Abstract
Background and purpose
Cervical spondylosis is well accepted as a common degenerative change in the cervical spine. Compelling evidence has shown that the incidence of cervical spondylosis increases with age. However, the relationship between age and the incidence of cervical spondylosis remains obscure. It is essential to note the relationship between age and the incidence of cervical spondylosis through more and more clinical data.
Methods
In the case-controlled study reported here, retrospective clinical analysis of 1,276 cases of cervical spondylosis has been conducted. We analyzed the general clinical data, the relationship between age and the incidence of cervical spondylosis, and the relationship between age-related risk factors and the incidence of cervical spondylosis. A chi-square test was used to analyze the associations between different variables. Statistical significance was defined as a P-value of less than 0.05.
Results
The imaging examination demonstrated the most prominent characteristic features of cervical spondylosis: bulge or herniation at C3-C4, C4-C5, and C5-C6. The incidence of cervical spondylosis increased with aging before age 50 years and decreased with aging after age 50 years, especially in the elderly after 60 years old. The occurrence rate of bulge or herniation at C3-C4, C4-C5, C5-C6, and C6-C7 increased with aging before age 50 years and decreased with aging after age 50 years, especially after 60 years. Moreover, the incidence of hyperosteogeny and spinal stenosis increased with aging before age 60 years and decreased with aging after age 60 years, although there was no obvious change in calcification. The age-related risk factors, such as hypertension, hyperlipidemia, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking, have no relationship with the incidence of cervical spondylosis.
Conclusion
A decreasing proportion of cervical spondylosis with aging occurs in the elderly, while the proportion of cervical spondylosis increases with aging in the young and the adults. This investigation implicates that aging is not only a contributor to the clinical performance of cervical spondylosis in the elderly, although the incidence of cervical spondylosis is proportional to the progress of age.
Introduction
Cervical spondylosis is a chronic degenerative process of the cervical spine that affects the vertebral bodies and intervertebral disks of the neck, and may progress into disk herniation, bone spur formation, compression of the spinal cord, or cervical spondylotic myelopathy.Citation1 Cervical spondylosis often develops at multiple interspaces and worsens with age.Citation2,Citation3 Cervical spondylosis can be identified in the majority of people older than 50 years. There also appears to be a genetic predisposition to develop diseases of the skeletal elements of the spine because some families will have more of these changes.Citation4–Citation6 It can also be shown that the degenerative changes in the cervical spines of twins follow a very similar pattern.Citation6,Citation7 Chronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. Spondylotic changes are frequently found in many asymptomatic adults, resulting in stenosis of the spinal canal, lateral recess, and foramina.Citation8,Citation9 Radiculopathy is a result of intervertebral foramina narrowing. Spinal canal stenosis can lead to spinal cord compression, ultimately resulting in cervical spondylosis myelopathy.Citation8 Cervical disk herniation occurs when the nucleus in the center of the disc pushes out of its normal space.Citation10 The nucleus presses against the annulus, causing the disc to bulge outward. Gradually, the nucleus herniates completely through the annulus and crushes the disc, compressing the spinal canal or nerve roots. Additionally, the nucleus releases chemicals that can irritate the surrounding nerves causing inflammation and pain.Citation11,Citation12 Symptoms of cervical spondylosis include one, or a combination, of the following: numbness, weakness and tingling in the neck and/or arms, pain in the neck and/or arms, neck stiffness, headaches, symptomatic compression of the spinal cord (myelopathy) orCitation13 nerve roots (radiculopathy)Citation14 or a combination of the two (myeloradiculopathy), or problems with bladder function from cervical myelopathy.Citation15,Citation16
Cervical spondylosis is a disorder of age-related wear affecting the disks and vertebrae of cervical spine.Citation17 Increasing clinical imaging data evidence that age is a risk factor and a contributor to the incidence of cervical spondylosis that increases with aging.Citation18,Citation19 However, our clinical investigation has recently demonstrated that the trend of the incidence of cervical spondylosis decreases with aging in the elderly and increases with aging in the young and the adults.
