, such as mental imagery, were only included if used in combination with physical rehabilitation. The outcome measures used in these studies must have had established fall risk cut-off scores. Fall risk cut-off scores were identified based upon previously published scores using balance outcome measures that are known to be valid and reliable in older adults and, if available, in people with DPN (see ). also includes the minimal clinically important difference (MCID: the minimal change in outcome scores necessary to produce a clinically meaningful improvement for a patient) for each of the included outcome measures (if available). Eligible studies included participants who were classified as being at risk for falls prior to the intervention according to the fall risk cut-off scores. In addition, study participants must have included adults with a medical diagnosis of both diabetes and sensory peripheral neuropathy of the lower limbs. Peripheral neuropathy was identified using one or more of the following criteria: reduced nerve conduction velocity, clinical neuropathy scales including the Michigan Neuropathy Screening Instrument and the modified Toronto Clinical Neuropathy Score, abnormal Semmes-Weinstein monofilaments examination, or increased vibration perception threshold.
Table 1 Fall Risk Cut-off Scores
Quality Assessment
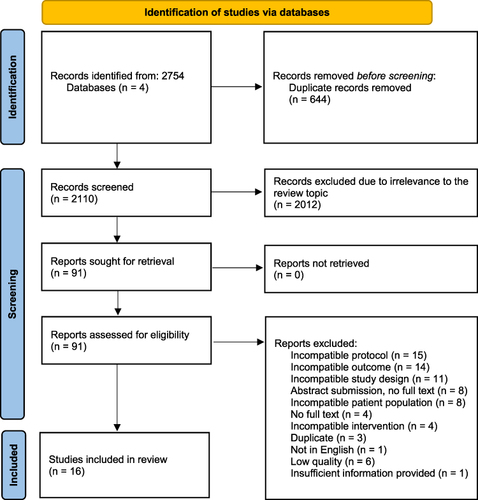
Two independent reviewers (NA, LZ) conducted a quality assessment of all eligible studies using the PEDro scale. When these two reviewers were unable to reach a consensus, a third reviewer (KW) was consulted. The PEDro scale includes 11 criteria designed to assess clinical trials for external validity (criterion 1), internal validity (criteria 2–9), and whether there is sufficient statistical information to make results interpretable (criteria 10–11).Citation19 A point was awarded for each criterion if that criterion was satisfied. The total score ranges from 0 to 11. Articles with a PEDro score of less than 4 or with insufficient details regarding the intervention were excluded from the review. The PRISMA flow diagram is depicted in .
Data Extraction
Data was manually extracted from all eligible articles by reviewer (NA). Data extracted included group means for fall-risk outcome measures with validated fall risk cut-off scores at two time points: pre-intervention and post-intervention. These fall risk outcome measures included one or more of the following measures: Berg Balance Scale, Functional Reach Test, Unilateral Stance Test, Timed Up and Go test, Dynamic Gait Index, Performance-Oriented Mobility Assessment, and Physiological Profile Approach. If any of the desired data was not provided in the article text, study investigators were contacted by (NA).
Results
Quality Assessment
The quality of the 16 included studies were assessed using the PEDro scale (). Total scores ranged from 1 to 10. Eleven of the 16 studies scored a total of 6 or above indicating moderate-to-high overall quality. All studies satisfied criterion 1 indicating good external validity. Some studies (12.5–81.3%) satisfied criteria 2–9 indicating poor-to-moderate internal validity. Most of the studies satisfied criteria 10 and 11 (87.5 and 100%, respectively) indicating sufficient statistical information to make their results interpretable. One study was excluded, despite scoring a 4 on the PEDro scale, due to insufficient details regarding the intervention.
Table 2 Quality Assessment
Types of Interventions
Physical rehabilitation interventions implemented in the included studies were balance training,Citation21–23,Citation25–27,Citation29,Citation30,Citation34,Citation35 sensorimotor training,Citation30 strength exercise,Citation22,Citation23,Citation26,Citation29,Citation30 gait training,Citation29,Citation30 Tai Chi,Citation24 yoga,Citation33,Citation35 aerobic training,Citation28 endurance training,Citation29 functional training,Citation29,Citation30 proprioceptive training,Citation20,Citation34 ball training,Citation32 and Frenkel exercise.Citation32 Four methods of passive rehabilitation (transcutaneous electrical nerve stimulation,Citation21 whole-body vibration,Citation27 mental imagery,Citation24 visual joint movement feedback)Citation36 were combined with physical rehabilitation in three of the included articles. Overall, the age range for participants with DPN in these intervention studies was 46–97 years old and the duration of interventions ranged from 2–12 weeks. Methods and results of all included studies are summarized in .
