Abstract
Purpose
To evaluate whether rehabilitation of muscle force or balance improves postural stability and quality of life (QoL), and whether self-administered training is comparable with guided training among older adults residing in an institutional setting.
Patients and methods
A randomized, prospective intervention study was undertaken among 55 elderly patients. Three intervention groups were evaluated: a muscle force training group; a balance and muscle force training group; and a self-administered training group. Each group underwent 1-hour-long training sessions, twice a week, for 3 months. Postural stability was measured at onset, after 3 months, and after 6 months. Time-domain-dependent body sway variables were calculated. The fall rate was evaluated for 3 years. General health related quality of life (HRQoL) was measured with a 15D instrument. Postural stability was used as a primary outcome, with QoL and falls used as secondary outcomes.
Results
Muscle force trainees were able to undertake training, progressing towards more strenuous exercises. In posturography, the number of spiky oscillations was reduced after training, and stationary fields of torque moments of the ankle increased, providing better postural stability in all groups; in particular, the zero crossing rate of weight signal and the number of low variability episodes in the stabilogram were improved after training. While no difference was found between different training groups in posturography outcomes, a reduction of fall rate was significant in only the guided training groups. A significant part of the variability of the QoL could be explained by the posturography outcome (46%). However, the outcome of training was associated with a reduced QoL.
Conclusion
Even moderate or severely demented residents could do exercises in five-person groups under the supervision of a physiotherapist. An improvement in postural stability was observed in all training groups, indicating that even self-administered training could be beneficial. Posturography outcome indicated that training alters the postural strategy by reducing the oscillatory fluctuations of body sway signal. However, only guided training tended to reduce falls. Short training intervention programs may decrease QoL by changing the elderly’s daily routine and making it more active and exhausting.
Introduction
Accidental falls are one of the leading causes of death among the elderly population, surpassing even those due to car accidents.Citation1 Among people aged 85 years and older, one out of five fatal falls occurs in a nursing home.Citation2 Rubenstein et alCitation3 reviewed such falls and showed that the mean incidence of falls in nursing homes is 1.5 falls per bed per year (range: 0.2–3.6 falls). Because of the high frequency of recurrent falls in nursing homes, the likelihood of sustaining an injurious fall is substantial.Citation4 In addition, falls reduce quality of life (QoL).Citation5
Posturography has been used to objectively screen and predict those elderly who are liable to fall. Era et alCitation6 studied 7,979 subjects using posturography. Measurements showed a decline in balance functions with advancing age, starting from about 60 years. Rasku et alCitation7 demonstrated that the decline of postural stability continued to deteriorate up to 90 years of age; by careful evaluation of a stabilogram, the age of subjects could be predicted with an accuracy of 5 years. Kerber et alCitation8 demonstrated an association of poor balance and accidental falls with the outcomes of posturographic measurements. They regarded postural imbalance as a key factor for explaining accidental falls. However, the clinical value of posturography is still controversial in assessing the elderly’s likelihood of falling.Citation9 One of the main problems in the use of posturography is that there is no standard for measurement or agreement on the variables to be analyzed.Citation10 The richness of existing variables calculated from stabilogram signals contains useful information on upright stance, but may also blur the data by unnecessarily increasing the dimension of feature space, thus making balance analysis more complicated.Citation11
Rehabilitation may improve postural stability and prevent falls when medical therapy has reached its limits, but in older adults residing in an institutional setting there is insufficient evidence of any benefit of fall interventions.Citation12 Recently Neyens et alCitation13 performed an extensive literature survey on interventions to prevent falls in long-term care facilities. They concluded that the evidence is inconclusive for multifaceted and single interventions in long-term care facilities. Most of the reviewed studies did not find a significant positive effect on fall incidents. However, their data supports the conclusion that multifactorial interventions in long-term care populations seems more likely to be beneficial (as also indicated by Gillespie et al)Citation14 among older people living in a community setting. A careful approach to fall prevention is needed as programs to prevent falls in these settings may be ineffective or may even have adverse effects.Citation13 Recently, we demonstrated that rehabilitation with balance and muscle force training reduced the number of accidental falls in older people living in a community setting, and even in residents with dementia.Citation15 The aim of the present study is to evaluate the effect of muscle force training, balance training, and self-training on several time-domain variables retrieved from stabilograms. A further aim was to explore the consequences of training on the general HRQoL.
