Abstract
Background
As the population ages, an increasing number of acute medical patients will be older and have comorbidities that may interact with their primary admission condition and worsen their prognosis.
Objectives
To examine whether 6-month mortality following acute medical admission was associated with gender, age, or comorbidity.
Methods
We used the Danish National Patient Registry, covering all Danish hospitals, to identify all acute medical admissions to Aarhus University Hospital during 2008 and comorbidities. We obtained mortality data from the Danish Civil Registration System. We computed mortality risks and hazard ratios with 95% confidence intervals (CIs) for gender, age, and comorbidity groups.
Results
We identified 3,727 patients (53.6% women) with a median age of 63 years for women and 60 years for men. The overall 6-month mortality rate was 12.8%. The adjusted hazard ratio was 2.77 (95% CI, 2.11–3.64) for patients aged 65–80 years and 5.25 (95% CI, 4.06–6.80) for patients older than 80 years, compared with patients younger than 65 years. The adjusted hazard ratio was 2.43 (95% CI, 1.82–3.24) and 3.87 (95% CI, 2.91–5.15) for patients with moderate and high comorbidity, respectively, compared with low comorbidity.
Conclusion
Age and comorbidity were important predictors of mortality after acute medical admission.
Introduction
The aging population and the increasing prevalence of chronic conditions present major public health challenges.Citation1,Citation2 The western population aged 65 years and older is projected to increase from approximately 15% in 2010 to 25% by 2040.Citation1,Citation3 The most rapid growth will occur in age groups older than 80 years.Citation1 Approximately 45% of the general population and 88% of the population older than 65 years have at least one chronic disease.Citation2 The vast majority of western health-care expenditures are already related to treatment of chronic conditions.Citation4 The increasing proportion of elderly people is expected to increase the general need for hospitalization.Citation2 Moreover, these hospitalizations will involve patients with comorbidities along with their primary admission condition. Thus, the future burden of comorbidity requiring medical attention will further increase health-care expenditures.Citation1,Citation2
Identifying prognostic factors for acute medical diseases is essential in the planning of health-care needs, evaluation of effectiveness of hospital care, and prevention of posthospital death. Previous studies of acute medical patients’ prognoses have focused entirely on the index condition.Citation5 Therefore, we conducted a feasibility study to examine the 6-month mortality following acute medical admission in Denmark and whether it was associated with gender, age, or comorbidity level. Furthermore, we aimed at describing the potential of the present study design for prognostic research on patients who were admitted acutely to internal medical departments.
Methods
Setting
We conducted this population-based cohort study in the Aarhus city area (population, 300,000) using data from Danish National Registries. The Danish National Health Service provides universal tax-supported health care, guaranteeing unfettered access to general practitioners and hospitals, and partial reimbursement for prescribed medications. Unambiguous linkage between all Danish registries is possible using the unique 10-digit central personal registry number assigned to each Danish citizen at birth and to residents upon immigration.Citation6
Patients
The Danish National Patient Registry (DNPR) covers all Danish hospitals and contains data on the admitting departments, admission priorities, dates of admission and discharge, and all primary and secondary discharge diagnoses from nonpsychiatric hospitals since 1977 and from emergency room and outpatient clinic visits since 1995.Citation7 Each discharge is associated with 1 primary diagnosis and 1 or more secondary diagnoses classified according to the International Classification of Diseases, Eighth Revision (ICD-8) until the end of 1993 and, thereafter, International Classification of Diseases, Tenth Revision (ICD-10).Citation7 We were interested in identifying medical patients only, distinct from surgical or psychiatric patients. All patients admitted to a medical admission unit (MAU) in Denmark are registered with a unique department code at the time of arrival, independently of later transfers to other departments. Using the DNPR, we identified patients with a first-ever acute admission to the MAU at Aarhus University Hospital, Nørrebrogade (code: 7003.071), between January 1, 2008, and December 31, 2008. This unit provides acute medical care for half of the Aarhus city population. The residence address determines to which hospital patients are referred. Codes for admission priorities registered independently in the DNPR confirmed that all patients identified were admitted acutely (code: ATA1). We defined the primary admission condition as the index condition and the date of admission as the index date. Per protocol, we excluded patients with a pregnancy-related index condition (n = 0), patients younger than 18 years (n = 83), and patients with missing records of vital statistics (primarily non-Danish citizens; n = 23). All types of medical patients are admitted to the MAU except patients with acute myocardial infarction or stroke, who are directly admitted to specialized departments. Patient admissions last until transfer to another hospital department, discharge, or in-hospital death.