Table 3 Study Characteristics and Results
Table 4 Studies with Improved Fall Risk Status
Table 5 Studies Without Improved Fall Risk Status
Effects of Physical Rehabilitation Interventions on Prospective Falls
Few physical rehabilitation studies for people with DPN assessed prospective fall rates.Citation23,Citation37,Citation38 Most studies recorded retrospective falls history over a specified period at baseline to characterize the study population, but not prospectively.Citation21,Citation25,Citation27–31 One study instructed participants to report any falls that occurred throughout the intervention to monitor adverse events.Citation23
Effects of Physical Rehabilitation Interventions on Balance Outcomes
Effects on Static Balance Outcomes
The most common outcome measures of balance control used in physical rehabilitation studies in people with DPN were static outcome measures. The static balance outcome measures included postural stability measured as center of pressure (COP) sway displacement and velocity during quiet standingCitation27,Citation30 or under a combination of conditions (eyes openCitation24,Citation25,Citation28,Citation35 or closedCitation24,Citation25,Citation28,Citation35 on firmCitation24,Citation28 or foamCitation24,Citation28 surface), UST with eyes openCitation23–25,Citation27,Citation30,Citation32,Citation34,Citation35 and closed,Citation23–25,Citation27,Citation30,Citation32,Citation34,Citation35 tandem stance,Citation26 and some items of the BBS.Citation20,Citation21,Citation25,Citation27,Citation31–34
Most studies assessing static balance following a physical rehabilitation intervention in people with DPN found significant changes. One studyCitation25 included only balance training in the intervention and found reductions in anteroposterior and mediolateral sway in the eyes open and eyes closed conditions, increased UST time, improvements in the static items of the BBS. Four studies using both balance training and strength exerciseCitation22,Citation23,Citation26,Citation29 found increased UST time,Citation23,Citation26 improved BBS scores,Citation23 and increased time in tandem stance.Citation26 Studies using Tai Chi,Citation24 yoga,Citation33 or yogasanaCitation35 found increased UST time,Citation24,Citation35 reduced COP excursion,Citation35 and improved BBS scores.Citation33 Two studies used gait training in combination with balance trainingCitation29,Citation30 and with sensorimotor trainingCitation30 and found reduced overall postural sway,Citation29,Citation30 and increased UST time.Citation29,Citation30 One study used balance training in combination with stimulation therapyCitation21 and found improved BBS scores. One study using only proprioceptive trainingCitation20 found improved BBS scores. One study used only aerobic trainingCitation28 and found decreased sway in the mediolateral direction, with eyes open and on a firm surface. A study comparing ball training and Frenkel exerciseCitation32 found greater increase in UST time and improved BBS scores in the ball training group compared to the Frenkel exercise group.
Effects on Dynamic Balance Outcomes
Relatively few intervention studies for people with DPN have assessed dynamic balance. The dynamic balance outcome measures included in this review were the FRT,Citation24–27,Citation30 PPA,Citation28 TUG,Citation34 some items of the BBS,Citation20,Citation21,Citation23,Citation25,Citation27,Citation31–34 POMA,Citation22,Citation29 and DGI.Citation31
Most studies assessing dynamic balance following a physical rehabilitation intervention in people with DPN have reported significant changes. Studies that included only balance trainingCitation25 in the intervention found improvements in the dynamic items of the BBS and improved FRT distance. Four studies using both balance training and strength exerciseCitation22,Citation23,Citation26,Citation29 found improved POMA scores,Citation29 improved BBS scores,Citation23 and increased FRT distance.Citation26 Studies using Tai Chi,Citation24 yoga,Citation33 or yogasanaCitation35 found increased FRT distance,Citation24 improved SEBT,Citation35 and improved BBS scores.Citation33 Two studies used gait training in combination with balance trainingCitation29,Citation30 and with sensorimotor trainingCitation30 and found increased FRT distanceCitation30 and increased POMA scores.Citation29 One study used balance training in combination with stimulation therapyCitation21 and found improved BBS scores. One study using only proprioceptive trainingCitation20 found improved BBS scores and 6MWT distance. A study comparing ball training and Frenkel exerciseCitation32 found greater improvement in SEBT performance and improved BBS scores in the ball training group compared to the Frenkel exercise group. One study compared aquatic- and land-based rehabilitationCitation31 and found greater improvement in DGI in the aquatic group compared to land group.
