Abstract
Objectives
To examine the rate of osteoporosis (OP) undertreatment and the association between gastrointestinal (GI) events and OP treatment initiation among elderly osteoporotic women with Medicare Part D drug coverage.
Methods
This retrospective cohort study utilized a 20% random sample of Medicare beneficiaries. Included were women ≥66 years old with Medicare Part D drug coverage, newly diagnosed with OP in 2007–2008 (first diagnosis date as the index date), and with no prior OP treatment. GI event was defined as a diagnosis or procedure for a GI condition between OP diagnosis and treatment initiation or at the end of a 12-month follow-up, whichever occurred first. OP treatment initiation was defined as the use of any bisphosphonate (BIS) or non-BIS within 1 year postindex. Logistic regression, adjusted for patient characteristics, was used to model the association between 1) GI events and OP treatment initiation (treated versus nontreated); and 2) GI events and type of initial therapy (BIS versus non-BIS) among treated patients only.
Results
A total of 126,188 women met the inclusion criteria: 72.1% did not receive OP medication within 1 year of diagnosis and 27.9% had GI events. Patients with a GI event were 75.7% less likely to start OP treatment (odds ratio [OR]=0.243; P<0.001); among treated patients, patients with a GI event had 11.3% lower odds of starting with BIS versus non-BIS (OR=0.887; P<0.001).
Conclusion
Among elderly women newly diagnosed with OP, only 28% initiated OP treatment. GI events were associated with a higher likelihood of not being treated and, among treated patients, a lower likelihood of being treated with BIS versus non-BIS.
Introduction
Over one-quarter of women aged 70 or older in the US are estimated to have osteoporosis (OP) and women account for nearly 90% of all OP cases in this age group.Citation1 Fragility fractures are the most serious consequence of OP and are more common in older patients than in their younger counterparts,Citation2,Citation3 affecting as many as 40% of those who are 85 years and older.Citation2 OP-related fractures result in significant health care costsCitation4 and they have been shown to adversely affect health-related quality of life.Citation5
Available treatments shown to reduce fracture risk include bisphosphonates (BIS) (alendronate, ibandronate, risedronate, zoledronic acid), polypeptide hormone (calcitonin), a selective estrogen receptor modulator (raloxifene), a receptor activator of nuclear factor kappa-B ligand inhibitor (denosumab), and parathyroid hormone 1–34 (teriparatide).Citation6 Based on recommendations from the National Osteoporosis Foundation, an estimated 30% of American women aged 50 years and older should be considered for pharmacologic treatment of OP to reduce the risk of fracture.Citation7,Citation8 Despite this recommendation, previous studies have demonstrated substantial undertreatment,Citation9–Citation17 including among patients who have previously experienced a fracture.Citation9,Citation15,Citation18–Citation20 The reasons for undertreatment are not fully understood.
There may be multiple barriers to treatment initiation, including concerns over side effects of OP medication.Citation21 Some observational studies have cited gastrointestinal (GI) events as contributing to therapy discontinuation of oral BIS.Citation22–Citation24 However, GI conditions are prevalent in elderly patients, as is the chronic use of non-OP medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs),Citation25 which can cause symptoms in the upper GI tract.Citation26,Citation27 The cost of therapy, patient frailty, and the presence of cognitive impairment – not uncommon in elderly fracture patientsCitation28,Citation29 – have also been identified as potential barriers to treatment.Citation29,Citation30
Given the frequency and seriousness of fractures in an elderly population, understanding the extent of treatment penetration in this population, as well as the risk factors for undertreatment, are essential to improving clinical outcomes. The objective of this study was to estimate the rate of pharmacologic treatment for OP among women with Medicare Part D coverage during the 1-year period after OP diagnosis, and to examine the association between GI events and OP treatment initiation.
Methods
Study design and data source
Review board approval was not sought as all data were de-identified and accessed in compliance with US Health Insurance Portability and Accountability Act privacy guidelines. This study used data from a random 20% sample of Medicare beneficiaries from 2006 to 2009 to identify a retrospective cohort of women diagnosed with OP during 2007–2008. The data source contains demographic data and medical (Medicare Parts A and B) and pharmacy (Medicare Part D) claims. Medicare Parts A and B claims include primary and secondary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes, Current Procedural Terminology Version 4 (CPT-4) procedure codes, type of service (including J-codes for physician-administered drugs), and setting of care (eg, physician’s office, emergency room). Medicare Part D claims include National Drug Code identifiers, days’ supply, and quantity dispensed.