Clinical data and methods
The study was conducted at Renmin Hospital, Hubei University of Medicine in the Central China. It is a general hospital with over 2,500 outpatient visits daily and 2,800 inpatient beds. Subjects (n=1,276) with cervical spondylosis were included. In this study, all data from January 2013 to December 2014 were collected from the all departments of Renmin Hospital, Hubei University of Medicine. This study was approved by the Research Ethics Board of Hubei University of Medicine. Diagnoses were determined according to 2012 ICD-9-CM Diagnosis Code 721 (721.0 Cervical spondylosis without myelopathy, 721.1 Cervical spondylosis with myelopathy). The comprehensive diagnostic process included medical history, physical examination, and diagnostic tests. All patients with cervical injury, tumor, or infection were excluded from the study. Computed tomography scans and/or magnetic resonance imaging were performed to confirm the diagnosis of cervical spondylosis. The clinical data of all cases were collected, including variables on sociodemographic characteristics, age-related risk factors (hypertension, hyperlipidemia, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking), and physical examination findings such as body weight, height, hip and waist circumferences, and blood pressure.
Retrospective clinical analysis of 1,276 cases of cervical spondylosis has been conducted. The data were edited and entered into a computer to be analyzed using SPSS, Windows version 13.0 (IBM Corporation, Armonk, NY, USA). A chi-square test was used to analyze the associations between different variables. Statistical significance was defined as a P-value of less than 0.05.
Results
The general clinical data analysis
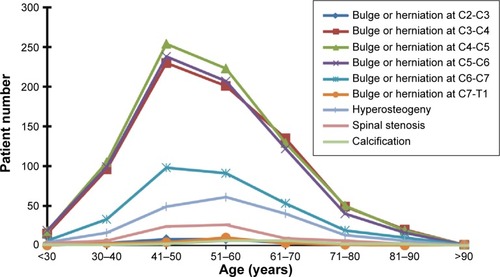
The general clinical data demonstrated that the main symptoms and signs of cervical spondylosis involved pain in the back, neck and/or arms, weakness and tingling in the neck and/or arms, dizziness, headache, vertigo and instability while walking, nausea and vomiting, and neck stiffness. The most prevalent symptom was pain in the back, neck, and/or arms (). The imaging examination with computed tomography and/or magnetic resonance imaging presented the most prominent characteristic features of cervical spondylosis: bulge or herniation at C3-C4, C4-C5, and C5-C6, besides spinal stenosis, vertebral hyperostosis, calcification, and the disappearance of the spine’s physiological curvature ().
Table 1 Clinical symptoms and signs
Table 2 Imaging features
The analysis of relationship between age and the incidence of cervical spondylosis
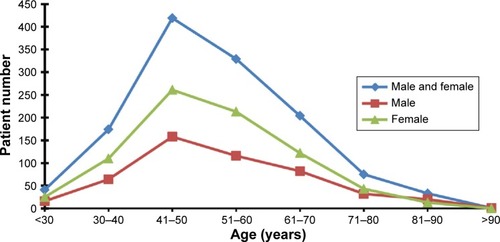
In general, clinical data showed that the proportion of patients with cervical spondylosis increased with aging before age 50 years and decreased with aging after age 50 years, especially in the elderly after 60 years. The same results were found in both the male and the female subjects. There is an obvious decrease in the incidence of the disease in elderly female patients ( and ).
Table 3 Age distribution of patients with cervical spondylosis
The imaging findings ( and ) are consistent with the previous results that the proportion of cervical spondylosis increased with aging before age 50 years and decreased with aging after age 50 years. The occurrence rate of bulge or herniation at C3-C4, C4-C5, and C5-C6, the most prominent characteristic imaging features, increased with aging before age 50 years and decreased with aging after age 50 years, especially after 60 years. The same finding was observed in the bulge or herniation at C6-C7. In addition, the proportion of hyperosteogeny and spinal stenosis increased with aging before age 60 years and decreased with aging after age 60 years, although there was no obvious change in calcification.
Table 4 Age distribution of patients with imaging features of cervical spondylosis
The relationship between risk factors and the incidence of cervical spondylosis
The association between the clinical risk factors and cervical spondylosis is listed in . It seems that the most related element with cervical spondylosis was hypertension. However, showed that the age-related risk factors (hypertension, hyperlipidemia, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking) have no relationship with the incidence of cervical spondylosis.
