Abstract
Rationale
Identifying patients at high risk of critical illness is necessary for the development and testing of strategies to prevent critical illness. The aim of this study was to determine the relationship between high elder risk assessment (ERA) score and critical illness requiring intensive care and to see if the ERA can be used as a prediction tool to identify elderly patients at the primary care visit who are at high risk of critical illness.
Methods
A population-based historical cohort study was conducted in elderly patients (age >65 years) identified at the time of primary care visit in Rochester, MN, USA. Predictors including age, previous hospital days, and comorbid health conditions were identified from routine administrative data available in the electronic medical record. The main outcome was critical illness, defined as sepsis, need for mechanical ventilation, or death within 2 years of initial visit. Patients with an ERA score of 16 were considered to be at high risk. The discrimination of the ERA score was assessed using area under the receiver operating characteristic curve.
Results
Of the 13,457 eligible patients, 9,872 gave consent for medical record review and had full information on intensive care unit utilization. The mean age was 75.8 years (standard deviation ±7.6 years), and 58% were female, 94% were Caucasian, 62% were married, and 13% were living in nursing homes. In the overall group, 417 patients (4.2%) suffered from critical illness. In the 1,134 patients with ERA >16, 154 (14%) suffered from critical illness. An ERA score ≥16 predicted critical illness (odds ratio 6.35; 95% confidence interval 3.51–11.48). The area under the receiver operating characteristic curve was 0.75, which indicated good discrimination.
Conclusion
A simple model based on easily obtainable administrative data predicted critical illness in the next 2 years in elderly outpatients with up to 14% of the highest risk population suffering from critical illness. This model can facilitate efficient enrollment of patients into clinical programs such as care transition programs and studies aimed at the prevention of critical illness. It also can serve as a reminder to initiate advance care planning for high-risk elderly patients. External validation of this tool in different populations may enhance its generalizability.
Introduction
Frequent hospitalizations and burdensome care transitions are common in the last 3 months of a frail elderly patient’s life.Citation1,Citation2 In a large study of Medicare beneficiaries, intensive care unit (ICU) use in the last month of life was 26.3%, a significant increase between 2000 and 2009.Citation2 There are increasing calls for advanced care planning to help patients and families facing advanced life-limiting illness.Citation3–Citation5 The American Geriatrics Society has called for a dramatic change in the approach to medical care for the frail elderly patients with multimorbidity, emphasizing that a discussion of goals of care and individualized prognosis should ideally precede that of treatment option.Citation6 Patients who have goals of care discussions with their physicians indicate a better understanding and comfort level afterward, and families report less bereavement-related stress.Citation7 Turning points in care such as changes in symptoms, new comorbidities, and indications for new interventions open opportunities for goals of care discussions.Citation8 However, many elderly patients are doing well until an acute unexpected illness precipitates sudden decline. Being able to predict such risk can be helpful to encourage discussions on goals of care.
The elder risk assessment (ERA) has been shown to predict hospital stay and emergency room visitsCitation9 as well as mortality and nursing home (NH) placement.Citation10 An equally important outcome is critical illness defined by Seymour et alCitation11 as the delivery of mechanical ventilation (MV), severe sepsis, or death. It remains unclear how well the ERA predicts critical illness. To answer this question, we performed a retrospective cohort analysis of a population of people using ERA and evaluated the subsequent admission to the ICU for MV or sepsis or death within 2 years of the initial outpatient visit. Our aim was to determine the relationship between high-risk people (as determined by ERA) and critical illness.
Methods
Study design
This was a population-based historical cohort study conducted in elderly patients (age >65 years) identified at the time of primary care visit in Rochester, MN, USA. The study was approved by the Mayo Clinic Institutional Review Board.
