Abstract
Background
The effect of perioperative oral nutritional supplementation (ONS) on elderly patients after hip surgery remains controversial. This study intended to ascertain whether perioperative ONS is beneficial for the rehabilitation of elderly patients after hip surgery.
Materials and methods
We searched databases including PubMed, Embase, and the Cochrane Central Register of Controlled Trials for articles published up to May 2014. Randomized controlled trials of ONS for elderly patients after hip surgery were included.
Results
The combined trials showed that ONS had a positive effect on the serum total protein (P<0.00001) and led to a significantly decreased number of complications (P=0.0005). Furthermore, data from the infection subgroups showed significant decreases in wound infection (P=0.02), respiratory infection (P=0.04), and urinary tract infection (P=0.03). Clinical observation suggests that the intervention may improve the level of serum albumin, although the data did not reach statistical significance (P=0.48). Regarding mortality, there was no significant statistical difference between the intervention group and the control (P=0.93).
Conclusion
Based on the evidence available, this meta-analysis is consistent with the hypothesis that perioperative ONS can help elderly patients recover after hip surgery and reduce complications.
Introduction
The incidence of hip fracture in elderly people will reach 11.9% by the end of 2030 with life extension and increasing social activities such as travelling, riding (bicycle and motorcycle), dancing, and so on.Citation1–Citation5 Nutritional status is an important influencing factor for early postoperative rehabilitation. However, a variety of factors, such as pre-fracture nutritional status, underlying diseases, and wound stress induce a high incidence of postoperative complications and mortality.Citation6–Citation8 Moreover, blood loss, postoperative poor appetite, and poor food intake occur regularly among elderly patients in hospital.Citation9–Citation11 Therefore, clinicians are seeking effective measures which can improve the perioperative nutritional status of elderly patients after hip surgery.Citation12–Citation14
Among various nutritional supplement interventions, many studies have proposed that oral nutritional supplementation (ONS) might be a convenient method to enhance energy and protein intake and be beneficial for elderly patients who are undergoing trauma stress reaction from hip fractures or surgeries to improve bowel health and nutrient intake. Furthermore, ONS is more economical and practical than parenteral nutritional supplementation.Citation15,Citation16 One multicenter, randomized controlled trial (RCT), which mainly investigated the cost-effectiveness of intensive nutritional supplementation, found that the cost of oral nutritional intervention is lower than that of other types of nutritional intervention. Meanwhile, cost-effectiveness evaluation showed that the ONS intervention route is more likely to be cost-effective.Citation16
While ONS has been increasingly attracting the attention of clinicians, more and more RCTs have been conducted to evaluate the effectiveness of ONS for elderly patients after hip surgery and suggest that ONS is a beneficial intervention for elderly patients after hip surgery to improve the nutritional status.Citation9,Citation12,Citation13,Citation17,Citation18 However, there remain opposing opinions about the efficiency of ONS. Some researchers have shown that functional recovery and mortality were not statistically improved after ONS intervention in elderly patients after hip surgery,Citation19–Citation21 while a relevant review mentioned that a definite conclusion about ONS for elderly patients with hip fracture, whether surgery was performed or not, could not be drawn because of weak evidence.Citation20
As orthopedic doctors, we are concerned about the management of nutritional status of elderly patients during the perioperative period. Obviously, we wish to have better knowledge about appropriate interventions to reduce complications, shorten the time of hospitalization, and improve the patients’ health. Therefore, the aim of this meta-analysis was to determine whether ONS can be recommended as a routine nutritional intervention for elderly patients after hip surgery.
Clinical relevance
It is very important to return the nutritional status back to normal levels in elderly patients aged over 65 years during the perioperative period. Meanwhile, strategy selection should be evidence based. The findings of this meta-analysis on whether perioperative ONS can reduce complications are clinically relevant for clinicians, including emergency physicians, orthopedic surgeons, nursing staff, geriatricians, and rehabilitation physicians, and can help them properly treat elderly patients and effectually improve clinical outcomes.
