Abstract
Background
This study aims at assessing the clinical results, radiographic findings, and associated complications after osteosynthesis of trochanteric hip fractures with proximal femoral nail (PFN).
Methods
A total of 152 patients with hip fractures who underwent osteosynthesis with PFN were included. The hip fracture types in the patients included in the study were classified according to the American Orthopedic/Orthopedic Trauma Association (AO/OTA). AO/OTA A1, A2, and A3 type fractures were found in 24 (15.8%), 107 (70.4%), and 21 (13.8%) patients, respectively. The Baumgaertner scale was used to assess the degree of postoperative reduction. The Salvati–Wilson hip function (SWS) scoring system was used to evaluate functional results. After a follow-up period, clinical and radiographic results were evaluated and complications were assessed. The relationship between the complications and SWS score, age, sex, fracture type, reduction quality, and time from the fracture to surgery was evaluated.
Results
Eighty-five (55.9%) female patients and 67 (44.1%) male patients were enrolled in the study. Seventy-nine (51.9%) patients had left hip fractures, and 73 (48.1%) had right hip fractures. The mean age was 76 (range 21–93) years, and the mean follow-up duration was 23.6 (range 7–49) months. Postoperatively, one patient (0.6%) had a poor reduction, 16 patients (10.5%) had an acceptable reduction, and 135 patients (88.9%) had a good reduction according to the above criteria. The SWS scores were excellent, good, moderate, and poor in 91 (59.8%), 45 (29.6%), 15 (9.8%), and one (0.6%) patients, respectively. Late postoperative complications were seen in 27 patients (17.7%). A total of 14 patients (9.2%) underwent a revision procedure for mechanical complications.
Conclusion
The study results suggest that the quality of fracture reduction is an important factor that affects the revision rate and SWS score in patients with mechanical complications after osteosynthesis with PFN for trochanteric fractures.
Introduction
Trochanteric femoral fractures are often seen in patients aged >65 years; they can be caused by high-energy or low-energy trauma or may be pathological in nature.Citation1–Citation4 Particularly in the elderly, hip fractures are a major cause of increased mortality and morbidity.Citation4,Citation5 Because of the decreased physical capacity, concomitant systemic diseases, and increased vulnerability to environmental dangers, even low-energy trauma can cause unstable femoral trochanteric fractures in this age group.Citation5–Citation7 Surgical management of hip fractures is targeted to help patients recover to the closest degree of functionality they had prior to the trauma; this is achieved by utilizing the most appropriate treatment methods and early ambulation, thereby preventing potential complications.Citation6,Citation8
Fractures involving the trochanteric area of the proximal femur are classified according to the American Orthopedic/Orthopedic Trauma Association (AO/OTA) classification system as AO/OTA 31-A, which delineates them as extracapsular fractures of the hip. These fractures are then subdivided into groups A1, A2, and A3. Simple, two-part fractures are classified as A1 fractures, whereas A2 fractures have multiple fragments. More complex fractures, including reverse oblique and transverse fracture patterns, are classified as A3.Citation9 The current approach for fractures involving the intertrochanteric region is to initially perform an anatomical reduction and then stabilize the fracture with rigid fixation.Citation10 Cephalomedullary nails, such as the gamma nail and proximal femoral nail (PFN), are the preferred implants in proximal extracapsular femoral fractures (AO/OTA 31-A).Citation2,Citation8,Citation10,Citation11 Compared with other implants, cephalomedullary nails provide biomechanical advantages because of their shorter lever arms and decreased deformity forces.Citation2,Citation7,Citation8,Citation10 They are the acceptable and preferred implants in the treatment of proximal femoral fractures, specifically because they allow for a closed reduction procedure.Citation2,Citation8,Citation11–Citation13 In addition, intramedullary fixation is associated with decreased soft tissue trauma, decreased blood loss, and lower rates of infection and wound complications.Citation2,Citation8,Citation11,Citation12 A meta-analysis by Ma et alCitation14 reported less blood loss and shorter length of hospital stay with proximal femoral nail antirotation (PFNA). Also, they found no significant difference in the rate of fixation failure between the gamma nail and PFNA or dynamic hip screw (DHS). Similarly, Shen et alCitation15 reported less blood loss and fewer complications in the PFNA group when compared to DHS group.
On the other hand, various complications may develop in the intraoperative and postoperative periods with the use of PFN.Citation1,Citation3,Citation8,Citation10,Citation12,Citation16–Citation20 The potential late complications may include neck screw cutouts, nonunion, Z-effect, reversed Z-effect, secondary varus deformity, thigh pain due to iliotibial tract irritation, and fracture development near the distal aspect of the nail.
