Abstract
Background
Pulmonary embolism (PE) can be an acute, life-threatening emergency, and studies suggest that advanced age is a risk factor for this condition. However, the literature is scarce regarding PE in patients above the age of 90 years. This study examined the relative risk for PE in the very elderly (>90 years) compared with that in the elderly (80–89 years).
Methods
A retrospective study was performed examining very elderly patients diagnosed with PE in the Department of Internal Medicine at the University Hospital Homburg/Saar in Germany between 2004 and 2012. Elderly patients (aged 80–89 years) diagnosed with PE served as controls. PE was confirmed by contrast-enhanced chest computed tomography or ventilation perfusion scintigraphy in both groups. A total of 2230 patients were examined for PE in this study. Of these, 15 (0.67%) in the study group and 197 (8.83%) in the control group underwent further evaluation for PE.
Results
After performing a radiological examination, 11 (73.3%, including six [54.55%] women) of the 15 study patients (mean age 91.6 ± 1.67 years) and 148 (75.1%, including 93 [62.84%] women) of the 197 controls (mean age 84.0 ± 2.59 years) were confirmed to have PE. There was a significantly lower proportion of the very elderly enrolled in the study (P < 0.001). There were no significant differences in clinical presentation, cardiovascular risk factors, electrocardiograms, blood gas analyses, radiological diagnoses, or acute comorbidities between the groups. However, the very elderly were more likely to experience minor bleeding in the extremities (P = 0.016) and to have more chronic diseases (P < 0.001). An increased relative risk of PE was not detected in the very elderly (relative risk 0.98, P = 0.88). Furthermore, D-dimer, troponin T, and high-sensitive troponin T levels had limited predictive value for PE in the very elderly. There were no significant differences in the number of hospital admissions, intensive care or ward treatments, or duration of hospitalization.
Conclusion
The relative risk for PE in the very elderly is not higher than that in the elderly.
Introduction
Pulmonary embolism (PE) occurs when the main pulmonary artery or one of its branches suddenly closes due to the presence of a thrombus deported from elsewhere in the body, usually the deep veins of the leg.Citation1 A small proportion of PEs are caused by fat, air, bone marrow, amniotic fluid, or septic substances.Citation1 If not quickly treated, PE can be life-threatening.Citation2 After myocardial infarction and cerebrovascular disease, PE is the third leading cause of death.Citation3 Unfortunately, it is also among the least accurately diagnosed acute emergency diseases.Citation3
The incidence of PE rises significantly with age, according to some hypotheses from recent studies.Citation2 In the elderly, diagnosing PE can be difficult due to the extensive number of cardiopulmonary conditions that may mimic the clinical presentation of PE in this population.Citation2 Diagnosis of PE relies on clinical likelihood, serum D-dimer levels, compression ultrasonography of the lower limb, ventilationperfusion lung scans, and/or helical computed tomography (CT).Citation2 Pulmonary angiography is seldom required because noninvasive diagnostic tests are generally sufficient.Citation2 Further, age can affect and confound the diagnostic tests for PE.Citation2 With increasing age, the predictive values of D-dimer and ventilation-perfusion lung scan are reduced.Citation2 Exclusion of PE in patients older than 80 years by assessment of the D-dimer level is possible in only 5% of patients.Citation2 However, age has no effect on the diagnostic precision of lower limb compression ultrasonography and helical CT.Citation2 Therefore, a rational diagnostic approach to PE in the elderly should rely mainly on investigations that are meaningful and have both high sensitivity and specificity.Citation2
The objective of this study was to compare the clinical presentation, cardiovascular risk factors, acute and chronic comorbidities, electrocardiographic changes, blood gas analyses, and radiologic imaging studies between the very elderly (aged >90 years) and elderly (aged 80–89 years) with a diagnosis of PE. This investigation was designed to acquire new insights into the accurate and prompt diagnosis of this acute emergency disease. Specifically, we examined whether there is an increased risk of PE in the very elderly population; whether the very elderly demonstrate an increased number of PEs; and whether PE diagnoses in the very elderly population can be made based on clinical symptoms, D-dimer values, electrocardiographic changes, blood gas analyses, and radiologic imaging.
