Abstract
Background
Acetaminophen (APAP) is frequently used for analgesia and is considered safer than nonsteroidal anti-inflammatory drugs (NSAIDs) for the kidneys. However, there is little epidemiological evidence of the association between APAP and acute kidney injury (AKI).
Objectives
To examine the association between APAP and AKI using the self-controlled case series (SCCS) method, which is a novel strategy to control between-person confounders by comparing the risk and reference periods in each patient.
Methods
We performed SCCS in 1,871 patients (39.9% female) who were administered APAP and subsequently developed AKI, by reviewing electronically stored hospital information system data from May 2011 to July 2016. We used conditional Poisson regression to compare each patient’s risk and reference period. As a time-varying confounder, we adjusted the status of liver and kidney functions, systemic inflammation, and exposure to NSAIDs.
Results
We identified 5,650 AKI events during the 260,549 person-day observation period. The unadjusted incidences during the reference and exposure periods were 2.01/100 and 3.12/100 person-days, respectively. The incidence rate ratio adjusted with SCCS was 1.03 (95% confidence interval [CI]: 0.95–1.12). When we restricted endpoints as stage 2 AKI- and stage 3 AKI-level creatinine elevations, the incidence rate ratios were 1.20 (95% CI 0.91–1.58) and 1.20 (95% CI 0.62–2.31), respectively, neither of which was statistically significant.
Conclusion
Our findings added epidemiological information for the relationship between APAP administration and AKI development. The results indicated scarce association between APAP and AKI, presumably supporting the general physicians’ impression that APAP is safer for kidney.
Introduction
Acetaminophen (N-acetyl-para-amino-phenol [APAP]) is a frequently used pain killer. APAP is generally regarded as a safer drug with regard to kidney function compared to nonsteroidal anti-inflammatory drugs (NSAIDs), which are known to contribute to the development of acute kidney injury (AKI).Citation1 However, little is known about the association between APAP and AKI, especially for therapeutic dosing.
Previous case reportsCitation2–Citation4 and cohort studiesCitation5,Citation6 have suggested an association between supratherapeutic doses of APAP and AKI. To our knowledge, there is only one case seriesCitation7 that reported two AKI cases suspiciously induced by therapeutic-dose APAP. The causality in those cases remains unclear because the patients had taken other suspicious drugs in addition to APAP, and the drug-induced lymphocyte stimulation tests, which examined their hypersensitivity to APAP, were negative.Citation7 Looking at in vitro data, APAP in therapeutic doses is said to induce fibroblast proliferation, possibly resulting in kidney injury, but its clinical implications have not yet been proven.Citation8 Although there is quite limited epidemiological evidence for the association between therapeutic-dose APAP and AKI, guidelines,Citation9,Citation10 textbook,Citation11 and even the National Kidney Foundation web pageCitation12 describes its safer profile for the kidney, which is widely known among physicians.Citation13 In contrast, an official medical package leaflet published in JapanCitation14 stated that APAP is contraindicated in patients with severe renal impairment in order to prevent further renal damage, but no evidence has been shown to reinforce this contraindication.
Therefore, we believe that it is important to investigate any association between therapeutic dose APAP and AKI, to enhance better decision making for pain management. However, APAP is so widely usedCitation13 that demographic variance of the target population is too large; many between-person confounding factors would exist if we intended to perform conventional retrospective methods. Hence, a contrivance in study design is required.
In this study, we aimed to demonstrate the possible association between the administration of therapeutic doses of APAP and the occurrence of AKI, using a recently introduced, retrospective, observational design named self-controlled case series (SCCS). As a model, SCCS can easily control for potential between-person confounding factors that do not change over time by comparing risk and reference periods within each individual.Citation15,Citation16
Methods
Study design and settings
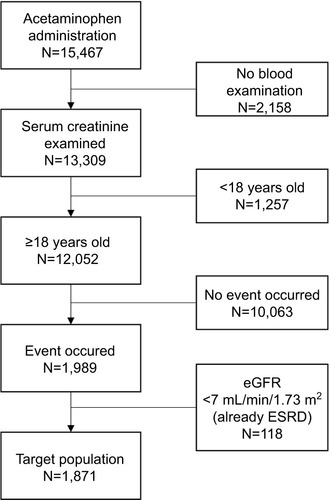
This is an SCCS study using drug prescription and biochemical blood test data obtained from the hospital information system (HIS) of a single facility. SCCS is a kind of case-series method developed recently.Citation15,Citation16 The method compares incident rates during time periods with different risk statuses within each individual in order to estimate the incident rate ratio of risk factors.Citation17 SCCS can therefore avoid time-independent confounding factors occurring between study subjects by comparing “risk” and “reference” periods within individuals; thus, there is no need for a separate control group. This feature makes it easier to examine drug adverse events retrospectively using HIS, in which a suitable control group is difficult to find.Citation18 The pictorial representation of the design is shown in .