Materials and methods
Data sources and searches
We searched for relevant articles published up to May 2014 in databases including PubMed, Embase, and the Cochrane Central Register of Controlled Trials. The terms “oral nutrition” or “oral supplement”, “hip surgery” or “hip fracture” or “femoral neck fracture” or “intertrochanteric fracture” or “subtrochanteric fracture”, and “old” or “elderly” or “aged” were used to search titles, abstracts, and medical subject headings. We also browsed the reference lists and consulted experts to search for potentially eligible studies.
Study identification
The inclusion criteria used in the selection were as follows: 1) target population: patients aged over 65 years who had had hip fractures (femoral neck, intertrochanteric or subtrochanteric, acetabulum fractures) and undergone surgery (open reduction and internal fixation or arthroplasty); 2) intervention measure: perioperative ONS (orally taking high-calorie or high-protein diets); and 3) design type: RCT. The exclusion criteria used in the selection were: 1) patients with multiple systemic fractures or pathologic fractures; 2) data without standard deviations; 3) participants with hip fractures who had undergone nonsurgical treatment.
Quality assessment
We assessed the quality of individual studies by using the validated Oxford Scale and obtaining Jadad scores,Citation22 which ranged from 1–5 points. Scores of 1–2 were considered as low quality, while scores of 3–5 were considered as high quality. Two independent reviewers performed the initial screening and extraction procedures. Then, another two investigators independently assessed all articles which met the inclusion criteria. Whenever there was a disagreement, it was solved by collective discussion among the investigators.Citation23
Main outcomes
We extracted information about the characteristics of the included studies, such as the research design, population of participants, age of participants, fracture classification, follow-up periods, intervention measurements, control measurements, and the assessment criteria. Then, we analyzed each study for its Jadad score.
Data were collected from the included studies, including data for: 1) total protein; 2) complications (including all infections, bed sores, cardiac disease, cognitive impairment, prolonged immobilization, thrombophlebitis, deep vein thrombosis, vomiting, diarrhea, pressure ulcers, dysphasia, severe hyponatremia, anaphylaxis, pneumonedema, pulmonary embolism, and myocardial infarction); 3) change in serum albumin levels (the difference in serum albumin levels before and after intervention [g/L]); and 4) mortality.
Data synthesis
Perioperative data regarding the patients, interventions, and outcomes mentioned above were extracted from the included studies. We used Review Manager 5.1 software to analyze the data and adopted a 95% confidence interval (CI). Two reviewers monitored the data inputting to ensure accuracy. For the measurement outcomes, the mean standard deviation, and n were recorded, and the standard mean difference (SMD) was calculated. For the enumeration outcomes, the scale and the numbers were recorded, then the odds ratio (OR) was calculated.Citation24,Citation25
Heterogeneity, sensitivity, and risk of bias
We used I2 to test heterogeneity and estimate total variation across studies. For I2, values between 25% and 50% were considered as low heterogeneity; those between 50% and 75% were considered as medium heterogeneity; and those over 75% were considered as high heterogeneity.Citation23,Citation24,Citation26 We qualitatively assessed each included study for allocation, attrition, and reporting bias, using Stata 11 software to perform the Begg’s test.Citation23,Citation27–Citation29
Results
Characteristics of included studies
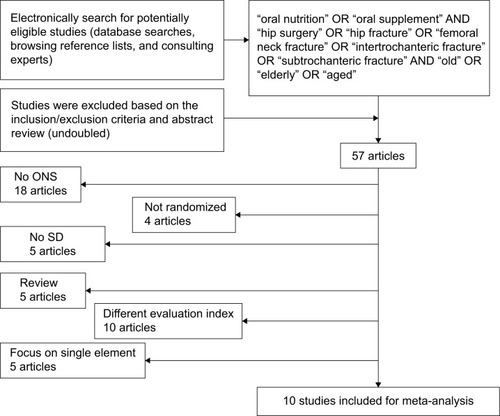
As shown in , 57 articles published from 1966 to May 2014 were retrieved. Following the inclusion and exclusion criteria, we eliminated the retrospective studies with historical control, the studies lacking original data or standard deviation analysis, and the research with different evaluation indicators. After reading the full texts, we eliminated the studies that were not RCTs, not full text or relevant to ONS or standard deviation. Finally, ten RCTsCitation13,Citation14,Citation19,Citation21,Citation30–Citation35 were included; the characteristics of these studies are presented in . A total of 986 elderly patients who had undergone hip surgery and were aged over 65 years were included. Each of the ten studies was an RCT, and two of them were double blind.Citation19,Citation33 Further, they all used standard deviation to analyze results.Citation23 The study quality varied across these trials: six of the ten included studies had Jadad scores of 3–5, while the other four studies scored 1–2.
