Abstract
Purpose
The aim of this study was to compare the results of phacoemulsification through a small pupil using minimal iris manipulation versus phacoemulsification through a well-dilated pupil.
Methods
This prospective randomized control (comparative) study comprised 78 patients (group I) with a maximally dilated pupil size of ≤4.00 mm and 45 patients (group II) with dilated pupil size of ≥7.00 mm. In group I patients, only viscodilation and minimal push-and-pull iris stretching with two collar-button iris-retractor hooks were utilized without iris manipulation. Phacoemulsification was performed by two senior surgeons and the technique used consisted of either stop and chop or quick chop, infusion/aspiration of lens cortex, capsular bag refill with ocular viscoelastic devices, and implantation of an acrylic foldable intraocular lens. Patients were examined on the first day and 1 month postoperatively.
Results
Forty-six eyes of group I patients had pseudoexfoliation syndrome, eleven eyes had previous glaucoma surgery, 14 eyes had angle-closure or open-angle glaucoma, and seven eyes had posterior synechiae with iritis. In group I patients, the mean pupil size measured under an operating microscope was 3.2 mm preoperatively, 4.3 mm after viscoelastic and mechanical pupil dilation, and 4.1 mm at the end of a surgical procedure. Rupture of the zonular fibers occurred in six patients of group I and the intraocular lens was implanted in the sulcus. Small iris-sphincter rupture and small hemorrhages occurred in four eyes during pupillary manipulation, but they were not evident at the end of the surgery. In group II patients, no intraoperative complications occurred. Signs of significant corneal edema and iritis were observed more frequently in group I eyes (26 eyes and 20 eyes, respectively) on the first postoperative day in comparison with group II eyes (ten eyes and six eyes, respectively). Intraocular pressure was <20 mmHg in all eyes of both groups. One month postoperatively, the pupil was round and reactive to light, the anterior chamber was quiet, and the cornea was clear in all eyes. The best-corrected visual acuity on Snellen chart was 20/40 (Monoyer’s scale) or better in both groups.
Conclusion
Phacoemulsification through a small pupil using minimal iris manipulation can be safe and exhibits the same results as those obtained with phacoemulsification through normal pupils.
Introduction
Cataract is a common cause of visual impairment in the elderly and represents the commonest etiology of blindness worldwide.Citation1 Clear corneal cataract surgery has become a common practice since eye surgeons commenced using topical anesthesia, phacoemulsification, and small foldable intraocular lenses (IOLs) during the past two decades.Citation2 Operating through small corneal incisions (<3.0 mm) requires high technical skills in order to perform a safe and successful cataract operation without increasing the risk of corneal, iris, or capsule damage. Some patients who need cataract extraction have eyes with small pupils, which is attributed to aging, pseudoexfoliation, diabetes, uveitis, glaucoma, installation of miotic agents, trauma, or previous intraocular surgical procedures.
A small pupil can hinder visualization and create significant difficulties in handling intraocular instruments, leading to inadequate or incomplete capsulorhexis. There is also a higher risk of complications during phacoemulsification through a small pupil, such as intraocular bleeding, iris sphincter tear and/or emulsification, rupture of posterior capsule, vitreous loss,Citation3,Citation4 and endothelial cell loss.Citation5 Moreover, intraoperative miosis constitutes the foremost risk factor that influences conversion from phacoemulsification to extracapsular cataract extraction. The aforementioned possible intraoperative difficulties and complications can cause photophobia, permanent ocular ache, and pupillary irregularities and dysfunction.
Several methods to mechanically stretch small pupils have been described. These comprise the use of a blade, needle, or scissors to create several iris sphincter tears.Citation6 Alternatively, iris hooks can be used to retract the iris through corneal stab incisions,Citation7 or mechanical stretching devices can be inserted to pull the iris sphincter.Citation7–Citation9 All these awkward methods necessitate sophisticated instruments and demand difficult intraocular maneuvers, which can potentially incur postoperative bleeding, damage of iris sphincter function, and an abnormal pupil shape.
In order to avoid all the abovementioned undesirable effects in patients with small pupils, we compared the outcomes of phacoemulsification through a small pupil using minimal iris manipulation and through a normal pupil performed by experienced surgeons.