Materials and methods
Patients
A retrospective study was performed using the medical records of patients treated for PE at the Department of Internal Medicine of the University Hospital Homburg/Saar in Germany between 2004 and 2012. The highest possible decade of life was used in this study, with the assumption that the highest life expectancy is, on average, 100 years of age. The two possible last decades of highest life used for comparison were close together to prevent any distortion in the data analysis due to age. Therefore, the study population was comprised of very elderly (aged >90 years) patients diagnosed with PE, and the controls were elderly patients (aged 80–89 years) with PE. The relative risk of developing PE was assessed as a ratio of the probability of PE occurring to the probability of PE not occurring among patients in both groups. Clinical symptoms of PE considered were dyspnea, chest pain, cough, hemoptysis, tachypnea, jugular venous distension, cyanosis, hypotension, and shock. The diagnosis of PE was made according to the latest edition of the International Classification of Disease (ICD I26.0–I26.9) from 2004 to 2012. PE was further defined as central or peripheral, depending on the location or arterial branch involved. Central vascular zones included the main pulmonary artery, the left and right main pulmonary arteries, the anterior trunk, the right and left interlobar arteries, the left upper lobe trunk, the right middle lobe artery, and the right and left lower lobe arteries. Peripheral vascular zones comprised the segmental and subsegmental arteries. A PE was considered massive when it involved both pulmonary arteries or resulted in hemodynamic compromise.
Clinical presentation of the patients in the emergency room was determined upon admission or hospital transfer. Acute and chronic comorbidities considered included cardiovascular, pulmonary, gastrointestinal tract, renal, urogenital, gynecological, neurological, psychiatric, orthopedic, dermatological, and allergic diseases. Plasma D-dimer concentrations were measured in citrated blood (1 + 10 mixture of 3.5% aqueous sodium citrate and blood; Sarstedt, Nümbrecht, Germany) using a well validated, commercial, particle-enhanced, immunoturbidimetric assay (Innovance® D-dimer, Siemens Medical Solutions, Erlangen, Germany) with the Behring Coagulation System analyzer (Dade Behring, Marburg, Germany). Highly sensitive troponin T levels were measured using the Elecsys® troponin T electrochemiluminescence immunoassay (fourth-generation) with the Roche Elecsys 2010 analyzer (Hoffman-La Roche Ltd, Mannheim, Germany). In addition to highly sensitive troponin T levels, conventional troponin T levels (Stat T, Roche Diagnostics, Mannheim, Germany) were measured using an electrochemiluminescence immunoassay (third-generation) on an Elecsys 2010 platform (Roche). D-dimer, troponin T, and highly sensitive troponin T were ordered as necessary (normal <0.5 mg/L, <0.10 ng/mL, <50 pg/mL, respectively). The 12-lead electrocardiogram was evaluated for sinus rhythm, atrial fibrillation, and tachyarrhythmia absolute in atrial fibrillation, T negativity, and S1Q3 changes suggestive of PE. Arterial or venous blood gas analyses were performed as soon as possible to support an early diagnosis of PE. Lower limb ultrasonography was used to detect deep venous thrombosis as a possible etiology for PE. Contrast-enhanced chest CT and/or ventilation perfusion scintigraphy were used to confirm the diagnoses of PE in each group. The presence of cor pulmonale with PE was determined using echocardiography in all patients.
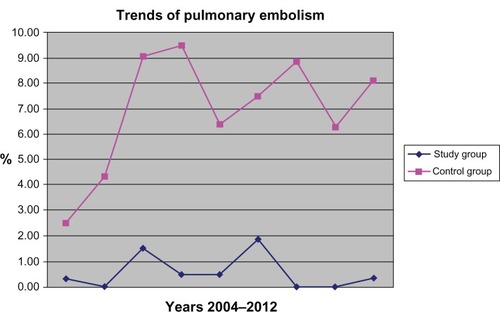
The medical treatment of both groups was also compared, along with hospital admissions, number of treatments in intensive care or general wards, and length of hospitalization. Numerical trends for PE in recent years were examined for both groups. Finally, the number of reanimations and autopsies as well as the mortality rate were calculated for both groups. Due to the retrospective nature of the study protocol, the Medical Association of Saarland’s Institutional Review Board waived the need for informed consent.
