Abstract
Eldecalcitol (1α, 25-dihydroxy-2β-[3-hydroxypropyloxy] vitamin D3; ED-71) is a new analog of the active form of vitamin D. Eldecalcitol has recently been approved for the treatment of osteoporosis in Japan. In addition to regulation of calcium metabolism carried out by conventional vitamin D analogs, eldecalcitol possesses a strong inhibitory effect on bone resorption and causes a significant increase in bone mineral density. A Phase III clinical trial on osteoporosis showed that eldecalcitol reduced the incidence of new vertebral fractures over 3 years by 26% compared with alfacalcidol. Although the overall risk of nonvertebral fractures was not reduced by eldecalcitol, the risk of wrist fracture was decreased significantly in the eldecalcitol group (71%) compared with the alfacalcidol group. The serum level of 25-hydroxyvitamin D (25[OH]D) was normalized by supplementation of native vitamin D in this trial, so the desirable effects on bone by eldecalcitol were considered to be derived from its distinctive pharmacological action. Increased blood calcium was observed in 21% of patients treated with eldecalcitol, and hypercalcemia (>11.5 mg/dL) occurred in 0.4% of eldecalcitol recipients, so serum calcium concentration should be monitored after starting eldecalcitol treatment. Eldecalcitol has dual effects on the metabolism of bone and calcium and is useful for the treatment of osteoporosis, especially for elderly patients (who frequently suffer from vitamin D deficiency). This article reviews the clinical efficacy and safety of eldecalcitol in the treatment of osteoporosis.
Introduction
Osteoporosis is a systemic skeletal disease associated with low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and fracture risk.Citation1 Osteoporosis-related fractures occur commonly in the spine, hip and distal radius. These fractures impact negatively on quality of life and increase morbidity and mortality.Citation2,Citation3 Treatment of osteoporosis is important for preventing osteoporotic fractures and reducing the health care burden.
Vitamin D is a crucial factor for the intestinal absorption of calcium to maintain bone strength. A deficiency in vitamin D causes impaired absorption of calcium and bone mineralization, leading to rickets in children and osteomalacia in adults.Citation4–Citation6 The elderly are at risk of a deficiency and an insufficiency of vitamin D because of their reduced mobility and consequent decreased exposure to sunshine, a low food intake, and decline in renal function.Citation4,Citation7 Vitamin D insufficiency causes greater secretion of parathyroid hormone (PTH) due to the low serum levels of calcium and active vitamin D, resulting in high bone turnover and increased bone resorption. Vitamin D insufficiency is also associated with muscle weakness, leading to an increased risk of falling.Citation8,Citation9 These detrimental effects may contribute to osteoporosis and increased fracture risk in patients with a deficiency and an insufficiency of vitamin D.Citation10
Clinical trials have suggested that the active form of vitamin D reduces the risk of fractures and falls.Citation11–Citation13 A new analog of vitamin D, eldecalcitol, has recently been approved for the treatment of osteoporosis in Japan. Eldecalcitol has strong effects on the reduction of bone resorption and increase in bone mineral density (BMD) in addition to the effects on calcium metabolism retained by conventional vitamin D analogs.Citation14,Citation15
Vitamin D
Metabolism and action
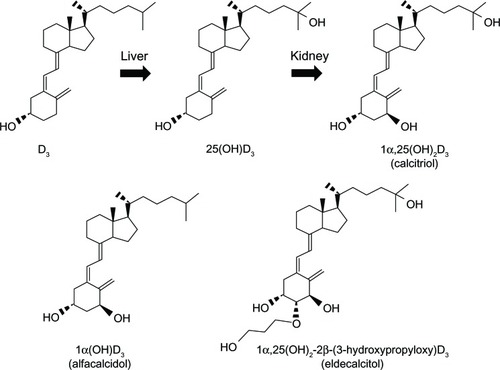
Vitamin D is one of the lipid-soluble hormones produced in the skin through ultraviolet irradiation of 7-dehydroc-holesterol. Vitamin D is also obtained from animal-based (vitamin D3) or plant-based (vitamin D2) foods.Citation10,Citation16 In the human body, vitamin D is hydroxylated in the liver to 25-hydroxyvitamin D (25[OH]D) and subsequently in the kidney to its biologically active form: 1,25-dihydroxyvitamin D (1,25[OH]2D) ().Citation16,Citation17 In the circulation, these vitamin D metabolites (25[OH]D and 1,25[OH]2D) are bound to vitamin D-binding protein (DBP). The active metabolite 1,25(OH)2D enters the cell and binds to the vitamin D receptor (VDR), which belongs to the nuclear receptor superfamily. This ligand-bound VDR forms a heterodimer with the retinoid X receptor (RXR). The VDR/RXR complex binds to the vitamin D-responsive element on a target gene to regulate its transcription. Vitamin D regulates serum concentrations of calcium and phosphate by increasing intestinal absorption of calcium and phosphate, promoting renal reabsorption of calcium, and stimulating bone resorption.Citation16,Citation18