One study assessing dynamic balance outcomes did not find any significant changes following the intervention (POMA).Citation22
Effects of Physical Rehabilitation Interventions on Fall Risk
Fall Risk Outcome Measures
The 16 included studies utilized a combined total of seven balance outcome measures with validated fall risk cut-off scores. Nine studies included the Berg Balance Scale (BBS).Citation20,Citation21,Citation23,Citation25,Citation27,Citation31–34 The BBS measures static and dynamic balance during 14 common tasks that are rated on a 5-point ordinal scale from 0 (lowest level of function) to 4 (highest level of function). The BBS has an MCID of 11.5.Citation39 Nine studies included unilateral stance time UST,Citation23–27,Citation30,Citation32,Citation34,Citation35 which measures unipedal static balance with eyes open. The UST has no known MCID. Five studies reported results from the Functional Reach Test (FRT),Citation24–27,Citation30 which measures anticipatory and dynamic balance. Participants are instructed to reach forward as far as they can without taking a step and the distance from the initial to end reach position is measured. The FRT has no known MCID. Two studies reported the Performance Oriented Mobility Assessment (POMA).Citation22,Citation29 The POMA, also called the Tinetti test, is a task-oriented 16 item test that measures balance and gait and is scored on a 3-point ordinal scale from 0 (high level of impairment) to 2 (independent). The POMA has no known MCID. Only one study included the Physiological Profile Assessment (PPA),Citation28 which is a fall risk assessment tool. The PPA includes measures of vision, peripheral sensation, muscle force, reaction time, and postural sway. The PPA has no known MCID. Only one study included the Dynamic Gait Index (DGI),Citation24 which assesses gait and balance while walking in the presence of external demands such as changing speeds and head turns. The DGI has an MCID of 1.9.Citation40 Five studies included the Timed Up and Go Test (TUG),Citation21,Citation25,Citation27,Citation30,Citation34 which involves timing the participant as they stand up from an armless chair, walk 3 meters, turn, walk back to the chair, and sit down. The TUG has an MCID of (0.8–3.4).Citation41,Citation42
Changes in Fall Risk
Results of the 16 included studies were examined for changes in fall risk status (ie, transitioned from being at fall risk to not at fall risk) resulting from the intervention and according to validated cut-off scores ().Citation20–35 We used the mean scores for each fall risk outcome at baseline and post-intervention testing since individual participant values were not always available.
Six of the 16 included studies reported improvement in fall risk status, changing from at risk of falls to not at risk of falls, following the intervention (). Within these studies, fall risk cut off scores were taken from the UST,Citation24,Citation34,Citation35 TUG,Citation34 BBS,Citation33,Citation34 FRT,Citation24 PPA,Citation28 POMA,Citation29 and DGI.Citation31 The interventions implemented in these studies included balance, gait, functional strength, endurance, tai chi with mental imagery, proprioceptive training, yogasana, aerobic training, and yoga and relaxation. Durations of these interventions were 8Citation24,Citation33 and 12Citation28,Citation29,Citation35 weeks.
Seven of the 16 studies did not report change in fall risk status by post-intervention (). Within these seven studies, fall risk cut off scores were taken from UST,Citation23,Citation26,Citation32 BBS,Citation20,Citation23,Citation31,Citation32 FRT,Citation26 TUG,Citation21 POMA,Citation22 and DGI.Citation31 Types of interventions implemented in these studies included proprioceptive training, sensorimotor training, balance, gait, postural stability training with TENS and infrared therapy, walking, ball training, and Frenkel training. Durations of these interventions were 3,Citation21,Citation26,Citation32 4 weeks,Citation22,Citation31 8,Citation20 and 12 months.Citation23
Three of the 16 included studies reported conflicting results regarding whether fall risk status improved following the intervention due to different outcome measures used within each study ().Citation25,Citation30 All three studies included UST and TUG,Citation25,Citation27,Citation30 with the TUG added in two of the studies.Citation25,Citation27 The interventions implemented in these studies included sensorimotor, balance, core, and gait training. The durations of these interventions were 6Citation27 and 8 weeks.Citation25,Citation30
Table 6 Studies with Mixed Results Regarding Fall Risk Status
Of the studies in this review reporting outcome scores that improved from below to above the fall risk cut off, only three reported a score increase that was greater than their respective MCID values. These three studies included the TUG and BBS. The interventions implemented in these studies included proprioceptive training,Citation34 sensorimotor training,Citation30 and balance training.Citation25
Discussion
This review summarizes the results from 16 physical rehabilitation studies that included people with DPN who were at risk of falls at baseline based on established fall risk cut off scores. Overall, although physical rehabilitation interventions found improvements in balance outcomes, it is less clear whether they are reducing fall risk. None of the included studies assessed prospective fall rates following physical rehabilitation interventions in people with DPN.