Patient identification and cohort definition
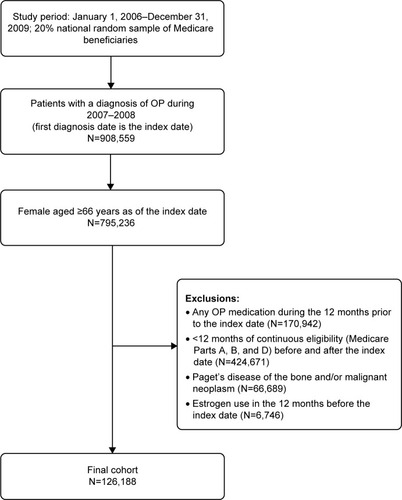
Patients newly diagnosed with OP (ICD-9-CM 733.0x) between January 1, 2007 and December 31, 2008 were identified. The index date was the first date of OP diagnosis. The baseline period (ie, preindex period) was the 12 months prior to the first OP diagnosis and patients were followed for up to 1 year after the index date (ie, postindex period). The sample was limited to women aged at least 66 years as of the index date who had continuous Medicare enrollment (with Medicare as the primary payer) in Parts A, B, and D during the entire study period (baseline and follow-up). To be included in the study, patients were also required to be naïve to OP pharmacotherapy during the baseline period, meaning that they could not have any claims for oral or intravenous BIS (alendronate, ibandronate, risedronate, zoledronic acid) or non-BIS (calcitonin, raloxifene, teriparatide). Denosumab was not included as a pharmacotherapy because it was approved in the USA in 2010, after the last index date for this study. Patients were excluded if they had a diagnosis of malignant neoplasm (ICD-9-CM codes 141–171, 173–208, and 230–239) or Paget’s disease of the bone (ICD-9-CM code 731.0) at any time during the study interval, or pharmacy claims for estrogen use during the baseline period. Treated patients were defined as those having received at least one pharmacologic OP medication identified on either Part B or Part D claims during the follow-up period. Patients who suffered a fracture and subsequently received and filled a prescription for an OP medication were considered as treated patients, but only if they had a diagnosis of OP.
Measures
Patient characteristics identified during the baseline period included age as of the index date, dual Medicare and Medicaid status, common OP-related comorbidities (from ICD-9-CM diagnosis codes: celiac disease; chronic inflammatory bowel disease; chronic inflammatory joint disease; diabetes [type 1 or type 2]; chronic kidney disease; hypertension; hyperparathyroidism; or vitamin D deficiency), bone mineral density (BMD) test status (yes/no) in the last 6 months of the baseline period, and a history of osteoporotic fractures (hip, vertebral, and nonvertebral). The count of comorbid conditions was computed using the Charlson comorbidity index (CCI), which represents 17 conditions and serves as a proxy for comorbid disease burden.Citation31 A score of 0 indicates the absence of any of the conditions, and scores >0 correspond to the number of comorbid conditions present. Medication use assessed during baseline included gastroprotective agents (proton pump inhibitors, H2-receptor blockers, and cytoprotectants), NSAIDs, and glucocorticoids. The baseline total pill burden was defined as the count of distinct oral drug molecules in the baseline period. The occurrence of GI events was also assessed during the baseline period and included acute gastritis, duodenal ulcer, duodenitis, dysphagia, gastric ulcer, esophagitis, gastroesophageal reflux disease, GI hemorrhage, nausea/vomiting, peptic ulcer, and ulcer/stricture/perforation/hemorrhage of the esophagus. Codes used to identify these events appear in . Total health care costs during the baseline period were determined from the sum of all patient-and health-plan paid amounts.
During the postindex period (follow-up), patients were considered to initiate OP treatment if they had a claim for either a BIS or a non-BIS within 12 months after the index date. Patients who initiated treatment were classified as “treated” patients, while all others were considered to be “untreated”. Among treated patients, the type of medication initiated was recorded and classified as BIS or non-BIS. The observation period for postindex GI events was 12 months for untreated patients. For treated patients, the postindex GI events were identified only up until the date of treatment initiation. Outcomes were OP treatment initiation (yes/no) and, among patients who initiated OP treatment, whether they initiated with a BIS versus a non-BIS.