Setting
The study was conducted at an academic medical center in Rochester, MN, USA. All individuals were impaneled within the primary care internal medicine practice and had a primary care physician. The initial cohort used to develop the ERA score was designed for January 1, 2005, and had incident outcomes for 2 years ending in December 31, 2006. Details of this study have been previously published.Citation9
Participants
All participants in the study were at the age of 65 years or older. Those individuals who did not give consent for medical record review were excluded from the study, according to Minnesota state statue with regard to medical record use and privacy (Minnesota Department of Educations, 2003).
Demographic variables were electronically abstracted from the electronic medical record (EMR) and the administrative databases of the health records system of Mayo Clinic. Those included date of birth, sex, race, marital status, prior hospital admissions, number of days hospitalized in the prior 2 years, and NH residence.
Predictors
The primary predictor variable was the ERA index, an administrative risk index that uses data from the EMR to identify those patients at the highest risk of adverse outcomes. This risk stratification is made available at the point of care, which overcomes the limitations of other prognostic indices, many of which require data collection that is not part of the routine clinical visit.Citation12 The ERA uses administrative data to help calculate a score on all individuals over the age of 60 years. The ERA scoring mechanism weighs age, previous hospital stay, and comorbid illnesses within the mechanism. The scores range from −1 to 43 with scores >16 determining high risk for hospitalization. The ERA score has also been shown to predict mortality and NH placement.Citation10 The demographic predictor variables collected included date of birth, sex, marital status, race, and the number of hospital admission days in the prior 2 years (January 1, 2003, to December 31, 2004). Age was stratified into categories of 65–74 years, 75–84 years, and >85 years. Comorbid medical illnesses included the presence or history of diabetes mellitus, coronary artery disease, congestive heart failure, stroke, chronic obstructive pulmonary disease, history of cancer, history of hip fracture, and dementia. History of cancer excluded nonmelanoma skin cancers. Diagnoses were identified using International Classification of Diseases Ninth Revision (ICD-9) billing codes entered by physicians during both inpatient and outpatient encounters. The Charlson Comorbidity Index (CCI) in this study used data based upon ICD-9 codes taken from the billing records. Administrative CCI methodologies have been proven to predict 1-year mortality.Citation13
Outcomes
The primary outcome was critical illness defined as MV use, death, or sepsis as previously done by Seymour et alCitation11 within 2 years of initial visit. MV use and sepsis were derived from billing information from the ICUs at St Mary’s Hospital and Rochester Methodist Hospital, the two primary hospitals of Mayo Clinic, Rochester, MN, USA. Mortality information was collected from the EMR and is updated within the EMR when death occurs within the hospital or health care system (NH). The record is also updated with local obituaries and death announcements.
Statistical analysis
The comparisons of the descriptive variables used univariate logistic regression comparing participants who did and did not have ICU outcomes. Because the ERA takes into account age, comorbid status, and utilization information, we did not adjust for other significant variables in this analysis. Dividing the ERA and the CCI into groups allowed the comparison of the lowest score as the baseline compared to higher scores. This comparison allowed the creation of odds ratios (ORs) for the higher scoring groups compared to the lowest scoring group. Confidence intervals (CIs) were set at 95%, and P-values <0.05 were considered significant. All analyses were completed using SAS 9.01 (SAS Institute Inc., Cary, NC, USA). The discrimination of the model was assessed using area under the receiver operating characteristic curve (AUC).
Results
In the initial cohort, there were 13,457 patients who were eligible. Of those, 12,650 had given consent for medical record review.Citation9 Within this cohort, claims and full information on ICU utilization were available for 9,872 participants. The demographics of the cohort show an older cohort with a mean age of 75.8 years (SD ±7.6 years), and 58% were female, 94% were Caucasian, 62% were married, and 13% were living in NHs. The mean CCI was 3.34 (±3.29). Eleven percent of the population had ERA score ≥16. Demographics of the cohort are presented in . In general, age, previous hospital utilization, and comorbid health issues were significant predictors for all three outcomes.