Methods
The older adults of the Koukkuniemi residential facility
The study was carried out in a residential facility in Koukkuniemi, Tampere, Finland. The home housed 869 older adults during the study period. The majority of the residents needed support for moving, or suffered moderate to severe dementia. The criteria for inclusion in the study were (a) the subject’s ability to raise herself/himself from a chair without using their hands or arms for support, and (b) their willingness to participate in the intervention. Of the 869 residents, 156 met the criteria and 59 (15 male and 44 female) volunteered to take part in the study. The City of Tampere’s institutional review board approved the study protocol. The participants were randomly assigned to three groups – one with muscle force training, one with balance and muscle force training, and one with self-administered training (with instructions) on the ward under the supervision of a personal geriatric nurse. Four of the participants died before baseline testing and commencement of the training, and thus the groups consisted of 18 participants with muscle force training, 19 with self-administered training, and 18 with balance and muscle force training ().
Table 1 Characteristics and number of elderly in each exercise training group
Data collection
In order to define the case history concerning vertigo, balance problems, and general health, a standardized questionnaire was administered that consisted of 98 questions about the resident’s symptoms, medical history, and medication.Citation16,Citation17 The character of balance problems and dizziness was explored to categorize the often vague and imprecise symptoms expressed by the subjects into consistent and more precisely defined terms. Balance problems and dizziness were broken down into more detail as rotatory vertigo, dizziness, movement instability, fear of falling, sudden loss of balance, light headiness, and a floating sensation and/or black-out. In addition, some related symptoms such as a feeling of unreality, loss of vitality, nervousness, and reduced mobility were queried. The subjects were rated for limitation in activities due to symptoms. Finally, the effect of balance problems, vertigo, or dizziness on the subjects’ everyday life was evaluated. In gathering the data, one of the authors (ET) interviewed the participants and, when necessary, used the participant’s personal nurses as proxies.
The Mini Mental Status Examination (MMSE) measures cognitive ability (attention, memory, language, and calculations) and has a maximum score of 30. For MMSE, 24 is the normal limit; anything lower indicates some impairment.Citation18
The 15D is a widely used method to assess general HRQoL; it consists of 15 questions, each graded to 5 levels. Thus the person has 15Citation5 possibilities with which to reply, and each reply to a question is weighted with a calculation to provide a final score. The 15D questions concern sensory functions and mobility, the participant’s ability to perform regular day-to-day tasks, and their perceptions about their capabilities and limitations.Citation19 The final score is between 0 and 1, where 0 indicates a condition akin to death and 1 a full, complaint-free life. The instrument is designed to establish the degree to which patients are content with their lives and abilities. For example, the question about walking ability is rated as follows: 0 = I can walk normally; 1 = I can walk with little difficulty; 2 = I can walk with notable difficulties; 3 = I can only walk a little; and 4 = I am unable to walk. As the participants were living in a residential home, we did not use the sex question available in the instrument. The QoL was investigated both at the beginning of training and after the 3-month training period had ended.
Training
Training took place in groups of five under the supervision of physiotherapists. Each day, two trained physiotherapists controlled the exercise intensity and adjusted it to the trainee’s capacity. In the self-training groups, personal nurses on the ward provided stimulation and encouraged the participants to keep up with their self-guided training tasks twice a week, for around 1 hour at a time. The self-guided training took place based on written instructions provided by the physiotherapists. Exercises were scheduled twice a week, 1 hour at a time, for 26 sessions over 13 weeks. We then followed the trainees over 3 years by recording their falls and the reasons for their falls during this period. Fall data was collected using fall questionnaires obtained from the ward nurses. Every fall was documented and efforts were made to find out the reasons and circumstances leading to the fall.
In muscle force training, the exercises focused on increasing the muscle strength of the hip and other postural muscles, with exercises becoming more strenuous over time. In sessions 1–5, the exercises started with warm-up training lasting 10 minutes. This included stretching each leg in the sitting position, standing up exercises, squats (bending deeply at the knees) to standing position beside parallel bars, three repeats of side steps to the left and right, standing on tiptoes, and alternatingly raising both knees with the support of a parallel bar. From the sixth training session onwards, 1.2 kg weights were fixed to the ankles. From the ninth training session onward, whilst standing, exercises included knee raising and extension, adduction and abduction of the lower limbs on training equipment with extra resistance, squat to standing, and exercises on a stepper board. The exercises were carried out with weights applied and repeated ten times, which was successively increased during each session to 20 times with two repetitions. From the 19th exercise session onwards, training to walk up a staircase was added.