Vitamin D deficiency and osteoporosis
The serum level of 25(OH)D is the best indicator of vitamin D status.Citation19,Citation20 Vitamin D deficiency is defined as a 25(OH)D level <20 ng/mL (50 nmol/L) and vitamin D insufficiency as a 25(OH)D level of 21–29 ng/mL (52.5–72.5 nmol/L).Citation4,Citation20 Deficiency/insufficiency of vitamin D is very common in elderly people due to their low intake of vitamin D, decreased exposure to sunlight, and impaired renal function. More than one-half of postmenopausal women have a 25(OH)D level <30 ng/mL.Citation21,Citation22
Severe vitamin D deficiency can cause rickets in children and osteomalacia in adults, characterized by impaired bone mineralization.Citation9,Citation10 Conversely, deficiency/insufficiency of vitamin D causes a decrease in the serum concentration of calcium due to a reduction in intestinal absorption of calcium. This hypocalcemia stimulates PTH secretion (secondary hyperparathyroidism), resulting in an increase in bone resorption and decrease of BMD. This may contribute to the pathogenesis of osteoporosis.Citation19,Citation20 Vitamin D deficiency is also associated with muscle weakness, leading to an increased risk of falling and fractures.Citation8,Citation9 A significant correlation between the serum concentration of 25(OH)D and falls in elderly people has been reported.Citation23–Citation25
Active form of vitamin D for the treatment of osteoporosis
The active form of vitamin D (1α,25-dihydroxyvitamin D3, calcitriol) and its prodrug (1α-hydroxyvitamin D3, alfacalcidol) have been approved for the treatment of osteoporosis in Japan ().Citation26 Both calcitriol and alfacalcidol showed a modest increase in BMD,Citation27,Citation28 and reduced the risk of vertebral and nonvertebral fractures.Citation11,Citation12,Citation29 The number of falls were also reduced by treatment with active vitamin D analogs.Citation13,Citation28–Citation30 Meta-analyses suggest that the vitamin D analogs (alfacalcidol and calcitriol) are more effective in preventing bone loss, fractures, and falls compared with native vitamin D.Citation12,Citation31
Eldecalcitol
Eldecalcitol: a new, active vitamin D analog
Eldecalcitol (1α, 25-dihydroxy-2β-[3-hydroxypropyloxy] vitamin D3, ED-71) has a hydroxypropyloxy group at the 2β-position of 1,25(OH)2D3, which has been isolated from >900 vitamin D analogs, based on the activity that stimulated BMD in vivo ().Citation14,Citation15,Citation32,Citation33 Compared with 1,25(OH)2D3, eldecalcitol has a higher affinity for serum DBP, binds more weakly to VDR, and shows lower potency in suppression of serum PTH ().Citation32–Citation35 The plasma half-life of eldecalcitol is longer than that of 1,25(OH)2D3, probably due to the higher affinity for DBP.
Table 1 Biological evaluation of eldecalcitol
Preclinical studies
In ovariectomized (OVX) animal models of osteoporosis, eldecalcitol suppressed osteoclastic bone resorption and increased BMD to a greater extent than alfacalcidol. There was no significant difference in calcium absorption and serum PTH suppression between eldecalcitol and alfacalcidol, so the effect of increasing BMD by eldecalcitol seems to be independent of calcium metabolism.Citation36 Eldecalcitol also prevented glucocorticoid-induced alterations in bone metabolism by increasing intestinal absorption of calcium, reducing osteoclastic bone resorption, and enhancing mineralization in rats.Citation37 Histological and histomorphological analyses revealed that eldecalcitol and alfacalcidol reduced osteoclast numbers and diminished osteoclastic activity/function without promoting osteoclast apoptosis in OVX rats.Citation36,Citation38 It has been shown that administration of eldecalcitol preferentially suppressed the expression of receptor activator of nuclear factor kappa B ligand (RANKL) in osteoblast-lineage cells around the trabecular bone compared with 1,25(OH)2D3.Citation39 Eldecalcitol and alfacalcidol dose-dependently stimulated focal bone formation that started without prior bone resorption (bone minimodeling).Citation40,Citation41 Reduction of bone resorption and stimulation of focal bone formation were more clearly observed in eldecalcitol-treated rats than in 1,25(OH)2D3-treated rats.Citation39,Citation41