Statistical analysis
Summary measures of baseline characteristics were calculated, including mean and standard deviation (SD) for continuous variables and number and percent for categorical variables. Differences in baseline characteristics between treated and untreated patients were compared using Wilcoxon rank-sum tests for continuous variables and chi-squared tests for categorical variables. Treatment outcomes (whether or not treatment was initiated and the type of treatment initiated [BIS versus non-BIS]) were modeled using logistic regression; the primary independent variable of interest was the presence or absence of postindex GI events. The model was stratified by the presence or absence of baseline GI events and also included the following adjustment variables: age (grouped in years: 66–74, 75–84, and ≥85); baseline count of CCI comorbid conditions; baseline health care costs; baseline pill burden; and binary variables indicating medication use (gastroprotective agents, glucocorticoids, and NSAIDs), dual eligibility status, baseline BMD test, and OP-related comorbidities. Two sensitivity analyses were also conducted. Because of the varying length of time between OP diagnosis and OP treatment initiation, the association between GI events that occurred after OP diagnosis and before OP treatment initiation was examined with Cox proportional hazards regression with the same adjustment variables used in the logistic regression model. The second analysis assessed the relationship between post-OP diagnosis GI events and BIS versus non-BIS treatment among patients who initiated treatment with a discrete choice conditional logit model and the same adjustment variables used in the logistic regression model. This analysis examined multiple mutually exclusive alternative choices, while the primary logistic regression analysis examined binary outcomes.
Results
Patient sample and treatment initiation patterns
A total of 126,188 patients met the study inclusion criteria (). Overall, a majority of patients (72.1%) did not initiate OP treatment in the year following their OP diagnosis; 21.6% of patients initiated BIS and 6.3% started with non-BIS (). Alendronate was the most common BIS (12.0% of patients) and calcitonin was the most common non-BIS (4.3% of patients). For those receiving OP treatment, initiation occurred, on average (SD), 75.4 (88.9) days after the index OP diagnosis.
Table 1 OP treatment patterns after diagnosis
Patient baseline characteristics
Baseline patient characteristics for all patients and by postindex OP treatment status are shown in . The mean age (SD) at the date of the first OP diagnosis was 78.5 (7.9) years. About one in five patients were dually eligible for Medicare and Medicaid. The mean (SD) count of CCI comorbid conditions was 1.53 (1.60), and the most common comorbidities identified were hypertension (76%), chronic inflammatory joint disease (59%), and diabetes (30%). Prior to the index date, 42% experienced a GI event and 12% had at least one OP-related fracture. During the baseline period, gastroprotective agents were used by 32% of the cohort, while 20% and 24% used glucocorticoids and NSAIDs, respectively.
Table 2 Baseline patient characteristics for all patients and by postindex OP treatment status
Patients initiating any OP treatment or BIS treatment were slightly younger than the patients in the respective comparator cohorts, and the proportion of patients in the OP treatment initiation group with dual eligibility was slightly higher than the cohort that did not initiate any OP treatment. A lesser percentage of patients who initiated with a BIS had dual eligibility compared to non-BIS patients. Patients initiating any OP treatment, as well as those initiating BIS, had slightly lower mean counts of CCI comorbid conditions than patients who did not initiate any OP treatment or who initiated non-BIS. During baseline, the proportion of patients with OP-related fractures was higher in both the OP treatment initiation and non-BIS treatment cohorts. The proportion of patients with gastroprotective agent use was higher in the OP treatment initiation and non-BIS treatment initiation cohorts.
Rate of GI events during baseline and follow-up periods
The distribution of patients by the presence or absence of GI events during baseline and after OP diagnosis is shown in . Overall, 41.6% of patients had a baseline GI event and 27.9% of patients had a GI event between their OP diagnosis and OP treatment initiation or end of follow-up, whichever occurred first. Among patients who did not initiate any OP treatment, 41.5% had baseline GI events; of these patients, 69.2% also experienced a GI event in the follow-up period. The rate of GI events during follow-up among all patients who did not initiate any OP treatment was 47.9%. For patients who initiated BIS, 40.0% had baseline GI events and 30.7% of these patients continued to experience GI events during follow-up. The rate of GI events during follow-up in the cohort of patients who initiated BIS was 18.9%. Among patients who initiated non-BIS, 48.7% had baseline GI events and 38.1% of these patients experienced a GI event during follow-up. The rate of GI events during follow-up was 27.0% among all patients who initiated non-BIS.