Table 1 Overall demographics and critical illness status
Critical illness
The ERA and the Charlson index and NH use were predictive for critical illness. The ORs for critical illness outcomes are listed in . Of the participants admitted to the ICU with critical illness, 290 (33%) had an ERA score >16 as compared to only 13 (1%) with a score of ≤1. Patients with an ERA score of 16 or higher had an OR of 6.35 (95% CI 3.51–11.48) as compared to the lowest scoring group. NH use at any point in the previous 2 years was also a predictor of critical illness, OR 2.02 (95% CI 1.70–2.40), P<0.0001. The CCI performed better than the ERA score with an OR of 6.17 (95% CI 3.93–9.70) for a score between 5 and 8 and 10.74 (95% CI 6.78–17.03) for a score of >9.
Table 2 Univariate logistic regression
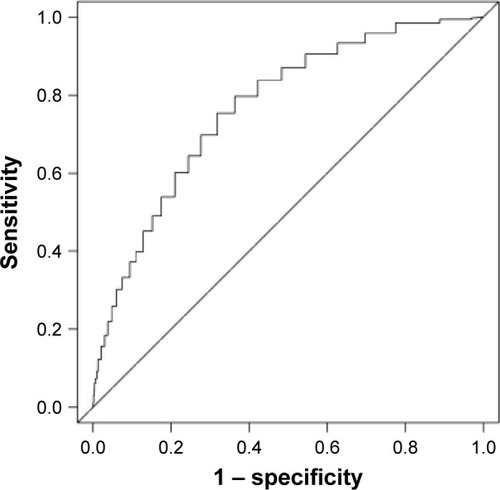
The receiver operating characteristic curve for the ERA score associated with the main combined outcome is shown in . The AUC for ERA score predicting the primary outcome of critical illness was 0.75. For MV use only, the AUC was 0.70. For mortality only, the AUC was 0.77.
MV use
We also looked separately at MV use as an important discussion point included in advance care planning. Thirty-two percent of the participants using MV had ERA scores >16 compared to only 3% with scores ≤1. The ERA score significantly predicted ventilator use with an OR of 2.49 (95% CI 1.09–5.69), P=0.03, comparing the highest to the lowest group. The CCI also predicted ventilator use with an OR of 22.35 (95% CI 7.79–64.12) comparing the highest to the lowest scoring group.
Discussion
In this retrospective cohort study, we found that higher ERA scores resulted in higher odds of critical illness. The ERA has previously been shown to predict risk for hospital admission or emergency room visitsCitation9 as well as mortality and NH admission.Citation10 Thus, the findings that higher ERA scores also predict critical illness, defined as death, MV, or sepsis, are consistent with the general premise that this simple administrative index can help predict patient-important outcomes. The CCI performed better than the ERA score in this study. This is in line with the previous attempts at trying to improve upon this important research tool. However, the CCI is not very practical to use at the bedside with patient because of the many variables included in the score. The ERA score achieves good discrimination with a much simpler index. At our institution, we have already made the ERA score available electronically at the point of care to facilitate efficient enrollment of patients into our clinical care transitions and palliative homebound programs aimed at the prevention of critical illness and rehospitalizations in our high-risk patients.Citation14,Citation15
Seymour et alCitation11 studied the prediction of critical illness, defined as the delivery of MV, severe sepsis, or death in nontrauma adult patients at the emergency care setting. Older age, lower systolic blood pressure, abnormal respiratory rate, lower Glasgow Coma Score, lower pulse oximetry, and NH residency were predictors of critical illness. Similar to our study, out-of-hospital variables predicted patient-important outcomes and might improve triage decisions in the emergency department. Our study is designed to identify patients in the primary care setting prior to the onset of acute illness to allow ample time for discussions of goals of care. Another difference between the Seymour prediction score and ours is that it is dependent on the collection of clinical data points and the manual scoring at the point of care, while in our system, the ERA score automatically pulls administrative data and makes a risk score available at the point of care. This minimizes the burden on the clinician and should increase its use.