Mortality
We obtained all-cause mortality from the Danish Civil Registration System.Citation8 This registry is updated daily and contains vital statistics – including date of birth, change of address, date of emigration, and exact date of death – on the Danish population since 1968.Citation8
Comorbidity
We searched the DNPR for inpatient and outpatient diagnoses for patient comorbidities before the index date.Citation9 We categorized patients’ comorbidity burden using Charlson comorbidity index (CCI).Citation10 The CCI is a validated method of classifying comorbidity to predict short-term and long-term mortality taking into consideration both the number and seriousness of diseases.Citation11–Citation13 In the CCI, a number of conditions are assigned weights of 1, 2, 3, or 6. The weights are allocated as follows: 1 – myocardial infarction, congestive heart failure, peripheral vascular disease, stroke, dementia, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease, or diabetes mellitus; 2 – hemiplegia, moderate or severe renal disease, diabetes with complications, any tumor, leukemia, or lymphoma; 3 – moderate to severe liver disease; 6 – metastatic solid tumor or AIDS. The Charlson index score is the total of the assigned weights, and thus represents a measure of the overall comorbidity burden.Citation10 Three levels of comorbidity were defined based on Charlson index scores of 0 (low), 1–2 (moderate), and 3 or more (high).Citation14 The ICD codes for each of the conditions included in the CCI are provided in the Appendix.
Statistical analysis
We characterized the patients according to gender, age, comorbidity, and index condition. Patients were followed from index date until the date of death, emigration, or completion of 6 months of follow-up, whichever came first.
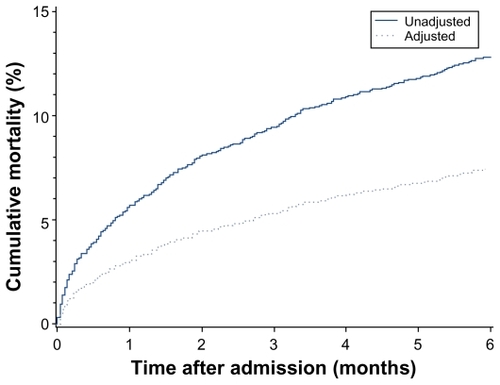
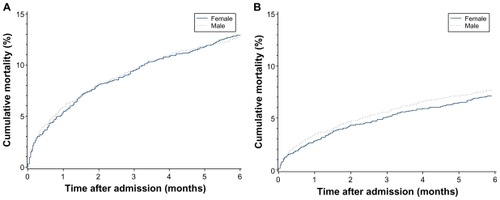
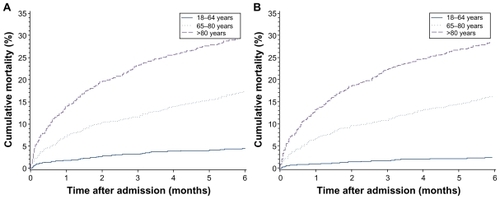
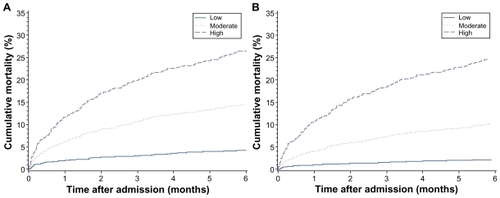
Using the Kaplan–Meier estimator, we plotted a 6-month overall mortality curve and calculated the cumulative 1-, 3-, and 6-month mortality risks, overall and stratified on gender, age, and comorbidity groups. The covariates eligible for inclusion in the model as potential confounders were gender, age as a continuous variable, and comorbidity level. Using the average covariate method,Citation15 we adjusted the mortality curves for these covariates.
