Abstract
Purpose
The aging population is predisposed to cardiovascular disease. Our goal was to determine the relationship between a higher Elder Risk Assessment (ERA) score and coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI), in adults over 60 years.
Methods
This was a retrospective cohort study in a primary care internal medicine practice. Patients included community-dwelling individuals aged 60 years or older on January 1, 2005. The primary outcome was a combined outcome of CABG and PCI in 2 years. The secondary outcome was mortality 5 years after CABG or PCI. The primary predictor variable was the score on the ERA Index, an instrument that predicts emergency room visits and hospitalization. The outcomes were obtained using administrative data from electronic medical records. The analysis included logistic regression, with odds ratios for the primary outcome and time-to-event analysis for mortality.
Results
The records of 12,650 patients were studied. A total of 902 patients (7.1%) had either CABG or PCI, with an average age of 74.5 years (±8.3 years). There were 205 patients (23%) who experienced CABG or PCI in the highest-score group (top 10%) compared with 29 patients (3%) in the lowest score group, for an odds ratio of 15.4; 95% confidence interval, 10.1–23.5. There was a greater association of revascularization events by increasing score group. We noted increased mortality by increasing ERA score, in patients undergoing CABG or PCI. The patients in the highest-scoring group had a 50% 5-year survival rate compared with a 97% 5-year survival rate in the lowest-scoring group (P < 0.001).
Conclusion
Older adults in the highest-ERA-scoring group had the highest utilization of CABG or PCI. Patients with high ERA scores undergoing coronary revascularization were also at the highest risk of mortality. Providers should be aware that higher ERA scores can potentially predict outcomes in high-risk patients.
Introduction
Frailty and high-risk, medically complex patients have attracted the attention of many providers because of the potential risk for future cardiovascular procedures as well as the potential for adverse events postprocedure. An estimated 83.6 million American adults (more than one in three) have coronary vascular disease (CVD). Of these, 42.2 million (50%) are estimated to be ≥60 years of age.Citation1 One concern is the potential for concomitant CVD and frailty. Although there is no consensus on the definition of frailty, Fried’s frailty definition incorporates a phenotype of low strength, slow gait speed, low physical activity, unintentional weight loss, and self-reported exhaustion.Citation2 The estimation of frailty with a burden of comorbid conditions is another common method for determining the risk of adverse health outcomes. The Frailty Index includes a checklist of 70 items, with multiple comorbid conditions, disabilities, cognitive impairment, mood disturbance, and mobility limitations.Citation3 The comorbid health burden has also been an important component of various hospital risk stratification models, such as the Ambulatory Care Group Risk Stratification Method developed by researchers at Johns Hopkins University.Citation4 The relationship between frailty, as determined by the above methods assessing comorbid burden or phenotype, and future cardiovascular procedures remains an important discussion for providers.
Given the importance of the comorbid health burden and cardiovascular disease, we sought to understand the relationship between cardiovascular revascularization (coronary artery bypass graft [CABG] and percutaneous coronary intervention [PCI]) and the Elder Risk Assessment (ERA) Index, in adults over 60 years. We hypothesized that patients with a higher ERA score, who were most at risk for hospitalization, would be more likely to undergo cardiovascular revascularization than those patients with a lower score and without this frailty burden. To answer this question we performed a retrospective cohort study to determine the association between score on the ERA Index and the combined outcomes of CABG and PCI, in adults aged 60 years or older. As a secondary question, we sought to understand the relationship between ERA score and mortality in those patients who underwent cardiovascular revascularization.
Design and methods
Study design
This was a retrospective cohort study. The study was approved by the Mayo Clinic Institutional Review Board.
Setting
The study was conducted in the Primary Care Internal Medicine (PCIM) Division at Mayo Clinic in Rochester, Minnesota, USA. The PCIM is a mixed internal medicine and geriatric outpatient practice that serves the residents of Olmsted County. In 2000, Olmsted County had a population of 124,277, consisting of 90% white, 4% Asian, and 2% African American.Citation5 The cohort was derived on January 1, 2005. Patients were followed for 2 years, from January 1, 2005 until December 31, 2006, to determine the occurrence of CABG or PCI. Mortality was followed for 5 years following a potential revascularization, until December 31, 2011, to determine the secondary outcome.
