Abstract
Population aging is unprecedented, without parallel in the history of humanity. As type 2 diabetes mellitus is predominantly more prevalent in aging populations, this creates a major public health burden. Older adults with diabetes have the highest rates of major lower-extremity amputation, myocardial infarction, visual impairment, and end-stage renal disease of any age group. The aims of our study were to assess whether age is an independent factor for the occurrence of diabetic neuropathy (DN), and to evaluate the relationship between the presence and the severity of DN and the diabetes duration and blood glucose level. In this study, we enrolled 198 patients, previously diagnosed with type 2 diabetes mellitus. For all patients, we measured hemoglobin A1c (HbA1c), lipid profile, and body mass index and we assessed the presence and severity of DN using the evaluation of clinical signs and symptoms. Patients had a median age of 62 years, with a median of diabetes duration of 7 years; 55.1% of the patients were men and the average HbA1c in the cohort was 8.2%. The prevalence of DN according to Michigan Neuropathy Screening Instrument was 28.8%, being significantly and positively correlated with higher age (65 vs 59 years; P=0.001) and HbA1c (8.6% vs 8.0%; P=0.027). No significant correlations were observed between the severity of DN and diabetes duration, body mass index (31.9 vs 29.9 kg/m2), or the number of centimeters exceeding the normal waist circumference (25.2 vs 17.3 cm; P=0.003). In conclusion, age influences the presence of DN, independent on other risk factors. This influence persists even after adjusting for other, very important risk factors, like blood glucose level or diabetes duration.
Introduction
As a consequence of population’s demographical changes, we are witnessing an increase in the proportion of persons of 60 years or older in parallel with a decline in the proportion of the young, such that by 2050 it is expected that the proportion of elderly persons will have risen from 15% (which is today’s ratio) up to 25%.Citation1
This demographic shift will have a direct impact on the epidemiology of chronic, nontransmissible diseases, including type 2 diabetes mellitus (T2DM). Nowadays, the prevalence of T2DM is approximated at 382 million cases, being expected to affect 592 million people by 2035. As T2DM is predominantly more prevalent in aging population, this premise is creating a major public health burden.Citation1
More than 25% of the US population aged ≥65 years has diabetes,Citation2 and the aging of the overall population is a significant driver of the diabetes epidemic. Although the burden of diabetes is often described in terms of its impact on working-age adults, diabetes in older adults is linked to higher mortality, reduced functional status, and increased risk of institutionalization.Citation3 Older adults with diabetes are at substantial risk for both acute and chronic microvascular and cardiovascular complications of the disease. Diabetic neuropathies (DN) encompass a wide range of nerve abnormalities and are common, with prevalence rates reported between 5% and 100% depending on the diagnostic criteria.Citation4–Citation6 Distal symmetric polyneuropathy is the most common form of DN.Citation7 The duration and severity of hyperglycemia, presence of dyslipidemia, hypertension, and smoking are major risk factors for the development of diabetic polyneuropathy.Citation8
The aims of our study were to assess whether age is an independent factor for the occurrence of DN, and to evaluate the relationship between the presence and the severity of DN and the diabetes duration and blood glucose level.
Materials and methods
Study design and patients
In this cross-sectional, noninterventional study, we enrolled 198 patients, previously diagnosed with T2DM, attending scheduled visits at the outpatient facility of the Emergency Hospital Timisoara between May 1, 2013 and June 30, 2014. Patients were enrolled according to a consecutive population principle, after signing an informed consent form. Since this is a noninterventional, cross-sectional study, according to the local protocols, this had to be approved only by the local Ethics Committee. The Ethics Committee of the Emergency Hospital Timisoara granted the approval number 266/2012. The following were exclusion criteria in the study protocol: inability to provide informed consent, inability to provide accurate anamnestic medical history data, prior history of non-DN (ie, alcoholic neuropathies), major cardiovascular events (according to Hicks 2014 criteria) 3 months prior to screening, or any other condition which, in the investigators’ opinion, could lead to biases in the study results.