Combination treatment of eldecalcitol with alendronate or raloxifene in OVX rats
In OVX rats, the combination of alendronate and eldecalcitol improved the mechanical properties of the lumbar spine and mid-shaft femur by additive suppression of bone resorption while maintaining bone formation, which was more beneficial than monotherapy with alendronate or eldecalcitol.Citation42 The combination of alendronate and eldecalcitol had a more beneficial antiosteoporotic effect by inhibiting osteoclastic bone resorption and maintaining osteoblastic function, compared with combination treatment with alendronate and alfacalcidol.Citation43 Combination treatment with eldecalcitol and raloxifene improved bone mechanical strength in OVX rats more than either type of monotherapy by increasing BMD and suppressing bone turnover.Citation44
Clinical studies
Pharmacokinetics and pharmacology
A single dose of eldecalcitol (0.75 μg) was administered to 32 healthy men while fasting. The vitamin D analog was absorbed rapidly and eliminated gradually from serum, with a mean time to maximum drug concentration (Tmax) of ~3.4 hours and a mean half-life (t1/2) of ~53 hours.Citation45 The time courses of serum eldecalcitol concentrations with administration while fasting and after a meal were similar. With multiple dosing, the serum eldecalcitol concentration reached steady state by 13 days after the first dose. The pharmacokinetics of eldecalcitol were linear in the dose range 0.1–1.0 μg.Citation45
To compare the effects of eldecalcitol and alfacalcidol on the metabolism of bone and calcium, a randomized open-label clinical trial was conducted in 59 post-menopausal women. Eldecalcitol could effectively inhibit bone resorption more strongly than alfacalcidol with a similar effect on bone formation and a comparable effect on urinary excretion of calcium.Citation46
Phase II studies
In an early Phase II clinical trial, a randomized controlled study with eldecalcitol was conducted with 109 osteoporotic subjects. The patients were assigned randomly to 0.25, 0.5, 0.75, or 1.0 μg/day of eldecalcitol administered via the oral route for 6 months. Eldecalcitol increased lumbar BMD in a dose-dependent manner without causing hypercalcemia or hypercalciuria. Eldecalcitol also exhibited a dose-dependent suppression of a bone resorption marker (urinary deoxypyridinoline) without a significant reduction in osteocalcin.Citation47,Citation48
Many patients have serum 25(OH)D levels <20 ng/mL. Hence, the effect of eldecalcitol on bone mass might be influenced by vitamin D insufficiency and could merely reflect a nutritional supplementary effect of vitamin D insufficiency. To solve this problem, a randomized double-blind placebo-controlled clinical trial was conducted with 219 osteoporotic patients under vitamin D supplementation (200 or 400 IU/day). Subjects were assigned randomly to receive 0.5, 0.75, or 1.0 μg/day of eldecalcitol for 12 months. After treatment with eldecalcitol for 12 months, lumbar spine BMD increased from baseline by 2.2%, 2.6%, and 3.1% in the 0.5, 0.75, and 1.0 μg eldecalcitol groups, respectively; whereas, lumbar spine BMD decreased by 0.7% in the placebo group. Total hip BMD also increased with 0.75 and 1.0 μg eldecalcitol from baseline by 0.6% and 0.9%, respectively. Conversely, in the placebo and 0.5 μg eldecalcitol group, total hip BMD decreased slightly from baseline (−0.9% and −0.8%). Markers of bone formation and resorption were suppressed by ≈20% after 12 months of treatment with 0.75 and 1.0 μg eldecalcitol. Transient increase in serum calcium level < 10.4 mg/dL (<2.6 mmol/L) occurred in 7%, 5%, and 23% of subjects in the 0.5, 0.75, and 1.0 μg eldecalcitol groups, respectively; but none of them developed sustained hypercalcemia.Citation49 Post hoc analyses of the trial revealed that eldecalcitol could increase lumbar and hip BMD in osteoporotic patients, regardless of their vitamin D status.Citation50 These results suggest that eldecalcitol can exert its effect on bone independently of the nutritional supplementation with native vitamin D.