This study evaluates the clinical results, radiographic findings, and associated complications in patients who underwent osteosynthesis with PFN for fracture of the proximal femur.
Materials and methods
Between January 2009 and July 2013, 202 patients were operated with PFN for trochanteric fracture of the proximal femur. Among them, 152 patients (152 hips) who were followed up for at least 6 months were included in the study. According to the AO/OTA classification criteria, A1, A2, and A3 type fractures were found in 24 (15.8%), 107 (70.4%), and 21 (13.8%) patients, respectively.
The mean time from hip fracture to osteosynthesis with PFN was 3.75 (range 1–13) days, and titanium alloy PROFIN PFN® nails (TST Medical Devices, Istanbul, Turkey) were used. Surgery was performed under spinal anesthesia using fluoroscopy-guided closed reduction on a traction table. All patients were ambulated on the first day after surgery with partial weight-bearing according to their pain tolerance levels. The mean duration of hospital stay was 6.05 (range 1–24) days. Postoperative reduction was assessed using the Baumgaertner et al’s scale.Citation21 Functional results were evaluated using the Salvati and Wilson assessment score (SWS)Citation22 (). After the follow-up period, clinical and radiographic results were evaluated and the complications were assessed. Intraoperative complications were excluded. Late complications, including implant cutout, Z-effect, reverse Z-effect, calcification of the tip of the greater trochanter, femoral neck shortening, nonunion, malunion, cortical thickening at the distal locking region, broken locking screw, broken PFN, and diaphyseal femoral fractures, were considered during radiographic assessment. The relationship between the complications and SWS score, age, sex, fracture type, reduction quality, and time from fracture to surgery was evaluated. This study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki and informed written consent was obtained from all the patients. The protocol was reviewed and approved by the Institutional Review Board of ˙Izmir Bozyaka Training and Research Hospital, ˙Izmir, Turkey (No. 16.03.2011-34).
Table 1 Salvati and Wilson assessment score
Statistical analysis
Statistical analysis was performed using PASW version 18.0 software (SPSS Inc., Chicago, IL, USA). Frequency analysis was performed for categorical variables. The data were expressed in numbers and percentages. The Pearson chi-square test was used to compare categorical variables. A P-value of <0.05 was considered statistically significant.
Results
Of the patients, 85 (55.9%) were females and 67 (44.1%) were males. The mean age was 76 (range 21–93) years, and the mean follow-up duration was 23.6 (range 7–49) months. Seventy-nine patients (51.9%) had left hip fractures, and 73 (48.1%) had right hip fractures. The mechanism of fracture was a simple fall in 146 patients (96.1%), a car accident in four patients (2.6%), and a motorcycle accident in two patients (1.3%). The mean duration of the operation was 63.35 (range 50–85) minutes. The demographic characteristics of the patients are shown in .
Table 2 Demographic characteristics of patients
The initial postoperative radiographic assessment revealed that reduction was poor in one patient (0.6%), acceptable in 16 patients (10.5%), and good in 135 patients (88.9%). The SWS scores were excellent, good, moderate, and poor in 91 (59.8%), 45 (29.6%), 15 (9.8%), and one (0.6%) patients, respectively. No pulmonary embolism or deep vein thrombosis, or no urinary tract infection or deep surgical site infection were observed in our study. Superficial incision site infection was observed in two (1.3%) patients. Infection resolved with antibiotic therapy and wound care.
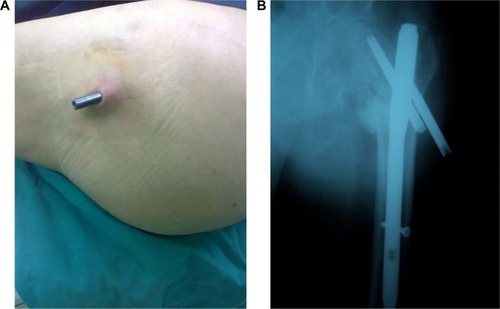
Late postoperative complications were seen in 27 patients (17.7%) (). Fourteen patients (9.2%) underwent a revision procedure for mechanical complications (). Of these, three (1.9%) underwent a revision procedure for nonunion. One patient (0.6%) underwent a 95° dynamic condylar screw, whereas the remaining two patients (1.3%) underwent a partial hip arthroplasty. In addition, one patient (0.6%) with implant cutout underwent a partial hip arthroplasty, and two patients (1.3%) with implant cutout underwent a total hip arthroplasty.
Table 3 Late complications and surgical procedures
Figure 1 (A and B) Images of lateral migration of PFN head screws and cutout.
