Abstract
Purpose
It has been shown that lower Barthel’s index (BI) at admission is associated with a higher in-hospital mortality. There is a lack of evidence regarding the association between the change in BI during hospitalization and mortality after discharge. Our purpose was to determine whether the BI change during hospitalization is associated with all-cause mortality in older adults with COVID-19 pneumonia.
Patients and Methods
We conducted a retrospective cohort study of 330 participants at Peking University Third Hospital during the COVID-19 pandemic period. In order to analyze the time to death data, a Kaplan-Meier survival curve was used. We used restricted cubic splines to analyze the association between BI change and all-cause mortality among COVID-19 pneumonia patients aged over 80 years old. Threshold effect analysis was used to assess the ability of BI change score to predict all-cause mortality.
Results
Our study included 330 patients aged over 80 years with COVID-19 pneumonia. The Kaplan-Meier curve for mortality showed significantly worst survival with reduced BI among three groups (χ2= 6.896, P < 0.05). There was a non-linear association between the BI change and all-cause mortality (P for all over <0.001). The effect sizes on the left and right sides of the inflection point were 0.958 (HR: 0.958, 95% CI 0.932–0.958, P < 0.05) and 1.013 (HR: 1.013, 95% CI 0.967–1.062, P > 0.05), respectively.
Conclusion
Reduced BI during hospitalization was associated with the highest mortality risk. It is crucial to monitor BI change among COVID-19 pneumonia patients aged over 80 years old.
Introduction
With the pandemic of coronavirus disease 2019 (COVID-19), it has become a public health crisis and continues to inflict a significant burden on health worldwide.Citation1 Since December 2022, a wave of the Omicron BA.5.2/BF.7 epidemic has escalated and then spread quickly across all provinces in China.Citation2 Adults aged 65 and older are particularly susceptible to multimorbidity and the negative mental health impacts of “lockdown” measures.Citation3,Citation4 They are also especially vulnerable to severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) infection and are at high risk for COVID-19-associated mortality.Citation5
Identifying and modifying mortality risk factors in older adults may provide new intervention opportunities. Functional status, including activities of daily living (ADL)Citation6,Citation7 and the six-minute walk test,Citation8 is an important factor influencing all-cause mortality in older adults with COVID-19. Barthel’s index (BI) is employed to measure the level of dependency in ADLs at both hospital admission and discharge. Previous studies have considered BI a potential indicator of functional status.Citation9 Studies have demonstrated that the BI score is significantly and independently associated with in-hospital mortality with COVID-19.Citation6,Citation10,Citation11
Although BI at hospital admission is a prognostic factor for older adults, a change in BI between hospital discharge and hospital admission has been expected and observed. However, it is not clear that whether the BI change can serve as a prognostic indicator in oldest old patients. In the current study, our purpose was to determine whether the BI change during hospitalization is associated with all-cause mortality among COVID-19 pneumonia patients aged over 80 years old.
Materials and Methods
Study Design and Patients
The retrospective observational cohort study was conducted at Peking University Third Hospital during the COVID-19 pandemic period from December 2022 to February 2023 in Beijing, China.
All patients aged over 80 years diagnosed with COVID-19 pneumonia based on Guidelines for the Diagnosis and Treatment of Coronavirus Disease 2019Citation12 who were discharged between Dec 26, 2022 and Feb 9, 2023 were included. The exclusion criterion was the absence of the important data. The study protocol was approved by the medical ethics committee of Peking University Third Hospital (M2024045). Informed consent is waived for all patients.
Data Collection and Definitions
The following data from all patients were collected: age, sex, Charlson comorbidity Index (CCI), ADL dependence at admission and discharge, and comorbidities such as hypertension, diabetes, coronary heart disease, heart failure, atrial fibrillation, chronic respiratory disease, cerebrovascular disease, chronic kidney disease and solid tumors. Additionally, we recorded vital signs at admission including heart rate, respiratory rate, respiratory failure and conscious status. Treatments during hospitalization were also documented, including antiviral therapy, hormone therapy, immunotherapy, anticoagulant therapy, traditional Chinese medicine, nutrition support and ventilator assisted ventilation. Laboratory parameters were collected within 24 hours of admission.