Phase III studies
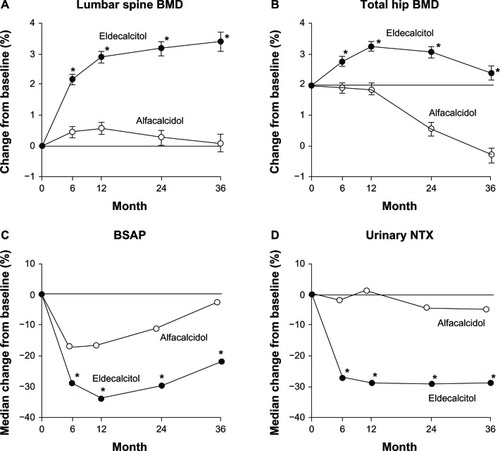
Based on the results of Phase II clinical studies, a 3-year, randomized, double-blind, active comparator, superiority trial was carried out to compare the effect of eldecalcitol (0.75 μg/day) with that of alfacalcidol (1 μg/day) in preventing fractures in patients with osteoporosis.Citation51 A total of 1,054 patients aged 46–92 years (mean, 72.1 years) were assigned randomly to receive eldecalcitol (n = 528) or alfacalcidol (n = 526). Patients with low serum levels of 25(OH)D (<20 ng/mL) were supplemented with 400 IU/day of vitamin D3. Compared with the alfacalcidol group, the incidence of vertebral fractures was lower in the eldecalcitol group after 36 months of treatment (13.4% versus 17.5%) with a relative risk reduction of 26% (P = 0.092; hazard ratio [HR] 0.74; 90% confidence interval [CI]: 0.56–0.97) (). The incidence of new vertebral fractures was not different between the two groups during the first year, but was significantly lower in the eldecalcitol group during the third year (3.9% versus 7.0%, odds ratio [OR] 0.51, P = 0.037; 95% CI 0.27–0.97). With regard to the total number of nonvertebral fractures at 36 months, no significant difference was observed between the eldecalcitol and alfacalcidol groups (8.0% versus 9.5%, HR 0.85, 95% CI 0.55–1.31). However, eldecalcitol reduced the incidence of three major nonvertebral fractures (humerus, wrist, hip) compared with alfacalcidol (2.5% versus 4.9%, HR 0.51, 95% CI 0.25–1.03), which was due, in particular, to a marked decrease in the incidence of wrist fractures (1.1% versus 3.6%, HR 0.29, 95% CI 0.11–0.77, P = 0.009) (). Eldecalcitol increased lumbar and hip BMD more strongly than alfacalcidol (). Levels of bone turnover markers (bone-specific alkaline phos-phatase [BSAP] and urinary crosslinked N-telopeptide of type-I bone collagen [NTX]) were significantly lower with eldecalcitol than with alfacalcidol (). The decrease from baseline in bone turnover markers after the eldecalcitol treatment exceeded the minimum significant change, authorized by the Japan Osteoporosis Society.Citation52 These results suggest that eldecalcitol is more efficacious than alfacalcidol in preventing vertebral and wrist fractures in osteoporotic patients.Citation51
Figure 2 Incidence of new vertebral fractures in the alfacalcidol (1.0 μg/day) group and the eldecalcitol (0.75 μg/day) group during the 3-year study period. Kaplan–Meier estimates of the incidence of new vertebral fractures.
Adapted from Matsumoto T, Ito M, Hayashi Y, et al. A new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures – a randomized, active comparator, double-blind study. Bone. 2011;49(4):605–612, with permission from Elsevier.Citation51
Abbreviation: CI, confidence interval.
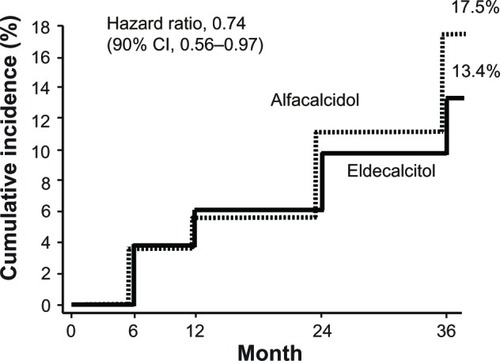
Figure 3 Incidence of all nonvertebral fractures, nonvertebral fractures at three major sites (humerus, wrist, hip), and wrist fracture in the alfacalcidol (1.0 μg/day) group and the eldecalcitol (0.75 μg/day) group during the 3-year study period.
Notes: *P = 0.009. Data from.Citation51
Abbreviations: HR, hazard ratio; CI, confidence interval.
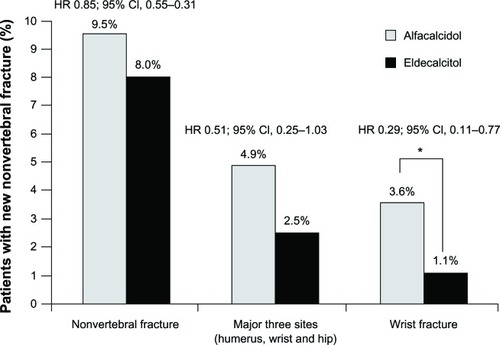
Figure 4 Effects of eldecalcitol and alfacalcidol on BMD (A and B) and bone turnover markers (C and D) during the 3-year study period.
Adapted from Matsumoto T, Ito M, Hayashi Y, et al. A new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures – a randomized, active comparator, double-blind study. Bone. 2011;49(4):605–612, with permission from the Elsevier.Citation51
Abbreviations: BMD, bone mineral density; BSAP, bone-specific alkaline phosphatase; NTX, urinary N-terminal propeptide of type I collagen; SE, standard error.
