Abstract
Objective
Non-valvular atrial fibrillation (NVAF) is one common arrhythmia in the elderly. However, use of antithrombotic therapy in this population is not well known in the People’s Republic of China. This study aimed at investigating antithrombotic therapy status in elderly patients with NVAF in our hospital.
Methods
A cross-sectional study of consecutive geriatric patients aged ≥60 years with NVAF who discharged from our hospital between January 2012 and December 2013 were collected. CHA2DS2-VASc score (cardiac failure or dysfunction, hypertension, age ≥75 [doubled], diabetes, stroke or transient ischemic attack [doubled], vascular disease, age 65–74, and sex category [female]) was used to analyze antithrombotic indication.
Results
We consecutively collected data of 1,000 discharged elderly patients (≥60 years) with NVAF (mean age 75.3±8.0 years, 75 years or older 54.7%, female 42.7%). The proportion of paroxysmal atrial fibrillation and non-paroxysmal atrial fibrillation (persistent or permanent) patients were 39.4% and 60.6%, respectively. Among 1,000 patients, 29.1% received oral anticoagulant therapy (OAT), including warfarin (27.8%) and novel oral anticoagulants (1.3%), 39.5% of patients received antiplatelet therapy, and 31.4% received neither therapy. Based on CHA2DS2-VASc score for stroke risk stratification, 68.9% patients with score ≥1 and 70.2% patients with score ≥2 received antithrombotic therapy, while the rates of OAT were 29.1% and 29.5%, respectively. Among patients with high stroke risk, those with paroxysmal atrial fibrillation were less likely to receive OAT compared with the patients with non-paroxysmal atrial fibrillation (19.5% vs 35.7%, P<0.001). The patients ≥75 years old had lower rate of OAT than the patients <75 years old (25.8% vs 34.8%, P=0.003). The patients with coronary artery disease had lower rate of OAT than the patients without coronary artery disease (24.4% vs 33.4%, P=0.003). Sex and history of stroke or transient ischemic attack had no effect on the use of OAT (30.8% vs 27.9%, P=0.326 and 28.8% vs 29.8%, P=0.761, respectively).
Conclusion
OAT in elderly patients with NVAF in our hospital is underused, especially in those patients with higher risk of stroke.
Introduction
Non-valvular atrial fibrillation (NVAF) is a very common arrhythmia, and its prevalence increases significantly with age.Citation1,Citation2 According to epidemic data, the prevalence of atrial fibrillation (AF) in the general Chinese population is 0.77%. What is more, it affects more than 12.2% people over 85 years old. AF is associated with higher risk of ischemic stroke and is responsible for greater mortality and morbidity.Citation3 Evidence from a series of trials has shown that oral anticoagulant therapy (OAT) reduces stroke and improves other outcomes in patients with NVAF.Citation4 Accordingly, in recent years, a number of international guidelines have recommended OAT for patients with NVAF.Citation5,Citation6 However, previous studies have shown the low rate of receiving OAT in NVAF patients in the People’s Republic of China several years ago.Citation1 As a result, this study is designed to investigate antithrombotic therapy status in elderly patients with NVAF in our hospital between January 2012 and December 2013.
Methods
Study population
This was an observational study based on chart review from an electronic clinical information system in our hospital. Older patients (≥60 years) with NVAF were eligible for this study. Diagnosis of AF is based on electrocardiography (ECG) (12-lead ECG), or 24-hour Holter. Demographics, other medical diagnoses, antithrombotic or antiplatelet therapy, and laboratory data were also collected. Exclusion criteria included any one of the following conditions: valvular AF, rheumatic mitral stenosis, a mechanical or bioprosthetic heart valve, mitral valve repair, and death in hospital. Data was consecutively collected from the patients discharged between January 2012 and December 2013. CHA2DS2-VASc score (cardiac failure or dysfunction, hypertension, age ≥75 [doubled], diabetes, stroke/transient ischemic attack [TIA] [doubled], vascular disease, age 65–74, and sex category [female])Citation5 was used for stroke risk stratification.