For all patients, we measured hemoglobin A1c (HbA1c), lipid profile, and body mass index (BMI) and we assessed the presence and severity of DN using the evaluation of clinical symptoms. Also, for all patients, we measured the waist circumference values; we considered normal for men <94 cm and for women <80 cm. The presence and severity of chronic kidney disease was diagnosed according to Kidney Disease: Improving Global Outcomes 2012 guidelines. Retinopathy diagnosis was established after performing a funduscopic examination by the same trained ophthalmologist, specialized in the diagnosis and treatment of diabetic eye complications.Citation9 Hypertension was defined as resting blood pressure >140 mmHg (systolic) and/or >90 mmHg (diastolic); autonomic neuropathy was assessed using the presence of orthostatic hypotension, defined as a fall in blood pressure in response to postural changes (>20 mmHg for systolic or >10 mmHg for diastolic blood pressure). Michigan Neuropathy Screening Instrument (MNSI) is a score instrument designed for diagnosis and severity evaluation of DN, which contains a patient’s symptoms questionnaire and clinical assessment tool. We considered positive for overt neuropathy the presence of one out of the following criteria: a global score ≥9.5, questionnaire score ≥7, or clinical score ≥2.5. A higher score is associated with more severe neuropathy.
Statistical analysis
Data were collected and analyzed using SPSS version 17 statistical software package (SPSS Inc., Chicago, IL, USA) and were presented as average ± standard deviation (numerical variables with Gaussian distribution), median, and interquartile range (numerical variables with nonparametric distributions), respectively percentage from the subgroup total and (number of individuals) for categorical variables. To assess the significance of the differences between groups, the Student’s t-test (means, Gaussian populations), Mann–Whitney U-test (medians, nonparametric populations), and chi-square test (proportions) were used. Continuous variables distributions were tested for normality using Shapiro–Wilk test, and for equality of variances using Levene’s test.
To evaluate the strength of the association between two continuous variables, we used Spearman’s correlation coefficient; the statistical significance of the correlation was evaluated using t-distribution test. The individual impact of several confounding factors on the variance of a continuous variable was assessed by building multivariate regression models or if the dependent variable was dichotomous by building multivariate logistic regressions. The predictors, in the final regression equations, were accepted according to a repeated backward-stepwise algorithm (inclusion criteria P<0.05, exclusion criteria P>0.10) in order to obtain the most appropriate theoretical model to fit the collected data. The quality of the model was described using the accuracy of the prediction by adjusted R2 (multivariate linear regression) and Nagelkerke’s R2 (logistic regression).
In this study, a P-value of 0.05 was considered the threshold for statistical significance.
Results
Patients had a median age of 62 years, with a median of diabetes duration of 7 years; 55.1% of the patients were men and the average HbA1c in the cohort was 8.2%. The detailed characteristics of the study cohort are presented in .
Table 1 Studied group baseline characteristics
In our studied group, the prevalence of DN according to MNSI score was 28.8% (57 individuals).
The presence of DN was associated with higher age (65 vs 59 years; P=0.001), HbA1c (8.6 vs 8.0%; P=0.027), BMI (31.9 vs 29.9 kg/m2), and with more accentuated exceed in waist circumference (25.2 vs 17.3 cm; P=0.003). Regarding the other studied parameters, we observed no significant differences with respect to the presence or absence of DN ().
Table 2 Comparison of studied parameters for patients with and without DN
Regarding the complications and comorbidities most commonly associated with T2DM, we observed a significantly higher prevalence in patients having DN for chronic kidney disease (56.1% vs 14.2%; P<0.001), retinopathy (54.4% vs 22.0%; P<0.001), and for autonomic neuropathy (52.6% vs 8.5%; P<0.001). No significant differences were observed for the prevalence of hypertension in the two studied subgroups ().
Table 3 Prevalence of complications and comorbidities in patients with and without DN
To evaluate the factors involved in the development of DN in diabetic patients, we built a backward-stepwise multivariate logistic regression model, having as dependent variable the positive diagnosis of DN and the initial predictors: patient’s age, diabetes duration, HbA1c value, sex, and BMI. The following three consecutive selection steps (having the exclusion criteria P>0.100) in the final regression equation were accepted as significant predictors for the development of DN: patient’s age, diabetes duration, and the BMI. The created model explained 17.3% of causality due to DN, the theoretical regression equation having 74.7% accuracy when compared with the collected data. According to our model, for every advance of 1 year in patient’s age, the odds for developing DN increased by 11.2% (P<0.001) and for each increase of 1 kg/m2 in patient’s BMI, the odds for developing DN increased by 10.9% (P=0.012).