Among the adverse events, the prevalence of an increase in serum and urinary levels of calcium was higher in the eldecalcitol group compared with the alfacalcidol group (). Increased serum calcium was observed in 21.0% of eldecalcitol recipients and 13.5% of alfacalcidol recipients, while hypercalcemia developed in two patients (0.4%) in the eldecalcitol group but none in the alfacalcidol group. There was no significant difference in the prevalence of urolithiasis and in the estimated glomerular filtration rate between the two groups.Citation51
Table 2 Incidence of adverse events
Post hoc analyses of the Phase III study
Post hoc analyses of the Phase III study revealed that the incidence of vertebral fracture at the lower spine was lower in the eldecalcitol group than in the alfacalcidol group (P = 0.029). The incidence of severe vertebral fractures (grade III) was lower in the eldecalcitol group than in the alfacalcidol group (3.8% versus 6.7%; HR, 0.53; 95% CI, 0.29–0.96; P = 0.036). Eldecalcitol and alfacalcidol improved health-related quality of life (HRQoL) scores, but overall improvement from the baseline of HRQoL scores was observed clearly in the eldecalcitol group.Citation53
Eldecalcitol reduced the incidence of osteoporotic fractures, as defined by the World Health Organization, more than alfacalcidol (18.6% versus 25.2%; HR, 0.70; 90% CI, 0.54–0.93; P = 0.013) and decreased the risk of major osteoporotic fractures included in the Fracture Risk Assessment Tool (FRAX)Citation54 (11.1% versus 16.3%; HR, 0.66; 95% CI, 0.46–0.94; P = 0.020). A significant decrease in the incidence of nonvertebral fractures was also observed in the eldecalcitol group.Citation55
To ascertain if eldecalcitol can cause severely suppressed bone turnover, post hoc analyses of the Phase III trial about the changes in bone turnover markers after eldecalcitol treatment in osteoporotic patients were undertaken. Eldecalcitol reduced markers of bone turnover rapidly and kept them within the normal range. In patients whose baseline values for bone turnover markers were low, eldecalcitol treatment did not reduce the bone turnover markers further during a 3-year treatment period.Citation56
The effects of eldecalcitol on bone geometry and the biomechanical properties of the proximal femur were investigated by computed tomography in a subgroup of the Phase III study (n = 193). Longitudinal analyses of hip geometry revealed the advantages of eldecalcitol over alfa-calcidol in: increased cortical cross-sectional area; volumetric BMD of the neck and shaft of the femur; bone mass; and maintenance of cortical thickness (probably through mitigating endocortical bone resorption). By improving the biomechanical properties of the proximal femur, eldecalcitol could reduce the risk of hip fracture.Citation57
Place of eldecalcitol in the treatment of osteoporosis
The vitamin D analogs alfacalcidol and calcitriol have been used for the treatment of osteoporosis in Japan. However, these drugs are not used as first-line therapy for osteoporosis, because they have weaker inhibitory effects on fractures than bisphosphonates, selective estrogen receptor modulators, or teriparatide. The new active form of vitamin D, eldecalcitol, has stronger effects on the inhibition of bone resorption, increases BMD, and prevents osteoporotic fractures compared with alfacalcidol. It has been reported that native and active vitamin D reduced the risk of falling among older individuals.Citation13 There are no data regarding the efficacy of eldecalcitol for preventing falls, but marked inhibition of wrist fractures by eldecalcitol may be explained (at least in part) by the preventive effects of the drug on falling. Moreover, it has recently been noted that low serum levels of vitamin D are associated with several adverse outcomes in the musculoskeletal, innate immune, and cardiovascular systems; and they are also associated with increased all-cause mortality.Citation19,Citation20 Eldecalcitol has effects on the metabolism of bone and calcium and may prevent falling, so multiple improvements in patients with osteoporosis can be expected with only one drug, which may lead to a reduction in the health care burden. Eldecalcitol would be preferable, especially for elderly people with osteoporosis, because of the high prevalence of vitamin D deficiency. It has recently been indicated that children, young adults, and middle-age adults are at an equally high risk for vitamin D deficiency/insufficiency,Citation4,Citation20 so osteoporosis in young people may also be a target for treatment with eldecalcitol.
In preclinical studies using OVX rats, favorable results have been obtained upon combination treatment of eldecalcitol with alendronate or raloxifene. Clinical studies have indicated the advantages of combination therapy with alfacalcidol and alendronate for the prevention of osteoporosis-related fractures.Citation58,Citation59 In the post hoc analyses of the Phase III trial, eldecalcitol normalized and did not overly suppress bone turnover – even in patients with low pretreatment levels of bone turnover markers.Citation56 These results may raise expectation of combined therapy with eldecalcitol and antiresorptive agents; however, clinical data for the combined therapy – including eldecalcitol – have not been available to date. Future clinical studies regarding the combination treatment of eldecalcitol with other drugs for osteoporosis are required.