ADL dependence was assessed using Barthel’s index (BI) score at admission and discharge. This assessment covered activities such as feeding, bathing, grooming, dressing, bowel control, bladder care, toileting, chair transfer, ambulation, and stair climbing.Citation13 Trained nurses and researchers conducted these evaluations. The total BI score ranged from 0 to 100, with higher scores indicating greater independence in daily activities. BI change during hospitalization was calculated by subtracting the BI score at discharge from the BI score at admission.
Charlson comorbidity Index (CCI) is calculated from the collected data and information using a coding algorithm and weight assignment.Citation14
Outcome
All-cause mortality was the primary outcome in the present study.
Statistical Analysis
We used R statistical software (version 4.1.2, R Core Team, Vienna, Austria) for the statistical analysis. Continuous variables were expressed as median [interquartile range] or mean ± standard deviation (SD). Categorical variables were reported in numbers and percentages. Patients were divided into three groups based on the BI change score (group 1: BI change < 0; group 2: BI change = 0; group 3: BI change > 0).
To explore the association between BI change and all-cause mortality after discharge, restricted cubic spline was adopted, and univariate and multivariate Cox regression analyses were conducted to assess the stability of the association, which used unadjusted and multivariate adjusted models. Confounders were selected in the fully adjusted model as adjusted on the basis of judgment, or the matched hazards ratio changed by at least 10%. In order to analyze the time to death data, a Kaplan-Meier survival curve was used. Threshold effect analysis was used to assess the ability of the BI change score to predict all-cause mortality. P < 0.05 was considered as statistically significant.
Results
Baseline Characteristics
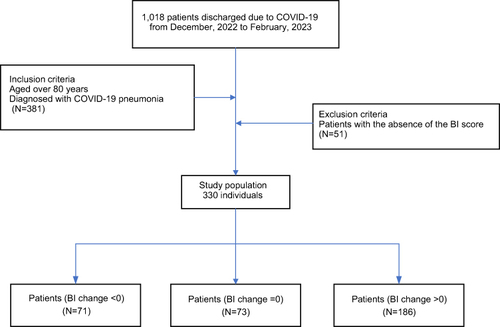
All 1018 patients with COVID-19 pneumonia were discharged from Peking University Third Hospital between December 26, 2022 and February 9, 2023. 381 of them aged over 80 years were screened; 51 of them were ruled out due to the absence of important data. A total of 330 patients were included in the study ().
The baseline characteristics of the patients stratified by change in BI were shown in . The average age was 86.4 years, with a range of 80 to 100 years. Of them, 204 (61.8%) were male. The mean BI scores at admission and discharge were 45.0 (IQR 20.0–65.0) and 60.0 (IQR 25.0–70.0), respectively. The average CCI score was 1.0 (IQR 1.0–2.0). The distribution of patients’ characteristics among BI change groups was similar, with no significant difference regarding age, sex, comorbidities, vital signs, therapies and laboratory parameters (all P value > 0.05), except for solid tumors with metastasis (P=0.017), immunotherapy (P=0.002) and nutritional support (P=0.004). The BI scores at admission (P=0.002) and discharge (P<0.001) were statistically different among the three groups.
Table 1 Baseline Characteristics of the Study Population Stratified by BI Change
Association Between BI Change and Outcome
The results of the univariate analysis of the risk factors associated with 6-month all-cause mortality in COVID-19 pneumonia patients aged over 80 years old were summarized in . BI change, coronary heart disease, atrial fibrillation, chronic kidney disease and BNP were significantly associated with all-cause mortality (P<0.05). Otherwise, factors such as other comorbidities, laboratory results and vital signs, were not significantly associated with all-cause mortality ().
Table 2 Association of Covariates and All-Cause Mortality in Older Patients with COVID-19 Pneumonia
In the multivariate Cox regression analysis (), BI change expressed as a continuous variable was significantly negatively associated with risk of all-cause mortality (HR=0.97, 95% CI 0.96–0.99, P=0.002). When considered as a categorical variable, a third group of BI change >0 was used as a baseline reference, and BI change <0 group was associated with the highest risk of all-cause mortality (crude HR: 2.79; 95% CI 1.26–6.22; P<0.05). Further, a first group of BI change < 0 was significantly associated with the highest risk of all-cause mortality after adjustment for sex, coronary heart disease, atrial fibrillation, chronic kidney disease, procalcitonin and platelet count in model 3 (adjusted HR:2.43; 95% CI 1.07–5.5; P < 0.05) ().