Using the established fall risk cut-off scores of included balance outcome measures, only six of the 16 studies led to an improvement in fall risk status post-intervention.Citation24,Citation28,Citation29,Citation33–35 Seven of the 16 studies failed to result in a change in fall risk status post-intervention,Citation20–23,Citation26,Citation31,Citation32 and three studies demonstrated variability in fall risk status change.Citation25,Citation27,Citation30 The lack of change in fall risk status in most of these studies may primarily be explained by differences in balance outcome measures as well as the type and dosage of physical rehabilitation interventions of the included studies.
Balance Outcome Measures
Interestingly, five of the seven outcomes within the studies included in this review were common among studies in which a reduction in fall risk was identified () and was not identified (). This discrepancy may be due, at least in part, to the fall risk sensitivity and specificity for each outcome and whether these values have been specifically tested in a DPN population. It may be argued that the results of were more dependent on the specificity by which fall risk cut off scores can accurately rule out the participants who were not at risk of falls following the intervention. Of the outcomes included in the six studies resulting in a reduction in fall risk, specificity ranged from 65.4–88.5%, suggesting that there may have been up to 35% of the study participants who remained at risk of falls following the intervention. In contrast, the results of may be more dependent on the sensitivity by which participants who remained at risk for falls could be accurately identified. Of the outcomes included in the seven studies in , the fall risk sensitivity ranged from 70–91%, suggesting that up to 30% of the study participants had improved their fall risk status. The range of fall risk specificity and sensitivity may also explain the within study discrepancy of results noted in . Moreover, only four of the seven reported outcomes have been validated for fall risk cut off scores in a population with DPN. Although UST, POMA, and PPA have been validated in an older adult population at risk of falling, specific fall risk cut off scores for DPN have not yet been established. To our knowledge, there are no studies that validate and compare the psychometric properties and sensitivity and specificity of fall risk cut off scores across balance outcome measures in people with DPN. Therefore, it is difficult to ascertain which of the outcome measures included in the studies of this review are optimal measures of fall risk in this population.
Differences in the test items included in the outcome measures included in this review should also be considered in light of the discrepancies of our results. For example, the UST and FRT are single-task tests that rely chiefly on feet in place balance strategies. On the other hand, the BBS measures a series of static and dynamic balance tasks but does not address balance while walking. Given that the conditions under which people with peripheral neuropathy most often fall include walking over irregular (67.1%) or slick (11.8%) surfaces,Citation43 outcome measures that include walking assessments such as the TUG, DGI, and POMA may be better options for the assessment of fall risk in people with DPN. People with peripheral neuropathy also commonly fall while turning and reaching beyond the base of support (22.5%).Citation43 Of the outcome measures included in this review, only the BBS, TUG, POMA, and DGI included turning assessments.
Another point of consideration is the presence of floor or ceiling effects among the reported outcome measures. Ceiling effects have been documented among older adults in the BBS,Citation40 UST,Citation44 POMA,Citation40 and DGI.Citation40 Floor effects have been documented among older adults in the TUG.Citation45 Therefore, in this review, relatively younger participants with less severe impairments may not be sufficiently challenged during the balance assessment tasks, resulting in a ceiling effect. In contrast, participants who were more severely impaired may have been unable to perform many of the tasks, resulting in a floor effect. To account for floor and ceiling effects, we included all fall risk assessments used in each of the studies. This allows for the consideration of other scales used in the same study which can corroborate any fall risk improvement or lack thereof. We also included outcomes with continuous measurements, such as the PPA and FRT, which avoid floor and ceiling effects. Moreover, it should be noted that even though six of the 16 included studies reported improvement in fall risk status from at risk of falls to not at risk of falls, only three of these six studies also reached MCID values.