Table 1 Characteristics of included trials
Figure 1 Flow diagram of the selection of studies.
Abbreviations: ONS, oral nutritional supplementation; SD, standard deviation.
As shown in , we extracted information about the research design characteristics of the included studies, including the population of participants, age of participants, fracture classification, follow-up period, intervention measurements, control measurements, the comparison of assessment criteria between control group and intervention group, and the Jadad score of each study. Not all evaluation indicators of the included studies were the same, so we merged the data of those studies with the same evaluation indicator to analyze the results.
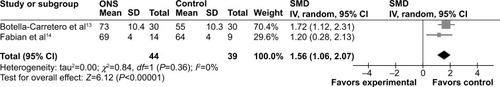
Total protein
Following the inclusion and exclusion criteria, two studies (Bottella-Carretero et alCitation13 and Fabian et alCitation14) were included. The two studies had a total of 83 patients in the meta-analysis, consisting of 44 patients in the ONS group and 39 in the control group. There was a statistically significant increase of the total protein levels in ONS group before patients were discharged (SMD =1.56 [95% CI: 1.06, 2.07]; P<0.00001) (). There was no evidence of heterogeneity between the studies (I2=0%; P=0.36).
Figure 2 Forest plot for total proteins.
Abbreviations: CI, confidence interval; df, degrees of freedom; IV, intravenous; ONS, oral nutritional supplementation; SD, standard deviation; SMD, standard mean difference.
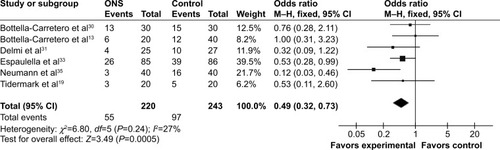
Complications
Following the inclusion and exclusion criteria, six studies (Tidermark et al,Citation19 Neumann et al,Citation35 Espaulella et al,Citation33 Delmi et alCitation31 and Bottella-Carretero et alCitation13,Citation30) were included in the complications meta-analysis. A total of 463 patients from the six studies were included in the meta-analysis, consisting of 220 patients in the ONS group and 243 in the control group. shows that the ONS had a measurable effect on reducing complications after hip surgery in elderly patients (OR =0.49 [95% CI: 0.32, 0.73]; P=0.0005). No evidence of statistical significance for heterogeneity was found among the studies (I2=27%; P=0.24).
Figure 3 Forest plot for complications.
Abbreviations: CI, confidence interval; df, degrees of freedom; ONS, oral nutritional supplementation; OR, odds ratio; M–H, Mantel–Haenszel.
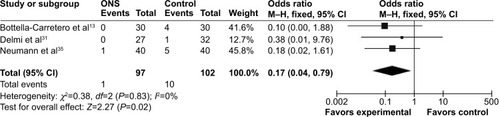
Wound infection
Following the inclusion and exclusion criteria, three studies (Bottella-Carretero et al,Citation13 Delmi et alCitation31 and Neumann et alCitation35) were included in the wound infection meta-analysis. A total of 199 patients from the three studies were included in the meta-analysis, consisting of 97 patients in the ONS group and 102 in the control group. Pooled results indicate that the ONS group had a lower rate of wound infection than the control group (OR =0.17 [95% CI: 0.04, 0.79]; P=0.02). There was no evidence of heterogeneity among the studies (I2=0%, P=0.83) ().