Table 3 Cox Proportional Hazard Regression Analyses for All-Cause Mortality
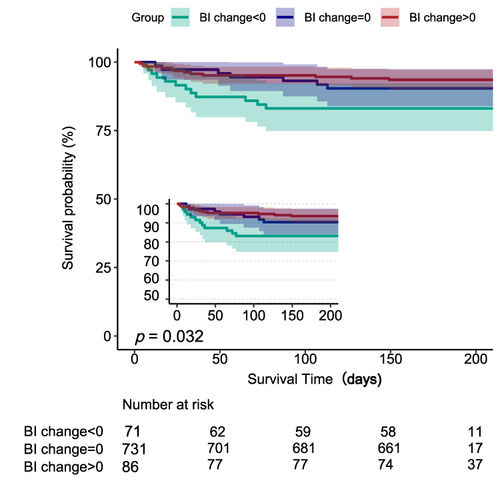
Survival analysis showed a statistical difference in time to death among the three groups. The Kaplan-Meier curve for all-cause mortality further showed significantly the worst survival with BI change <0 (χ2=6.896, P= 0.032) ().
Figure 2 Kaplan-Meier survival curves for oldest old patients with COVID-19 pneumonia by the BI change categories.
A multivariable adjusted restricted cubic spline showed a nonlinear relationship between BI change and all-cause mortality (P for non-linearity =0.027) ().
Figure 3 Association between BI change and all-cause mortality in oldest old patients with COVID-19 pneumonia. Solid and dashed lines represent the predicted value and 95% confidence intervals. They were adjusted for age, sex, coronary heart disease, atrial fibrillation, chronic kidney disease, procalcitonin and platelets count. 99% of the data is shown.
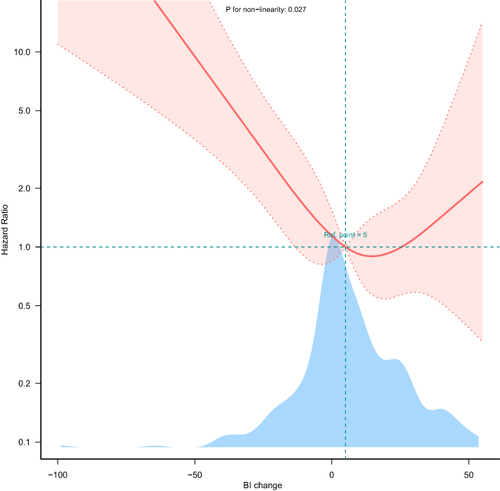
In the threshold analysis, we found an inflection point at approximately 4.468. On the left side of the inflection point, the effect size was 0.958 (HR: 0.958, 95% CI 0.932–0.985, P<0.05). This indicates that a decrease of 1 in BI change is associated with a 4.2% increase in the risk of all-cause mortality. On the contrary, there was no significant association between BI change and all-cause mortality in those patients with BI change ≥5 (). This means that the risk of all-cause mortality no longer increases with decreasing BI change.
Table 4 Threshold Effect Analysis of BI Change and the All-Cause Mortality Using Cox Regression Models
Discussion
This retrospective study focuses on older patients aged over 80 years with COVID-19 pneumonia, demonstrating that changes in the Barthel’s index are a simple and effective predictor of 6-month all-cause mortality. Our study observed a non-linear association and threshold effect between BI change and all-cause mortality. This rapid and cost-effective test effectively classifies oldest old patients, thereby more accurately predicting who will experience major adverse outcomes and who will need further medical care and rehabilitation.
ADL was introduced in the early 1980s as a means of evaluating individual independence in daily living. At first, it was intended to determine life expectancy for older patients.Citation15 Independent ADL accounts for a large part of the functions of the older adults.Citation16 In fact, the older adults who perform ADL independently have a higher quality of life and a lower mortality rate than those who do not.Citation17 It has been found that lower ADL scores in non-COVID patients who require mechanical ventilation were associated with a worse outcome, implying a higher degree of dependence.Citation18 Similarly, it was found that ADL impairment was associated with functional decline and was also associated with in-hospital mortality among older patients with COVID-19. Previous studies have shown that Barthel Index of prognostic value for in-hospital mortality to measure the level of ADL dependency among older adults with COVID-19.Citation6,Citation10,Citation11 Lower BI scores were associated with higher all-cause mortality in older patients with COVID-19.Citation6 In this study, Cos et al suggested that ADL dependence was significantly related to in-hospital mortality (OR 6.296; 95% CI 1.795–22.088, P <0.05). However, there is a lack of evidence regarding the association between BI change during hospitalization and mortality after discharge. Our study examined the impact of BI change on survival in older patients aged over 80 years old. A non-linear association between BI change and 6-month all-cause mortality was observed in this study. Participants with worse BI scores at discharge than at admission had the highest risk of death.