Participants
The inclusion criteria included all adults who were living in the community or in an assisted-living facility, aged 60 years or older, and who had given consent for medical record review. The patients were enrolled and had a primary care provider in PCIM. The exclusion criteria included those patients who did not give consent for medical record review and those patients who lived in a skilled-nursing facility on January 1, 2005.
Outcome variables
The primary outcome variable was a combined outcome of CABG and PCI. Each outcome of CABG and PCI was also analyzed separately for comparison. Both outcomes were derived from administrative billing data within the Mayo Clinic system. The secondary outcome was mortality in those subjects undergoing combined cardiovascular procedures. The mortality data was obtained from the electronic medical record (EMR) and was recorded from death within hospitals, nursing homes, and hospices within Olmsted County. Mortality statistics from a review of local newspapers and other resources are updated regularly in the EMR.
Predictor variables
The primary predictor variable was a calculated score on the ERA Index. This ERA was developed, using information from EMRs, to identify community-dwelling older adults at high risk for hospitalizations or emergency room visits.Citation6 The ERA Index is a risk stratification instrument that uses several risk factors: age, marital status, hospital days in the preceding 2 years, and the comorbid medical illnesses diabetes mellitus, heart disease, stroke, emphysema, cancer (excluding nonmelanomatous skin cancer), and dementia.Citation6 Patients were scored based on their individual factors. Individuals were categorized into five groups based on the ERA score, with the lowest scoring group reflecting the bottom quartile, second group the second quartile, third group the third highest quartile, fourth group between 75%–90% top score, and the highest scoring ERA group reflecting the top 10%. The ERA not only predicts hospitalization, but also predicts other health outcomes, like hip fracture.Citation7
Data collection
The data were collected using the EMR at the Mayo Clinic in Rochester, MN, USA. The EMR is a comprehensive record of all hospital admissions, diagnoses, and comorbid health conditions within the institution.Citation8 Mayo Clinic maintains all EMR information within one system, including hospital, emergency room, nursing home, and clinic visit information. Staff associates from the Division of Health Sciences Research extracted information from the EMR related to demographic characteristics, comorbid health problems, hospital utilization, and the outcomes of PCI and CABG.
Data analysis
We summarized the demographic differences and outcomes between participants who underwent a cardiovascular procedure and those who did not. The risk factors between the cardiovascular revascularization group and the nonrevascularization group were analyzed using either a Pearson χ2 test for proportional outcomes or a two-sample t-test if outcomes were continuous. We divided the cohort into five groups, according to the ERA scores: group A (−7 to −1); group B (0 to 3); group C (4 to 8); group D (9 to 15); and the highest group E (≥16). We used a logistic regression model that included groups B, C, D, and E, with the lowest scoring group (A) as the reference group. We computed the odds ratio (OR) with 95% confidence interval (CI) of undergoing cardiac revascularization within 2 years for each of these groups, using multiple logistic regression analyses for age, sex, and the ERA score group.
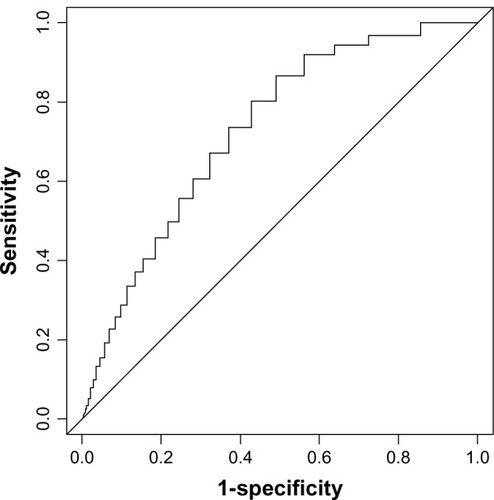
We calculated the sensitivity and specificity of predicting cardiac revascularization at each possible ERA cutoff score. A receiver operating characteristic curve was plotted, and the area under the curve was obtained. We identified the best cutoff point by using the ERA score that provided the highest sum of sensitivity and specificity. The secondary analysis included a time-to-event for mortality in those patients who underwent CABG or PCI. All information was analyzed using SAS version 9.3 software (SAS Institute Inc, Cary, NC, USA). Lastly, we analyzed overall mortality in the entire cohort using the ERA scoring group as a predictor and CABG or PCI as a time-dependent covariate. We stratified the mortality analysis into men and women for further comparison.