Figure 1 Pictorial representation of SCCS we used in our context of interest.
Abbreviations: AKI, acute kidney injury; NSAIDs, nonsteroidal anti-inflammatory drugs; SCCS, self-controlled case series.
We identified people who were prescribed oral APAP from May 2011 to July 2016, by searching the HIS database of Kyoto University Hospital. The hospital is a tertiary general hospital with 34 divisions including internal medicine, surgery, emergency department, and psychiatry that take care of both the acute and chronic conditions of various diseases. The database covers all the patients who have ever consulted doctors working in the hospital. Its prescription database includes all outpatient and inpatient prescriptions in the hospital but does not include those written outside the hospital (eg, by general practitioners). From these potentially eligible patients, we excluded patients younger than 18 years at the beginning of the observation period, because our research scope was adult patients. In addition, we excluded patients on chronic dialysis therapy who would no longer be burdened by the initiation of renal replacement therapy (RRT). Similar to the prescription, our database does not include any treatment outside the hospital, such as at dialysis facilities. Furthermore, because acute blood purification in the hospital is recorded using paper documents, we could not extract the exact day of RRT. Therefore, we excluded patients whose estimated glomerular filtration rate (eGFR) value at the beginning of the observation was <7 mL/min/1.73 m2, as calculated with MDRD formula for the Japanese population, because patients with an eGFR <7 mL/min/1.73 m2 can be seen as end-stage renal disease (ESRD) patients.Citation19
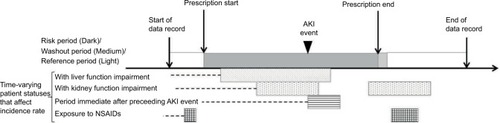
The inclusion flow diagram is shown in . This study was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine (R0290). The Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan, on which committee approval is based, advised consent from patients was not required because we secondarily used existing patient data collected for clinical purpose. Patient recruitment was done with an adequately managed opt-out method, as required in aforementioned guideline: we disclosed documents showing their right to decline participation to patients. Personal information was handled using secure computers in accordance with the Guideline on the Personal Information Protection Law in Japan.
Exposure and risk period
We defined our exposure group as those patients who were administered APAP, as identified by data extracted from the HIS of Kyoto University Hospital in the aforementioned period. We used the Japanese drug code specific to oral APAP, which is identical to the Anatomical Therapeutic Chemical (ATC) Classification of D00217, in our database search queries. A risk period in SCCS (“exposed period” in this study) is a period during which the individuals are biologically considered to be at risk of the drug’s adverse event of interest. We define the risk period here by the calendar days of APAP administration. If a patient was instructed to take APAP regularly, the corresponding days were considered to be the exposed period, assuming that all patients took all drugs when prescribed. If a patient was prescribed APAP to be taken on an as-needed basis, we assumed that he/she took the medication regularly three times a day and the corresponding periods were seen as the exposed period.
Endpoints and event measures
The primary endpoint was the occurrence of an AKI event. An AKI event was defined as serum creatinine elevation by ≥0.3 mg/dL in 2 days or ≥1.5 times in 7 days compared to the result of the most recent examination. These criteria were based on the definition of stage 1 AKI by the Kidney Disease Improving Global Outcomes Foundation.Citation20 Therefore, in this study, we included only periods in which the patients received blood examinations at least twice in 7 days, based on our method of defining AKI. The onset date of AKI was determined by laboratory data that satisfied the aforementioned criteria. Our blood examination database includes examination date and result but not the exact time when the blood specimen was collected. In a precise sense, KDIGO defines stage 1 AKI as a serum creatinine elevation by ≥0.3 mg/dL in 48 h; however, in this study, we used two calendar days instead of 48 h because of the aforementioned limitation of data granularity.