The precise pharmacological action of the active form of vitamin D on bone metabolism is not fully understood. It has been shown that c-Fos and RANKL may be the targets of the action of vitamin D.Citation39,Citation60 Although eldecalcitol and 1,25(OH)2D3 are known to enhance RANKL expression in vitro, eldecalcitol suppresses the expression of RANKL in osteoblast-lineage cells and reduces the bone resorption in vivo.Citation39,Citation40 This discrepancy between in vitro and in vivo studies has not been fully explained. Recent histological analyses in OVX rats revealed that the preosteoblastic layer, with which osteoclastic precursors interact for mutual differentiation, was poorly developed in eldecalcitol-treated rats.Citation40 Eldecalcitol also promoted focal bone formation, known as bone minimodeling, which is independent of bone resorption. The increased macrophage number and the decreased osteoclast number in the bone marrow of eldecalcitol-treated rats were also observed.Citation40 It has also been reported that RANKL was expressed preferentially by immature osteoblasts, and the expression level decreased during their maturation.Citation61 Based on these results, eldecalcitol may force osteoblast maturation and prevent cell-to-cell interaction between preosteoblasts and osteoclastic precursors, leading to lower osteoclast number and decreased bone resorption.
A recent study revealed that the active form of vitamin D, including eldecalcitol, significantly suppressed the expression of bone tropic S1PR2 in circulating osteoclast precursor monocytes. As a result, mobilization of the osteoclast precursor monocytes from the bone to the blood was enhanced, causing a suppression of bone resorption.Citation62
Conclusion
Eldecalcitol possesses a strong inhibitory effect on bone resorption and causes a significant increase in BMD. Phase III clinical trials revealed that the incidence of vertebral and wrist fractures was significantly reduced in the eldecalcitol group compared with the alfacalcidol group. To date, eldecalcitol is not available outside of Japan. Therefore, all clinical trials have been conducted in Japan. This unique vitamin D analog is thought to be useful, especially for patients with osteoporosis and vitamin D deficiency. Approval of the drug for osteoporosis treatment in other countries is expected. Increases in blood and urinary levels of calcium were the most frequent adverse events in the treatment with eldecalcitol, though hypercalcemia was observed in only a few patients. Blood and urinary calcium should be monitored during eldecalcitol treatment. Large-scale clinical trials that compare the effects of eldecalcitol with other drugs for osteoporosis, as well as evaluation of combination therapy, should be carried out.
Disclosure
The authors report no conflicts of interest in this work.
References
- No authors listedConsensus development conference: diagnosis, prophylaxis, and treatment of osteoporosisAm J Med19939466466508506892
- CauleyJAThompsonDEEnsrudKCScottJCBlackDRisk of mortality following clinical fracturesOsteoporos Int200011755656111069188
- BianchiMLOrsiniMRSaraifogerSOrtolaniSRadaelliGBettiSQuality of life in post-menopausal osteoporosisHealth Qual Life Outcomes200537816321148
- HolickMFVitamin D deficiencyN Engl J Med2007357326628117634462
- PeacockMCalcium metabolism in health and diseaseClin J Am Soc Nephrol20105Suppl 1S23S3020089499
- KennelKADrakeMTHurleyDLVitamin D deficiency in adults: when to test and how to treatMayo Clin Proc201085875275720675513
- LipsPBouillonRvan SchoorNMReducing fracture risk with calcium and vitamin DClin Endocrinol (Oxf)201073327728520796001
- JanssenHCSamsonMMVerhaarHJVitamin D deficiency, muscle function, and falls in elderly peopleAm J Clin Nutr200275461161511916748
- HolickMFResurrection of vitamin D deficiency and ricketsJ Clin Invest200611682062207216886050
- LipsPVitamin D physiologyProg Biophys Mol Biol20069214816563471
- PapadimitropoulosEWellsGSheaBOsteoporosis Methodology Group and The Osteoporosis Research Advisory GroupMeta-analyses of therapies for postmenopausal osteoporosis. VIII: Meta-analysis of the efficacy of vitamin D treatment in preventing osteoporosis in postmenopausal womenEndocr Rev200223456056912202471
- O’DonnellSMoherDThomasKHanleyDACranneyASystematic review of the benefits and harms of calcitriol and alfacalcidol for fractures and fallsJ Bone Miner Metab200826653154218979152