The balance and muscle force training aimed to increase a combination of strength, flexibility, and balance training. It started with walking on a model trace painted on the floor, shifting weight from one leg to the other, walking backwards, tandem stance training, and standing with feet together and eyes closed. From the third session onwards, we added moving by turning and twisting and walking with a beanbag on the head. From the ninth session onwards, we added a stepping exercise, blind walking in parallel bars with hindrances on the support base, blind walking straight, and a bean bag stretching exercise (from squat to tiptoe). From exercise 18 onwards, a trampoline, balance board, ball bouncing, ball throwing and catching, walking on a line beside the parallel bar, and walking while turning the head side to side and head nodding were added. The muscle force training was similar to that of the muscle force group, but weights were not increased.
The self-administered training consisted of three exercises; in the sitting position there was the stretching of each leg and raises from the chair, and crouching and rising were conducted from the standing position. Instructions were given in written form and were supervised twice a week by geriatric nurses on the ward.
Posturography
Posturography was carried out before training, immediately after training, and 6 months after commencing the training. Posturography measures vertical forces on the force platform surface. The center point of force on the platform surface records the movement of the body’s center point of mass projecting on the platform (body sway). The weight signal of the platform measures corrective forces made by the person when adjusting posture. We used a custom-made force platform that measured vertical force distribution over the platform surface.Citation20 Analysis of the data was collected on a stance lasting 15 seconds. The subjects were asked to close their eyes and instructed to keep their hands on their chest, lock their knee joints, and stand as stably as they could. The sampling frequency of the force platform was 50 Hz. Two of the signal components in the stabilogram give the location of the force reaction under the subject’s feet in mediolateral (x) and anterior-posterior (y) directions in each sample (t). The third component of the stabilogram provides the magnitude of force reaction acting on the force platform in respective sampling instants. This signal also outlines the mass of the subject; although the subject’s mass remains constant, the applied weight changes are due to muscle forces exerted in efforts to control posture.
To remove the effect of transition error and, to give the subject some time to become accustomed to the test, we removed 150 samples from the beginning of the filtered stabilograms. After preprocessing, the lengths of stabilograms amounted to 600 samples for an average of 12 seconds. We removed the mean values of the stabilogram’s positional components before further processing.
Variables
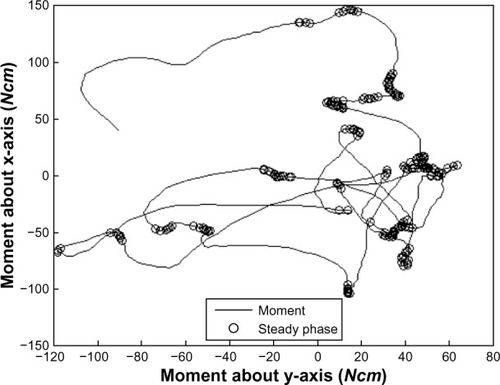
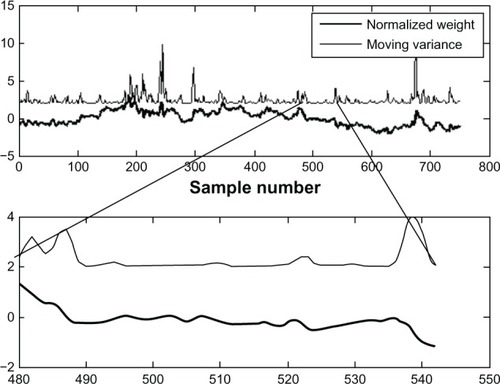
In the present study we selected eight time-domain variables which had the greatest associations between age and sex; for reference, we selected body sway velocity and Romberg’s quotient.Citation7 Our selected variables and their abbreviations were the 95% confidence amplitude in anterior posterior direction C(Y) and the sway velocity of body sway (SV). The Romberg’s quotient was calculated (mm/s) from sway velocity values (SV eyes closed/SV eyes open). We calculated the mean of the absolute moment about the mediolateral axis M(MY), the area of ellipse which contained all stabilogram samples EA, the area of an ellipse which contained 95% of stabilogram samples CEA, the zero crossing rate of a stationary point in anterior-posterior direction ZCR(Y), the zero crossing rate of velocity in the mediolateral direction ZCR(VX), the critical time where an open loop control changes into a closed loop control CRI(T), and the number of samples which belong to a steady phase standing ST(N). In our statistical work, we took the natural logarithms of the variables in order to make their distributions closer to normal. ST(N) describes the number of moment signal samples that belong to a steady phase standing. The steady phases during quiet standing (ST[N]) are illustrated in . The location of the center point of force (CPF) can be extracted directly from the preprocessed stabilogram; illustrates the steady phase standing, and is marked with circles.