Statistical analysis
Relative risk and 95% confidence intervals (CIs) were calculated and compared between the very elderly and the elderly. The chi-square test was used to compare any differences in gender, clinical presentation, cardiovascular risk factors, acute and chronic comorbidities, D-dimer values, troponin T, high sensitive troponin T, electrocardiogram, hospital admissions, number of intensive care or ward treatments, recurrent PE, recurrent deep vein thrombosis, and location of PE (central versus peripheral). The Mann–Whitney test was used to calculate the differences in age, duration of hospitalization, D-dimer levels, and total chronic disease profiles. All results are expressed as the mean and standard deviation. Survival rates for both groups were calculated using the Kaplan–Meier method. P < 0.05 was considered to be statistically significant.
Results
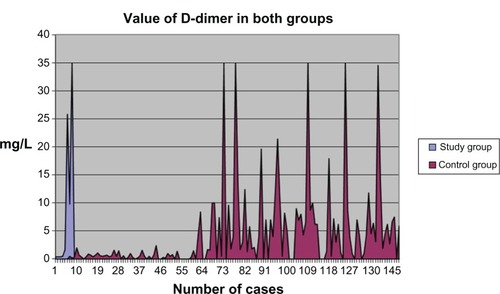
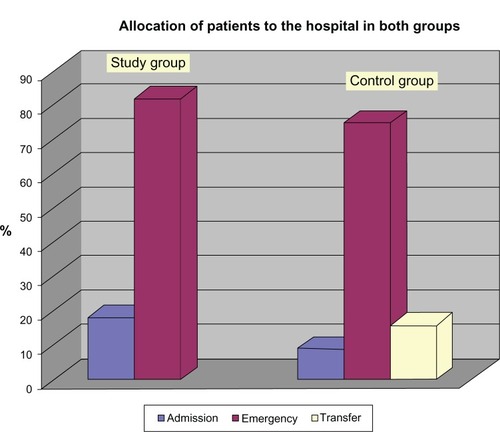
From the total of 2230 patients evaluated for PE during the study period, 15 (0.67%) patients were assigned to the study group and 197 (8.83%) patients were assigned to the control group. Eleven (including six [54.55%] women) of the 15 study patients (73.3%, 95% CI 51.0–95.7) and 148 (including 93 [62.84%] women) of the 197 control patients (75.1%, 95% CI 69.1–81.2) were diagnosed with PE. Compared with the elderly, there was no increase in relative risk for PE in the very elderly (0.98, 95% CI 0.72–1.34, P = 0.88). There was a significant difference in the number of cases between the two groups during the study period (P = 0.0003, ). The mean age of the patients in the study group was 91.6 ± 1.67 years compared with 84.0 ± 2.59 years in the control group (P < 0.0001). There was no significant difference in gender ratio between the two groups (P = 0.584). There were also no significant differences in the diagnostic procedures, clinical features of PE subtypes, and medical therapy administered (). The study group was more likely to experience minor bleeding at the extremities (P = 0.016, ). There was no significant difference in cardiovascular risk factors (). Multiple significant differences were found in chronic comorbidities between the two groups (P < 0.001, ). Pulmonary embolism (P = 0.365) and recurrences of deep vein thrombosis (P = 0.64) were detected in the two groups but without any statistically significant differences ().The mean D-dimer value was 9.24 ± 12.8 mg/L (range 0.4–34.9 mg/L; mode 0.4 mg/L) in the study group and 5.57 ± 7.73 mg/L (range 0.2–34.9 mg/L; mode 0.5 mg/L) in the control group (); this difference was not statistically significant (P = 0.67). In the study group, there were four positive, four negative, and three indeterminate D-dimer results. In comparison, there were 87 positive, 23 negative, and 38 indeterminate D-dimer results in the control group. Therefore, the D-dimer level does not have a significant predictive value in the very elderly (P = 0.059). All seven troponin tests drawn in the study group were negative. Of the 96 troponin tests drawn in the controls, there were 21 positive and 75 negative results. Similar to D-dimer, troponin has limited predictive value for PE in the very elderly (P = 0.166).