Reduced BI score is an important indicator of functional decline. Previous studies have reported that older patients suffered from severe functional decline after hospitalization due to COVID-19Citation19 and functional decline was closely related to prognosis among older adults with COVID-19.Citation20,Citation21 Meanwhile, functional decline may be at high risk for increasing frailty, and frailty is a predictor of COVID-19 outcomes.Citation22 This is consistent with our study, which found that a BI change below around 5 scores significantly increase the risk of 6-month all-cause mortality. When the BI change was below 4.468 scores, each 1 score reduction in BI change was associated with a 4.2% increase in the risk of 6-month all-cause mortality after discharge. According to our findings, it is practical to monitor BI changes during hospitalization in addition to a single- time point BI at admission.
Indeed, hospitalization for an acute infection can lead to an increased functional decline and is associated with a deterioration in health-related quality of life in the post-discharge period. Functional decline was reported 27 to 54% in older patients after COVID-19.Citation9,Citation19 According to the study, at least 35% of COVID-19 survivors became dependent within one year of discharge (BI lower than 100).Citation23 Our study showed that the older patients with BI change < 0 (21.5%) after an acute disease experienced the worst survival outcome. Geriatrists should be aware that ADL-dependent patients discharged from the hospital are at increased risk of not regaining their independence. Based on our study, we infer that for those with decreased BI, rehabilitation should be done after discharge to improve the patient’s functional status, and maybe it is helpful to improve the patient’s survival prognosis.
Besides, our study had some limitations that should be mentioned. Firstly, given the observational nature of this study, we could not establish causality between BI change and mortality. Further prospective studies are needed to explore whether elevated BI after discharge with rehabilitation improves patients’ prognosis. Secondly, our study population included individuals aged 80 and older. However, we did not investigate the impact of BI change on the prognosis of young older individuals. Further study should consider different age groups. Thirdly, due to the single-center study design, there may be regional and population bias. Further study should consider multiple regions to verify our results. Finally, several studies have demonstrated that malnutrition,Citation24 sarcopenia,Citation25 and frailtyCitation26 were associated with poor prognosis in COVID-19 patients. Our study did not consider above factors in predicting outcomes for older COVID-19 patients. Future research should explore these factors to verify our findings.
Conclusion
Our study showed the BI change during hospitalization could be considered a valid test to predict 6-moth all-cause mortality in oldest old patients with COVID-19 pneumonia. It is important to recognize that the broader background of ADL plays a key role in the outcome of acute viral pneumonia infection. These results suggest that practitioners should create individualized discharge plans that consider both aging and functional status assessments, as well as severity assessments. Moreover, these patients require specialized geriatric follow-up in order to develop a long-term personalized care plan.
Ethics Approval and Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the medical ethics committee of Peking University Third Hospital (M2024045). The consent was waived due to the retrospective nature of the review, we confirmed that the data was anonymized or maintained with confidentiality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. doi:10.1016/j.ijsu.2020.02.034
- China center for disease control and prevention: seven new cases of local focus mutant strains involving two strains were discovered; 2023. Available from: https://news.sina.com.cn/c/2023-02-26/doc-imyhyscv1270943.shtml. Accessed February 26, 2023.