Table 3 Distribution of patients by GI events before and after OP diagnosis
Association of GI events with treatment initiation and choice of treatment
The results of the logistic regression model for the association between postindex GI events and OP treatment initiation, adjusted for patient baseline characteristics, are shown in . Patients with GI events post-OP diagnosis had lower odds of initiating any OP treatment; patients who experienced both baseline and follow-up GI events were 74.0% less likely to initiate OP treatment (odds ratio [OR]=0.260; 95% confidence interval [CI]=0.250–0.270), and patients who had only follow-up GI events (ie, no baseline events) were 75.7% less likely to initiate OP treatment (OR=0.243; 95% CI=0.232–0.254). Other risk factors for the reduced likelihood of treatment initiation included baseline comorbidities of diabetes, hypertension, chronic kidney disease, and vitamin D deficiency. Patient characteristics associated with greater odds of treatment initiation were older age, the presence of baseline BMD testing, and the baseline use of gastroprotective agents, NSAIDs, and glucocorticoids. In the sensitivity analysis, using Cox proportional hazards regression to account for the varying time from OP diagnosis to treatment initiation, the results were similar (data not shown): patients with GI events during follow-up were 70.9% less likely to initiate OP treatment (hazard ratio [HR]=0.291; 95% CI=0.284–0.299); the same pattern was evident in the strata of patients who also experienced baseline GI events (HR=0.254; 95% CI=0.246–0.264) and among those who did not have baseline GI events (HR=0.312; 95% CI=0.299–0.325).
Table 4 Logistic regression analysis of the association of postdiagnosis GI events and OP treatment initiation
The logistic regression analysis examining the association between postindex GI events and the choice of OP treatment (BIS versus non-BIS) among patients who initiated treatment, and adjusted for patient baseline characteristics, is shown in . Patients with follow-up GI events were less likely to initiate treatment with a BIS compared with a non-BIS. Patients who experienced GI events during both baseline and follow-up were 14.1% less likely to receive a BIS (OR=0.859; 95% CI=0.797–0.926), and patients with GI events only during follow-up were 11.3% less likely to receive a BIS (OR=0.887; 95% CI=0.804–0.979). Other risk factors for the reduced likelihood of receiving a BIS included older age, higher pill burden, greater number of CCI comorbid conditions, and gastroprotective agent use. Patient characteristics associated with a greater likelihood of initiating with a BIS versus a non-BIS included the presence of a baseline BMD test and the baseline use of glucocorticoids and NSAIDs. The results of the sensitivity analysis employing a discrete choice model showed that patients with GI events during follow-up (irrespective of baseline GI events) had 11.6% lower odds of initiating BIS versus non-BIS (OR=0.884; 95% CI=0.829–0.942), and that patients with baseline GI events (irrespective of follow-up GI events) were 9.0% less likely to receive BIS versus non-BIS (OR=0.910; 95% CI=0.856–0.967) (data not shown).
Table 5 Logistic regression of the association of postdiagnosis GI events and the type of treatment initiated among those patients who initiated treatment
Discussion
This study demonstrates significant undertreatment among osteoporotic women with Medicare Part D coverage. Only 27.9% of patients started OP treatment in the first year after their diagnosis. Patients who experienced GI events following their OP diagnosis were 74%–76% less likely to initiate OP treatment than their counterparts who did not experience a postdiagnosis GI event. Among patients who did begin treatment, GI events were associated with 11%–14% lower likelihood of receiving BIS versus non-BIS treatment. The association between GI events and both OP treatment initiation and choice of OP treatment were robust in the sensitivity analyses.