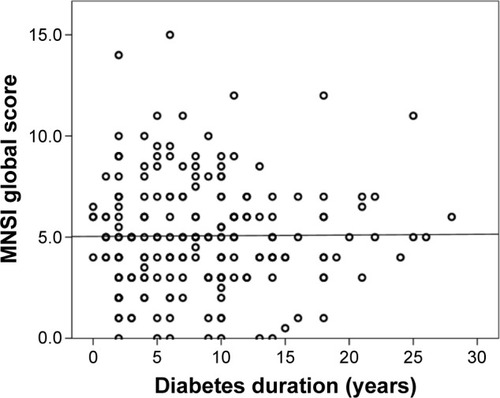
In our study, the severity of DN, assessed using the MNSI global score, was significantly and positively correlated with age (r=0.344; P<0.001; ) and with the HbA1c value (r=0.380; P<0.001). No significant correlations were observed between the severity of DN and diabetes duration (), BMI, or the number of centimeters exceeding the normal waist circumference.
Figure 1 Correlation between patient’s age and the MNSI score.
Abbreviation: MNSI, Michigan Neuropathy Screening Instrument.
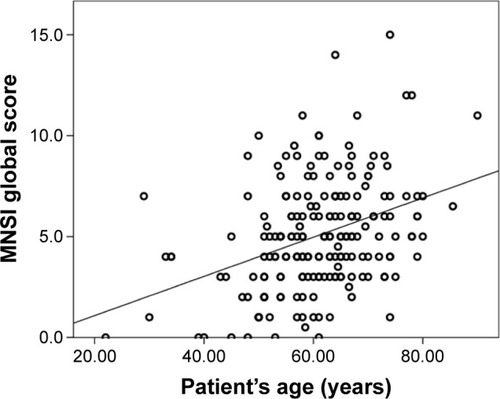
Figure 2 Correlation between diabetes duration and MNSI score.
To assess the independent impact (and not only as cofactors) on the severity of DN, we built a backward-stepwise multivariate regression model, having as dependent variable the DN severity and as initial predictors: patient’s age, diabetes duration, HbA1c value, and BMI. Our regression equation proved to be a good fit for the model, explaining 28.6% of the DN severity variations (R2=0.286). The model revealed a significant impact, as independent predictors, for patient’s age (P<0.001), diabetes duration (P=0.004), and HbA1c value (P<0.001), while BMI was only marginally significant (P=0.081). Our model suggests that for one standard deviation increase in patient’s age, we expect an increase in the DN severity of 0.43 standard deviations. The detailed results of the regression model are presented in .
Table 4 Multivariate regression model
Discussion
Older adults with diabetes have the highest rates of major lower-extremity amputation,Citation10 myocardial infarction, visual impairment, and end-stage renal disease of any age group. Those aged ≥75 years have higher rates than those aged 65–74 years for most complications. Deaths from hyperglycemic crises also are significantly higher in older adults. Those aged ≥75 years also have double the rate of emergency department visits for hypoglycemia than the general population with diabetes.Citation11
Peripheral neuropathies commonly affect older people. Peripheral neuropathy can be caused by axonal damage or demyelination, as well as damage to large or small fibers. In the US for 1999–2000, 28% of adults aged 70–79 years and 35% of adults aged ≥80 years had peripheral neuropathy based on a simple screen for reduced sensation at the foot.Citation12
The risk of falls and disabling symptoms like pain are quite pronounced in the elderly, leading to poor quality of life. Epidemiologic studies have found that older adults with poor peripheral nerve function have worse physical performance, balance, muscle density, and bone density.Citation13–Citation17
Diabetes and heavy alcohol use commonly cause symmetrical axonal polyneuropathies.
