Abstract
Background
Registry-based monitoring of the safety and efficacy of interventions in patients with ischemic heart disease requires validated algorithms.
Objective
We aimed to evaluate algorithms to identify acute myocardial infarction (AMI) in the Danish National Patient Registry following percutaneous coronary intervention (PCI).
Methods
Patients enrolled in clinical drug-eluting stent studies at the Department of Cardiology, Aarhus University Hospital, Denmark, from January 2006 to August 2012 were included. These patients were evaluated for ischemic events, including AMI, during follow-up using an end point committee adjudication of AMI as reference standard.
Results
Of 5,719 included patients, 285 patients suffered AMI within a mean follow-up time of 3 years after stent implantation. An AMI discharge diagnosis (primary or secondary) from any acute or elective admission had a sensitivity of 95%, a specificity of 93%, and a positive predictive value of 42%. Restriction to acute admissions decreased the sensitivity to 94% but increased the specificity to 98% and the positive predictive value to 73%. Further restriction to include only AMI as primary diagnosis from acute admissions decreased the sensitivity further to 82%, but increased the specificity to 99% and the positive predictive value to 81%. Restriction to patients admitted to hospitals with a coronary angiography catheterization laboratory increased the positive predictive value to 87%.
Conclusion
Algorithms utilizing additional information from the Danish National Patient Registry yield different sensitivities, specificities, and predictive values in registry-based detection of AMI following PCI. We were able to identify AMI following PCI with moderate-to-high validity. However, the choice of algorithm will depend on the specific study purpose.
Introduction
First-time ischemic events such as acute myocardial infarction (AMI) are used to study the risk and to improve the prognosis of ischemic heart disease. AMI is often treated with percutaneous coronary intervention (PCI). To monitor the safety and efficacy of this intervention, robust registry-based algorithms are required for the detection of AMI in this population.Citation1
In Denmark, record linkage using the ten-digit civil registration number offers unique possibilities for epidemiological studies.Citation2 As the key registry, the Danish National Patient Registry contains data on all Danish hospital admissions and outpatient clinic visits, starting in 1997.Citation3 Thereby, the Danish National Patient Registry can be utilized for the detection of AMI in the Danish population. However, to what extent the Danish National Patient Registry can be used to identify AMI in patients with existing ischemic heart disease undergoing PCI is unknown.Citation3 In this study, we aimed to create an algorithm for using the Danish National Patient Registry to identify patients with AMI following PCI.
Methods
Study design, setting, and participants
We performed the evaluation in a population of patients treated with drug-eluting coronary stents as a part of clinical drug-eluting coronary stent studies. These patients were enrolled in the Central Region of Denmark, which covers a population of ~1.3 million inhabitants corresponding to 23% of the Danish population. The patients were treated with PCI at the Department of Cardiology, Aarhus University Hospital, Denmark, from January 2006 to August 2012.Citation4–Citation7 Using this cohort with end-point committee adjudication of AMI as reference standard, we compared different algorithms for the detection of AMI in the Danish National Patient Registry following PCI.
Definition of AMI
Clinical end-point committee adjudication of AMI was performed in each trial as previously described.Citation4–Citation7 Briefly, possible AMI events were screened using the Danish National Patient RegistryCitation3 and the Western Denmark Heart Registry.Citation8 Possible events were subsequently reviewed by a clinical end-point committee, with reference to the contemporary universal definitions of AMI.Citation9 The end-point committee also reviewed all deaths in order to classify these as cardiac or noncardiac. In case of cardiac death, the end-point committee evaluated whether it was secondary to AMI.
The Danish National Patient Registry
The Danish National Patient Registry contains information on all nonpsychiatric hospital admissions since 1977 and emergency room and outpatient clinic visits since 1995.Citation3 The registry contains data from each admission including the admission and discharge dates, admission type, discharge diagnoses, and procedures performed during the admission.Citation3 The International Classification of Diseases tenth revision (ICD-10) codes have been used since 1994. All admissions have one primary discharge diagnosis reflecting the primary reason for the admission. Additionally, admissions may have one or more secondary discharge diagnoses reflecting coexisting conditions. Discharge diagnoses are determined exclusively by the discharging physician.
The Danish national health care service is tax supported and provides free health care. Mandatory reporting to the Danish National Patient Registry, which is managed by the Danish Health Authority, ensures nationwide coverage of AMI hospitalisations.Citation3
Algorithms for detection of AMI in the Danish National Patient Registry
To establish an algorithm for the detection of AMI in the Danish National Patient Registry, we identified AMI from discharge diagnoses using the ICD-10 code I21. Diagnoses were identified as primary (only) and primary or secondary discharge diagnoses. Furthermore, algorithms were based on patient contact type (inpatient admission), admission type (acute or elective), and hospital type (with or without coronary angiography capability). shows the details of the different algorithms.