Figure 4 Forest plot for wound infections.
Abbreviations: CI, confidence interval; df, degrees of freedom; ONS, oral nutritional supplementation; M–H, Mantel–Haenszel.
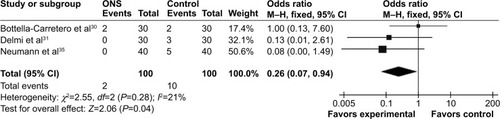
Respiratory infection
Following the inclusion and exclusion criteria, three studies (Bottella-Carretero et al,Citation30 Delmi et alCitation31 and Neumann et alCitation35) were included in the respiratory infection meta-analysis. A total of 200 patients from the three studies were included in the meta-analysis, consisting of 100 patients in the ONS group and 100 in the control group. shows the respiratory infection rates between ONS patients and the control group. According to the three trials included, there were significant statistical difference in the baseline and the length of hospitalization between two groups (OR =0.26 [95% CI: 0.07, 0.94]; P=0.04). No statistical significance of heterogeneity was found among the included studies (I2=21%; P=0.28).
Figure 5 Forest plot for respiratory infections.
Abbreviations: CI, confidence interval; df, degrees of freedom; ONS, oral nutritional supplementation; M–H, Mantel–Haenszel.
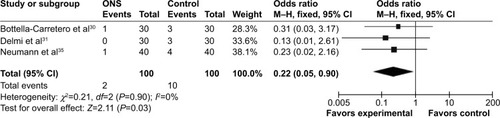
Urinary tract infection
Following the inclusion and exclusion criteria, three studies (Bottella-Carretero et al,Citation30 Delmi et alCitation31 and Neumann et alCitation35) were included in the urinary tract infection meta-analysis. A total of 200 patients from the three studies were included in the meta-analysis. shows the urinary tract infection rates between ONS patients and the control group. Based on the three trials, there were significant differences between the two groups both on baseline and hospitalization time (OR =0.22 [95% CI: 0.05, 0.90]; P=0.03). There was no evidence for heterogeneity among the studies (I2=0%; P=0.90).
Figure 6 Forest plot for urinary tract infections.
Abbreviations: CI, confidence interval; df, degrees of freedom; ONS, oral nutritional supplementation; M–H, Mantel–Haenszel.
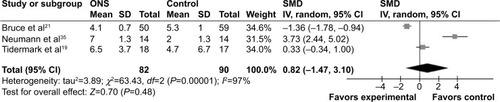
Change in serum albumin
Following the inclusion and exclusion criteria, data for the change in serum albumin levels from three studies (Bruce et al,Citation21 Neumann et alCitation35 and Tidermark et alCitation19) were included. These three studies had a total of 172 patients, consisting of 82 patients in the ONS group and 90 in the control group in the meta-analysis. As shown in , the change in serum albumin did not have any statistically significant difference between ONS patients and control group (SMD =0.82 [95% CI: −1.47, 3.10]; P=0.48). Heterogeneity was found to be large and statistically significant for the change in serum albumin in this analysis (I2=97%, P<0.00001).
Figure 7 Forest plot for changes in serum albumin.
Abbreviations: CI, confidence interval; df, degrees of freedom; IV, intravenous; ONS, oral nutritional supplementation; SD, standard deviation; SMD, standard mean difference.
Mortality
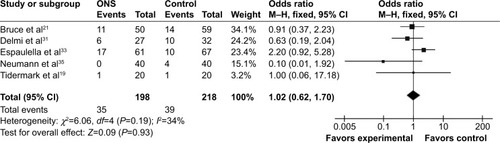
Following the inclusion and exclusion criteria, five studies (Bruce et al,Citation21 Delmi et al,Citation31 Espaulella et al,Citation33 Neumann et alCitation35 and Tidermark et alCitation19) were included. The five studies had a total of 416 patients, consisting of 198 patients in the ONS group and 218 in the control group in the meta-analysis. The analysis of mortality indicated that ONS had no statistically significant effect on mortality (ONS group 35/198 versus control group 39/218; OR =1.02 [95% CI: 0.62, 1.70]; P=0.93). Large and statistically significant heterogeneity was found in this meta-analysis (I2=34%; P=0.19) ().