The significant undertreatment of OP we found in this study is consistent with previous research. In studies of elderly patients with low-impact fractures or surgical repair of fracture, over 70% lacked treatment with OP medications other than estrogen prior to experiencing a fracture.Citation9,Citation10,Citation13,Citation14 In a retrospective analysis of claims data that identified patients based on an OP diagnosis or low bone mass density during 2000–2007 (mean age: 67 years), 42% received treatment within 90 daysCitation32 and, in a study that utilized data from the 2007 National Health and Wellness Survey, only 55% of those who self-reported a diagnosis of OP (mean age: 64 years) also reported using prescription medication to treat OP.Citation33
The literature examining the contribution of GI events to OP treatment initiation and choice of OP treatment is sparse. However, some studies have suggested a potential relationship. In a study of elderly women who had experienced a wrist or hip fracture, a prior history of GI disease was associated with slightly lower, although not significantly lower, odds of receiving either OP treatment or BMD testing within 6 months of the fracture.Citation34 However, this study was not limited to patients who were naïve to OP treatment, and prior OP treatment was by far the strongest predictor of receipt of OP treatment postfracture. Our population included only women who were OP treatment naïve, and our outcome was OP treatment initiation, not the combination of OP treatment initiation or BMD testing; thus, our study likely provides a more refined assessment of the association between pretreatment GI events and OP treatment initiation. Among patients who initiated OP treatment, we also noted slightly higher odds of receiving non-BIS treatment among patients who experienced a pretreatment GI event. Foster et alCitation35 examined the relationship between patient characteristics and the receipt of raloxifene versus BIS; in their Medicare/commercially-insured cohort, patients with a pretreatment gastric ulcer, but not other GI conditions, had greater odds of receiving raloxifene compared with BIS, but the association was not apparent in the Medicaid cohort. There were several differences between the two studies, including the pretreatment rate of GI events. The baseline rate of GI events was 41.6% in our study versus less than 10% of patients in either the Medicare/commercial or Medicaid cohort in the study by Foster et al.Citation35 We also used a more comprehensive series of codes to define a GI event and examined the collective impact of all GI events on choice of OP treatment, rather than individual categories of GI events (eg, peptic ulcer, gastric ulcer). Further, our non-BIS cohort was not limited to only patients receiving raloxifene, but it also included patients initiating treatment with calcitonin or teraparatide.
There were other characteristics, in addition to GI events, that were predictive of OP treatment initiation in our study. The strongest predictor of treatment initiation was the presence of a BMD test during baseline. Patients with a baseline BMD test were more than twice as likely to initiate OP treatment when compared with patients who did not have a baseline BMD test and, among patients who initiated OP treatment, those with a baseline BMD test were 2.4 times more likely to receive BIS versus non-BIS. There was also a modest, positive association between older age and OP treatment initiation. Some, but not all, previous studies have shown a positive link between older age and treatment initiation.Citation32,Citation36–Citation38 The use of gastroprotective agents, NSAIDS, and glucocorticoids at baseline was also positively correlated with treatment initiation. Previous studies have noted a similar association between glucocorticoid or corticosteroid use and treatment initiation.Citation32,Citation34,Citation37 Chronic kidney disease was also associated with a slightly lower likelihood of treatment initiation. Alendronate, the most commonly prescribed treatment in this study, is contraindicated for patients with severe renal impairment.
Our findings advance the understanding of the patient characteristics that contribute to undertreatment, an essential step in improving the management of OP patients. GI events are prevalent in older women diagnosed with OP, and our results suggest that GI events that occur following OP diagnosis are a significant risk factor for failure to initiate OP treatment. Elderly women have a heightened risk of fracture, and the clinical management of these patients should integrate characteristics that promote treatment and address risk factors for undertreatment. Future research is needed to distinguish between characteristics driven by clinician prescribing patterns versus patient choice to appropriately target interventions that promote treatment.
Limitations
There are several limitations to our study, and the results should be considered in this context. We included only patients with a claim for an OP diagnosis. BMD test results were not available to confirm the diagnosis, and the presence of a diagnosis code may indicate that a patient was simply screened for OP, potentially inflating our estimate of under-treatment. We also used Medicare prescription drug claims data to determine OP treatment initiation. If a patient had non-Medicare prescription drug coverage, claims for OP pharmacotherapy would not be captured in this analysis. We do not know the rationale for not initiating OP treatment, which may reflect a clinician’s decision not to prescribe treatment or a patient decision not to fill a prescription. Only GI events that resulted in medical service utilization were captured in this analysis. The potential association between less severe events (ie, that did not result in a medical encounter) and treatment initiation is unknown. Claims data do not provide information regarding the severity of symptoms (other than the medical classification) associated with each GI event, which could influence treatment initiation. Further, our analysis examining the relationship between baseline medication use and treatment initiation is limited to prescription drug claims and would not include over-the-counter drugs such as low-dose NSAIDs and aspirin. There may have been other unmeasured patient and clinician characteristics that influenced OP treatment initiation and the receipt of BIS versus non-BIS treatment. Finally, our results are based on a sample of women aged 66 years and older with Medicare Parts A, B, and D coverage, and they may not be applicable to younger patients or to patients with other forms of insurance.