Using Cox proportional hazards regression model, we calculated mortality hazard ratios (HRs) with 95% confidence intervals (CIs) comparing mortality rates within gender, age, and comorbidity groups. For each group, the category with the lowest mortality rate was set as reference, ie, female gender, age 18–64 years, and low comorbidity level, respectively. To examine any interaction between covariates, we performed stratified analyses on all 3 covariates. In the overall analysis, we adjusted for the other 2 covariates. In the stratified analysis, we adjusted for the remaining covariate only, except within age strata where additional adjustment for age as a continuous variable was made to reduce residual confounding. Analyses were performed using Statistical Analysis System (SAS) version 9.2 (SAS Institute Inc, Cary, North Carolina, USA).
Results
Patient characteristics
We identified 3,727 adult patients with a first-ever acute hospital admission during 2008 to the MAU at Aarhus University Hospital, Nørrebrogade. Patient characteristics are presented in . Slightly more than half of these patients were female (53.6%). At index date, 2,045 (54.9%) patients were younger than 65 years, 886 (23.8%) were aged between 65 and 80 years, and 796 (21.4%) were older than 80 years. The female patients were slightly older (median age, 63 years) than the male patients (median age, 60 years). The comorbidity level was low for 1,624 (43.6%) patients, moderate for 1,241 (33.3%) patients, and high for 862 (23.1%) patients. The frequency and proportion of index conditions according to major ICD-10 groups are presented in and . A surprisingly large proportion (17.9%) of the admitting causes were, rather imprecisely, coded as “factors influencing health status and contact with health services” (Z00–Z99), of which 84.9% were “medical observation and evaluation for suspected diseases and conditions” (Z03). The most frequent single cause of admission to the MAU was disease of the respiratory system.
Figure 1 Relative frequency of primary admission conditions according to major ICD-10 groups (corresponding disease categories are shown in ).
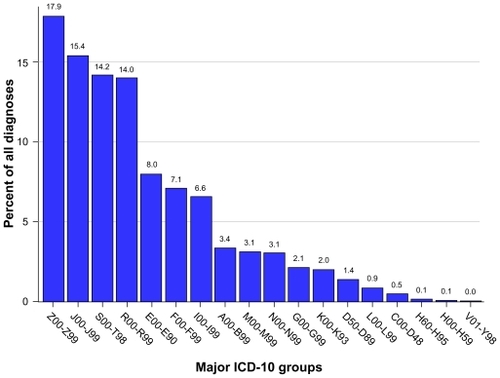
Table 1 Characteristics of patients with a first-ever admission to the medical admission unit at Aarhus University Hospital, Nørrebrogade, during 2008
Table 2 Frequency and proportion of primary admission conditions according to major ICD-10 groups
Cumulative mortality
The cumulative mortalities are presented in and –. The overall unadjusted mortality was 5.7% after 1 month, 9.5% after 3 months, and 12.8% after 6 months (). Men had a slightly higher adjusted mortality compared with women (). Patients younger than 65 years had a lower 1-, 3-, and 6-month adjusted mortality (0.9%, 1.6%, and 2.3%, respectively) compared with those aged 65–80 years (6.8%, 10.7%, and 16.1%, respectively) and with those older than 80 years (13.2%, 22.3%, and 28.4%, respectively). Similarly, patients with a low comorbidity level had a reduced 1-, 3-, and 6-month adjusted mortality (1.0%, 1.5%, and 2.1%, respectively) compared with those with moderate comorbidity level (4.2%, 7.2%, and 10.1%, respectively) and with those with high comorbidity level (10.8%, 18.6%, and 24.8%, respectively).
Table 3 Cumulative mortality risk after 1, 3, and 6 months, overall and according to gender, age, and comorbidity groups
Relative mortality
The results from the Cox regression analysis are presented in and . The overall adjusted HR comparing males with females was 1.16 (95% CI, 0.97–1.39). Compared with patients younger than 65 years, the adjusted HR was 2.77 (95% CI, 2.11–3.64) for patients aged 65–80 years and 5.25 (95% CI, 4.06–6.80) for patients older than 80 years. The impact of increasing age on the mortality HR was most evident among patients with low comorbidity. Compared with low comorbidity patients, the adjusted HR was 2.43 (95% CI, 1.82–3.24) for patients with a moderate comorbidity and 3.87 (95% CI, 2.91–5.15) for patients with a high comorbidity. The impact of comorbidity level on the mortality HR was most evident in the youngest group of patients.