Figure 8 Forest plot for mortality.
Abbreviations: CI, confidence interval; df, degrees of freedom; ONS, oral nutritional supplementation; M–H, Mantel–Haenszel.
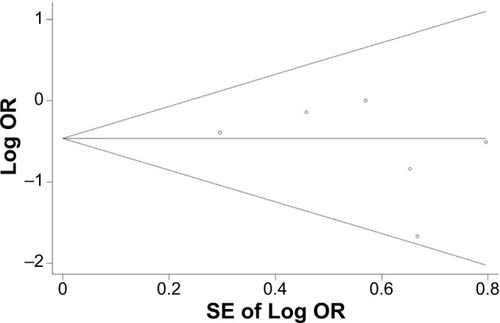
Assessment of publication bias
As shown in , the Begg’s funnel plot shows no significant Begg’s test for publication bias (P>0.05), indicating no evidence of publication bias among the studies.
Discussion
To our knowledge, this is the first meta-analysis assessing studies about elderly patients receiving ONS after hip surgery. The overall results of the current investigation suggest that ONS improves early recovery by increasing the total protein level and reducing complications in elderly patients after hip surgery.
As shown in our meta-analysis, there was a statistically significant improvement in the serum total protein level in the ONS group compared with that in the control group. As a nutritional marker, serum total protein, along with nutrition-rich supplements, helps patients to recover more quickly. Moreover, protein-rich supplementation might further lower blood pressure, improve lipid levels, and reduce estimated cardiovascular risks.Citation36
Complications are always directly related to the quality of the patient’s lifestyle and the quality of medical services. The incidence of complications (eg, pressure sores, infections, deep venous thromboses, cardiovascular events) in elderly patients after hip surgery is high and deserves more attention. Our study showed the complications rate was lower in elderly patients receiving ONS than in the control group. Similar results were found in previous studies of nasogastric feeding and parenteral nutrition.Citation13,Citation19,Citation30,Citation31,Citation33,Citation37 Further, we carried out a subgroup analysis on infections (including wound infection, respiratory tract infection, and urinary tract infection), the results of which showed a consistent reduction in each infection rate in the ONS group. The wound infection rate showed that ONS had a positive effect on wound healing. The decreased infection rates observed in the ONS group could be related to the increased serum total protein level, which would benefit the elderly patients to maintain the immunological functions.Citation38 ONS had a positive effect on the respiratory infection rate as well as the wound infection rate. Furthermore, high-protein and high-calorie diets have been shown to reduce the urinary tract infection rate.Citation39
As an independent prognostic factor for elderly patients after hip surgery, serum albumin is an important index for assessing rehabilitation after surgery.Citation40 A change in serum albumin levels before and after ONS was observed in the present study. The merged data from three trials about the change in serum albumin showed no statistically significant difference (),Citation19,Citation21,Citation35 while there was significant heterogeneity (χ2=63.43, df=2 [P<0.00001]; I2=97%) was found using the random effects model. Further research should aim to define whether ONS can influence the serum albumin levels.
Our mortality data indicate that there were no statistical differences between the ONS group and the control group. This finding is consistent with previous studies.Citation20,Citation21,Citation33 However, more attention should be paid to one important element: unavoidable death. The differences in mortality between the ONS group and the control group were not statistically significant because inevitable deaths were not excluded. Approximately one-quarter (28%) of deaths after hip surgery in the elderly are unavoidable regardless of the perioperative care regimen.Citation8 The mortality rates of the two groups in the present study are both below one-quarter (ONS group: 35/198≈17.68%; control group: 39/218≈17.89%). Thus, it is inadvisable to draw the conclusion that the use of ONS in elderly patients after hip surgery has no proven effect on mortality according to . Among the included studies, three studies had follow-up within 1 month; three within 4 months; one within 6 months; one at both 6 months and 12 months; and the other three followed-up only on the day of discharge (). Further large and high-quality randomized trials are needed to confirm these findings showing the unavoidable deaths of some patients.