In one patient (0.6%) with reverse Z-effect, one of the femoral head screws was removed without any additional surgical intervention. In another patient (0.6%), the nail was removed with Z-effect and secondary varus deformity at 6 months following surgery without any additional surgical intervention.
Femoral head screws were removed in four patients (2.6%). They were removed in two patients (1.3%) with Z-effect and secondary varus deformity – one patient (0.6%) had implant cutout and the other patient (0.6%) had reverse Z-effect and secondary varus deformity. Among these four patients, two (1.3%) underwent partial hip arthroplasty.
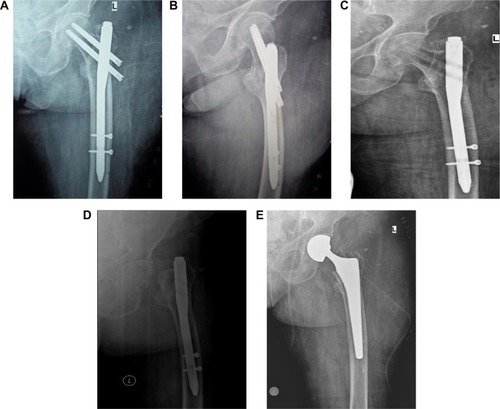
A total of seven patients (4.6%) had thigh pain due to the nail-point effects. Femoral head screws were shortened in one patient (0.6%) because they caused trochanteric bursitis due to nail-point effect. The nail was removed in another patient (0.6%) because of nail-point-effect-related femoral fractures, and the patient underwent partial hip arthroplasty ().
Figure 2 (A–E) Femoral head fracture due to the lateral thigh pain in a patient in whom PFN screws were removed undergoing partial hip arthroplasty.
The SWS score was not significantly associated with the fracture type, age, sex, and time from fracture to surgery (P=0.051, P=0.628, P=0.608, and P=0.462, respectively). A postoperative SWS score of very good correlated with an excellent reduction in the early postoperative stage. We found a significant association between SWS score and reduction quality (χ2=35.446, P=0.000).
Furthermore, the patients with mechanical failure had a lower SWS score (χ2=68.538, P=0.000). On the basis of radiographic assessment, these patients also were found to have a poor reduction in the early stage (χ2=39.261, P=0.000). Mechanical failure was not significantly associated with the fracture type and age (P=0.597 and P=0.531).
In addition, the necessity of a revision procedure was not significantly associated with the fracture type and age (P=0.478 and P=0.407, respectively). Early postoperative imaging studies revealed a poor reduction in patients who underwent revision procedures (χ2=11.823, P=0.003). Revision procedures were significantly associated with mechanical failure (χ2=56.699, P=0.000).
Discussion
The complication rate of PFN and the related necessity of a revision procedure varies from 3% to 28% in the literature.Citation2,Citation3,Citation7,Citation8,Citation10,Citation11,Citation16–Citation20,Citation23–Citation25 Consistent with the published data, the revision rate related to PFN osteosynthesis was not high in our study (9.2%; n=14/152).
In a series of 191 fractures, Simmermacher et alCitation20 reported an overall technical failure rate of 4.6%. In another study including 178 patients, Appelt et alCitation1 reported a complication rate of 15.2% (n=27). In a case series including 47 peritrochanteric fractures, Fogagnolo et alCitation2 found mechanical failures in 23.4% patients (n=11). In another case series including 80 patients, Akan et alCitation13 observed technical complications in 10% patients (n=8). In a prospective study including 55 patients treated with PFN, Boldin et alCitation24 reported a complication rate of 21.8% patients (n=12). Similar to the previous findings, our study showed that the rate of late complications following surgery was 17.7% (27 patients).
In a study including 295 patients, Domingo et alCitation11 reported that ten patients (3.3%) who required a revision procedure had AO type 2 and type 3 fractures. Similarly, Simmermacher et alCitation20 concluded that PFN-related complications were mostly associated with AO type 2 fractures. In the present study, among 16 patients with moderate or poor SWS scores, 13 and three had AO type 2 and type 3 fractures, respectively. Of the patients who underwent revision, one patient had type A1 fractures, eight patients had type A2 fractures, and four patients had type A3 fractures.
In addition, PFN-related secondary varus deformities may occur in 0.8%–8.6% patients.Citation8,Citation10,Citation11,Citation16,Citation19 Consistent with the published literature, our study found PFN-related secondary varus deformities in 8.5% of the patients (13 patients). According to the AO classification, among these 13 patients, nine patients had type A2 and four patients had type A3 fractures.