The signal was also composed of many low variance periods and many “spiky” periods that were indicators of rapid and frequent oscillations in posture. A moving window was ultimately slid over the entire weight signal. depicts the low and high variation areas and also indicates the zero crossing rate of weight. Inside the low variation areas the signal changes signs relatively frequently; however, in the “spiky” areas the signal sign does not change so often. The postural stability was evaluated in visual and nonvisual conditions. Sway velocity and maximum amplitude of body sway were used as outcome variables. The Romberg’s quotient was calculated (mm/s).
Statistical analysis
Differences in continuous variables between the training groups were analyzed with an analysis of variance (ANOVA) and in discrete variables with the Mann–Whitney U-test, Chi-square test, or Wilcoxon signed-rank test. In exploring associations, a linear correlation was made and evaluated using Kendall’s tau. In analyzing the posturography outcome and changes in QoL, a paired Student’s t-test was used. In searching for associations between risk factors and the posturography outcome analysis of variance (ANOVA), and in the case of binary variables, logistic regression analysis was carried out.
Results
Before the end of the training, six residents stopped training (four in the balance and muscle force training group; two in the muscle force training group). Their scores in the 15D instrument were significantly lower than the others (Mann– Whitney U-test, P = 0.032); in particular, their scores were significantly lower in vigilance (P = 0.014), depression (P = 0.005), and anxiousness (P = 0.015). In presbyequilibrium the participants who stopped their training had more frequent vertigo (P = 0.047) and floating sensations (P = 0.033).
Effects of training on postural stability
When inspecting the effect of training on postural stability using posturography, all groups showed significant improvements (). The muscle force training groups tended to improve most, followed by the self-training group and then the balance training group, but the differences were not statistically significant.
Table 2 Posturography measurements at 3 months from training in the muscle force, self-administered, and balance training groups
After training, the occurrence of “spiky” oscillations was reduced and the stationary fields of torque moment of the ankle increased, providing better stability. Postural strategy was changed in all groups so that the participants reduced their random body sway and started to oscillate around a predetermined attractor (neutral point), and tried to hold their posture without exceeding stability ranges. They did however sway to the same extent as before commencing the training when measured by means of sway velocity and area of body sway. In regard to the risk factors for falls, those participants who indicated problems with gait and mobility had significantly worsened postural stability. Within the ANOVA analysis, a model consisting of the zero crossing rate of weight signal and the number of low variability episodes in the stabilogram was significant (P < 0.001), and explained 16.5% of the variance of problems in mobility.
Associations with falls
In posturography the training groups differed in Romberg’s quotient with respect to falls in ANOVA (P < 0.01). Thus, non-fallers used visual information to stabilize their balance on the force platform; however, such a positive integration of visual and vestibular influxes was not seen in fallers.
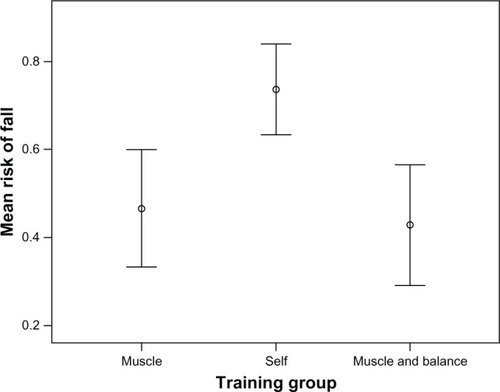
The participants with muscle force training and those with balance and muscle force training tended to have fewer falls than those with self-administered training (). The difference between the groups was statistically significant (Chi-square test, P = 0.02) (). However, in logistic regression analysis, only in habitual fallers did the posturography measures correlate with outcome in falls (number of low variability r = –0,466, P < 0.01; zero crossing rate of velocity signal in AP-direction r = 0.278, P < 0.05).