Statistical analysis
Data analysis was performed with SPSS, version 19.0 (IBM Corporation, Armonk, NY, USA). Continuous variables were reported as mean ± standard deviation or as median (interquartile range). Among-group comparisons of continuous variables were analyzed with nonparametric test (Kruskal–Wallis test). Categorical variables were reported as frequencies (percentages). Among-group comparisons of categorical variables were analyzed with chi-square test. All P-values were two sided, and a P-value of <0.05 was considered to be defined as statistically significant.
Results
Patient characteristics
Between January 2012 and December 2013, a total of 1,000 elderly NVAF patients were consecutively enrolled, and 128 elderly AF patients were excluded. Demographic characteristics and risk factors of stroke are presented in .
Table 1 Patient characteristics according to CHA2DS2-VASc risk score
Use of antithrombotics
Among the 1,000 patients, 291 patients (29.1%) received OAT, including 278 patients (27.8%) prescribed warfarin and the rest (1.3%) took novel oral anticoagulants, 395 patients (39.5%) took antiplatelet drugs including aspirin and/or clopidogrel, and 314 patients (31.4%) were not on oral anticoagulants or antiplatelet drugs.
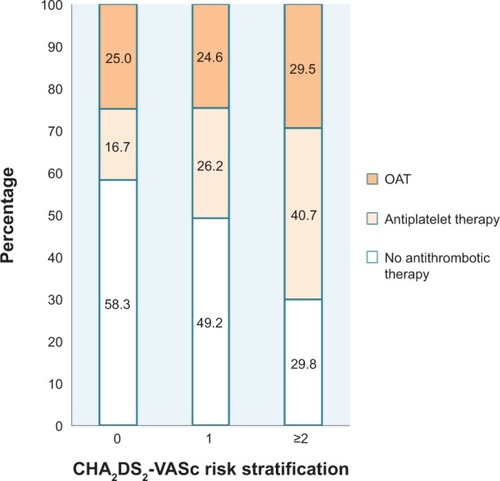
Use of OAT according to CHA2DS2-VASc score
Based on the CHA2DS2-VASc score, the OAT rates were 25.0%, 24.6%, and 29.5%, respectively, in patients with the score of 0, 1, and ≥2. The CHA2DS2-VASc score was not significantly associated with the rate of receiving OAT (P=0.403) (). What is more, the proportion of patients receiving antithrombotic therapy in the score ≥1 and score ≥2 groups were 68.9% (681/988) and 70.2% (648/923), respectively. The rate of OAT in the score ≥1 group reached 29.1% (288/988).
Figure 1 Prescription rate of antithrombotics according to CHA2DS2-VASc risk stratification.
Abbreviation: OAT, oral anticoagulant therapy.
Use of OAT in high-risk stroke patients (CHA2DS2-VASc score ≥2)
The use of OAT among high-risk stroke patients ie, in the CHA2DS2-VASc score ≥2 (n=923) cohort is shown in . There were more patients with persistent or permanent AF receiving OAT than patients with paroxysmal AF (P<0.001). The patients aged between 60 and 74 years used more OAT than patients aged ≥75 years (P=0.003). Patients without coronary artery diseases were more likely to receive OAT than patients with coronary artery disease (P=0.003). The sex and history of stroke or TIA had no effect on use of OAT.