Furthermore, malpositioning of screws or placement of screws with an inappropriate size may lead to cutout from the femoral head.Citation3,Citation10,Citation11,Citation16,Citation17 Several studies have reported a cutout rate of 2%–8%.Citation3,Citation7,Citation8,Citation11,Citation13–Citation18,Citation24 We observed a cut-out complication in four patients (2.6%). Two of them underwent partial hip arthroplasty, whereas the remaining two underwent total hip arthroplasty.
The Z-effect phenomenon is a potential complication of double lag screw intramedullary nail designs,Citation25–Citation27 and the term was first introduced by Werner-Tutschku et alCitation26 in five (7.1%) of 70 patients. The Z-effect and reverse Z-effect phenomena were reported in five patients (11.1%) and in one patient (2.2%), respectively, in the Tyllianakis et al study;Citation8 in one patient (1.2%) and in three patients (3.7%), respectively, in the Akan et al study;Citation13 in three patients (5.4%) and in two patients (3.6%), respectively, in the Boldin et al study;Citation24 and in four patients (3.3%) and in one patient (0.8%), respectively, in the Papasimos et al study.Citation25 Similar to the former studies, we observed Z-effect and reverse Z-effect in three (1.9%) and two patients (1.3%), respectively. One of the patients underwent a partial hip arthroplasty, whereas femoral head screws were removed in three patients. PFN was removed without any additional surgical intervention in another patient.
Calcification of the tip of the greater trochanter is a late radiographic complication with PFN insertion. A total of 13 of 295 patients suffered from this complication in the Domingo et al study,Citation11 whereas Herrera et alCitation19 reported six patients with calcification of the tip of the greater trochanter. In another study, Uzun et alCitation16 found calcification of the tip of the greater trochanter in two patients. Menezes et alCitation10 reported heterotopic ossification in nine out of 129 patients. Unlike these findings, none of the patients showed radiographic evidence of calcification in our study.
In addition, seven patients (4.6%) presented with thigh pain due to the nail-point effects. As a late complication, thigh pain was reported to be 2.7% (eight out of 295) and 3.2% (four out of 125) by Domingo et alCitation11 and Herrera et al,Citation19 respectively.
The use of a double lag screw intramedullary nail design and cortical hypertrophy of the distal locking screw region due to thick distal nails can be associated with thigh pain during the recovery period.Citation11,Citation12,Citation28 In the present study, two distal locking screws were used in 140 patients (92.2%), whereas a single distal locking screw was used in 12 patients (7.8%). The distal locking screw was broken in four patients (2.6%).
As a result, PFN is a relatively easy-to-use and effective device in the treatment of unstable trochanteric femoral fractures.Citation2,Citation8,Citation11,Citation12,Citation29 It enables early postoperative ambulation with a biomechanically stable structure.Citation2,Citation11 In addition to using an appropriate implant, adequate reduction quality, proper implant insertion, and the experience of the surgeon play a key role in the successful osteosynthesis for trochanteric fractures.Citation1,Citation8,Citation29–Citation31 Windolf et alCitation29 reported that the major causes of poor outcomes included poor fracture reduction and the use of an inappropriate screw. Osteosynthesis with PFN is a safe method for simple trochanteric fractures with excellent bone quality; however, PFN may not be the preferred method of fixation for complex fractures in patients with poor bone quality.Citation1 In our study, poor reduction was significantly associated with increased mechanical failure and revision rates. However, the fracture type was not significantly associated with mechanical failure.
This study has some limitations. First, there is no control group, including an alternative treatment modality other than PFN. Second, we were unable to investigate the effects of comorbidities such as cognitive status, health status, and activity level, all of which may likely affect the outcomes. The preoperative comorbid factors can have influence on the development of mechanical complications. Third, PFN implants from diverse manufacturers can also have influence on the development of mechanical failure.
In conclusion, the quality of fracture reduction is an important factor that affects the revision rate and SWS score in patients with mechanical complications after PFN was used for trochanteric fractures.
Disclosure
The authors report no conflicts of interest in this work.