Table 1 Algorithms for detection of acute myocardial infarction following percutaneous coronary intervention in the Danish National Patient Registry
Statistical analyses
Follow-up of the trial participants started upon discharge after drug-eluting stent implantation.Citation4–Citation7 Patients were followed until a first AMI was detected in the Danish National Patient Registry, by the end-point committee, or in both simultaneously.
For each algorithm for identifying AMI following PCI in the Danish National Patient Registry, we calculated sensitivity, specificity, and predictive values using the end-point committee adjudicated cases of AMI as reference. We stratified the results according to AMI status at the time of PCI (AMI before PCI, AMI at same date of PCI, or PCI without prior AMI) to determine whether recurrent AMI could be detected equally well as first-time AMI. We also stratified according to sex, age (≤65 years vs >65 years), indication for PCI (acute coronary syndrome vs stable angina pectoris), and time from index procedure to AMI. Confidence intervals were calculated with Jeffrey’s method.Citation10
All statistical analyses were performed using SAS software Version 9.4 (SAS Institute Inc., Cary, NC, USA). The study was approved by the Danish Data Protection Agency (Ref no 2012-41-0164) and the Danish Health Authority (Ref no 6-8011-270/2). Registry studies do not require ethical committee approval or patients consent in Denmark.
Results
We evaluated 5,719 patients with a mean follow-up time of 3 years. Of these, 285 had an end-point committee adjudicated AMI. Baseline characteristics of the PCI cohort are presented in .
Table 2 Baseline characteristics of patients with percutaneous coronary intervention
The results from different algorithms are reported in and . Since patients with a detected AMI, either by the algorithm or by the end-point committee, were censored from the time of AMI detection, the number of patients with AMI and the average follow-up period vary between algorithm evaluations. Two-way tables for each algorithm evaluation are provided in –.
Figure 1 Sensitivity vs 1-positive predictive value for algorithms A–F.
Abbreviation: PPV, positive predictive value.
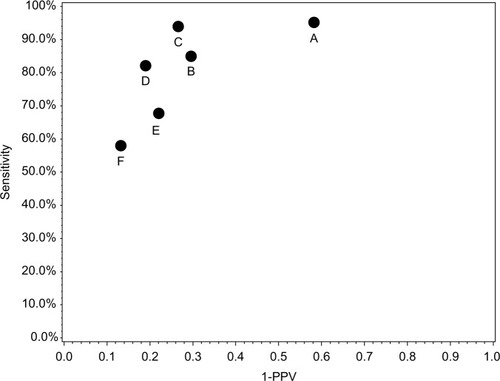
Table 3 Performance of algorithms for detection of acute myocardial infarction following percutaneous coronary intervention in the Danish National Patient Registry
The algorithms with the best performance were the combination of AMI as primary (algorithm D) or primary or secondary (C) discharge diagnosis combined with acute admission. A broader algorithm (A) combining AMI as primary or secondary discharge diagnosis and all inpatients, instead of acute admissions, improved the sensitivity (95%), but decreased the positive predictive value considerably (42%). Restricting the algorithm to admissions at a hospital with coronary angiography capability increased the positive predictive value. However, these narrower algorithms all had a decreased sensitivity (, ).
Evaluation of a broad algorithm of AMI diagnosis (code I21) as either primary or secondary diagnosis and inpatient (algorithm A, ) showed that 13 patients with a validated AMI were not detected (). These AMIs resulted in cardiac arrest (n=6) and were recorded as such with the corresponding ICD-10 code in the Danish National Patient Registry. For the remaining patients, the discharge diagnosis codes covered various ICD-10 codes for ischemic heart disease, examination for angina, and examination for acute coronary syndrome.
Evaluation of a narrow algorithm of AMI diagnosis (code I21) as both primary or secondary diagnosis and acute admission (algorithm C, ) showed that 95 patients were recorded with AMI diagnoses in the Danish National Patient Registry without having an end-point committee adjudicated AMI (). The majority of these were patients admitted for examination for angina or examination for acute coronary syndrome.