Olmsted County has a relatively low rate of ICU utilization during a terminal hospital admissionCitation16 when compared to national rates.Citation17 Still a significant proportion of the total within-age group ICU days are used by elderly decedents in the last year of life ranging from 27.2% in the 65–74-year olds to 68.1% in the >85-year olds. This amounts to one in five ICU days used by elderly decedents in their last year of life.Citation16 Sepsis and other critical illness states could possibly be prevented by targeting the high-risk elderly patients for priority triage and early intervention for ambulatory care-sensitive conditions. Identifying elderly individuals as having high risk should also serve to prompt discussions of goals of care. The current moral and technological imperatives to treat against all odds are powerful and overshadow patient’s choice.Citation18 We have argued that this is, to a large extent, based on a narrow interpretation of beneficence as life extension as opposed to a broader view of patient-defined goals and values.Citation19 Many elderly patients value independence over life extension.Citation20 Thus, clarifying goals of care before the onset of acute illness may avoid burdensome ICU care near the end of life where it may not be consistent with the patient’s values and preferences. Palliative care should be presented as options to all patients with poor prognosis as this has been shown to increase quality of care, lengthen life,Citation21 and save moneyCitation22 – a rare win–win situation.
This study has strengths and limitations that are inherent with a retrospective cohort analysis. The strength lies in the strong population-based data in Olmsted County. The patients were required to be impaneled within the primary care groups at Mayo Clinic. This excludes the large referral population, which otherwise could have biased the data. The population of Olmsted County has similar age- and sex-specific mortality as the entire US population; however, it is less ethnically diverse, wealthier, and more educated.Citation23 These differences need to be taken into account when evaluating the generalizability of our data. The limitations include obtaining patient information from administrative databases that was recorded for purposes other than the pursuit of our hypothesis. The predictors and outcomes were determined from billing data, which may underestimate secondary diagnoses. However, administrative data such as ICD-9 codes have been found to correlate well with chart diagnoses.Citation24 Second, this is a retrospective cohort analysis, which also risks underreported risk factors and outcomes; however, both the ERA score and the outcomes are based on hospitalization data that are well captured by Mayo administrative data. It is also possible that patients in the cohort could have hospitalizations or chronic diagnoses elsewhere and of which our EMR is therefore unaware. However, most impaneled patients receive both their acute and chronic care from Mayo Clinic. By design, the model only collected retrospective collection of risk factor variables and did not include functional status measures or other patient-provided information, which has been shown to predict outcomes. Functional status data are dependent on patient-provided information or clinician-administered performance testing, which is neither routinely collected nor easily extractible from administrative data.Citation25–Citation27 The use of a combined end point for our outcome of critical illness can be contested. Few will disagree that sepsis is a critical illness and that patient requiring MV is usually although not invariably critically ill. However, death, while an important outcome, is not always preceded by critical illness, and this definition may miss other critical disease states that were not included in the definition. Because of the inherent limitations of working with secondary data, we chose to go with a definition previously used and published.Citation11 Finally, we did not estimate calibration of prediction tool.
Conclusion
A simple model based on easily obtainable administrative data predicts death and critical illness in the next 2 years in elderly outpatients. This model has already proven valuable at Mayo Clinic to facilitate efficient enrollment of patients into studies aiming to prevent critical illness and increase the rate of advanced care planning.Citation14,Citation28 External validation is required prior to clinical use at other institutions.
Disclosure
The authors report no conflicts of interest in this work.