Table 5 Clinical risk factors
Table 6 The relationship between risk factors and the incidence of cervical spondylosis
Discussion
The one hospital-based clinical investigation showed that the most prevalence symptom of cervical spondylosis is pain in the back, neck, and/or arms, and the most prominent characteristic feature is the bulge or herniation at C3-C4, C4-C5, and C5-C6. The most age-related risk element with cervical spondylosis was hypertension, and to a lesser extent, hyperlipidemia, diabetes, cerebral infarct, cardiovascular diseases, smoking, and drinking. Different from past reports that the incidence of cervical spondylosis increases with aging, the distinctive characteristics of this study have indicated that the incidence of cervical spondylosis increases with aging before age 50 years, and decreases with aging after age 50 years, especially in the elderly after 60 years.
Increasing evidence shows that intervertebral disks lose hydration and elasticity with age, gradually resulting in cracks and fissures and causing a loss of their elastic properties for the surrounding ligaments and developing the onset of spurs.Citation20–Citation23 The disk subsequently collapses as a result of biomechanical disability, leading to serious consequences (the annulus to bulge outward). Annulus fissures and herniation can occur directly after the annulus bulges.Citation18,Citation24 Disk herniation may be a very poor source of chronic spondylotic changes on the basis of annulus fissures and herniation.Citation25,Citation26 An increasing clinical and pathological literature supports that cervical spondylotic changes are also a common occurrence with age.Citation19 With the progress of cervical spondylotic changes, symptoms often develop slowly over time, such as headache, neck stiffness, pain in the back, neck and/or arms, weakness and tingling in the neck and/or arms, dizziness, and so on.Citation27–Citation30 Patients with cervical spondylosis usually present with neck pain with or without radiculopathy or myelopathy.Citation26,Citation31 It is well known that the major risk factor is aging. By the age of 60, most persons show signs of cervical spondylosis (according to imaging examination).Citation2,Citation3,Citation19 With the process of aging, discs gradually dry out, lose their strength and resiliency, and easily induce the occurrence of herniation.Citation32,Citation33 Accordingly, the clinical presentation will become more pronounced. However, our clinical investigation has implicated that the incidence of cervical spondylosis decreases with aging in the elderly population, especially after 60 years, although it increases with aging before age 50 years. Further assays subsequently proved that there is no relationship between the incidence of cervical spondylosis in the elderly and the age-related risk factors. Thus, we addressed the pathogenesis of cervical spondylosis and showed that the volume and inflammation of the nucleus gets lesser since chronic degeneration contributes to atrophy of the nucleus with the aging process.Citation34–Citation36 The pressure from the nucleus will become gradually less, resulting in the lower incidence of annulus injury and occurrence of cervical spondylosis, and less clinical manifestations, especially after 60 years of age. Considering that the inflammatory effect of the nucleus is stronger than degeneration in the young and the adults before 50 years, the highest incidence of cervical spondylosis corresponds with this age stage – approximately 50 years. With the process of aging, the inflammatory effect of the nucleus is weaker than the degeneration of the nucleus after 60 years of age, the incidence of cervical spondylosis will decrease with aging.
Cervical spondylosis is a common condition that is estimated to account for the degenerative changes in the cervical spine, with approximately 90% of cases occurring in those older than 50 years.Citation37,Citation38 Age may play a dual role in the pathogenesis of cervical spondylosis. In different age stages, cervical spondylosis will have a different clinical feature. In consideration of the previous finding that the incidence of cervical spondylosis increases with aging before age 50 years and decreases with aging after age 50 years, our clinical data indicated that surgery is not the treatment of first choice in elderly patients with cervical spondylosis. If it is not an acute case of nerve and spinal cord compression, nonoperative therapeutic interventions should be designed for the elderly cervical spondylosis patients, such as physical therapy and pain medications. Older cervical spondylosis patients usually have more lesions of cervical disc levels, and then surgery will not benefit to improve functional outcome.Citation39,Citation40 As age progresses, the volume of the nucleus becomes smaller, and the pressure from the nucleus is less. Hence, the mainstay of the treatment for the old adult patients with cervical spondylosis is in a rehabilitation center if they present with degenerative changes and have no acute symptoms and signs. Moreover, this study also provides new consideration for the future treatment of cervical spondylosis, especially in the elderly population.