The main limitations of this review were the small number of available studies and the gap between the follow-up times of included studies. When the publication bias was adjusted and each study was excluded from the model once, all the significant results observed remained valid. We found no evidence of existing publication bias. Moreover, data about the types, quantities, compositions, and timing of nutritional supplementation at any stage were not reported in any of the included studies.
Conclusion
The results from this meta-analysis suggest that perioperative ONS for elderly patients after hip surgery promotes early rehabilitation with reduced complications and decreased infection rate. Because of the high heterogeneity, it is unclear whether perioperative ONS has an effect on increasing serum albumin levels or reducing mortality. More high-quality investigations are needed for further detailed study.
Acknowledgments
This work was supported by the National Natural Sciences Foundation of China (grant numbers 81401813 and 31370984).
Disclosure
The authors report no conflicts of interest in this work.
References
- StevensJARuddRAThe impact of decreasing U.S. hip fracture rates on future hip fracture estimatesOsteoporos Int201324102725272823632827
- HarveyNDennisonECooperCOsteoporosis: impact on health and economicsNat Rev Rheumatol201069910520125177
- JohnellOKanisJEpidemiology of osteoporotic fracturesOsteoporos Int200516Suppl 2S3S715365697
- KanisJOdénAMcCloskeyEJohanssonHWahlDCooperCIOF Working Group on Epidemiology and Quality of LifeA systematic review of hip fracture incidence and probability of fracture worldwideOsteoporos Int20122392239225622419370
- ChengSYLevyARLefaivreKAGuyPKuramotoLSobolevBGeographic trends in incidence of hip fractures: a comprehensive literature reviewOsteoporos Int201122102575258621484361
- Bachrach-LindströmMJohanssonTUnossonMEkACWahlströmONutritional status and functional capacity after femoral neck fractures: a prospective randomized one-year follow-up studyAging (Milano)20001236637411126523
- McMurdoMEWithamMDGillespieNDIncluding older people in clinical researchBMJ20053311036103716269472
- FossNBKehletHMortality analysis in hip fracture patients: implications for design of future outcome trialsBr J Anaesth200594242915516350
- PirlichMSchützTNormanKThe German hospital malnutrition studyClin Nutr20062556357216698132
- RasmussenHHKondrupJStaunMLadefogedKKristensenHWenglerAPrevalence of patients at nutritional risk in Danish hospitalsClin Nutr2004231009101515380890
- BruunLIBosaeusIBergstadLNygaardKPrevalence of malnutrition in surgical patients: evaluation of nutritional support and documentationClin Nutr19991814114710451474
- MakJCCameronIDMarchLMNational Health and Medical Research CouncilEvidence-based guidelines for the management of hip fractures in older persons: an updateMed J Aust2010192374120047547
- Botella-CarreteroJIIglesiasBBalsaJAArrietaFZamarrónIVázquezCPerioperative oral nutritional supplements in normally or mildly undernourished geriatric patients submitted to surgery for hip fracture: a randomized clinical trialClin Nutr20102957457920199828
- FabianEGerstorferIThalerHWStundnerHBiswasPElmadfaINutritional supplementation affects postoperative oxidative stress and duration of hospitalization in patients with hip fractureWien Klin Wochenschr2011123889321253774
- PriceRDalyFPenningtonCRMcMurdoMENutritional supplementation of very old people at hospital discharge increases muscle strength: a randomised controlled trialGerontology20055117918515832045
- WyersCEReijvenPLEversSMCost-effectiveness of nutritional intervention in elderly subjects after hip fracture. A randomized controlled trialOsteoporos Int201224115116222638708