Table 3 Falls measured during 3 years of follow-up among participants in the muscle force, self-administered, and balance training groups
Figure 3 Observed falls in different training groups (mean value and standard error of the mean are shown).
There was no significant long-term effect of training on the death rate between the different groups. On average, the MMSE-index showed that global cognitive status was impaired in 29% of the study groups when training began, and in 79% after 3 years. The MMSE index neither correlated with the level of falls, training group nor the outcomes of posturography.
QoL
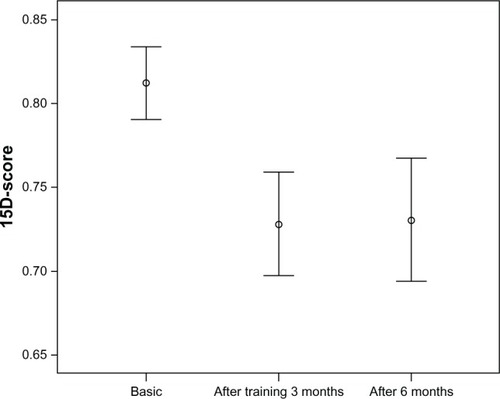
The 15D QoL was 0.8 at the beginning of training but was reduced to 0.71 as the training ended (paired Student’s t-test, P < 0.001) and 0.73 after 6 months (paired Student’s t-test, P < 0.001) (). No differences were observed in 15D measures between the different training groups (). When exploring the association between the 15D instrument and the outcome of posturography in ANOVA, we found significant association between postural stability and QoL (F = 11.4, P < 0.001, beta –0.587). A model explaining 46% of the variability in the 15D QoL consisted of the critical time (P < 0.001, beta –0.650) and the zero crossing rate of the weight signal (P < 0.024, beta 0.344).
Table 4 General HRQoL in different training groups and at different time points
Figure 4 15D quality of life scores before, immediately after cessation of training, and 6 months from the baseline measurements (mean and 95% confidence intervals are shown).
When analyzing internal factors of the 15D instrument, the mobility rating at the beginning and after training showed no significant changes. However, vitality scores significantly worsened immediately after training, but recovered after 6 months (Student’s t-test, P < 0.001). A similar observation was seen in analyzing the activity scores (Student’s t-test, P < 0.05) (). Participants also felt more weary, tired, or feeble than at the beginning of training (Student’s t-test, P < 0.001) (). No differences were found between the training groups.
Figure 5 Usual activities (left) and vitality (right) based on 15D scores in the beginning, immediately after cessation of the training, and after 6 months from baseline measurements (mean and 95% confidence intervals are shown).
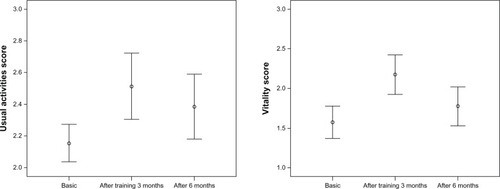
Figure 6 Depression score (left) and mental function score (right) derived from 15D QoL (quality of life) at the beginning of training, immediately after training, and 6 months after commencing the training (mean and 95% confidence levels are shown).
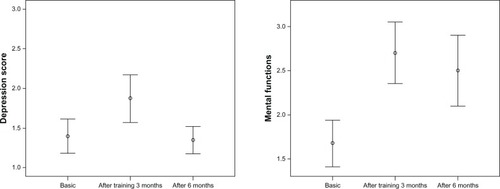
When investigating the effect of training on mood disorders and mental function, we used the depression and mental score questions. After the training period had ended, participants felt more depressed (Student’s t-test, P < 0.05) and impaired in mental functions (Student’s t-test, P < 0.001) than at the beginning of training; the depression scores returned to baseline levels 6 months after commencing the training ().