Table 1 Comparison of clinical presentation, diagnosis, and treatment for pulmonary embolism in the study and control groups
Table 2 Acute comorbidities in the study and control groups
Table 3 Cardiovascular risk factors in the study and control groups
Table 4 Chronic comorbidities in the study and control groups
None of the study patients were treated in the intensive care unit, whereas 30 (20.3%) control patients were; regardless, there was no significant difference between the numbers of critical care and ward treatments (P = 0.097). The duration of hospitalization was not significantly different (P = 0.387) between the study patients (15.6 ± 11.9 days) and control patients (12.0 ± 10.3 days). There was no significant difference in the number of hospital admissions between the two groups (P = 0.578, ). Although there were no deaths during the study, there were 16 (10.8%, 95% CI 5.81–15.8) deaths in the control group, including nine (59.25%) with fatal PE; however, a statistically significant difference in fatal outcomes between the groups could not be detected (P = 0.735). Thus, the survival rate was 100% in the study group and 89.2% (95% CI 83.9–94.5) in the control group.
Discussion
This study did not find an increased relative risk for PE in the very elderly compared with the elderly. PEs are common among the elderly,Citation3 but are the least often accurately diagnosed cardiovascular disease.Citation3 The annual incidence rates for PE and deep vein thrombosis have been reported to increase steadily with advancing age.Citation4 However, there was a significantly lower proportion of very elderly patients enrolled in this study, and these patients did not demonstrate an increased incidence of PE compared with the elderly population. Moreover, no increased relative risk for PE was detected in the very elderly. Women have also been reported to have lower rates of PE compared with men,Citation4 but both groups in this study contained more affected women, with no statistically significant difference found between the groups. These findings could be due to the small size of the study group and because of the study being conducted in a single department. Further, numbers of patients become smaller with advancing biological age. Recurrent PEs were observed, but with no statistically significant difference in rate of recurrence between the two groups during this investigation.
Risk factors for PE include congestive heart failure, cancer, orthopedic conditions such as hip fracture, and other debilitating diseases.Citation5 We observed an increased prevalence of congestive heart failure among the very elderly, but the difference relative to the elderly population was not statistically significant. Further, using the example of renal tumors, cancer among those of very advanced age was not observed in this study. Bone disorders were found to be significantly more prevalent among the very elderly than in the elderly. There were other multiple chronic diseases affecting a significantly higher proportion of the very elderly in this study.
The most commonly reported comorbidities in elderly patients with PE are cardiomegaly (22%–64%), pleural effusion (15.8%–57%), right heart overload (50%), syncope (8%–62%), shock (5%–31%), cough (12%–43%), hemoptysis (3%–14%), deep vein thrombosis (15%–50%), cancer (4%–32%), surgery (5%–44%), heart failure (5%–33%), previous deep vein thrombosis or PE (18%–41%), stroke (3%–13.5%), acute myocardial infarction (3%–11%), and chronic obstructive pulmonary disease (2%–27%).Citation6–Citation17 The most acute disorders documented in our study were cor pulmonale, cardiac decompensation, syncope, minor bleeding in the extremities, bronchopulmonary infection, gastrointestinal hemorrhage, gastritis, and glucose derangement in the very elderly, but not at significantly higher rates compared with the general elderly population. There was no correlation between these acute illnesses and PE in the very elderly, with these diseases appearing to be separate entities. A number of studies have shown that elderly patients over 80 years have a higher incidence of bleeding complications.Citation18 In our study, the very elderly had more minor bleeding complications, but we did not examine this relationship further.
The clinical presentation of PE can be subtle and atypical,Citation5 as this was also noted in our study. Traditional abnormalities in vital signs in the patient with PE can be missing, and syncope without chest pain or dyspnea is a frequent clinical symptom in the elderly.Citation5 In our study, although not statistically significant, the very elderly were more likely to experience syncope. Therefore, the differential diagnosis of syncope in the elderly should always include PE. Previous studies have reported that the main symptoms in the elderly with PE are dyspnea (59%–91.5%), tachypnea (46%–74%), tachycardia (29%–76%), and chest pain (26%–59%).Citation6–Citation17 In our study, dyspnea (45%–56%), chest pain (9%–21%), and cough (6%) were more frequent symptoms in the very elderly and elderly, although not significantly so.
The most common electrocardiographic changes reported in previous studies included sinus tachycardia (18%–62.5%), right bundle branch block (4.5%–40.5%), ST-T abnormalities (9%–37%), and S1Q3 (8%).Citation6–Citation17 In this study, the most common electrocardiographic abnormalities were tachyarrhythmia absolute in atrial fibrillation, T-negativity, and S1Q3, but these did not occur at significantly high rates compared with the elderly population. Further studies are needed to examine electrocardiographic changes in the elderly and very elderly with PE.