- CameronIDKurrleSEUyCLockwoodKAAuLSchaafsmaFGEffectiveness of oral nutritional supplementation for older women after a fracture: rationale, design and study of the feasibility of a randomized controlled studyBMC Geriatr2011113221663680
- DwyerAJJohnBMamMKAntonyPAbrahamRJoshiMRelation of nutritional status to healing of compound fractures of long bones of the lower limbsOrthopedics20073070971217899910
- TidermarkJPonzerSCarlssonSEffects of protein-rich supplementation and nandrolone in lean elderly women with femoral neck fracturesClin Nutr20042358759615297095
- AvenellAHandollHHNutritional supplementation for hip fracture aftercare in older peopleCochrane Database Syst Rev20101CD00188020091525
- BruceDLauranceIMcGuinessMRidleyMGoldswainPNutritional supplements after hip fracture: poor compliance limits effectivenessClin Nutr20032249750014512038
- JadadARMooreRACarrollDAssessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials1996171128721797
- HigginsJPTGreenSCochrane Handbook for Systematic Reviews of InterventionsWest SussexJohn Wiley & Sons Ltd2008
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ200332755756012958120
- ClarkeMOxmanACochrane Reviewers’. Handbook 4.0 (updated July 1999)the Cochrane Liburay Issue 1OxfordUpdate Software2000
- HigginsJPThompsonSGQuantifying heterogeneity in a meta-analysisStat Med2002211539155812111919
- HarbordRMHigginsJPTMeta-regression in StataStata J20088493519
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials198671771883802833
- BeggCBA measure to aid in the interpretation of published clinical trialsStat Med20064193992068
- Botella-CarreteroJIIglesiasBBalsaJAZamarrónIArrietaFVázquezCEffects of oral nutritional supplements in normally nourished or mildly undernourished geriatric patients after surgery for hip fracture: a randomized clinical trialJPEN J Parenter Enteral Nutr20083212012818407904
- DelmiMRapinCHBengoaJMDelmasPDVaseyHBonjourJPDietary supplementation in elderly patients with fractured neck of the femurLancet1990335101310161970070
- EnerothMOlssonUBThorngrenKGNutritional supplementation decreases hip fracture-related complicationsClin Orthop Relat Res200645121221716770284
- EspaulellaJGuyerHDiaz-EscriuFNutritional supplementation of elderly hip fracture patients. A randomized, double-blind, placebo-controlled trialAge Ageing200029542543111108415
- DuncanDGBeckSJHoodKJohansenAUsing dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma wardAge Ageing20063514815316354710
- NeumannMFriedmannJRoyMAJensenGLProvision of high-protein supplement for patients recovering from hip fractureNutrition20042041541915105027
- AppelLJSacksFMCareyVJOmniHeart Collaborative Research GroupEffects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trialJAMA20052942455246416287956
- HartgrinkHHWilleJKönigPHermansJBreslauPJPressure sores and tube feeding in patients with a fracture of the hip: a randomized clinical trialClin Nutr19981728729210205352
- GaineWJRamamohanNAHusseinNAHullinMGMcCreathSWWound infection in hip and knee arthroplastyJ Bone Joint Surg Br20008256156510855883
- WangYFYancyWSJrYuDChampagneCAppelLJLinPHThe relationship between dietary protein intake and blood pressure: results from the PREMIER studyJ Hum Hypertens20082274575418580887
- SymeonidisPDClarkDAssessment of malnutrition in hip fracture patients: effects on surgical delay, hospital stay and mortalityActa Orthop Belg20067242042717009822
- StableforthPGSupplement feeds and nitrogen and calorie balance following femoral neck fractureBr J Surg19867386516553742182
- MillerMDBannermanEDanielsLACrottyMLower limb fracture, cognitive impairment and risk of subsequent malnutrition: a prospective evaluation of dietary energy and protein intake on an orthopaedic wardEur J Clin Nutr200660785386116452913