- Amerio A, Aguglia A, Odone A, et al. Covid-19 pandemic impact on mental health of vulnerable populations. Acta Bio Med. 2020;91(9–s):95–96. doi:10.23750/abm.v91i9-S.10112
- Ambrosetti J, Macheret L, Folliet A, et al. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatry. 2021;21(1):465. doi:10.1186/s12888-021-03469-8
- Catalano A, Dansero L, Gilcrease W, et al. Multimorbidity and SARS-CoV-2-related outcomes: analysis of a cohort of Italian patients. JMIR Pub Health Surv. 2023;9:e41404. doi:10.2196/41404
- da Costa JC, Manso MC, Gregório S, Leite M, Pinto JM. Barthel’s index: a better predictor for COVID-19 mortality than comorbidities. Tuberc Respir Dis. 2022;85(4):349–357. doi:10.4046/trd.2022.0006
- Heras E, Garibaldi P, Boix M, et al. COVID-19 mortality risk factors in older people in a long-term care center. Eur Geriatr Med. 2021;12(3):601–607. doi:10.1007/s41999-020-00432-w
- Klanidhi KB, Chakrawarty A, Bhadouria SS, et al. Six-minute walk test and its predictability in outcome of COVID-19 patients. J Educ Health Promot. 2022;11(1):58. doi:10.4103/jehp.jehp_544_21
- Hosoda T, Hamada S. Functional decline in hospitalized older patients with coronavirus disease 2019: a retrospective cohort study. BMC Geriatr. 2021;21(1):638. doi:10.1186/s12877-021-02597-w
- Wang E, Liu A, Wang Z, et al. The prognostic value of the Barthel Index for mortality in patients with COVID-19: a cross-sectional study. Front Public Health. 2022;10:978237. doi:10.3389/fpubh.2022.978237
- Mateos-Arroyo JA, Zaragoza-García I, Sánchez-Gómez R, Posada-Moreno P, Ortuño-Soriano I. Validation of the Barthel index as a predictor of in-hospital mortality among COVID-19 patients. Healthcare. 2023;11(9):1338. doi:10.3390/healthcare11091338
- Commission NH, Medicine NAo TC. Guidelines for the diagnosis and treatment of coronavirus disease 2019 (trial version ninth). Chin J Viral Dis. 2022;12(03):161–169.
- Hartigan I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int J Older People Nurs. 2007;2(3):204–212. doi:10.1111/j.1748-3743.2007.00074.x
- Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi:10.1093/aje/kwq433
- Steinberg A, Levy-Lahad E, Karni T, Zohar N, Siegal G, Sprung CL. Israeli position paper: triage decisions for severely ill patients during the COVID-19 pandemic. joint commission of the Israel national bioethics council, the ethics bureau of the Israel medical association and representatives from the Israeli ministry of health. Ram Maimon Med J. 2020;11(3). doi:10.5041/RMMJ.10411
- Reynolds SL, Silverstein M. Observing the onset of disability in older adults. Soc sci med. 2003;57(10):1875–1889. doi:10.1016/S0277-9536(03)00053-4
- Nakazawa A, Nakamura K, Kitamura K, Yoshizawa Y. Association between activities of daily living and mortality among institutionalized elderly adults in Japan. J Epidemiol. 2012;22(6):501–507. doi:10.2188/jea.JE20110153
- Demiselle J, Duval G, Hamel JF, et al. Determinants of hospital and one-year mortality among older patients admitted to intensive care units: results from the multicentric SENIOREA cohort. Ann Intens Care. 2021;11(1):35. doi:10.1186/s13613-021-00804-w
- Carrillo-Garcia P, Garmendia-Prieto B, Cristofori G, et al. Health status in survivors older than 70 years after hospitalization with COVID-19: observational follow-up study at 3 months. Eur Geriatr Med. 2021;12(5):1091–1094. doi:10.1007/s41999-021-00516-1
- Kastora S, Kounidas G, Perrott S, Carter B, Hewitt J, Myint PK. Clinical frailty scale as a point of care prognostic indicator of mortality in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;36:100896. doi:10.1016/j.eclinm.2021.100896
- Tsai YL, Cheng YY. Predictors of Basic activity in daily living and length of hospitalization in patients with COVID-19. Healthcare. 2022;10(8). doi:10.3390/healthcare10081589
- Anne O’Malley P. Frailty and disability: predictors or outcomes or both in post COVID-19. Crit Care Med. 2022;50(6):1023–1025. doi:10.1097/CCM.0000000000005502
- Cavalleri J, Treguier D, Deliège T, et al. One-year functional decline in COVID-19 and Non-COVID-19 Critically Ill survivors: a prospective study incorporating a pre-ICU status assessment. Healthcare. 2022;10(10):2023. doi:10.3390/healthcare10102023
- Bedock D, Bel Lassen P, Mathian A, et al. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin Nutr ESPEN. 2020;40:214–219. doi:10.1016/j.clnesp.2020.09.018
- Yakti FAZ, Abusalah L, Ganji V. Sarcopenia and mortality in critically ill COVID-19 patients. Life. 2023;14(1):24. doi:10.3390/life14010024
- Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5(8):e444–e451. doi:10.1016/S2468-2667(20)30146-8