- Bischoff-FerrariHADawson-HughesBStaehelinHBFall prevention with supplemental and active forms of vitamin D: a metaanalysis of randomised controlled trialsBMJ2009339b369219797342
- SanfordMMcCormackPLEldecalcitol: a review of its use in the treatment of osteoporosisDrugs201171131755177021902297
- MatsumotoTEndoIEldecalcitol for the treatment of osteoporosisDrugs Today (Barc)201248318919622462038
- DeLucaHFOverview of general physiologic features and functions of vitamin DAm J Clin Nutr200480Suppl 61689S1696S15585789
- HolickMFSunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular diseaseAm J Clin Nutr200480Suppl 61678S1688S15585788
- HausslerMRWhitfieldGKKanekoIMolecular mechanisms of vitamin D actionCalcif Tissue Int2013922779822782502
- AdamsJSHewisonMUpdate in vitamin DJ Clin Endocrinol Metab201095247147820133466
- HolickMFBinkleyNCBischoff-FerrariHAGuidelines for preventing and treating vitamin D deficiency and insufficiency revisitedJ Clin Endocrinol Metab20129741153115822442274
- HolickMFSirisESBinkleyNPrevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapyJ Clin Endocrinol Metab20059063215322415797954
- LipsPHoskingDLippunerKThe prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigationJ Intern Med2006260324525416918822
- MowéMHaugEBøhmerTLow serum calcidiol concentration in older adults with reduced muscular functionJ Am Geriatr Soc19994722202269988294
- SteinMSWarkJDSchererSCFalls relate to vitamin D and parathyroid hormone in an Australian nursing home and hostelJ Am Geriatr Soc199947101195120110522952
- Bischoff-FerrariHADawson-HughesBWillettWCEffect of Vitamin D on falls: a meta-analysisJAMA2004291161999200615113819
- OrimoHNakamuraTHosoiTJapanese 2011 guidelines for prevention and treatment of osteoporosis – executive summaryArch Osteoporos201271–232023203733
- ShikariMKushidaKYamazakiKNagaiTInoueTOrimoHEffects of 2 years’ treatment of osteoporosis with 1 alpha-hydroxy vitamin D3 on bone mineral density and incidence of fracture: a placebo-controlled, double-blind prospective studyEndocr J19964322112209026268
- GallagherJCFowlerSEDetterJRShermanSSCombination treatment with estrogen and calcitriol in the prevention of age-related bone lossJ Clin Endocrinol Metab20018683618362811502787
- RingeJDSchachtEPotential of alfacalcidol for reducing increased risk of falls and fracturesRheumatol Int200929101177118519159932
- DukasLBischoffHALindpaintnerLSAlfacalcidol reduces the number of fallers in a community-dwelling elderly population with a minimum calcium intake of more than 500 mg dailyJ Am Geriatr Soc200452223023614728632
- RichyFSchachtEBruyereOEthgenOGourlayMReginsterJYVitamin D analogs versus native vitamin D in preventing bone loss and osteoporosis-related fractures: a comparative meta-analysisCalcif Tissue Int200576317618615692726
- OkanoTTsugawaNMasudaSRegulatory activities of 2 beta-(3-hydroxypropoxy)-1 alpha, 25-dihydroxyvitamin D3, a novel synthetic vitamin D3 derivative, on calcium metabolismBiochem Biophys Res Commun19891633144414492551289
- TakahashiNMechanism of inhibitory action of Eldecalcitol, an active vitamin D analog, on bone resorption in vivoJ Steroid Biochem Mol Biol201313617117423220095
- HatakeyamaSNagashimaSImaiNSynthesis and biological evaluation of a 3-positon epimer of 1alpha,25-dihydroxy-2beta-(3-hydroxypropoxy)vitamin D3 (ED-71)J Steroid Biochem Mol Biol20071033–522222617207991
- HaradaSTakedaSUnoATakahashiFSaitoHEldecalcitol is less effective in suppressing parathyroid hormone compared to calcitriol in vivoJ Steroid Biochem Mol Biol20101211–228128320398764
- UchiyamaYHiguchiYTakedaSED-71, a vitamin D analog, is a more potent inhibitor of bone resorption than alfacalcidol in an estrogen-deficient rat model of osteoporosisBone200230458258811934649
- TanakaYNakamuraTNishidaSEffects of a synthetic vitamin D analog, ED-71, on bone dynamics and strength in cancellous and cortical bone in prednisolone-treated ratsJ Bone Miner Res19961133253368852943
- ShiraishiAHigashiSOhkawaHThe advantage of alfacalcidol over vitamin D in the treatment of osteoporosisCalcif Tissue Int199965431131610485984
- HaradaSMizoguchiTKobayashiYDaily administration of eldecalcitol (ED-71), an active vitamin D analog, increases bone mineral density by suppressing RANKL expression in mouse trabecular boneJ Bone Miner Res201227246147322052469
- de FreitasPHHasegawaTTakedaSEldecalcitol, a second-generation vitamin D analog, drives bone minimodeling and reduces osteoclastic number in trabecular bone of ovariectomized ratsBone201149333534221664310