Results
Patients
On January 1, 2005, 13,457 patients 60 years of age or older were enrolled in the PCIM practice and eligible for study enrollment. Among the eligible patients, 807 patients (6%) did not agree to medical record review, which led to a total study cohort of 12,650 patients (94%). The patients with CABG or PCI revascularization were older age (74 compared with 72.6 yrs), male, and white. The coronary revascularization group was also more likely to have all potential vascular comorbidities. The demographic characteristics, comorbid health characteristics, and ERA score groups of the cohort are listed in . The specific characteristics for individual outcomes of CABG alone and PCI alone are also listed in .
Table 1 Baseline characteristics of 12,650 adults over 60 who underwent coronary artery bypass grafting, percutaneous coronary interventions or both
Era scores and outcome of CABG and PCI
Overall, 902 of the 12,650 patients (7.1%) had PCI or CABG or both procedures in the 2 years following January 1, 2005. An increase in ERA score group corresponded with the increased odds of performing CABG or PCI. Specifically, in the group with an ERA score ≥16, 23% of the participants underwent a procedure compared with only 3% in the lowest scoring group (−7 to −1) (P < 0.001). Comparing the highest scoring ERA group with the lowest scoring group, we found incremental increases in OR. The OR for the highest group compared with the lowest group was 15.4 (95% CI, 10.1–23.5). In a similar fashion, increasing ERA score significantly increased CABG use alone (P < 0.001) and also PCI use alone (P < 0.001), as noted in . The ORs adjusted for age and sex are noted in . When plotting the ERA score versus the combined outcome of CABG and PCI, the receiver operator curve revealed an optimal ERA score of 4, with a sensitivity of 0.80 and a specificity of 0.51. The area under the curve was 0.71 (95% CI, 0.69–0.73) ().
Table 2 Odds of CABG or PCI, by ERA score and demographic predictors, in 12,650 patients over 60
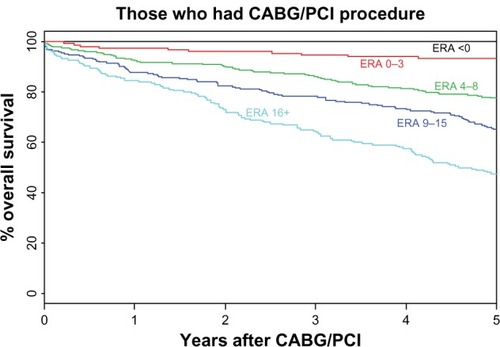
CABG, PCI, and survival
Among the 902 patients undergoing PCI or CABG, survival over the following 5 years showed a significant impact of the ERA score on survival. Patients in the group with the highest ERA score, of ≥16 had a 5-year survival of 50% compared with an over 97% survival in patients with ERA scores <−1. These results are noted on the Kaplan–Meier curve () (P < 0.001). We noted a decreased survival with increasing ERA scoring categories (). presents the overall mortality in the entire cohort of 12,650 participants. We noted an increased mortality with increasing ERA score and that CABG or PCI was not a significant factor for mortality in this model (either protective or harmful). In the stratified analysis for male and female sex, there was no mortality difference between men and women within all ERA scoring categories. At 5 years, patients with an ERA score ≥16 had a survival, of 0.497 (95% CI 0.416 to 0.595) in males and of 0.438 (95% CI 0.342 to 0.560) in females. Thus, the survival at 5 years overlaps between 50% to 44% in men and women respectively.
Table 3 Hazard ratios for overall mortality in 902 patients who underwent coronary artery bypass or percutaneous coronary intervention, by ERA score
Table 4 Hazard ratios for overall mortality for all 12,650 primary care patients, by ERA score with added coronary revascularization term
Figure 2 Time to mortality for 902 patients who underwent coronary artery bypass graft and percutaneous coronary intervention, according to ERA score.
Abbreviations: CABG; coronary artery bypass graft; ERA, Elder Risk Assessment; PCI, percutaneous coronary intervention.