Patients and methods
This prospective randomized control study comprised 78 patients (group I) with a maximally dilated pupil size of ≤4.00 mm. Another 45 patients (group II) with dilated pupil size of ≥7.00 mm were involved in order to compare the results of phacoemulsification procedure in the two groups. All cataract patients with significant nuclear sclerotic (NS) cataract (NS++ or more) and reduced visual acuity (VA; best-corrected visual acuity [BCVA] <4/10 on Snellen chart) had a comprehensive preoperative examination including ultrasonic biometry (by IOL master), corneal topography, and measurement of the pupil diameter with calipers at the slit lamp. All operations were performed in the first eye clinic of the University of Athens in “G. Gennimatas” hospital by two experienced surgeons between November 2012 and April 2014. Written informed consent was obtained from all patients prior to surgery. The study was approved by the ethics committee of G.Gennimatas Hospital and followed the principles of the Declaration of Helsinki.
Inclusion criteria were as follows: pupillary size of ≤4 mm in group I patients and ≥7 mm in group II patients. Subjects involved in the study had NS cataracts >+2. Exclusion criteria were as follows: patients with VA >5/10 on Snellen chart (Monoyer’s scale), patients with <18 years of age, any corneal pathology (eg, Fuchs’ corneal dystrophy and keratoconus), retinal pathology (eg, age macular degeneration, epiretinal membrane, and diabetic retinopathy), and traumatic cataracts.
Preoperatively, one eyedrop of 1% tropicamide (Tropixal; Demo SA Pharmaceutical Industry, Kryoneri, Greece), 5% phenylephrine (Phenylephrine; Cooper Pharmaceuticals SA, Athina, Greece), and 1% cyclopentolate (Cyclogyl; Alcon Laboratories, Inc., Fort Worth, TX, USA) was instilled four times at 30-minute intervals 2 hours before surgery. Topical povidone–iodine 5% (Betadine; Lavipharm, Peania Attica, Greece) was instilled, the patient’s eye was draped with a sterile adhesive disposable drape and an eyelid speculum was inserted. All procedures were performed using topical anesthesia.Citation10,Citation11 In addition, 0.5% tetracaine hydrochloride (Tetracaine; Cooper Pharmaceutical SA) drops were instilled.
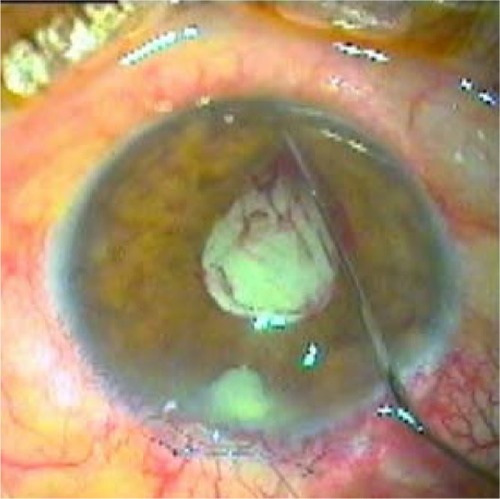
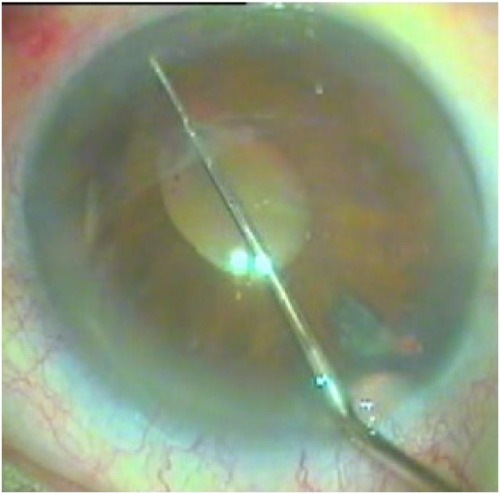
A 2.8 mm clear corneal, self-sealing incision was made at the 11 o’clock position, and the anterior chamber was filled with viscoelastic agent (Viscoat; Alcon Laboratories, Inc.). This injection in group I patients was performed in the pupillary plane in an attempt to viscodilate the small pupil.Citation12 Then, a side-port incision was made at the 1 o’clock position. In group I patients, an extra second side-port incision was performed at the 8 o’clock position. Two collar-button iris-retractor hooks were used to perform minimal push-and-pull iris stretching, first horizontally and then vertically ( and ). In each of the 78 eyes in group I, pupil size was measured horizontally before the initiation of surgery, after the injection of viscoelastic material and mechanical pupil dilation, and postoperatively. Measurements were made to the nearest half-millimeter with calipers under the same operating microscope.