Hypoxia has often been described in blood-gas analysis in previous studies of patients with PE.Citation6,Citation8,Citation19 Similarly, hypoxia was frequently observed in both groups in our study, but we found no significant difference between the elderly and very elderly in this regard. Respiratory and metabolic acidosis has also been reported to be more frequent in elderly patients with PE than in their younger counterparts.Citation6,Citation8,Citation19 However, respiratory and metabolic acidosis was not detected in either group in our study. Nevertheless, we noted hypoxia in more than one third of our very elderly study patients. These respiratory changes and their implications for the diagnosis and treatment of PE require further evaluation in future prospective studies.
The specificity of D-dimer values in patients suspected of having PE decreases with advancing age.Citation20,Citation21 Two studies have examined the specificity of D-dimer for diagnosis of PE in the elderly and reported similar specificities (5%) for PE diagnosis in the elderly.Citation20,Citation21 This very low specificity has led to the proposal of an augmented cutoff value for D-dimer.Citation6 An elevated cutoff would reduce the number of false positives but also increase the proportion of false negatives.Citation6 We found a higher mean D-dimer value in the study group; however, there was no statistically significant difference in D-dimer values between the two groups. Hence, D-dimer has very limited predictive value for diagnosing PE in the very elderly.
The prognostic value of troponin has been demonstrated in high-risk patients with PE.Citation22 Troponin can improve the risk stratification of patients with PE and help to identify patients who may require aggressive treatment.Citation22,Citation23 Although troponin was not routinely tested, the findings of our study suggest that troponin also has limited predictive value for PE in the very elderly. Further, we did not observe a direct relationship between PE and release of troponin.
Aging did not affect the diagnostic quality of single detector or multidetector pulmonary angio-CT for PE.Citation24,Citation25 Use of lung scintigraphy for diagnosing PE is limited by pre-existing lung disease or an abnormal chest radiograph.Citation26,Citation27 In our study, chest CT was used almost equally in both groups. Although not statistically significant, the elderly were more likely to undergo ventilation perfusion scintigraphy.
The sensitivity of Doppler ultrasound for detecting deep vein thrombosis increases with age, but not the specificity.Citation27 Because more Doppler ultrasound examinations were performed in the very elderly in our study, more deep venous thromboses were found in this age group. Pulmonary angiography for the diagnosis of PE has the same diagnostic value in the elderly as in young age groups.Citation15 However, this test was not available for our study, so its utility and diagnostic value cannot be commented upon.
Population-based studies have identified a greater risk of death from PE in the elderly.Citation28 The mortality rates in this study were surprising, in that there were more deaths observed in controls than in patients from the study group. Our findings do not provide a reasonable explanation for this discrepancy, and further research is required.
Study limitations
This study examined all patients with PE treated in a department of internal medicine, but did not investigate patients with PE diagnosed in other departments. D-dimer, conventional troponin T, and highly sensitive troponin T levels were not routinely tested in all patients with PE, including those with malignancy. The differences in our descriptive results may be due to the age difference between the study population groups and individual biological variations with regard to limited life expectancy. Other limitations of this study were its small size (particularly that of the study group), its retrospective nature, and the fact that it was a single-center analysis.
Conclusion
An increased incidence of PE was not observed among the very elderly compared with the elderly. The clinical presentation of PE in the very elderly was subtle and there were no clear clinical symptoms in this group. Blood gas analyses were nonspecific, and D-dimer and troponin had minimal predictive value in this population. Further, there were no typical electrocardiographic changes, and an ideal radiological modality for diagnosing PE in the very elderly could not be identified.
Disclosure
The author reports no conflicts of interest in this work.