A twofold higher prospective decline in motor performance exists for older adults with distal symmetrical neuropathy.Citation18
The studied group had a relatively poor glycemic and lipid control, having at the same time a moderate T2DM duration. These characteristics, representative of the local population of patients with T2DM, were not influenced by the investigators selection, thus we cannot add in the discussion a possible selection bias. The studied group baseline characteristics were a consequence of the population-based consecutive-case enrollment principle.
DNs are the most common forms of neuropathy, they account for more hospitalizations than all other diabetic complications combined, and are responsible for 50%–75% of nontraumatic amputations.Citation19,Citation20
Clinical consequences of higher fall and fracture rates are also evident in older adults with peripheral nerve impairments. In a prospective cohort aged ≥70 years, those with loss of touch sensation in their feet had 2.5-times greater risk of major injurious falls, including fractures, joint dislocations, lacerations requiring sutures, and intracranial injuries.Citation21 In the Study of Osteoporotic Fractures, recurrent falling was related to worse vibration sense (age-adjusted odds ratio =1.12, 95% confidence interval: 1.05–1.19) and loss of touch sensation (age-adjusted odds ratio =1.58, 95% confidence interval: 1.34–1.87) in older women.Citation22
The management of diabetic polyneuropathy has three main elements: normal blood glucose level, foot care, and treatment of pain. Blood glucose level is the most important factor in the prevention and progression of DN.Citation23 For optimal foot care, patients should be educated to inspect their feet on a daily basis to look for dry or cracking skin, fissures, plantar callus formation, and signs of early infection between the toes and around the toe nails. Fortunately, only a minority of patients with diabetic polyneuropathy will develop painful symptoms and sometimes pain symptoms may resolve spontaneously. In other cases, pain control may be achieved using one or more of the drugs.
Usually, there are no specific treatments available. A multidisciplinary approach with pain relief, physiotherapy, management of anxiety and depression are important in managing these patients.
According to our study, for every advance of 1 year in patient’s age, the odds for developing DN increased by 11.2%.
As in published literature, we found that DN is more common among elderly people and during its evolution is accompanied by an account of complications, which is why DN should be diagnosed and treated earlier.Citation24 Like in other studies, we observed that the influence of age persists even after adjusting for other, very important risk factors, like glycemic control or diabetes duration. It is known that complications of T2DM are a consequence of a long-time poor glycemic control, this being the reason why in many studies the presence and severity of DN and other T2DM complications is described as being associated with a longer diabetes duration.Citation25 However, if a good glycemic control is obtained during the entire course of DM, the probability of developing T2DM complications is similar to a nondiabetic one. After adjustments for glycemic control and other possible confounding factors in our study, we observed that diabetes duration is a significant predictor for DN only as a cofactor to others, having a nonsignificant influence when analyzed independently. This statement demonstrates furthermore that the advance in age acts in an independent manner in relation to the diabetes duration, being associated with an increased risk of developing DN; this is why, we agree that age is an independent factor for the development of DN in T2DM patients.
Regarding the limitations of this study, we identified that this study had a cross-sectional design and the T2DM complications developed during a long-time exposure to elevated blood-sugar levels. The quality of the glycemic control, measured using the HbA1c value, can be evaluated for no longer than 3 months prior to the enrollment in the study. However, in many patients, a cross-sectional not-adequate glycemic control is associated with a prior history of deteriorated metabolic control, thus it may reflect the association between this parameter and the occurrence of T2DM chronic complications, including DN. Another limitation of the study is the use of the MNSI tool for the diagnosis of DN; MNSI is a validated screening tool for the diagnosis of DN, however, it cannot be considered as a “gold standard” in the diagnosis and severity evaluation of DN.
The results of this study, demonstrating that advancing age is associated with an increased risk of developing DN in T2DM patients, emphasize the necessity of an intensified, proactive screening for DN in elderly patients with T2DM.
Conclusion
According to our study, the severity of DN was significantly and positively correlated with age and with the HbA1c value. No significant correlations were observed between the severity of DN and diabetes duration, BMI, or the number of centimeters exceeding the normal waist circumference. Age influenced the presence of DN, independent of other risk factors.
Disclosure
The authors report no conflicts of interest in this work.