After pupil dilatation, capsulorhexis, and hydrodissection, phacoemulsification was performed by means of standard stop and chop or quick chop techniques with Infiniti (Alcon Laboratories, Inc.) machine. Either of the phacoemulsification technique (stop and chop and quick chop) has quite the same value in minimal iris manipulation. Balanced salt solution (BSS) containing 0.5 mL of 1:1,000 preservative-free adrenaline was used for the irrigation solution in all cases. After phacoemulsification was completed, all cases had an infusion/aspiration of the lens cortex, capsular bag refill with ocular viscoelastic devices (OVD; Viscoat), and implantation of an acrylic foldable IOL in the bag except six cases, where the IOL was implanted in the sulcus due to intraoperative complication. The OVD was then aspirated and the anterior chamber was reformed with BSS. The corneal wound and side port were hydrated with BSS. Pupil size at the end of the surgery was recorded. Postoperative medication was composed of guttae 0.1% dexamethasone (Maxidex; Alcon Laboratories, Inc.) and 1% guttae azidamfenicol (Thilocof; Pharmex SA, Athens, Greece) every 6 hours, for 1 month.
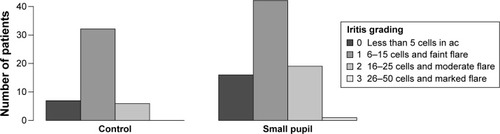
Patients were reviewed on the first and 30th postoperative days. Postoperatively, we recorded patients’ VA, intraocular pressure (IOP), corneal edema, and iritis/anterior chamber flare. Corneal edema was gradedCitation13,Citation14 as grade 0, if there was no edema, grade 1, if it was none to minimal, and significant if it was grades 2–4. Grade 2 edema was mild to moderate (visible iris details), grade 3 was moderate to severe (obscuring iris details), and grade 4 was marked (obscuring pupil). Iritis/anterior chamber flare was gradedCitation15 as grade 0, if there were <5 cells in the anterior chamber and no flare, grade 1+ if there were 6–15 cells and faint flare, and significant if there were grades 2+ to 4+. In grade 2+, there were 16–25 cells and moderate flare (iris and lens details clear), in grade 3+, there were 26–50 cells and marked flare (iris and lens details hazy), and in grade 4+, there were >50 cells and intense flare (fibrin or plastic aqueous). All findings were recorded by the operating surgeons. The final VA was evaluated at the second visit.
Statistical analysis
Parametric statistical tests depend on the assumption that data are sampled from a normal (Gaussian) distribution. Testing composite normality was performed using the Shapiro–Wilk W-test. Mean comparisons of parametric continuous data (ie, the ages of patients and controls) were performed using Student’s t-test. Under violation of normality, which was the case both for the VA and the IOP data, median comparisons were performed with Wilcoxon’s rank-sum test and the Kruskal–Wallis test; the latter was performed when the number of groups were >2. For the paired scenario, the sign-rank test was utilized (comparisons of VA and IOP before and after). Associations between discrete attributes were examined using the Pearson’s χ2 test of independence. Correlation analysis for nonparametric data was performed utilizing Kendall’s τ rank correlation, and in each case, a line-to-fit data (in a least squares sense) was computed. In all statistical tests, the significance level was defined as P<0.05. Statistical analysis was implemented in R Version 3.1.0 (The R Project for Statistical Computing, http://www.r-project.org/), with the assistance of R Studio.
Results
A total of 123 eyes of 123 patients were included in the study. There were no statistically significant differences in age between the two study groups (P>0.05). In 46 eyes (59%) of group I, the cause of small pupil was pseudoexfoliation syndrome. Eleven eyes had previous glaucoma surgery, 14 eyes had angle-closure or open-angle glaucoma, and seven eyes had posterior synechiae with iritis ().
Table 1 Patient demographics
In group I patients, the mean pupil size measured under an operating microscope was 3.2 mm preoperatively, 4.3 mm after viscoelastic and mechanical pupil dilation, and 4.1 mm after the end of surgical procedure (). On the other hand, in group II patients, the mean pupil size measured under an operating microscope was 7.2 mm after the installation of mydriatic drops.
Table 2 Group I mean pupil size
The most significant intraoperative complication that occurred was the rupture of the zonular fibers in six patients of group I, and subsequently the IOL was implanted in the sulcus (no statistical significance in comparison with group II patients, where no complications occurred [P=0.06]). Small iris sphincter ruptures and self-limited small hemorrhages ( and ) were evident in four eyes of group I patients during pupillary manipulation, but they were not evident after the end of the procedure.