Differences in Rehabilitation Interventions
Balance training was included in most of the included studies, but only one of these studies resulted in reduced fall riskCitation29 and three others reported conflicting results.Citation25,Citation27,Citation30 There are several possible explanations for the lack of fall risk reduction in these studies. First, the intensity of the intervention, either duration, frequency, or a combination of these exercise dosage parameters, may not have been sufficient to produce significant changes. The one study that resulted in reduced fall risk had a longer intervention duration than the others (ie, 12 weeks vs 6 or 8 weeks). Second, some studies only included static balance training, which may not be as effective as dynamic or walking balance interventions in reducing fall risk. Third, it is possible that balance interventions alone are not capable of reducing fall risk in individuals with DPN and that balance training needs to be combined with other related interventions. A recent meta-analysis comparing the effectiveness of different exercise interventions in reducing falls in healthy older adultsCitation46 found that the greatest reduction in numbers of fallers occurred with exercise combinations that included four components of balance (anticipatory control, dynamic stability, functional stability limits, and reactive control) and flexibility. People with DPN typically experience somatosensory loss beginning in the distal lower limbs, resulting in reduced feedback control.Citation7 It is possible that multiple domains of balance need be trained as a comprehensive training protocol to effectively target the deficits caused by sensory loss and the integration of residual sensory systems.
Three studies included training that involved mindful whole-body motions (Tai Chi, yoga, and yogasana).Citation24,Citation33,Citation35 All three of these studies improved balance as well as improvements in fall risk status from at-risk to not-at-risk in all included balance assessments. These studies involved intentional weight shifting, base of support manipulation, and center of mass displacement. Such movements place a high demand on balance control and whole-body awareness, which may explain the consistent balance and fall risk improvement shown in all the included studies that involved this type of intervention. However, these results should be interpreted with caution as these three studies received lower quality assessment scores.
Two studies included gait training, both of which showed improvements in balance, however, only one resulted in reduced fall riskCitation29 and the other produced contradictory results.Citation30 Gait training was combined with strength and balance training in both studies with the addition of sensorimotor training in one of these studies.Citation30 In addition, the study that resulted in reduced fall risk had a longer intervention duration. Given that most falls in people with peripheral neuropathy occur while walking, it is plausible that a fall prevention program including interventions aimed at improving balance control while walking may have greater potential for reducing falls in people with DPN.Citation43,Citation47
People with DPN typically experience somatosensory loss resulting in reduced feedback control.Citation7 To date, all physical rehabilitation interventions in people with DPN have focused on training and exercises aimed at improving feedforward (ie, anticipatory) control. An intervention aimed at improving feedback (ie, reactive) rather than feedforward balance control may potentially have a greater impact on balance and fall risk in people with DPN. Reactive balance training has proven effective in reducing falls in other populations.Citation48,Citation49 To our knowledge, no previous studies have examined the effects of a reactive balance training intervention on balance or falls in people with DPN.
The physical rehabilitation interventions included in this review were highly variable regarding the type, duration, intensity, and frequency of training. The included studies used a total of fourteen different types of physical rehabilitation interventions with durations ranging from two weeks to twelve months and frequencies of daily to twice weekly sessions. However, there were a few intervention types in common between the studies that resulted in improved fall status.
Limitations
There are several Limitations of this review that should be mentioned. First, many studies included a relatively wide age range, including middle aged and older adults, but not all controlled for age-related differences in balance control when analyzing and reporting their results. Consequentially, it was not always clear whether reduced fall risk, or lack thereof, is due to age-related or DPN-related physiological changes. Second, there was high variability in severity of DPN among participants, intervention type, intensity, frequency, and duration, as well as outcome measures and the instruments and analysis methods used to measure them, which may limit generalizability of some results. Third, it is important to note that to definitively declare that fall risk has improved would require that the individual studies complete a long-term follow-up with their participants to determine whether they have experienced any new falls. There is currently a paucity of physical rehabilitation training studies in people with peripheral neuropathy, which have prospectively followed up with their participants. In this review, we used the information available to us to infer the effects of the included interventions on fall risk. Finally, many of the interventions were conducted as a pre-post single cohort study. As a result, these studies received low PEDro scores for items concerning between group differences, blinding, and randomization. Single group design increases the risk for bias and makes it difficult to determine if any improvements in outcomes are due to the intervention or another factor that may not have been considered or controlled. Future studies should improve quality where possible by utilizing randomized controlled trial design, blinding assessors, and providing clear and detailed results.