References
- International Diabetes FederationGlobal Guideline for Managing Older People with Type 2 DiabetesBelgiumInternational Diabetes Federation201367
- Centers for Disease Control and PreventionNational Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United StatesAtlanta, GAUS Department of Health and Human Services2011
- BrownAFMangioneCMSalibaDSarkisianCACalifornia Health-care Foundation/American Geriatrics Society Panel on Improving Care for Elders with DiabetesGuidelines for improving the care of the older person with diabetes mellitusJ Am Geriatr Soc200351Suppl GuidelinesS265S28012694461
- VinikAIMitchellBDLeichterSBWagnerALO’BrianJTGeorgesLPEpidemiology of the complications of diabetesLeslieRDGRobbinsDCDiabetes: Clinical Science in PracticeCambridge, UKCambridge University Press1995221287
- KnuimanMWelbornTMcCannVStantonKConstableIPrevalence of diabetic complications in relation to risk factorsDiabetes198635133213393770311
- YoungMJBoultonAJMacLeodAFWilliamsDRSonksenPHA multicenter study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic populationDiabetologia19933615
- WatkinsPJThomasPKDiabetes mellitus and the nervous systemJ Neurol Neurosurg Psychiatry19986556206329810929
- SiyumSPippaMPeripheral neuropathy in older peopleGM2012424752
- StevensPELevinAKidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guidelineAnn Intern Med20131581182583023732715
- LiYBurrowsNRGreggEWAlbrightAGeissLSDeclining rates of hospitalization for nontraumatic lower extremity amputation in the diabetic population aged 40 years or older: U.S., 1988–2008Diabetes Care20123527327722275440
- Centers for Disease Control and PreventionDiabetes Public Health Resource Available from: www.cdc.gov/diabetesAccessed December 17, 2015
- GreggEWSorliePPaulose-RamRPrevalence of lower-extremity disease in the US adult population ≥40 years of age with and without diabetes: 1999–2000 National Health and Nutrition Examination SurveyDiabetes Care2004271591159715220233
- FordESBody mass index, diabetes, and C-reactive protein among U.S. adultsDiabetes Care1999221971197710587828
- FestaAD’AgostinoRJrHowardGMykkanenLTracyRPHaffnerSMChronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS)Circulation2000102424710880413
- ResnickHEStansberryKBHarrisTBDiabetes, peripheral neuropathy, and old age disabilityMuscle Nerve200225435011754184
- StrotmeyerESCauleyJASchwartzAVReduced peripheral nerve function is related to lower hip BMD and calcaneal QUS in older white and black adults: the Health, Aging, and Body Composition StudyJ Bone Miner Res2006211803181017002569
- LauretaniFBandinelliSBartaliBAxonal degeneration affects muscle density in older men and womenNeurobiol Aging2006271145115416085338
- InzitariMCarloABaldereschiMRisk and predictors of motor-performance decline in a normally functioning population-based sample of elderly subjects: the Italian Longitudinal Study on AgingJ Am Geriatr Soc20065431832416460385
- HolzerSECamerotaAMartensLCuerdonTCrystalPZagariMCosts and duration of care for lower extremity ulcers in patients with diabetesClin Ther1998201691819522113
- CaputoGMCavanaghPRUlbrechtJSGibbonsGWKarchmerAWAssessment and management of foot disease in patients with diabetesN Engl J Med19943318548607848417
- KoskiKLuukinenHLaippalaPKivelaSLRisk factors for major injurious falls among the home-dwelling elderly by functional abilities. A prospective population-based studyGerontology1998442322389657085
- SchwartzAVHillierTASellmeyerDEOlder women with diabetes have a higher risk of falls: a prospective studyDiabetes Care2002251749175412351472
- ViswanathanVTilakPKumpatlaSRisk factors associated with the development of overt nephropathy in type 2 diabetes patients: a 12-year observational studyIndian J Med Res20121361465322885263
- VinikAIStrotmeyerESNakaveAAPatelCVDiabetic neuropathy in older adultsClin Geriatr Med200824340718672180
- ValensiPGirouxCSeeboth-GhalayiniBAttaliJRDiabetic peripheral neuropathy: effects of age, duration of diabetes, glycemic control, and vascular factorsJ Diabetes Complications199711127349025010