Discussion
We compared guided balance and muscle force training with self-administered training in older adults residing in an institutional setting. The postural stability was measured with a force platform, and general HRQoL measures were used. Residents with moderate or severe dementia could perform exercises in a five person group under the supervision of a physiotherapist. Personal nurses proved to be an effective resource on the ward when stimulating and encouraging the participants to keep up with their self-guided training. When inspecting the effect of training on postural stability, all groups showed significant improvements. The muscle force training groups tended to improve the most, followed by the self-training group and then the balance training group, although the differences were not statistically significant. Posturography revealed an improvement in postural stability and balance control strategy. The outcome of fall rates differed between the training groups; guided training was more effective than self-training. The training was associated with a reduced QoL. It is possible that the training efforts, although carefully controlled and individually tailored, proved too strenuous for the frail participants, and perhaps different protocols should be evaluated before any therapeutic recommendation can be made.
Postural stability on the force platform
In posturography, the center point of force has commonly been used to characterize the subject’s ability to control their posture. The conventional parameters used have failed to distinguish fallers from non-fallers in geriatric facilities. There are many possible explanations for this, including a shortage of optimal reference persons, that “near falls” are handled as non-falls, the stochastic nature of falls, and the shortage of descriptive parameters used in evaluation. In spite of these shortcomings however, posturography can be a useful instrument in describing the outcomes of rehabilitation. We have previously indicated that body sway is a random phenomenon in the elderly; this phenomenon contrasts with younger residents in whom body sway is predictive and seems to oscillate around an attractor.Citation21,Citation22 Interestingly, after 3 months of training we were able to show that participants regained the strategy to sway around an attractor. In this way they recalled their “postural memory” and could avoid falling to the outside of their stability area. In the variables analyzed with the zero crossing rate of weight signal, it is possible to detect transients in the stabilogram signal. The time delay between two zero crossings is usually small and quite constant. During the transients however, the time delay is greater. This time delay was reduced among the participants after training, and the number of zero crossing rates increased. In a time-domain, the zero crossing rate varies during measurement for reasons which are related to postural control strategy and other physical actions.Citation23 The zero crossing rate strategy will tend to keep the person in proximity to the selected attractor. An improvement in postural stability was not observed in traditional measures such as the velocity of body sway or sway area; however, an improvement was noted in strategy with a move towards diminishing periods of random body oscillations. This change of strategy will thus reduce postural effort.Citation21 Muscle force training is especially useful to prevent slips and falls but also improves the postural stability during quiet stance.
Rehabilitation of muscle force and balance
Preventing falls may require the selection of a population that is most likely to benefit from rehabilitation, as well as a selection of interventions.Citation24 Rubenstein et alCitation3 concluded in a review that lower-extremity weakness was a significant risk factor and increased the odds of falling about six-fold. Studies have reported that the prevalence of detectable lower-extremity weakness ranges from 48% among community-living older persons,Citation25 to 57% among residents of an intermediate care facility,Citation26 to more than 80% of residents of a skilled nursing facility.Citation27 We therefore focused part of the training on enhancing the strength of the lower extremities, and in the second group, we also looked to improve gait and balance. Participants of guided training had to be able to perform muscle force training, starting from levels of low strain and increasing the strain of exercises with time; this was not the case in the balance force training as they used a walking frame, and other balance training merely added to the muscle force training. However, both training regimes focused on the improvement of strength and use of the postural muscles. Theoretically, balance training should be more effective in changing the postural control strategy, but this was not the case based on our posturography analysis. Multifactorial interventions have been successful in some, but not all, fall prevention trials.Citation5,Citation9 Several studies favor using physiotherapy as a tool to prevent falls in older adults residing in an institutional setting.Citation28,Citation29 Common to all these studies was that they used balance training and walking exercises. In contrast, several other studies were unable to show that rehabilitation prevented falls in these subjects.Citation30,Citation31 The studies also used walking and endurance training, as used in the present study. While in some training programs balance improved, in others with similar training programs, no changes were seen.Citation32 Rapp et alCitation4 suggested that fallers represent cases with multiple different pathologies and that elderly people with certain symptom complexes respond better to rehabilitation than others. The training periods in previous studies were 1–3 times per week and did not explain the differences between the efficacies of fall prevention. Perhaps a better effect could be achieved by having shorter but more frequent interventions, which lasted throughout the year. This, however, demands resources drawn from the personnel of elderly homes to transport the patients to training units, and increases the number of rehabilitation personnel needed to perform the training. A further study should be attempted to optimize the weekly training periods.