Conclusions
Although physical rehabilitation interventions have been found to improve walking speed, strength, and other static and dynamic balance tests, the effect on fall risk and prospective fall rates remains unclear. Regarding the clinical implications of this review, the intervention types that consistently resulted in reduced fall risk were interventions such as Tai Chi and yoga, which require intentional weight shifting, base of support manipulation, and center of mass displacement. In addition, clinicians should consider the psychometric properties of fall risk assessments, as well as the ceiling and floor effects, when deciding which clinical balance measures to use to determine whether improvements in fall risk have been achieved. Future studies should explore the long-term effects of physical rehabilitation interventions on prospective fall rates. In addition, future studies should carefully consider the properties and design of their chosen outcome measures when assessing fall risk in people with DPN.
Disclosure
The authors report no conflicts of interest in this work.
References
- Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. 2012;11(6):521–534. doi:10.1016/S1474-4422(12)70065-0
- Allen MD, Doherty TJ, Rice CL, Kimpinski K. Physiology in medicine: neuromuscular consequences of diabetic neuropathy. J Appl Physiol. 2016;121(1):1–6. doi:10.1152/japplphysiol.00733.2015
- Rosenblatt NJ, Young J, Andersen R, Wu SC, Crews RT. Diabetes and reactive balance: quantifying stepping thresholds with a simple spring scale to measure fall-risk in ambulatory older adults. J Diabetes Sci Technol. 2021;15(6):1352–1360. doi:10.1177/1932296820979970
- Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G. Falls in frequent neurological diseases: prevalence, risk factors and aetiology. J Neurol. 2004;251(1):79–84. doi:10.1007/s00415-004-0276-8
- London ZN. A structured approach to the diagnosis of peripheral nervous system disorders. Continuum (Minneap Minn). 2020;26:1130–1160. doi:10.1212/CON.0000000000000922
- Ito T, Sakai Y, Kubo A, et al. The relationship between physical function and postural sway during local vibratory stimulation of middle-aged people in the standing position. J Phys Ther Sci. 2014;26(10):1627. doi:10.1589/JPTS.26.1627
- Bloem BR, Allum JHJ, Carpenter MG, Honegger F. Is lower leg proprioception essential for triggering human automatic postural responses? Exp Brain Res. 2000;130(3):375–391. doi:10.1007/s002219900259
- Inglis JT, Horak FB, Shupert CL, Jones-Rycewicz C. The importance of somatosensory information in triggering and scaling automatic postural responses in humans. Exp Brain Res. 1994;101(1):159–164. doi:10.1007/BF00243226
- Henry M, Baudry S. Age-related changes in leg proprioception: implications for postural control. J Neurophysiol. 2019;122(2):525–538. doi:10.1152/JN.00067.2019
- Toosizadeh N, Wahlert G, Fain M, Mohler J. The effect of vibratory stimulation on the timed-up-and-go mobility test: a pilot study for sensory-related fall risk assessment. Physiol Res. 2020;69:721–730. doi:10.33549/PHYSIOLRES.934451
- Cavanagh PR, Derr JA, Ulbrecht JS, Maser RE, Orchard TJ. Problems with gait and posture in neuropathic patients with insulin‐dependent diabetes mellitus. Diabetic Med. 1992;9(5):469–474. doi:10.1111/j.1464-5491.1992.tb01819.x
- Gu Y, Dennis SM. Are falls prevention programs effective at reducing the risk factors for falls in people with type-2 diabetes mellitus and peripheral neuropathy: a systematic review with narrative synthesis. J Diabetes Complications. 2017;31(2):504–516. doi:10.1016/j.jdiacomp.2016.10.004
- Streckmann F, Zopf EM, Lehmann HC, et al. Exercise intervention studies in patients with peripheral neuropathy: a systematic review. Sports Med. 2014;44(9):1289–1304. doi:10.1007/s40279-014-0207-5
- Ites KI, Anderson EJ, Cahill ML, Kearney JA, Post EC, Gilchrist LS. Balance interventions for diabetic peripheral neuropathy: a systematic review. J Geriatric PhysTher. 2011;34(3):109–116. doi:10.1519/JPT.0b013e318212659a