Table 4 Mortality hazard ratios within gender, age, and comorbidity groups
Table 5 Mortality hazard ratios stratified on gender, age, and comorbidity groups
Discussion
In this population-based cohort study, age and comorbidity level were important predictors of 1-, 3-, and 6-month mortality following acute admission to the MAU at Aarhus University Hospital, Nørrebrogade. Furthermore, age and comorbidity seemed to modify the effect of each other. Thus, the prognostic effect of comorbidity level decreased with increasing age, and vice versa. Thus, a high comorbidity level increases mortality rates relatively more in young patients than old patients, which may be due to the fact that old age itself increases mortality rates substantially. Although not substantial, male gender may also be a predictor of mortality.
This feasibility study is the first to examine the 6-month mortality after acute admission to a MAU in a Scandinavian population-based setting. The design presented has not previously been described in Denmark for patients admitted to a MAU and may therefore be used in future studies on the prevalence and course of acute medical diseases and on prognostic factors for different outcomes of interest.
Comorbidity was a major prognostic factor in our study. Because the population is aging, it is expected that an increasing proportion of acutely hospitalized medical patients will present with more comorbidity in the future.Citation2 It is therefore important to identify prognostic comorbid conditions associated with acute medical diseases to plan health-care needs, evaluate effectiveness of hospital care, and prevent posthospital death. To examine whether comorbid diseases and index conditions interact with one another to increase mortality (beyond their independent effects alone), future studies should include a comparison cohort from the general population matched on gender and age and calculate the comorbidity level for members of this comparison cohort also.
Several issues should be considered when interpreting our results. Our population-based design within a tax-supported universal health-care system with complete, independently and prospectively recorded medical history reduced the risk of referral, diagnostic, and information biases.Citation16
The department registration procedure in the DNPR made it possible to identify hospital admissions for acute medical conditionsCitation17 as well as all in-hospital mortality. A limitation was that we were not able to include patients with acute myocardial infarction or stroke. The fact that 1 in 6 index conditions were imprecisely coded as “medical observation and evaluation for suspected diseases and conditions” does not affect the present study but suggest that some index conditions are underreported in the DNPR.
It is possible that confounding by unmeasured variables, such as former or current use of tobacco, alcohol, and medications, and biochemical markers, influenced our results. Future studies should, if possible, include such variablesCitation18,Citation19 and furthermore differentiate between index conditions because risk factors, prognostic factors, and survival probabilities vary among these conditions. Comparing mortality following acute medical conditions for different time periods may also add evidence on the effectiveness of newer treatment regimens. Moreover, comparing whether short-term or long-term mortality depends on the admission time during the day and week may challenge the internal organization of health-care systems. Other important outcome measures include length of stay, hospital acquired infections, venous thromboembolism, readmission rates, cause-specific mortality, and in-hospital mortality.
In conclusion, age and comorbidity were important predictors of mortality after acute medical admission.
Disclosure
The authors report no conflicts of interest in this work.
References
- GavrilovLAHeuvelinePDemenyPMcNicollGAging of populationThe Encyclopedia of PopulationNew YorkMacmillan Reference USA2003
- WolffJLStarfieldBAndersonGPrevalence, expenditures, and complications of multiple chronic conditions in the elderlyArch Intern Med2002162202269227612418941
- Statistics Denmark www.dst.dk