Acknowledgments
This work was supported by grants from the Natural Science Foundation of Hubei Province (2015CFB260), the Hubei Province Health and Family Planning Scientific Research Project (WJ2015MB219), the Shiyan Natural Science Foundation (15K70), and the Natural Science Foundation of Renmin Hospital, Hubei University of Medicine to Dr Zhiyou Cai.
Disclosure
The authors report no conflicts of interest in this work.
References
- XiongWLiFGuanHTetraplegia after thyroidectomy in a patient with cervical spondylosis: a case report and literature reviewMedicine (Baltimore)2015946e52425674751
- MamataHJoleszFAMaierSEApparent diffusion coefficient and fractional anisotropy in spinal cord: age and cervical spondylosis-related changesJ Magn Reson Imaging2005221384315971186
- ZalewskiPKonopkaWPietkiewiczPAnalysis of vascular vertigo due to cervical spondylosis and vertebro-basilar insufficiency based on sex and age in clinical materialsOtolaryngol Pol200458197100 Polish15101267
- YooKOrigitanoTCFamilial cervical spondylosis. Case reportJ Neurosurg19988911391419647185
- WilsonJRPatelAABrodtEDDettoriJRBrodkeDSFehlingsMGGenetics and heritability of cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: results of a systematic reviewSpine (Phila Pa 1976)20133822 Suppl 1S123S14623963008
- MukerjiNSinarEJIdentical twins with cervical myelopathy: a case for hereditary cervical spondylosis? Report of two cases and review of the literatureJ Neurosurg Spine20076434434917436924
- PalmerPEStadalnickRArnonSThe genetic factor in cervical spondylosisSkeletal Radiol19841131781826538995
- KellyJCGroarkePJButlerJSPoyntonARO’ByrneJMThe natural history and clinical syndromes of degenerative cervical spondylosisAdv Orthop2012201239364222162812
- InoueSMoriyamaTTachibanaTRisk factors for intraoperative lateral mass fracture of lateral mass screw fixation in the subaxial cervical spineJ Neurosurg Spine2014201111724180312
- PetersonCKSchmidCLeemannSAnklinBHumphreysBKOutcomes from magnetic resonance imaging-confirmed symptomatic cervical disk herniation patients treated with high-velocity, low-amplitude spinal manipulative therapy: a prospective cohort study with 3-month follow-upJ Manipulative Physiol Ther201336846146723948425
- PodichettyVKThe aging spine: the role of inflammatory mediators in intervertebral disc degenerationCell Mol Biol (Noisy-le-grand)200753541817543240
- NackleyAGMakriyannisAHohmannAGSelective activation of cannabinoid CB(2) receptors suppresses spinal fos protein expression and pain behavior in a rat model of inflammationNeuroscience2003119374775712809695
- KatoYNishidaNTaguchiTParaplegia caused by posture during MRI in a patient with cervical disk herniationOrthopedics201033644820806756
- TzengYSChenSGChenTMHerniation of the cervical disk in plastic surgeonsAnn Plast Surg201269667267423154341
- AurichMHofmannGOGrasFMCervical myelopathy after low grade distortion of the cervical spine: possible association with pre-existing spondylosis of the cervical spineUnfallchirurg20151184372375 German25336350
- JohanssonBDegeneration of the cervical vertebral disk is seldom the only cause of disk herniation. Cause of disk herniation is a common dispute in insurance cases after whiplash injuriesLakartidningen1999963435403541 Swedish10492559
- IwanamiAToyamaYCervical spondylosisNihon Rinsho2014721017551760 Japanese25509798
- NagashimaHDokaiTHashiguchiHClinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: a multi-center retrospective studyEur Spine J201120224024621197553
- HayashiHOkadaKHamadaMTadaKUenoREtiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spineClin Orthop Relat Res19872142002093791744
- CuellarVGCuellarJMVaccaroARCarrageeEJScuderiGJAccelerated degeneration after failed cervical and lumbar nucleoplastyJ Spinal Disord Tech201023852152421131800