Table 2 Use of OAT in high-risk stroke patients (CHA2DS2-VASc score ≥2)
Discussion
The clinical practice guidelines strongly recommend OAT for NVAF patients.Citation5,Citation6 However, it was observed that various antithrombotics such as oral anticoagulants and antiplatelet drugs were used in elderly AF patients, whose mean age was 75 years old. Although OAT rates in domestic elderly NVAF patients was higher than previously published survey data, which range from 5.7% to 14.5%,Citation7,Citation8 OAT were underused in older patients with NVAF (29.1%), particularly in those with high risk of stroke (29.5%). Therefore, treatment prescription still deviated largely from guideline recommendations based on CHA2DS2-VASc score. When compared with European countries, the underuse of OAT in elderly AF patients was also remarkable. Lip et alCitation9 reported that in European real-world clinical practice, a total of 95.6% NVAF patients with CHA2DS2-VASc score ≥1 received antithrombotic therapy, among which 80.5% received OAT, and the proportion of OAT prescriptions in those with score ≥2 was 83.7%. We also found that in our study, three patients with AF and CHA2DS2-VASc =0 took short-term anticoagulation, for they received radio-frequency catheter ablation during hospitalizing, in order to prevent secondary thrombosis after the treatment. However, the total number of patients with AF and CHA2DS2-VASc score of 0 was few (n=12), thus leading to the relatively high OAT rate (25.0% [3/12]) in this population. As a result, no significant difference was observed in the OAT rate between patients with CHA2DS2-VASc score of 0 and those with score of 1 and ≥2. Otherwise, we noticed that OAT rate was between 20% and 30% in both CHA2DS2-VASc score =1 and ≥2 patients, not increased significantly with the increase of the score; and we found that antiplatelet therapy rate was 16.7% in the score =0 group and 40.7% in the score ≥2 group. Both of which weren’t consistent with the antithrombotic therapy strategies recommended by AF guidelines,Citation5,Citation6 and indicated unreasonable application of antithrombotic therapy. Several possible reasons might explain the inconsistency in our study: 1) some clinical doctors might have insufficient understanding of stroke risk caused by NVAF and be unfamiliar with CHA2DS2-VASc score and AF guidelines about antithrombotic treatment, so that they gave antiplatelet therapy to patients with the score of 0 and 2; 2) patients with NVAF would be more inclined to choose antiplatelet therapy rather than OAT, as they were supposed that the former was safer, more convenient or cheaper; 3) a considerable number of doctors and patients were worried about bleeding risk, especially intracerebral hemorrhage caused by OAT, mainly by warfarin.
Through further analysis, we learned that patients with advanced age were less likely to be prescribed OAT despite high stroke risk, especially in patients older than 75 years. Partington et alCitation10 also found that aging was the strongest predictor for warfarin non-use. Actually, in trials considering the elderly population, OAT was associated with significant reduction in thromboembolism occurrence, as well as lower major bleeding risk.Citation11,Citation12 As a consequence, we should enhance the rate of OAT in elderly NVAF patients, especially in patients over 75 years.
We found OAT was also less likely to be used in paroxysmal AF patients (19.5%), even if a high risk of thromboembolism remained in those patients. This situation was similar to the study outcomes of Friberg et al and Hohnloser et al.Citation13,Citation14 Indeed, what really determines stroke risk depends on various elements such as hypertension and diabetes, rather than AF pattern. So it is emphasized in guidelines that in presence of stroke risk factors, OAT should be prescribed regardless of clinical AF type (paroxysmal, persistent, or permanent).Citation6
Previous stroke or TIA increases the risk of stroke recurrence, and usually leads to the worst prognosis in AF patients.Citation3 Thus, in the CHA2DS2-VASc score, the highest value was given to previous stroke or TIA. Guidelines recommend OAT to be the preferred treatment option for AF patients with a history of stroke or TIA.Citation6 However, in this study, we found that the prevalence of stroke or TIA in elderly AF patients has reached 31.9%, while less than 30% of those patients received OAT, which meant OAT was critically insufficient in this group.
Comorbidity of vascular disease also independently increases the risk of stroke in AF patients.Citation15 For one thing, in AF patients with stable vascular disease, OAT is the optimal treatment option. What is more, combination therapy (OAT plus antiplatelets) not only reduces the occurrence rate of thromboembolism, but also substantially increases the risk of major bleeding.Citation5 For another thing, situation in AF patients presenting acute coronary syndrome and/or stenting might be much more complicated. The 2012 ESC Atrial Fibrillation Guidelines recommended triple therapy (OAT plus dual antiplatelet therapy) at the early stage, and followed by OAT plus single antiplatelet therapy, then OAT alone.Citation5 However, triple therapy is usually associated with high bleeding risk.Citation16 Dewilde et alCitation17 found that in patients undergoing percutaneous coronary intervention, coadministration of clopidogrel without aspirin was associated with significant reduction in bleeding complications when compared with dual antiplatelet therapy. Also, no increase in the occurrence rate of thrombotic events was observed. Therefore, the 2014 AHA/ACC/HRS Atrial Fibrillation Guideline suggests that following coronary revascularization in patients with CHA2DS2-VASc score of ≥2, it may be reasonable to use clopidogrel concurrently with OAT.Citation6 In addition, we observed that compared with those elderly patients without coronary disease, elderly AF patients complicated with coronary disease were more likely to take antiplatelet therapy than OAT, so new strategies should be considered for optimizing the use of OAT in this population.