Conclusion
Among women with Medicare Part D coverage, only 28% of those diagnosed with OP received pharmacologic treatment for OP in the first year following the diagnosis. A total of 28% experienced a GI event between their diagnosis and OP treatment initiation during the first year of OP diagnosis. The presence of a GI event following OP diagnosis was associated with 76% lower odds of initiating OP treatment. Among patients who did initiate OP treatment, a postdiagnosis GI event was associated with 11% lower odds of initiating BIS versus non-BIS treatment.
Acknowledgments
This study was funded by Merck & Co., Inc. Medical writing support was provided by Optum (Eden Prairie, MN) and funded by Merck & Co., Inc.
Disclosure
Ethel S Siris has done consulting for Amgen, Eli Lilly, Merck, Novartis, AgNovos and Radius. Katalin Bognar and Anshu Shrestha are employees of Precision Health Economics, LLC which provides consulting services to Merck. Mitch DeKoven is an employee of IMS Health which provides consulting services to Merck. John A Romley provided consulting services to Precision Health Economics in support of this study. Ankita Modi is an employee of Merck & Co., Inc. Jingbo Yu was an employee of Merck & Co., Inc. at the time of the study and during manuscript development.
Supplementary material
Table S1 Codes for the identification of gastrointestinal events
References
- WrightNCLookerACSaagKGThe Recent Prevalence of Osteoporosis and Low Bone Mass in the United States Based on Bone Mineral Density at the Femoral Neck or Lumbar SpineJ Bone Miner Res201429112520252624771492
- EttingerBBlackDMDawson-HughesBPressmanARMeltonLJ3rdUpdated fracture incidence rates for the US version of FRAXOsteoporos Int2010211253319705048
- PfeilschifterJCooperCWattsNBRegional and age-related variations in the proportions of hip fractures and major fractures among postmenopausal women: the Global Longitudinal Study of Osteoporosis in WomenOsteoporos Int20122382179218822086311
- BlumeSWCurtisJRMedical costs of osteoporosis in the elderly Medicare populationOsteoporos Int20112261835184421165602
- RouxCWymanAHoovenFHGLOW investigatorsBurden of non-hip, non-vertebral fractures on quality of life in postmenopausal women: the Global Longitudinal study of Osteoporosis in Women (GLOW)Osteoporos Int201223122863287122398855
- WattsNBBilezikianJPCamachoPMAACE Osteoporosis Task ForceAmerican Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosisEndocr Pract201016Suppl 313721224201
- National Osteoporosis FoundationThe Clinician’s Guide to Prevention and Treatment of OsteoporosisWashington, DCNational Osteoporosis Foundation2014 Available from: http://nof.org/files/nof/public/content/file/2791/upload/919.pdfAccessed January 12, 2015
- Dawson-HughesBLookerACTostesonANJohanssonHKanisJAMeltonLJThe potential impact of the National Osteoporosis Foundation guidance on treatment eligibility in the USA: an update in NHANES 2005–2008Osteoporos Int201223381182021717247
- AndradeSEMajumdarSRChanKALow frequency of treatment of osteoporosis among postmenopausal women following a fractureArch Intern Med2003163172052205714504118
- GleasonLJMenziesIBMendelsonDAKatesSLFriedmanSMDiagnosis and treatment of osteoporosis in high-risk patients prior to hip fractureGeriatr Orthop Surg Rehabil201232798323569701
- GreenspanSLWymanAHoovenFHPredictors of treatment with osteoporosis medications after recent fragility fractures in a multinational cohort of postmenopausal womenJ Am Geriatr Soc201260345546122316070
- GugginaPFlahiveJHoovenFHGLOW InvestigatorsCharacteristics associated with anti-osteoporosis medication use: data from the Global Longitudinal Study of Osteoporosis in Women (GLOW) USA cohortBone201251697598022964142
- PetrellaRJJonesTJDo patients receive recommended treatment of osteoporosis following hip fracture in primary care?BMC Fam Pract200673116684358
- PremaorMOPilbrowLTonkinCAdamsMParkerRACompstonJLow rates of treatment in postmenopausal women with a history of low trauma fractures: results of audit in a Fracture Liaison ServiceQJM20101031334019864348