- SaitoHTakedaSAmizukaNEldecalcitol and calcitriol stimulates ‘bone minimodeling,’ focal bone formation without prior bone resorption, in rat trabecular boneJ Steroid Biochem Mol Biol201313617818223069645
- SakaiSEndoKTakedaSMiharaMShiraishiACombination therapy with eldecalcitol and alendronate has therapeutic advantages over monotherapy by improving bone strengthBone20125051054106322366400
- SugimotoMFutakiNHaradaMKakuSEffects of combined treatment with eldecalcitol and alendronate on bone mass, mechanical properties, and bone histomorphometry in ovariectomized rats: a comparison with alfacalcidol and alendronateBone201352118118823041510
- TakedaSSakaiSShiraishiAKoikeNMiharaMEndoKCombination treatment with eldecalcitol (ED-71) and raloxifene improves bone mechanical strength by suppressing bone turnover and increasing bone mineral density in ovariectomized ratsBone201353116717323232307
- AbeMTsujiNTakahashiFTanigawaYOverview of the clinical pharmacokinetics of eldecalcitol, a new active vitamin D3 derivativeJpn Pharmacol Ther2011393261274
- MatsumotoTTakanoTYamakidoSTakahashiFTsujiNComparison of the effects of eldecalcitol and alfacalcidol on bone and calcium metabolismJ Steroid Biochem Mol Biol20101211–226126420298784
- MatsumotoTKuboderaNThe ED-71 Study Group1α,25-Dihydroxy-2β-(3-hydroxypropoxy) vitamin D3(ED-71): a promising candidate for the treatment of osteoporosisProceedings of the 11th Workshop on Vitamin D2000985992
- KuboderaNTsujiNUchiyamaYEndoKA new active vitamin D analog, ED-71, causes increase in bone mass with preferential effects on bone in osteoporotic patientsJ Cell Biochem200388228628912520528
- MatsumotoTMikiTHaginoHA new active vitamin D, ED-71, increases bone mass in osteoporotic patients under vitamin D supplementation: a randomized, double-blind, placebo-controlled clinical trialJ Clin Endocrinol Metab20059095031503615972580
- MatsumotoTKuboderaNED-71, a new active vitamin D3, increases bone mineral density regardless of serum 25(OH)D levels in osteoporotic subjectsJ Steroid Biochem Mol Biol20071033–558458617298881
- MatsumotoTItoMHayashiYA new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures – a randomized, active comparator, double-blind studyBone201149460561221784190
- NishizawaYOhtaHMiuraMGuidelines for the use of bone metabolic markers in the diagnosis and treatment of osteoporosis (2012 edition)J Bone Miner Metab201331111523143508
- HaginoHTakanoTFukunagaMShirakiMNakamuraTMatsumotoTEldecalcitol reduces the risk of severe vertebral fractures and improves the health-related quality of life in patients with osteoporosisJ Bone Miner Metab201331218318923129180
- KanisJAOdenAJohanssonHBorgströmFStrömOMcCloskeyEFRAX and its applications to clinical practiceBone200944573474319195497
- NakamuraTTakanoTFukunagaMShirakiMMatsumotoTEldecalcitol is more effective for the prevention of osteoporotic fractures than alfacalcidolJ Bone Miner Metab201331441742223575909
- ShirakiMSaitoHMatsumotoTEldecalcitol normalizes bone turnover markers regardless of their pre-treatment levelsCurr Med Res Opin20122891547155222794117
- ItoMNakamuraTFukunagaMShirakiMMatsumotoTEffect of eldecalcitol, an active vitamin D analog, on hip structure and biomechanical properties: 3D assessment by clinical CTBone201149332833421605716
- RingeJDFarahmandPSchachtERozehnalASuperiority of a combined treatment of Alendronate and Alfacalcidol compared to the combination of Alendronate and plain vitamin D or Alfacalcidol alone in established postmenopausal or male osteoporosis (AAC-Trial)Rheumatol Int200727542543417216477
- OrimoHNakamuraTFukunagaMA-TOP (Adequate Treatment of Osteoporosis) research groupEffects of alendronate plus alfacalcidol in osteoporosis patients with a high risk of fracture: the Japanese Osteoporosis Intervention Trial (JOINT) – 02Curr Med Res Opin20112761273128421554143
- TakasuHSugitaAUchiyamaYc-Fos protein as a target of anti-osteoclastogenic action of vitamin D, and synthesis of new analogsJ Clin Invest2006116252853516424941
- AtkinsGJKostakisPPanBRANKL expression is related to the differentiation state of human osteoblastsJ Bone Miner Res20031861088109812817763
- KikutaJKawamuraSOkijiFSphingosine-1-phosphate-mediated osteoclast precursor monocyte migration is a critical point of control in antibone-resorptive action of active vitamin DProc Natl Acad Sci U S A2013110177009701323569273