- HoffmanCRiceDSungHYPersons with chronic conditions. Their prevalence and costsJAMA199627618147314798903258
- VaartjesIde BorstGJReitsmaJBLong-term survival after initial hospital admission for peripheral arterial disease in the lower extremitiesBMC Cardiovasc Disord200994319715567
- FrankLEpidemiology. When an entire country is a cohortScience200028754622398239910766613
- AndersenTFMadsenMJorgensenJMellemkjaerLOlsenJHThe Danish National Hospital Register. A valuable source of data for modern health sciencesDan Med Bull199946326326810421985
- PedersenCBGøtzscheHMøllerJOMortensenPBThe Danish Civil Registration System. A cohort of eight million personsDan Med Bull200653444144917150149
- SørensenHTChristensenSMehnertFUse of bisphosphonates among women and risk of atrial fibrillation and flutter: population based case-control studyBMJ2008336764881381618334527
- CharlsonMEPompeiPAlesKlMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- de GrootVBeckermanHLankhorstGJBouterLMHow to measure comorbidity. A critical review of available methodsJ Clin Epidemiol200356322122912725876
- DeyoRACherkinDCCiolMAAdapting a clinical comorbidity index for use with ICD-9-CM administrative databasesJ Clin Epidemiol19924566136191607900
- D’HooreWBouckaertATilquinCPractical considerations on the use of the Charlson comorbidity index with administrative data basesJ Clin Epidemiol19964912142914338991959
- TahaASMcCloskeyCPrasadRBezlyakVFamotidine for the prevention of peptic ulcers and oesophagitis in patients taking low-dose aspirin (FAMOUS): a phase III, randomised, double-blind, placebo- controlled trialLancet2009374968411912519577798
- NietoFJCoreshJAdjusting survival curves for confounders: a review and a new methodAm J Epidemiol199614310105910688629613
- SørensenHTRegional administrative health registers as a resource in clinical epidemiology. A study of options, strengths, limitations and data quality provided with examples of useInt J Risk Safety Med199710122
- WeissNSRothmanKJGreenlandSLashTLClinical epidemiologyModern Epidemiology3rd edPhiladelphia, PALippincott Williams and Wilkins2008642646
- ChristiansenJUMaruardCDNielsenHCLABKA. A real-time computer system for the clinical laboratoryScand J Clin Lab Invest Suppl198919457612772556
- GaistDAndersenMAarupAlHallasJGramLFUse of sumatriptan in Denmark in 1994–5: an epidemiological analysis of nationwide prescription dataBr J Clin Pharmacol19974344294339146856
Appendix ICD codes for Charlson comorbidity index
Myocardial infarction: ICD-8: 410; ICD-10: I21, I22, I23.
Congestive heart failure: ICD-8: 427.09, 427.10, 427.11, 427.19, 428.99, 782.49; ICD-10: I50, I11.0, I13.0, I13.2.
Peripheral vascular disease: ICD-8: 440, 441, 442, 443, 444, 445; ICD-10: I70, I71, I72, I73, I74, I77.
Cerebrovascular disease: ICD-8: 430–438; ICD-10: I60–I69, G45, G46.
Dementia: ICD-8: 290.09–290.19, 293.09; ICD-10: F00– F03, F05.1, G30.
Chronic pulmonary disease: ICD-8: 490–493, 515–518; ICD-10: J40–J47, J60–J67, J68.4, J70.1, J70.3, J84.1, J92.0, J96.1, J98.2, J98.3.
Connective tissue disease: ICD-8: 712, 716, 734, 446, 135.99; ICD-10: M05, M06, M08, M09, M30, M31, M32, M33, M34, M35, M36, D86.
Ulcer disease: ICD-8: 530.91, 530.98, 531–534; ICD-10: K22.1, K25–K28.
Mild liver disease: ICD-8: 571, 573.01, 573.04; ICD-10: B18, K70.0–K70.3, K70.9, K71, K73, K74, K76.0.
Diabetes mellitus: ICD-8: 249.00, 249.06, 249.07, 249.09, 250.00, 250.06, 250.07, 250.09; ICD-10: E10.0, E10.1, E10.9, E11.0, E11.1, E11.9.
Hemiplegia: ICD-8: 344; ICD-10: G81, G82.
Moderate to severe renal disease: ICD-8: 403, 404, 580–583, 584, 590.09, 593.19, 753.10–753.19, 792; ICD-10: I12, I13, N00–N05, N07, N11, N14, N17–N19, Q61.
Diabetes with end-organ damage: ICD-8: 249.01–249.05, 249.08, 250.01–250.05, 250.08; ICD-10: E10.2–E10.8, E11.2–E11.8.
Any tumor: ICD-8: 140–194; ICD-10: C00–C75.
Leukemia: ICD-8: 204–207; ICD-10: C91–C95.
Lymphoma: ICD-8: 200–203, 275.59; ICD-10: C81–C85, C88, C90, C96.
Moderate to severe liver disease: ICD-8: 070.00, 070.02, 070.04, 070.06, 070.08, 573.00, 456.00–456.09; ICD-10: B15.0, B16.0, B16.2, B19.0, K70.4, K72, K76.6, I85; Metastatic solid tumor: ICD-8: 195–198, 199; ICD-10: C76–C80.
AIDS: ICD-8: 079.83; ICD-10: B21–B24.