- SimonelliCChenYTMoranceyJLewisAFAbbottTAEvaluation and management of osteoporosis following hospitalization for low-impact fractureJ Gen Intern Med2003181172212534759
- SinghSFosterRKhanKMAccident or osteoporosis?: Survey of community follow-up after low-trauma fractureCan Fam Physician2011574e128e13321490344
- TeedeHJJayasuriyaIAGilfillanCPFracture prevention strategies in patients presenting to Australian hospitals with minimal-trauma fractures: a major treatment gapIntern Med J2007371067467917894764
- KrothPJMurrayMDMcDonaldCJUndertreatment of osteoporosis in women, based on detection of vertebral compression fractures on chest radiographyAm J Geriatr Pharmacother20042211211815555487
- LüthjePNurmi-LüthjeIKaukonenJPKuurneSNaboulsiHKatajaMUndertreatment of osteoporosis following hip fracture in the elderlyArch Gerontol Geriatr200949115315718706704
- PannemanMJLipsPSenSSHeringsRMUndertreatment with anti-osteoporotic drugs after hospitalization for fractureOsteoporos Int200415212012414618302
- National Osteoporosis Foundation [webpage on the Internet]Types of osteoporosis medicationsWashington, DCNational Osteoporosis Foundation2014 Available from: http://nof.org/articles/22Accessed July 21,2014
- EttingerBAlendronate use among 812 women: prevalence of gastrointestinal complaints, noncompliance with patient instructions, and discontinuationJ Manage Care Spec Pharm199845488492
- HamiltonBMcCoyKTaggartHTolerability and compliance with risedronate in clinical practiceOsteoporos Int200314325926212730745
- TurbíCHerrero-BeaumontGAcebesJCCompliance and satisfaction with raloxifene versus alendronate for the treatment of postmenopausal osteoporosis in clinical practice: An open-label, prospective, nonrandomized, observational studyClin Ther200426224525615038947
- HallKEProctorDDFisherLRoseSAmerican gastroenterological association future trends committee report: effects of aging of the population on gastroenterology practice, education, and researchGastroenterology200512941305133816230084
- Knopp-SihotaJACummingsGGHomikJVoaklanderDThe association between serious upper gastrointestinal bleeding and incident bisphosphonate use: a population-based nested cohort studyBMC Geriatr2013133623602075
- VestergaardPSchwartzKPinholtEMRejnmarkLMosekildeLGastric and esophagus events before and during treatment of osteoporosisCalcif Tissue Int201086211011519957165
- DanielsAHDaielloLALareauCRPreoperative cognitive impairment and psychological distress in hospitalized elderly hip fracture patientsAm J Orthop (Belle Mead NJ)2014437E146E15225046191
- SwitzerJAJaglalSBogochEROvercoming barriers to osteoporosis care in vulnerable elderly patients with hip fracturesJ Orthop Trauma200923645445919550234
- SimonelliCKilleenKMehleSSwansonLBarriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeonsMayo Clin Proc200277433433811936928
- QuanHSundararajanVHalfonPCoding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative dataMed Care200543111130113916224307
- AscheCNelsonRMcAdam-MarxCJhaveriMYeXPredictors of oral bisphosphonate prescriptions in post-menopausal women with osteoporosis in a real-world setting in the USAOsteoporos Int20102181427143619798459
- MeadowsESMitchellBDBolgeSCJohnstonJAColNFFactors associated with treatment of women with osteoporosis or osteopenia from a national surveyBMC Womens Health201212122225919
- BlockAESolomonDHCadaretteSMMogunHChoudhryNKPatient and physician predictors of post-fracture osteoporosis managementJ Gen Intern Med20082391447145118584260
- FosterSAFoleyKAMeadowsESCharacteristics of patients initiating raloxifene compared to those initiating bisphosphonatesBMC Womens Health200882419105828
- CranneyATsangJFLeslieWDFactors predicting osteoporosis treatment initiation in a regionally based cohortOsteoporos Int20092091621162519096744
- PressmanAForsythBEttingerBTostesonANInitiation of osteoporosis treatment after bone mineral density testingOsteoporos Int200112533734211444079
- RyderKMShorrRITylavskyFAHealth ABC StudyCorrelates of use of antifracture therapy in older women with low bone mineral densityJ Gen Intern Med200621663664116808749