Discussion
In this retrospective cohort study of 12,650 patients, an increasing ERA score predicted CABG and PCI utilization. Almost 23% of all patients with an ERA score ≥16 underwent either CABG or PCI in the following 2 years. These findings are not completely unexpected, as higher ERA scores are associated with future hospitalizationCitation6 and likely measure some degree of frailty. Frailty, the loss of physiologic organ reserve leading to disease, occurs commonly with increasing age and chronic illness, including heart disease.Citation9 An association between frailty and increased coronary disease has been reported often. In the Zutphen Elderly Study of 450 adults aged 69–89 years, 62% of frail men were found to have CVD compared with only 28% of nonfrail men (OR 4.1; 95% CI, 1.8–9.3).Citation10 In a cardiovascular health study of 4,753 adults, the investigators found that patients who had CVD were 2.79 times (95% CI, 2.12–3.67) more likely to be frail.Citation11 The Women’s Health and Aging Studies (WHAS) I and II of 670 community-dwelling elders showed similar predictive associations between frailty and CVD.Citation12,Citation13 The ERA is likely associated with a phenotype that places the individual at risk for coronary revascularization. The ERA Index is not a direct measure of frailty; however, it does predict hospitalization, which likely reflects a phenotype that mirrors frailty with older age, previous hospitalization, and comorbid burden.
The relationship between risk factors and the instruments calculating scores for risk factors and coronary revascularization is important for clinical providers. Patients often suffer multiple illnesses when they undergo coronary revascularization. A comparison study of frail patients versus nonfrail patients undergoing PCI showed that one-fifth of older patients were frail at the time of PCI and possessed a greater comorbid burden, angiographic disease severity, and poorer health status than did the nonfrail adults.Citation14 Investigators have developed other clinical instruments that measure this comorbid burden and can help providers assess potential risk. The Framingham heart predictive tool is the most widely used instrument in clinical practice to help predict heart disease and has been validated in multiple populations.Citation15 The Framingham risk score accounts for age, sex, blood pressure, smoking status, and cholesterol. The Framingham risk score can also include other biomarkers that can add to its predictive value.Citation16 The primary weakness of the Framingham risk score relates to its reliance on active data and cholesterol levels to predict risk. The ERA Index, while not a specific instrument for CABG and PCI, can certainly perform well to help predict future revascularization. The potential advantage of using ERA scores is related to the use of a single score that can help clinicians gauge the potential risk for hospitalization and cardiovascular revascularization. Using this single instrument may also predict other health outcomes, which may improve its clinical utility. This universal utility differs from disease-specific instruments, like the Framingham risk score, which may have higher sensitivity and specificity for PCI or CABG.
In our secondary analysis of patients who underwent CABG or PCI, we observed a relationship between increasing ERA score and rising mortality over the following 5 years. Previous investigators have shown increases in mortality with increasing frailty. The Beaver Dam Eye Study followed 2,962 community-dwelling elders for 4.5 years and found that an increase of one level in the Klein four-level Frailty Index resulted in an increase of 56% in all-cause mortality.Citation17 In our previous work with the ERA Index, we found among patients over the age of 60 years, a 50-fold increased risk of mortality in high-ERA-scoring patients compared with that in low-scoring patients.Citation18 Thus, our finding that higher ERA scores predict mortality is not unexpected in this higher-comorbidity group of CABG or PCI patients. However, due to the magnitude of mortality, with only a 50% 5-year survival rate in patients with ERA scores over 16, health service providers should have some caution when recommending coronary revascularization to patients. These findings emphasize that the prognosis of patients with the highest score should be discussed prior to coronary revascularization.
This study has some limitations that are inherent within a retrospective cohort study. There are risks of missing outcomes if patients seek hospital or emergency room care in outside institutions. It is possible that patients with lower ERA scores are more mobile; thus, we may have missed outcomes such as hospitalizations in other medical systems. This bias could result in higher hospitalization or ER visit rates among the less mobile, more complex older adults compared with less complex, lower-scoring ERA patients. Pragmatically, most patients, including patients with lower ERA scores, have received care within their primary care medical system, and the outcomes should be captured. It is also possible that the scoring system for the ERA was not accurate because of misentered diagnosis codes or diagnostic codes that were not captured; however, there should not be a differential effect of this potential bias among ERA scoring groups. The population in Olmsted County consists of mostly white patients; thus, it may not generalize to other clinical practices. Further studies are needed to be able to project the outcomes in a broader ethnic mix of patients.