Limitations of this study were as follows: 1) it is a single medical center survey, 2) the sample size was relatively small, and 3) the quality of OAT use was not studied. Patients on OAT might not get therapeutic level of international normalized ratio. So it is possible that the current situation of anticoagulant therapy in elderly AF patients nationwide may not be fully reflected. As a result, further multicenter and larger-scale studies are required to show the status of antithrombotic therapy in elderly AF patients. Furthermore, there were no data considering quality control of anticoagulation. Last but not least, we did not have detailed data on outcomes, which will be illustrated by the ongoing follow-up phase of our study.
In conclusion, our single medical center survey provides contemporary data on oral anticoagulation prescription in elderly AF patients. Oral anticoagulation (mostly vitamin K antagonist administration) has improved in contrast with situations several years ago. Nevertheless, under-treatment with OAT and an inclination to use antiplatelet drugs are still common in elderly patients with NVAF.
Acknowledgments
This work was supported by the National Science and Technology Support Program, whose topic is Translational Medicine Research of Treatment Risk and Strategy in the Elderly Population (2012BAI37B05). The sponsors did not have a role in the design or conduct of this study, the analysis of data, or preparation of the manuscript. We thank the participants and all of the staff involved in this study.
Disclosure
The authors have no conflicts of interest to report.
References
- ZhouZQHuDYAn epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland ChinaJ Epidemiol200818520921618776706
- GoASHylekEMPhillipsKAPrevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) StudyJAMA2001285182370237511343485
- MariniCDe SantisFSaccoSContribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based studyStroke20053661115111915879330
- HartRGPearceLAAguilarMIMeta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillationAnn Intern Med20071461285786717577005
- CammAJLipGYDe CaterinaR2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm AssociationEur Heart J201233212719274722922413
- JanuaryCTWannLSAlpertJS2014AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm SocietyJ Am Coll Cardiol Epub2014328
- QiZGWangHZGaoYAntithrombotic therapy in 875 elderly patients with atrial fibrillationChinese Journal of Geriatric Heart Brain and Vessel Diseases20119805807 Chinese
- GuoYTWuQZhangLAntithrombotic therapy in very elderly patients with atrial fibrillation: is it enough to assess thromboembolic risk?Clin Interv Aging201052515716220517485
- LipGYLarocheCDanGA‘Real-world’ antithrombotic treatment in atrial fibrillation: the EORP-AF pilot surveyAm J Med20141276519529.e124486284
- PartingtonSLAbidSTeoKOczkowskiWO’DonnellMJPre-admission warfarin use in patients with acute ischemic stroke and atrial fibrillation: The appropriate use and barriers to oral anticoagulant therapyThromb Res2007120566366917434577
- PoliDAntonucciETestaSTosettoAAgenoWPalaretiGBleeding risk in very old patients on vitamin K antagonist treatment: results of a prospective collaborative study on elderly patients followed by Italian Centres for AnticoagulationCirculation2011124782482921810658
- TincaniEBaldiniPCrowtherMABleeding rates in patients older than 90 years of age on vitamin K antagonist therapy for nonvalvular atrial fibrillationBlood Coagul Fibrinolysis2009201475120523164
- FribergLHammarNRosenqvistMStroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial FibrillationEur Heart J201031896797519176537
- HohnloserSHPajitnevDPogueJIncidence of stroke in paroxysmal versus sustained atrial fibrillation in patients taking oral anticoagulation or combined antiplatelet therapy: an ACTIVE W SubstudyJ Am Coll Cardiol200750222156216118036454
- OlesenJBLipGYLaneDAVascular disease and stroke risk in atrial fibrillation: a nationwide cohort studyAm J Med20121258813826
- HansenMLSorensenRClausenMTRisk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillationArch Intern Med2010170161433144120837828
- DewildeWJOirbansTVerheugtFWUse of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trialLancet201338198721107111523415013