References
- GozaloPTenoJMMitchellSLEnd-of-life transitions among nursing home residents with cognitive issuesN Engl J Med2011365131212122121991894
- TenoJMGozaloPLBynumJPChange in end-of-life care for medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009JAMA2013309547047723385273
- KettlPA piece of my mind. One vote for death panelsJAMA2010303131234123520371773
- VierraMDeath panelsAnn Intern Med2012156539439522393137
- KirkpatrickJNHauptmanPJGoodlinSJBundling informed consent and advance care planning in chronic cardiovascular disease: we need to talkJAMA Intern Med201517515625419993
- American Geriatrics Society Expert Panel on the Care of Older Adults with MultimorbidityPatient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics SocietyJ Am Geriatr Soc201260101957196822994844
- WrightAAZhangBRayAAssociations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustmentJAMA2008300141665167318840840
- GoodlinSJHauptmanPJArnoldRConsensus statement: palliative and supportive care in advanced heart failureJ Card Fail200410320020915190529
- CraneSJTungEEHansonGJChaSChaudhryRTakahashiPYUse of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: the elders risk assessment indexBMC Health Serv Res20101033821144042
- TakahashiPYTungEECraneSJChaudhryRChaSHansonGJUse of the elderly risk assessment (ERA) index to predict 2-year mortality and nursing home placement among community dwelling older adultsArch Gerontol Geriatr2012541343821397346
- SeymourCWKahnJMCookeCRWatkinsTRHeckbertSRReaTDPrediction of critical illness during out-of-hospital emergency careJAMA2010304774775420716737
- YourmanLCLeeSJSchonbergMAWideraEWSmithAKPrognostic indices for older adults: a systematic reviewJAMA2012307218219222235089
- ChaudhrySJinLMeltzerDUse of a self-report-generated Charlson Comorbidity Index for predicting mortalityMed Care200543660761515908856
- ChenCYThorsteinsdottirBChaSSHealth care outcomes and advance care planning in older adults who receive home-based palliative care: a pilot cohort studyJ Palliat Med2014181384425375663
- TakahashiPYHaasLRQuiggSM30-day hospital readmission of older adults using care transitions after hospitalization: a pilot prospective cohort studyClin Interv Aging2013872973623818770
- SeferianEGAfessaBAdult intensive care unit use at the end of life: a population-based studyMayo Clin Proc200681789690116835969
- AngusDCBarnatoAELinde-ZwirbleWTRobert Wood Johnson Foundation ICU End-Of-Life Peer GroupUse of intensive care at the end of life in the United States: an epidemiologic studyCrit Care Med200432363864315090940
- KaufmanSRShimJKRussAJOld age, life extension, and the character of medical choiceJ Gerontol B Psychol Sci Soc Sci2006614S175S18416855038
- ThorsteinsdottirBSwetzKMTilburtJCDialysis in the frail elderly – a current ethical problem, an impending ethical crisisJ Gen Intern Med201328111511151623686511
- HaberleTHShinkunasLAEreksonZDKaldjianLCGoals of care among hospitalized patients: a validation studyAm J Hosp Palliat Care201128533534121097876
- TemelJSGreerJAMuzikanskyAEarly palliative care for patients with metastatic non-small-cell lung cancerN Engl J Med2010363873374220818875
- TaylorDHJrOstermannJVan HoutvenCHTulskyJASteinhauserKWhat length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program?Soc Sci Med20076571466147817600605
- St SauverJLGrossardtBRLeibsonCLYawnBPMeltonLJ3rdRoccaWAGeneralizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology ProjectMayo Clin Proc201287215116022305027
- QuanHParsonsGAGhaliWAValidity of information on comorbidity derived rom ICD-9-CCM administrative dataMed Care200240867568512187181
- BogardusSTJrTowleVWilliamsCSDesaiMMInouyeSKWhat does the medical record reveal about functional status? A comparison of medical record and interview dataJ Gen Intern Med2001161172873611722685
- FriedLPGuralnikJMDisability in older adults: evidence regarding significance, etiology, and riskJ Am Geriatr Soc1997451921008994496
- FriedLPKronmalRANewmanABRisk factors for 5-year mortality in older adults: the Cardiovascular Health StudyJAMA199827985855929486752
- TakahashiPYHansonGJThorsteinsdottirBThe impact of telemonitoring upon hospice referral in the community: a randomized controlled trialClin Interv Aging2012744545123152674