- Jernigan SD, Pohl PS, Mahnken JD, Kluding PM. Diagnostic accuracy of fall risk assessment tools in people with diabetic peripheral neuropathy. Phys Ther. 2012;92(11):1461. doi:10.2522/PTJ.20120070
- Hurvitz EA, Richardson JK, Werner RA, Ruhl AM, Dixon MR. Unipedal stance testing as an indicator of fall risk among older outpatients matic. Arch Phys Med Rehabil. 2000;81(5):587–591. doi:10.1053/mr.2000.6293
- Tinetti ME. Performance‐oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119–126. doi:10.1111/j.1532-5415.1986.tb05480.x
- Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther. 2003;83(3):237–252. doi:10.1093/ptj/83.3.237
- de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. doi:10.1016/S0004-9514(09)70043-1
- Abdelbasset WK, Alrawaili SM, Nambi G, Yassen E, Moawd SA, Ahmed AS. Therapeutic effects of proprioceptive exercise on functional capacity, anxiety, and depression in patients with diabetic neuropathy: a 2-month prospective study. Clin Rheumatol. 2020;39(10):3091–3097. doi:10.1007/s10067-020-05086-4
- Eftekhar-Sadat B, Azizi R, Aliasgharzadeh A, Toopchizadeh V, Ghojazadeh M. Effect of balance training with Biodex Stability System on balance in diabetic neuropathy. Ther Adv Endocrinol Metab. 2015;6(5):233–240. doi:10.1177/2042018815595566
- Taveggia G, Villafañe JH, Vavassori F, Lecchi C, Borboni A, Negrini S. Multimodal treatment of distal sensorimotor polyneuropathy in diabetic patients: a randomized clinical trial. J Manipulative Physiol Ther. 2014;37(4):242–252. doi:10.1016/j.jmpt.2013.09.007
- Kruse RL, LeMaster JW, Madsen RW. Fall and balance outcomes after an intervention to promote leg strength, balance, and walking in people with diabetic peripheral neuropathy: “feet first” randomized controlled trial. Phys Ther. 2010;90(11):1568–1579. doi:10.2522/ptj.20090362
- Alsubiheen A, Petrofsky J, Daher N, Lohman E, Balbas E. Effect of Tai Chi exercise combined with mental imagery theory in improving balance in a diabetic and elderly population. Med Sci Monit. 2015;21:3054–3061. doi:10.12659/MSM.894243
- Song CH, Petrofsky JS, Lee SW, Lee KJ, Yim JE. Effects of an exercise program on balance and trunk proprioception in older adults with diabetic neuropathies. Diabetes Technol Ther. 2011;13(8):803–811. doi:10.1089/dia.2011.0036
- Richardson JK, Sandman D, Vela S. A focused exercise regimen improves clinical measures of balance in patients with peripheral neuropathy. Arch Phys Med Rehabil. 2001;82(2):205–209. doi:10.1053/apmr.2001.19742
- Lee K, Lee S, Song C. Whole-body vibration training improves balance, muscle strength and glycosylated hemoglobin in elderly patients with diabetic neuropathy. Tohoku J Exp Med. 2013;231(4):305–314. doi:10.1620/tjem.231.305
- Morrison S, Colberg SR, Parson HK, Vinik AI. Exercise improves gait, reaction time and postural stability in older adults with type 2 diabetes and neuropathy. J Diabetes Complications. 2014;28(5):715–722. doi:10.1016/j.jdiacomp.2014.04.007
- Allet L, Armand S, De Bie RA, et al. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia. 2010;53(3):458–466. doi:10.1007/s00125-009-1592-4
- Ahmad I, Noohu MM, Verma S, Singla D, Hussain ME. Effect of sensorimotor training on balance measures and proprioception among middle and older age adults with diabetic peripheral neuropathy. Gait Posture. 2019;74:114–120. doi:10.1016/j.gaitpost.2019.08.018
- Zivi I, Maffia S, Ferrari V, et al. Effectiveness of aquatic versus land physiotherapy in the treatment of peripheral neuropathies: a randomized controlled trial. Clin Rehabil. 2018;32(5):663–670. doi:10.1177/0269215517746716
- Rojhani-Shirazi Z, Barzintaj F, Salimifard MR. Comparison the effects of two types of therapeutic exercises Frenkele vs. Swiss ball on the clinical balance measures in patients with type II diabetic neuropathy. Diabetes Metab Syndr. 2017;11:S29–S32. doi:10.1016/j.dsx.2016.08.020