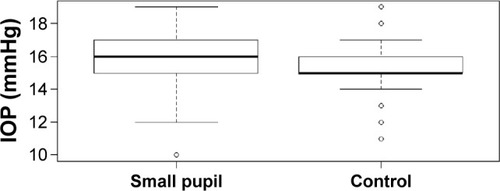
All 123 eyes had round and symmetric pupils at the first postoperative day. Significant corneal edema and iritis (grades 2–3) were observed more frequently in group I eyes rather than group II (). In 26 eyes of group I patients, there was corneal edema of grades 2–3 and in 20 eyes of the same group, there was iritis/anterior chamber flare of grades 2–3. On the other hand, in ten eyes of group II patients, there was corneal edema of grades 2–3 and in six eyes of the same group, there was iritis/anterior chamber flares of grade 2. IOP was <20 mmHg in all eyes studied.
Table 3 Corneal edema and iritis/anterior chamber flare at the first postoperative day and BCVA on the 30th postoperative day
Figure 3 Comparison of postoperative corneal edema between the two groups, P=0.92.
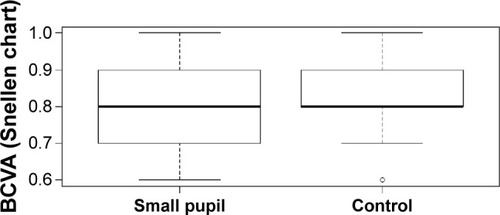
One month after surgery, the pupils were round and reactive to light; the anterior chambers were quiet; and the corneas were clear in all studied eyes. The BCVA on Snellen chart was 20/40 (Monoyer’s scale) or better and there were no statistically significant differences between the two groups (–).
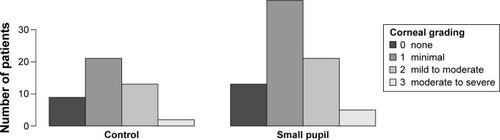
Figure 4 Comparison of postoperative iritis between the two groups, P=0.25.
Abbreviation: ac, anterior chamber.
Discussion
In our time, phacoemulsification is a technically high-demanding operation that requires the implementation of accurately executed surgical steps, from corneal incision to IOL implantation. Sufficient pupillary dilation before proceeding to cataract extraction is extremely important. Some patients with cataract requiring phacoemulsification do not have well-dilated eyes despite instilling topical mydriatic agents repeatedly. The main causes include iris sphincter sclerosis due to aging, uveitis with synechiae, diabetes, angle-closure glaucoma with chronic miotic therapy, chronic open-angle glaucoma, pseudoexfoliation, previous intraocular surgery, or trauma.
Patients presenting with a small pupil at the time of cataract surgery can cause a major clinical dilemma, since the surgeon must decide whether to insert pupillary dilating devices (eg, iris hooks or iris rings) in order to perform an uncomplicated operation or not. In some cases, not dilating the pupil mechanically will suffice. However, performing a cataract surgery through a poorly dilated pupil can be challenging, since visualization of the cataract can be compromised and can lead to insufficient capsulorhexis. However, even if a satisfactory capsulorhexis is made, attempting to operate through an inadequately dilated pupil can result in iris damage, intraocular bleeding, ruptured posterior capsule, vitreous loss, and dropped nucleus.
The vast majority of cataract surgeons usually decide to mechanically dilate the pupil during surgery, if it is still miotic after installation of dilating eyedrops. Various techniques and instruments can be implemented for enlarging a poorly dilating pupil. The most common devices and techniques are the iris-retractor hooks, the poly(methyl methacrylate) (PMMA) pupil dilator rings,Citation16 the Beehler pupil dilator, and the bimanual stretching technique.Citation7 The first three methods produce a mean pupil size of 5.9 mm, which remains constant throughout the surgery especially with PMMA pupil-dilator rings preventing the iris from being aspirated into the aspiration port, thus acting as a barrier between the iris and the phacoemulsification tip. Despite the fact that these methods enlarge the pupil adequately, some are expensive (especially PMMA pupil-dilator rings), entail extra instrumentation and surgical skills, are time-consuming (positioning the iris-retractor hooks takes ~5 minutes), and are not always offered in some parts of the world. Additionally, mechanical dilation of the pupil might permanently damage the iris sphincter causing a large atonic pupil.Citation17
Any surgical technique to dilate a miotic pupil must be safe, readily available to all surgeons, and minimize intra-/postoperative complications. A sufficient pupil size for uncomplicated phacoemulsification depends on the surgeon’s expertise, the nature of cataract, and the anatomy of the anterior chamber. Any techniques used for intraoperative mechanical dilatation of the pupil must be safe, quick, and cost-effective. In our study, all patients with small pupils were operated on by two senior surgeons who used simple stretching methods (bimanual stretching and viscodilation) to address these factors. A limitation of our study is the fact that Cohen’s kappa was not used to standardize the capability between the two surgeons. We compared the results of phacoemulsification in patients with small versus well-dilated pupils, and there were no statistically significant differences regarding intra-/postoperative complications. It is worth mentioning that bimanual stretching with viscodilation can achieve good pupil size, but the size is usually smaller than that obtained with the other devices mentioned. Bimanual stretching with viscodilation can be performed in less than a minute and is less time-consuming than devices used to dilate the pupil but can cause small ruptures of the sphincter. However, the esthetic and functional effects were not significant at 30 days, and occurred in only four patients in our study. In addition, it is well-known that excessive iris manipulation leads to more pronounced postoperative inflammatory reaction. The early inflammatory reaction and corneal edema observed in our study were probably due to iris manipulation, but both subsided within a short period of time (ie, 30 days). In our study, all patients had NS++ or more cataracts and above. Thus, no statistical analysis based on cataract density was feasible. It would be useful for future studies to compare the postoperative findings related to cataract density using the Lens Opacities Classification System III.