References
- HirshJHoakJManagement of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart AssociationCirculation199693221222458925592
- RighiniMLe GalGPerrierABounameauxHThe challenge of diagnosing pulmonary embolism in elderly patients: influence of age on commonly used diagnostic tests and strategiesJ Am Geriatr Soc2005531039104515935031
- WeberováDWeberPKubesováHOccurrence of pulmonary embolism among 260 in-patients of acute geriatric department aged 65+ years in 2005–2010Adv Gerontol20122550651223289231
- KniffinWDJrBaronJABarrettJBirkmeyerJDAndersonFAJrThe epidemiology of diagnosed pulmonary embolism and deep venous thrombosis in the elderlyArch Intern Med19941548618668154949
- RogersRLVenous thromboembolic disease in the elderly patient: atypical, subtle, and enigmaticClin Geriatr Med20072341342317462526
- MasottiLRayPRighiniMPulmonary embolism in the elderly: a review on clinical, instrumental and laboratory presentationVasc Health Risk Manag2008462963618827912
- BusbyWBayerAPathyJPulmonary embolism in the elderlyAge Ageing1988172052093389249
- CeccarelliEMasottiLBarabesiLForconiSCappelliRPulmonary embolism in very old patientsAging Clin Exp Res20031511712212889842
- GisselbrechtMDiehlJLMeyerGCollignonMASorsHClinical presentation and results of thrombolytic therapy in older patients with massive pulmonary embolism: a comparison with non-elderly patientsJ Am Geriatr Soc1996441891938576511
- KokturkNOguzulgenIKDemirNDemirelKEkimNDifferences in clinical presentation of pulmonary embolism in older vs younger patientsCirc J20056998198616041171
- Le GalGRighiniMRoyPMDifferential value of risk factors and clinical signs for diagnosing pulmonary embolism according to ageJ Thromb Haemost200532457246416241944
- MasottiLCeccarelliECappelliRGuerriniMForconiSPulmonary embolism in the elderly: clinical, instrumental and laboratory aspectsGerontology20004620521110859460
- PunukolluHKhanIAPunukolluGGowdaRMMendozaCSacchiTJAcute pulmonary embolism in elderly: clinical characteristics and outcomeInt J Cardiol20059921321615749178
- RamosAMurillasJMascíasCCarreteroBPorteroJLInfluence of age on clinical presentation of acute pulmonary embolismArch Gerontol Geriatr20003018919810867163
- SteinPDGottschalkASaltzmanHATerrinMLDiagnosis of acute pulmonary embolism in the elderlyJ Am Coll Cardiol199118145214571939945
- TimmonsSKingstonMHussainMKellyHListonRPulmonary embolism: differences in presentation between older and younger patientsAge Ageing20033260160514600000
- ChungTEmmettLKhouryVAtrial and ventricular echocardiographic correlates of the extent of pulmonary embolism in the elderlyJ Am Soc Echocardiogr200619347135316500500
- PoliDAntonucciETestaSCosmiBPalaretiGAgenoWTheFCSA(Italian Federation of Anticoagulation Clinics). The predictive ability of bleeding risk stratification models in very old patients on VKA treatment for venous thromboembolism. Results of the Prospective Collaborative EPICA studyJ Thromb Haemost4112013 [Epub ahead of print.]
- JonesJSVan DeelenNWhiteLDoughertyJAlveolar-arterial oxygen gradients in elderly patients with suspected pulmonary embolismAnn Emerg Med199322117711818517570
- HarperPLTheakstonEAhmedJOckelfordPD-dimer concentration increases with age reducing the clinical value of the D-dimer assay in the elderlyIntern Med J20073760761317543005
- RighiniMde MoerloosePReberGPerrierABounameauxHShould the D-dimer cut-off value be increased in elderly patients suspected of pulmonary embolism?Thromb Haemost20018574411341515
- GiannitsisEMüller-BardorffMKurowskiVIndependent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolismCirculation200010221121710889133
- EneaICeparanoGMazzarellaGDi SarnoRCangianoGBusinoCABiohumoral markers and right ventricular dysfunction in acute pulmonary embolism: the answer to thrombolytic therapyItal Heart J Suppl200452935 Italian15253142
- RighiniMLe GalGPerrierABounameauxHEffect of age on the assessment of clinical probability of pulmonary embolism by prediction rulesJ Thromb Haemost200421206120815219218
- SteinPDWoodardPKWegJGPIOPED II investigatorsDiagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigatorsAm J Med20061191048105517145249
- SteinPDHullRDKayaliFGhaliWAAlshabAKOlsonREVenous thromboembolism according to age: the impact of an aging populationArch Intern Med20041642260226515534164
- RighiniMGoehringCBounameauxHPerrierAEffects of age on the performance of common diagnostic tests for pulmonary embolismAm J Med200010935736111020391
- SakumaMNakamuraMTakahashiTPulmonary embolism is an important cause of death in young adultsCirc J2007711765177017965499