- Willis Boslego LA, Munterfering Phillips CE, Atler KE, Tracy BL, Van Puymbroeck M, Schmid AA. Impact of yoga on balance, balance confidence and occupational performance for adults with diabetic peripheral neuropathy: a pilot study. Br J Occup Ther. 2017;80(3):155–162. doi:10.1177/0308022616680364
- Iram H, Kashif M, Hassan HMJ, Bunyad S, Asghar S. Effects of proprioception training programme on balance among patients with diabetic neuropathy: a quasi-experimental trial. J Pak Med Assoc. 2021;71(7):1818–1821. doi:10.47391/JPMA.286
- Kanjirathingal J, Mullerpatan R, Nehete G, Raghuram N. Effect of yogasana intervention on standing balance performance among people with diabetic peripheral neuropathy: a pilot study. Int J Yoga. 2021;14(1):60. doi:10.4103/IJOY.IJOY_75_20
- Grewal GS, Schwenk M, Lee-Eng J, et al. Sensor-Based interactive balance training with visual joint movement feedback for improving postural stability in diabetics with peripheral neuropathy: a randomized controlled trial. Gerontology. 2015;61(6):567–574. doi:10.1159/000371846
- Kochman AB. Monochromatic infrared photo energy and physical therapy for peripheral neuropathy: influence on sensation, balance, and falls. J Geriatric PhysTher. 2004;27(1):18–21. doi:10.1519/00139143-200404000-00003
- Venkataraman K, Tai BC, Khoo EYH, et al. Short-term strength and balance training does not improve quality of life but improves functional status in individuals with diabetic peripheral neuropathy: a randomised controlled trial. Diabetologia. 2019;62(12):2200–2210. doi:10.1007/s00125-019-04979-7
- Tamura S, Miyata K, Kobayashi S, Takeda R, Iwamoto H. Minimal clinically important difference of the berg balance scale score in older adults with Hip fractures. Disabil Rehabil. 2022;44(21):6432–6437. doi:10.1080/09638288.2021.1962993
- Pardasaney PK, Latham NK, Jette AM, et al. Sensitivity to change and responsiveness of four balance measures for community-dwelling older adults. Phys Ther. 2012;92(3):388–397. doi:10.2522/PTJ.20100398
- Wright AA, Cook CE, Baxter GD, Dockerty JD, Abbott JH. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with Hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41(5):319–327. doi:10.2519/JOSPT.2011.3515
- Gautschi OP, Stienen MN, Corniola MV, et al. Assessment of the minimum clinically important difference in the timed up and go test after surgery for lumbar degenerative disc disease. Neurosurgery. 2017;80(3):380–385. doi:10.1227/NEU.0000000000001320
- DeMott TK, Richardson JK, Thies SB, Ashton-Miller JA. Falls and gait characteristics among older persons with peripheral neuropathy. Am J Phys Med Rehabil. 2007;86(2):125–132. doi:10.1097/PHM.0b013e31802ee1d1
- Choi YM, Dobson F, Martin J, Bennell KL, Hinman RS. Interrater and intrarater reliability of common clinical standing balance tests for people with hip osteoarthritis. Phys Ther. 2014;94(5):696–704. doi:10.2522/PTJ.20130266
- Rockwood K, Awalt E, Carver D, MacKnight C. Feasibility and measurement properties of the functional reach and the timed up and go tests in the Canadian study of health and aging. J Gerontol a Biol Sci Med Sci. 2000;55. Doi:10.1093/GERONA/55.2.M70.
- Sibley KM, Thomas SM, Veroniki AA, et al. Comparative effectiveness of exercise interventions for preventing falls in older adults: a secondary analysis of a systematic review with network meta-analysis. Exp Gerontol. 2021;143:111151. doi:10.1016/J.EXGER.2020.111151
- Richardson JK, Ching C, Hurvitz EA. The Relationship between electromyographically documented peripheral neuropatny and falls. J Am Geriatr Soc. 1992;40(10):1008–1012. doi:10.1111/j.1532-5415.1992.tb04477.x
- Dusane S, Bhatt T. Mixed slip-trip perturbation training for improving reactive responses in people with chronic stroke. J Neurophysiol. 2020;124(1):20–31. doi:10.1152/jn.00671.2019
- Lee A, Bhatt T, Liu X, Wang Y, Wang S, Pai YC. Can treadmill slip-perturbation training reduce longer-term fall risk upon overground slip exposure? J Appl Biomech. 2020;36(5):298–306. doi:10.1123/JAB.2019-0211