When inspecting the efficacy of the training program to prevent falls, guided training was more efficient than self-training. The participants were quite passive, with only about half the subjects who were able to participate actually attending the study program. This may be a reflection of the development of a negative attitude when moving from one’s own apartment to the institutionalized setting. A change in such attitudes is needed; however, such a change appears difficult as it would require more in the way of personnel resources than the 0.5 nurses per bed currently regulated by law in Finland today.
Effect on QoL
General HRQoL measures can be used to compare the impact of different diseases and to evaluate the costs of illness.Citation19 Kato et alCitation33 suggested that taking account of mental confidence is important for physical QoL and that fall prevention self-efficacy (including not only the physical activity per se, but also mental confidence) should be given prominence in the physical QoL of the elderly. We demonstrated using the 15D instrument that psychological and physical components (mood, vitality, mental function, and regular day-to-day tasks) were altered after rehabilitation. Nevertheless, guided training produced significantly less falls. The risk of fall is also important in causing neuropsychiatric symptoms.Citation34 Unlike the present study, most intervention studies have been carried out among community-dwelling elderly, differing in age and physical and mental conditions. It seems that for the elderly there is a tradeoff between training exercises and QoL when it comes to rehabilitation. Supporting the importance of postural stability and QoL, we noticed that 17% of the variability of QoL was associated with a history of fall tendency and motility problems; postural stability measurements could explain 46% of the variability in the QoL data. This result provides additional perspectives on the use of sophisticated analysis of stabilograms among the elderly.
Training of previously passive elderly alters their daily routines and may be perceived as being excessive; this was seen as a reason for the reduction of psychological and physical dimensions in the present study. Although the elderly had a positive attitude towards rehabilitation, they experienced a level of fatigue that they could not recover from in time for the next training session. A less forceful regime of training amongst nursing home residents increased the QoL by improving their emotional functioning, vitality, and mental health;Citation35 however, fall outcomes were not documented. A softer start-up level of training and the inclusion of emotional support and attitude education could be used to avoid reductions in QoL by minimizing the effects of “post training fatigue”.
Conclusion
In the present study we compared guided exercises and self-administered training and their role in fall prevention in the elderly. Guided exercises carried out twice a week focused on increasing muscle strength and balance. Elderly with moderate or severe dementia could undertake exercises as part of five person groups, under the supervision of a physiotherapist, and with personal nurses overseeing the self-training participants. After 3 months of training, participants in all groups improved their postural stability. Using posturography, we observed that training induced previously used control strategies for posture; elderly residents started to oscillate around a predetermined attractor and in this vein rejuvenated their postural control. Guided training tended to reduce the number of falls when compared to self-administered training. However, we observed that the QoL of residents was reduced after the training had ended, in terms of mood, mental functions, vitality, and usual activities. This indicated that the training program was perhaps perceived to be too laborious. A further study should be carried out to reveal the differences between guided and self-training efforts with a less strenuous training program, so as to avoid consequences adverse to QoL. We conclude that in residential homes, efforts should be made to increase guided muscle force training, but that training activities should be moderate. Additionally, self-training could be used as a daily supplement to a guided training program.