- PavlovaMNPogozhevaTIStructural and functional characteristics of the intervertebral disks of infants in the 1st year of lifeArkh Anat Gistol Embriol198079119198 Russian7458700
- StokesIALaibleJPGardner-MorseMGCostiJJIatridisJCRefinement of elastic, poroelastic, and osmotic tissue properties of intervertebral disks to analyze behavior in compressionAnn Biomed Eng201139112213120711754
- TyndykMAMcGarryJPBarronVEffects of intervertebral disk degeneration on the flexibility of the human thoracolumbar spineJ Long Term Eff Med Implants200818426928820370640
- Del GrandeFMausTPCarrinoJAImaging the intervertebral disk: age-related changes, herniations, and radicular painRadiol Clin North Am201250462964922643389
- MisterskaEJankowskiRGlowackiMChronic pain coping styles in patients with herniated lumbar discs and coexisting spondylotic changes treated surgically: considering clinical pain characteristics, degenerative changes, disability, mood disturbances, and beliefs about pain controlMed Sci Monit2013191211122024370564
- Fernandez de RotaJJMeschianSFernandez de RotaAUrbanoVBaronMCervical spondylotic myelopathy due to chronic compression: the role of signal intensity changes in magnetic resonance imagesJ Neurosurg Spine200761172217233286
- MisterskaEJankowskiRGlowackiMPsychometric properties of the Polish language version of the chronic pain coping inventory-42 for patients treated surgically due to herniated lumbar discs and spondylotic changesMed Sci Monit20142078980124824781
- RaoRNeck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluationInstr Course Lect20035247948812690874
- SasakiHPrograms for continuing medical education: a session; 4. Clinical manifestation of cervical spondylosisNihon Naika Gakkai Zasshi20121013675679 Japanese22620034
- TakagiIEliyasJKStadlanNCervical spondylosis: an update on pathophysiology, clinical manifestation, and management strategiesDis Mon2011571058359122036114
- GerardCSO’TooleJECurrent techniques in the management of cervical myelopathy and radiculopathyNeurosurg Clin N Am201425226127024703445
- MorishitaYNaitoMHymansonHMiyazakiMWuGWangJCThe relationship between the cervical spinal canal diameter and the pathological changes in the cervical spineEur Spine J200918687788319357877
- KokuboYUchidaKKobayashiSHerniated and spondylotic intervertebral discs of the human cervical spine: histological and immunohistological findings in 500 en bloc surgical samples. Laboratory investigationJ Neurosurg Spine20089328529518928227
- TakanoMKawabataSKomakiYInflammatory cascades mediate synapse elimination in spinal cord compressionJ Neuroinflammation2014114024589419
- BeattieMSManleyGTTight squeeze, slow burn: inflammation and the aetiology of cervical myelopathyBrain2011134Pt 51259126121596766
- NagashimaHMorioYYamaneKNanjoYTeshimaRTumor necrosis factor-alpha, interleukin-1beta, and interleukin-6 in the cerebrospinal fluid of patients with cervical myelopathy and lumbar radiculopathyEur Spine J200918121946195019543752
- BirnieDHealeyJSKrahnADPrevalence and risk factors for cervical and lumbar spondylosis in interventional electrophysiologistsJ Cardiovasc Electrophysiol201122995796021385267
- OkadaEMatsumotoMIchiharaDAging of the cervical spine in healthy volunteers: a 10-year longitudinal magnetic resonance imaging studySpine (Phila Pa 1976)200934770671219333104
- TauchiRImagamaSInohHRisk factors for a poor outcome following surgical treatment of cervical spondylotic amyotrophy: a multicenter studyEur Spine J201322115616123001450
- InuiYMiyamotoHSumiMUnoKClinical outcomes and predictive factors relating to prognosis of conservative and surgical treatments for cervical spondylotic amyotrophySpine (Phila Pa 1976)2011361079479920736889