The stratified analyses of algorithm C are reported in , with corresponding two-way tables provided in –. Sex and age had no major impact on the parameters. Among patients with acute coronary syndrome, positive predictive value was lower than among patients with stable angina pectoris. Time from index procedure to AMI seemed to influence positive predictive values, which were lowest within the first 30 days after discharge following PCI and improved thereafter.
Table 4 Performance of algorithm C (all acute admissions with acute myocardial infarction as primary or secondary discharge diagnosis) across subgroups
Discussion
We found that different algorithms yielded different sensitivities, specificities, and predictive values to detect AMI in the Danish National Patient Registry. The choice of algorithm will depend on the specific study purpose. However, combining the discharge diagnosis of AMI (I21) and acute admission yielded a better positive predictive value for patients with prior PCI than use of a discharge diagnosis of AMI alone.
Apart from the diagnosis AMI, our algorithms relied on the variable “acute admission”, which has been shown to have a high validity in the Danish National Patient Registry.Citation11 Previously, the validity of AMI diagnoses in the general population, as registered in the Danish National Patient Registry, has been validated using medical records,Citation12,Citation13 discharge summaries,Citation14,Citation15 or a clinical registry.Citation16 We recorded a lower positive predictive value of first-time AMI in the Danish National Patient Registry than in these earlier studies.Citation12–Citation14 This was expected as our study population consisted of patients with established ischemic heart disease undergoing PCI. These patients are therefore more likely to be given a later discharge diagnosis of AMI, ie, to be misclassified due to their prior medical history. Similar misclassification has also been previously shown for other conditions, eg, venous thromboembolism.Citation16 In agreement with this interpretation, we found a lower positive predictive value of the algorithm among patients with AMI during the index admission or with acute coronary syndrome as indication for stent implantation and within the first 30 days after stent implantation as compared to later.
The choice of algorithm will depend on the specific study purpose. For example, in registry-based randomized clinical trials with end-point adjudication by an end-point committee, it is important to detect as many of the potential events as possible. In this case, a broad algorithm, like algorithm A, seems the optimal choice. The low positive predictive value for this algorithm will be corrected by the end-point committee. In traditional randomized cohort studies relying on registry-based end points, ie, without adjudication by an end-point committee, algorithms C and D are preferable due to the combination of high sensitivity (although lower than algorithm A) and higher positive predictive values. Finally, in case–control studies, a high positive predictive value is preferred to correctly detect cases.
A small number of patients with adjudicated AMI did not have this diagnosis in the Danish National Patient Registry. One half of these patients died from cardiac arrest and were diagnosed with AMI by the end-point committee when the cause of death was reviewed. The other half had various ischemia-related diagnoses and were diagnosed by endpoint committee review of all angiographies and coronary interventions during the study period. A composite end point of registry-based AMI and all-cause death, often used in registry-based studies, would thus include half of the missed AMIs, ie, only very few true events would be overlooked by a use of combined end point and thereby improve sensitivity.
Strengths and limitations
We were able to evaluate the described algorithms using a large study population with end-point committee-validated AMIs. In comparison with earlier studies, this gave us an opportunity to evaluate sensitivity and specificity of the algorithms and also the positive predictive values in a subgroup of patients undergoing PCI. Thus, this study included patients treated with drug-eluting coronary stents, and the reported sensitivities and specificities of the different algorithms may not extend to the general population, to patients with ischemic heart disease without stent implantation, or to patients without previous ischemic heart disease.
Conclusion
Different algorithms utilizing additional information from the Danish National Patient Registry yielded different sensitivities, specificities, and predictive values in registry-based detection of AMI following PCI. The choice of algorithm will depend on the specific study purpose. However, it was possible to identify algorithms for AMI detection following PCI in the Danish National Patient Registry with moderate-to-high validity.
Supplementary Material
Table S1 Two-way table for detection algorithm A
Table S2 Two-way table for detection algorithm B
Table S3 Two-way table for detection algorithm C
Table S4 Two-way table for detection algorithm D
Table S5 Two-way table for detection algorithm E
Table S6 Two-way table for detection algorithm F
Table S7 Two-way table for algorithm C stratified for female sex
Table S8 Two-way table for algorithm C stratified for male sex
Table S9 Two-way table for algorithm C stratified for age ≤ 65 years
Table S10 Two-way table for algorithm C stratified for age > 65 years
Table S11 Two-way table for algorithm C stratified for indication of index stent, acute coronary syndrome
Table S12 Two-way table for algorithm C stratified for indication of index stent, stable angina
Table S13 Two-way table for algorithm C stratified on acute myocardial infarction prior to index admission
Table S14 Two-way table for algorithm C stratified on acute myocardial infarction at index admission
Table S15 Two-way table for algorithm C stratified on no prior acute myocardial infarction
Table S16 Two-way table for algorithm C stratified on time from admission, 0–30 days
Table S17 Two-way table for algorithm C stratified on time from admission, >30 days to 1 year
Table S18 Two-way table for algorithm C stratified on time from admission, < 1 year
Table S19 Two-way table for algorithm C stratified on time from admission, 1–2 years
Table S20 Two-way table for algorithm C stratified on time from admission, 2–3 years
Table S21 Two-way table for algorithm C stratified on time from admission, 3–4 years
Table S22 Two-way table for algorithm C stratified on time from admission, 4–5 years
Table S23 Two-way table for algorithm C stratified on time from admission, >30 days to 5 years
Disclosure
The authors report no conflicts of interest in this work.