Acknowledgments
This work has been carried out with the kind collaboration of the personnel of the Koukkuniemi Residential Home in Tampere, Finland. We acknowledge Jussi Ripsaluoma, the chief physician of the residential home, for providing the facilities in which to conduct the study. Financial support for this study was provided by EU PROFANE (Prevention of Falls Network, Europe) and the Pirkanmaa Cultural and Science Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
- KorhonenNNiemiSParkkariJPalvanenMKannusPUnintentional injury deaths among adult Finns in 1971–2008Injury201142988588820851395
- BakerSPHarveyAHFall injuries in the elderlyClin Geriatr Med1985135015123913506
- RubensteinLZJosephsonKRRobbinsASFalls in the nursing homeAnn Intern Med199412164424518053619
- RappKLambSEErhardt-BeerLEffect of a statewide fall prevention program on incidence of femoral fractures in residents of long-term care facilitiesJ Am Geriatr Soc2010581707520002505
- VaapioSSSalminenMJOjanlatvaAKivelaSLQuality of life as an outcome of fall prevention interventions among the aged: a systematic reviewEur J Public Health200919171518971207
- EraPSainioPKoskinenSHaavistoPVaaraMAromaaAPostural balance in a random sample of 7,979 subjects aged 30 years and overGerontology200652420421316849863
- RaskuJPyykköIJuholaMEvaluation of the postural stability of elderly persons using time domain signal analysisJ Vestib Res2012225–624325223302705
- KerberKAEnriettoJAJacobsonKMBalohRWDisequilibrium in older people: a prospective studyNeurology19985125745809710038
- KingmaHGauchardGCde WaeleCStocktaking on the development of posturography for clinical useJ Vestib Res201121311712521558637
- VisserJECarpenterMGvan der KooijHBloemBRThe clinical utility of posturographyClin Neurophysiol2008119112424243618789756
- RaskuJA method for the classification of corrective activity in context dependent postural controlling tasksComput Biol Med2009391094094519665113
- GillespieWJGillespieLDHandollHHMadhokRThe Cochrane Musculoskeletal Injuries GroupActa Orthop Scand Suppl200273305151912545658
- NeyensJCvan HaastregtJCDijcksBPEffectiveness and implementation aspects of interventions for preventing falls in elderly people in long-term care facilities: a systematic review of RCTsJ Am Med Dir Assoc201112641042521450201
- GillespieLDRobertsonMCGillespieWJInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20129CD00714622972103
- TuunainenEMoisio-VileniusPMäkinenERaskuJToppilaEPyykköIIntervention to prevent falls in elderly living in residential homeJournal of Amderican Geriatric Society2013 In Press
- KentalaEPyykköIAuramoYJuholaMOtoneurological expert systemAnn Otol Rhinol Laryngol199610586546588712638
- KentalaEPyykköIAuramoYLaurikkalaJJuholaMOtoneurological expert system for vertigoActa Otolaryngol19991195517521
- FolsteinMFFolsteinSEMcHughPR“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res19751231891981202204
- SaarniSIHarkanenTSintonenHThe impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5DQual Life Res20061581403141416960751
- PyykköIJänttiPAaltoHPostural control in elderly subjectsAge Ageing19901932152212363386
- ToppilaEPyykköIChaotic model of postural stability-a position and velocity dependent systemAutomedica2000196399
- RaskuJJuholaMTossavainenTPyykkoIToppilaEModelling stabilograms with hidden Markov modelsJ Med Eng Technol200832427328318666007
- PrietoTEMyklebustJBHoffmannRGLovettEGMyklebustBMMeasures of postural steadiness: differences between healthy young and elderly adultsIEEE Trans Biomed Eng19964399569669214811
- Guideline for the prevention of falls in older personsAmerican Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls PreventionJ Am Geriatr Soc200149566467211380764
- CampbellAJRobertsonMCImplementation of multifactorial interventions for fall and fracture preventionAge Ageing200635Suppl 2ii60ii6416926208
- TinettiMEPerformance-oriented assessment of mobility problems in elderly patientsJ Am Geriatr Soc19863421191263944402
- RobbinsASRubensteinLZJosephsonKRSchulmanBLOsterweilDFineGPredictors of falls among elderly people. Results of two population-based studiesArch Intern Med19891497162816332742437
- BeckerCKronMLindemannUEffectiveness of a multifaceted intervention on falls in nursing home residentsJ Am Geriatr Soc3200351330631312588573
- SihvonenSSipiläSTaskinenSEraPFall incidence in frail older women after individualized visual feedback-based balance trainingGerontology200450641141615477703
- McMurdoMEMillarAMDalyFA randomized controlled trial of fall prevention strategies in old peoples’ homesGerontology2000462838710671804
- ShimadaHObuchiSFurunaTSuzukiTNew intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmillAm J Phys Med Rehabil200483749349915213472
- SchoenfelderDPA fall prevention program for elderly individuals. Exercise in long-term care settingsJ Gerontol Nurs2000263435111111630
- KatoCIdaKKawamuraMRelation of falls efficacy scale (FES) to quality of life among nursing home female residents with comparatively intact cognitive function in JapanNagoya J Med Sci2008701–2192718807292
- LinMRWolfSLHwangHFGongSYChenCYA randomized, controlled trial of fall prevention programs and quality of life in older fallersJ Am Geriatr Soc200755449950617397426
- BruyereOWuidartMADi PalmaEControlled whole body vibration to decrease fall risk and improve health-related quality of life of nursing home residentsArch Phys Med Rehabil200586230330715706558