Conclusion
Phacoemulsification is safer, more efficient, and significantly faster when compared with conventional cataract operations, resulting in extremely good visual outcomes. Operating through a small corneal incision requires high surgical expertise as well as a clear view of the intraocular anatomical structures and the surgical instruments. A poorly dilated pupil can impede visualization, making phacoemulsification more complex and can potentially cause more complications leading to poorer visual outcomes. The adequate pupil size for safe completion of phacoemulsification depends on many factors: one of the most important factors seems to be the surgeon’s level of experience. Phacoemulsification through a small pupil using minimal iris manipulation may be safe and may exhibit the same results with clear cornea cataract surgery through normal pupils.
Acknowledgments
The authors would like to sincerely thank Dr John Lakoumentas, PhD (Department of Medical Physics, School of Medicine, University of Patras, Greece) for his invaluable help in the statistical analysis of the study’s data.
Disclosure
The authors report no conflicts of interest in this work.
References
- FosterAJohnsonGJMagnitude and causes of blindness in the developing worldInt Ophthalmol1990141351402188914
- KershnerRMClear corneal cataract surgery and the correction of myopia, hyperopia, and astigmatismOphthalmology19971043813899082260
- MasketSCataract surgery complicated by the miotic pupilBurattoLOsherRHMasketSCataract Surgery in Complicated CasesThorofare, NJSlack Inc2000132135
- GuzekJPHolmMCotterJBRisk factors for intraoperative complications in 1000 extracapsular cataract casesOphthalmology1987944614663601359
- HayashiKHayashiHNakaoFHyashiFRisk factors for corneal endothelial injury during phacoemulsificationJ Cataract Refract Surg199622107910848915805
- FineIHPupilloplasty for small pupil phacoemulsificationJ Cataract Refract Surg1994201921968201574
- AkmanAYilmazGOtoSAkovaYAComparison of various pupil dilatation methods for phacoemulsification in eyes with a small pupil secondary to pseudoexfoliationOphthalmology20041111693169815350324
- MalyuginBSmall pupil phaco surgery: a new techniqueAnn Ophthalmol200739185193
- KershnerRMManagement of the small pupil for clear corneal cataract surgeryJ Cataract Refract Surg2002281826183112388036
- O’BrienPDFitzpatrickPPowerWPatient pain during stretching of small pupils in phacoemulsification performed using topical anesthesiaJ Cataract Refract Surg2005311760176316246780
- KershnerRMTopical anesthesia for small incision self-sealing cataract surgery; a prospective evaluation of the first 100 patientsJ Cataract Refract Surg1993192902928487176
- Bissen-MiyajimaHOphthalmic viscosurgical devicesCurr Opin Ophthalmol200819505418090898
- HughesWFJrAlkali injuries of the eye. I. Review of the literature and summary of present knowledgeArch Ophthalmol194635423449
- PfisterRRPatersonCKoskiJThe pathophysiology and treatment of the alkali burned eyeSouth Med J1982754174227041279
- JabsDANussenblattRBRosenbaumJTStandardization of uveitis nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International WorkshopAm J Ophthalmol200514050951616196117
- SturmerJScherreMLanselNMechanical dilatation of the pupil in phacoemulsification surgery: first experiences with the 6.25 mm Malyugin-ringKlin Monbl Augenheilkd201222936536822496005
- VasavadaASinghRPhacoemulsification in eyes with a small pupilJ Cataract Refract Surg2000261210121811008050