References
- ThuesenLJensenLOTilstedHHEvent detection using population-based health care databases in randomized clinical trials: a novel research tool in interventional cardiologyClin Epidemiol2013535736124068874
- SchmidtMPedersenLSørensenHTThe Danish Civil Registration System as a tool in epidemiologyEur J Epidemiol201429854154924965263
- SchmidtMSchmidtSASandegaardJLEhrensteinVPedersenLSørensenHTThe Danish National Patient Registry: a review of content, data quality, and research potentialClin Epidemiol2015744949026604824
- ChristiansenEHJensenLOThayssenPScandinavian Organi-zation for Randomized Trials with Clinical Outcome (SORT OUT) V investigatorsBiolimus-eluting biodegradable polymer-coated stent versus durable polymer-coated sirolimus-eluting stent in unselected patients receiving percutaneous coronary intervention (SORT OUT V): a randomised non-inferiority trialLancet2013381986766166923374649
- JensenLOThayssenPMaengMScandinavian Organization for Randomized Trials With Clinical Outcome SORT OUT IV InvestigatorsThree-year outcomes after revascularization with everolimus- and sirolimus-eluting stents from the SORT OUT IV trialJACC Cardiovasc Interv20147884084825086842
- MaengMTilstedHHJensenLODifferential clinical outcomes after 1 year versus 5 years in a randomised comparison of zotarolimus-eluting and sirolimus-eluting coronary stents (the SORT OUT III study): a multicentre, open-label, randomised superiority trialLancet201438399342047205624631162
- RaungaardBJensenLOTilstedHHScandinavian Organization for Randomized Trials with Clinical Outcome (SORT OUT)Zotaro-limus-eluting durable-polymer-coated stent versus a biolimus-eluting biodegradable-polymer-coated stent in unselected patients undergoing percutaneous coronary intervention (SORT OUT VI): a randomised non-inferiority trialLancet201538599771527153525601789
- SchmidtMMaengMJakobsenCJExisting data sources for clinical epidemiology: the Western Denmark Heart RegistryClin Epidemiol2010213714420865111
- ThygesenKAlpertJSJaffeASWriting Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction, ESC Committee for Practice Guidelines (CPG)Third universal definition of myocardial infarctionEur Heart J201233202551256722922414
- BrownLDCaiTTDasGuptaAInterval estimation for a binomial proportionStat Sci2001162101117
- Vest-HansenBRiisAHChristiansenCFRegistration of acute medical hospital admissions in the Danish National Patient Registry: a validation studyClin Epidemiol2013512913323658498
- JoensenAMJensenMKOvervadKPredictive values of acute coronary syndrome discharge diagnoses differed in the Danish National Patient RegistryJ Clin Epidemiol200962218819418722087
- ColomaPMValkhoffVEMazzagliaGEU-ADR ConsortiumIdentification of acute myocardial infarction from electronic healthcare records using different disease coding systems: a validation study in three European countriesBMJ Open201336e002862
- MadsenMBallingHEriksenLSThe validity of the diagnosis of acute myocardial infarction in 2 registries: the Heart Registry compared to the National Patient RegistryUgeskr Laeger199015253083142301079
- ThygesenSKChristiansenCFChristensenSLashTLSørensenHTThe predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish national registry of patientsBMC Med Res Methodol2011118321619668
- MadsenMDavidsenMRasmussenSAbildstromSZOslerMThe validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA RegistryJ Clin Epidemiol200356212413012654406
- SchmidtMCannegieterSCJohannesdottirSADekkersOMHorváth-PuhóESørensenHTStatin use and venous thromboembolism recurrence: a combined nationwide cohort and nested case-control studyJ Thromb Haemost20141281207121524818818