The clinical and research implications provide some insight into potential future work. The ERA is an electronic score that is obtained for each patient and is updated without input from staff.Citation6 In this study, we found that ERA predicts CABG or PCI. It is quite possible that other administrative hospital risk scores would provide similar clinical utility. Providers can integrate common administrative demographics and medical diagnoses into a risk score. This knowledge may change the risk-factor management of, for example, blood pressure and cholesterol, for patients at the highest risk for future revascularization. Second, in patients with ERA scores ≥16, providers need to understand that the mortality risks within 5 years after coronary revascularization may only be 50%. In this population, adding CABG or PCI did not modify survival; thus, CABG or PCI would primarily be used for symptom management.
Acknowledgments
We would like to acknowledge the Department of Internal Medicine for supporting this work. We also acknowledge Gladys Hebl, of Grant and Publication Support Services, for help with preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- American Heart AssociationStatistical Fact Sheet: Older Americans and Cardiovascular DiseasesDallas, TXAmerican Heart Association Statistical fact sheet2013 Available from: http://www.heart.org/idc/groups/heart-public/@wcm/@sop/@smd/documents/downloadable/ucm_319574.pdfAccessed August 5, 2013
- FriedLPTangenCMWalstonJCardiovascular Health Study Collaborative Research GroupFrailty in older adults: evidence for a phenotypeJ Gerontol A Biol Sci Med Sci2001563M146M15611253156
- RockwoodKMitnitskiAFrailty in relation to the accumulation of deficitsJ Gerontol A Biol Sci Med Sci200762772272717634318
- WeinerJPStarfieldBHSteinwachsDMMumfordLMDevelopment and application of a population-oriented measure of ambulatory care case-mixMed Care19912954524721902278
- factfinder2.census.gov [homepage on the Internet]Profile of general demographic characteristics: 2000US Census Bureau2000 [cited May 4, 2010]. Available from: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_00_SF1_DP1&prodType=tableAccessed August 5, 2013
- CraneSJTungEEHansonGJChaSChaudhryRTakahashiPYUse of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: the elders risk assessment indexBMC Health Serv Res20101033821144042
- AlbabaMChaSSTakahashiPYThe Elders Risk Assessment Index, an electronic administrative database-derived frailty index, can identify risk of hip fracture in a cohort of community-dwelling adultsMayo Clin Proc201287765265822766085
- St SauverJLGrossardtBRYawnBPData resource profile: the Rochester Epidemiology Project (REP) medical records-linkage systemInt J Epidemiol20124161614162423159830
- RockwoodKMitnitskiAFrailty defined by deficit accumulation and geriatric medicine defined by frailtyClin Geriatr Med2011271172621093719
- ChinAPawMJDekkerJMFeskensEJSchoutenEGKromhoutDHow to select a frail elderly population? A comparison of three working definitionsJ Clin Epidemiol199952111015102110526994
- NewmanABGottdienerJSMcburnieMACardiovascular Health Study Research GroupAssociations of subclinical cardiovascular disease with frailtyJ Gerontol A Biol Sci Med Sci2001563M158M16611253157
- Bandeen-RocheKXueQLFerrucciLPhenotype of frailty: characterization in the women’s health and aging studiesJ Gerontol A Biol Sci Med Sci200661326226616567375
- ChavesPHSembaRDLengSXImpact of anemia and cardiovascular disease on frailty status of community-dwelling older women: the Women’s Health and Aging Studies I and IIJ Gerontol A Biol Sci Med Sci200560672973515983175
- GharacholouSMRogerVLLennonRJComparison of frail patients versus nonfrail patients ≥65 years of age undergoing percutaneous coronary interventionAm J Cardiol2012109111569157522440119
- D’AgostinoRBGrundySSullivanLMWilsonPCHD Risk Prediction GroupValidation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigationJAMA2001286218018711448281
- YeboahJMcClellandRLPolonskyTSComparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individualsJAMA2012308878879522910756
- KleinBEKleinRKnudtsonMDLeeKEFrailty, morbidity and survivalArch Gerontol Geriatr200541214114916085065
- TakahashiPYTungEECraneSJChaudhryRChaSHansonGJUse of the elderly risk assessment (ERA) index to predict 2-year mortality and nursing home placement among community dwelling older adultsArch Gerontol Geriatr2012541343821397346