References
- AppeltASuhmNBaierMMeederPJComplications after intramedullary stabilization of proximal femur fractures: a retrospective analysis of 178 patientsEur J Trauma Emerg Surg2007333262267
- FogagnoloFKfuriMJrPaccolaCAIntramedullary fixation of pertrochanteric hip fractures with the short AOASIF proximal femoral nailArch Orthop Trauma Surg20041241313713680275
- SchipperIBSteyerbergEWCasteleinRMTreatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral nailJ Bone Joint Surg Br2004861869414765872
- KorkmazMFErdemMNDisliZSelcukEBKarakaplanMGogusAOutcomes of trochanteric femoral fractures treated with proximal femoral nail: an analysis of 100 consecutive casesClin Interv Aging20143956957424729697
- WhiteBLFisherWDLaurinCARate of mortality for elderly patients after fracture of the hip in the1980’sJ Bone Joint Surg Am1987699133513403440792
- ZuckermanJDSkovronMLKovalKJAharonoffGFrankelVHPostoperative complications and mortality associated with operative delay in older patients who have a fracture of the hipJ Bone Joint Surg Am19957710155115567593064
- BananHAl-SabtiAJimuliaTHartAJThe treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN) – our first 60 casesInjury200233540140512095719
- TyllianakisMPanagopoulosAPapadopoulosAPapasimosSMousafirisKTreatment of extracapsular hip fractures with the proximal femoral nail (PFN): long term results in 45 patientsActa Orthop Belg200470544445415587033
- MüllerMENazarianSKochPSchatzkerJThe Comprehensive Classification of Fractures of Long BonesBerlin, GermanySpringer-Verlag1990
- MenezesDFGamulinANoesbergerBIs the proximal femoral nail a suitable implant for treatment of all trochanteric fractures?Clin Orthop Relat Res200543922122716205163
- DomingoLJCeciliaDHerreraAResinesCTrochanteric fractures treated with a proximal femoral nailInt Orthop200125529830111794263
- OzkanKUnayKDemircayCCakirMEcevizEDistal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fracturesInt Orthop20093351397140018956183
- AkanKCiftHOzkanKEcevizETasyikanLErenAEffect of osteoporosis on clinical outcomes in intertrochanteric hip fractures treated with a proximal femoral nailJ Int Med Res201139385786521819718
- MaKLWangXLuanFJProximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysisOrthop Traumatol Surg Res2014100885986625453927
- ShenLZhangYShenYCuiZAntirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studiesOrthop Traumatol Surg Res201399437738323707739
- UzunMErtürerEOztürkIAkmanSSeçkinFOzçelikIBLong-term radiographic complications following treatment of unstable intertrochanteric femoral fractures with the proximal femoral nail and effects on functional resultsActa Orthop Traumatol Turc200943645746320134211
- ErturerRESönmezMMSariSSeckinMFKaraAOzturkIIntramedullary osteosynthesis of instable intertrochanteric femur fractures with Profin® nail in elderly patientsActa Orthop Traumatol Turc201246210711222491435
- SaudanMLübbekeASadowskiCRiandNSternRHoffmeyerPPertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of patients comparing the dynamic hip screw and proximal femoral nailJ Orthop Trauma200216638639312142826
- HerreraADomingoLJCalvoAMartínezACuencaJA comparative study of trochanteric fractures treated with the Gamma nail or the proximal femoral nailInt Orthop200226636536912466870
- SimmermacherRKBoschAMVan der WerkenCThe AO/ASIF-proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fracturesInjury199930532733210505125
- BaumgaertnerMRCurtinSLLindskogDMIntramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fracturesClin Orthop Relat Res199834887949553538
- SalvatiEAWilsonPDLong term results of femoral-head replacementJ Bone Joint Surg19735535165244703204
- Al-yassariGLangstaffRJJonesJWAl-LamiMThe AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fractureInjury200233539539912095718
- BoldinCSeibertFJFankhauserFPeichaGGrechenigWSzyszkowitzRThe proximal femoral nail (PFN)-a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 monthsActa Orthop Scand2003741535812635794
- PapasimosSKoutsojannisCMPanagopoulosAMegasPLambirisEA randomised comparison of AMBI, TGN and PFN for treatment of unstable trochanteric fracturesArch Orthop Trauma Surg2005125746246816059696
- Werner-TutschkuWLajtaiGSchmiedhuberGLangTPirklCOrthnerEIntra- and perioperative complications in the stabilization of per- and subtrochanteric femoral fractures by means of PFNUnfallchirurg20021051088188512376894
- StraussEJKummerFJKovalKJEgolKAThe “Z-effect” phenomenon defined: a laboratory studyJ Orthop Res200725121568157317592624
- HardyDCDescampsPYKrallisPUse of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patientsJ Bone Joint Surg Am19988056186309611022
- WindolfJHollanderDAHakimiMLinhartWPitfalls and complications in the use of the proximal femoral nailLangenbecks Arch Surg20053901596515088148
- BaumgaertnerMRCurtinSLLindskogDMKeggiJMThe value of the tip-apex distance in predicting failure of peritrochanteric fractures of the hipJ Bone Joint Surg Am1995777105810647608228
- BiberRGrüningerSSinglerKSieberCCBailHJIs proximal femoral nailing a good procedure for teaching in orthogeriatrics?Arch Orthop Trauma Surg20121327997100222467120