We also examined the incidence of advanced AKI events as endpoints. Stage 2 AKI (defined as serum creatinine elevation of greater than or equal to twice the baseline level) and stage 3 AKI-level creatinine elevation (≥4.0 mg/dL, or greater than or equal to three times the baseline level) were selected. As mentioned earlier, we could not extract the exact date of RRT, hence we applied creatinine elevation condition only as a definition of severer AKI equivalent to stage 3 AKI.
Washout period
Serum creatinine, which is the key value defining AKI, is reported to elevate 24 and 48 h after kidney damage.Citation21 In addition, little is known about the lead time between APAP administration and the onset of kidney injury. Therefore, an AKI event could be detected shortly after the cessation of APAP exposure. In this study, we treated two calendar days after the cessation as a washout period, which had a different risk structure than the control period. We also modified the assumption for the length of the washout period with the sensitivity analysis described later.
Adjustment of time-varying confounders
As discussed earlier, SCCS can avoid between-person con-founders that do not change over time, but we had to adjust time-varying variables that correlate to both the exposure and the occurrence of the event. shows the causal diagram of our context of interest. We identified several time-varying confounders: liver function impairment, kidney function impairment, systemic inflammation, and NSAIDs use. In addition, we adjusted the effect of AKI occurrence itself on subsequent events.
Figure 3 Causal diagram of our context of interest.
Abbreviations: AKI, acute kidney injury; ALP, alkaline phosphatase; ALT, alanine aminotransferase; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; NSAIDs, nonsteroidal anti-inflammatory drugs; ULN, upper limits of normal.
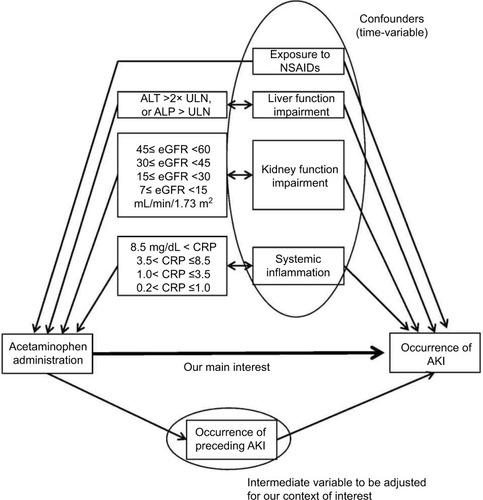
Liver function impairment
APAP has been shown to induce renal damage in patients with impaired liver function.Citation5 In addition, physicians may hesitate to prescribe APAP for patients with impaired liver function, due to its well-known hepatotoxicity. Therefore, liver function acts as a confounding factor that needs to be adjusted. We defined liver function impairment as the elevation of serum alanine aminotransferase to levels of more than double the upper limits of normal (ULN), or the elevation of alkaline phosphatase above its ULN, referring to the criteria of drug-induced liver injury.Citation22 We assumed liver function impairment to be transient and to occur independently of the kidney injury.
Kidney function impairment
Kidney function declines gradually over time,Citation23 and impaired kidney function is revealed to be the risk factor of AKI development.Citation24,Citation25 In addition, patients with impaired kidney function are more likely to be prescribed APAP,Citation26 adhering to the recommendation of guidelinesCitation27 and others discussed earlier.Citation9–Citation12 Therefore, kidney function is also a time-varying confounder to be adjusted. In this study, we defined kidney function impairment to be an eGFR value of <60 mL/min/1.73 m2 and subdivided them into four strata (45≤ eGFR <60 mL/min/1.73 m2, 30≤ eGFR <45 mL/min/1.73 m2, 15≤ eGFR <30 mL/min/1.73 m2, and 7≤ eGFR <15 mL/ min/1.73 m2).Citation28
Systemic inflammation
AKI occurs in 22.7% of hospitalized patients, especially those in a severely ill condition.Citation29,Citation30 Clinically ill conditions are generally transient and such patients tend to need APAP as analgesic agents, hence, the general condition of the patient is a time-variable confounder. As an indicator of the patients’ general condition, we used C-reactive protein (CRP) to represent the status of systemic inflammation. We assumed that a CRP value of >0.2 mg/dL indicated systemic inflammation because this value is the threshold in the Kyoto University Hospital laboratory. In addition, we subdivided systemic inflammation status into four strata, decided by the 50th, 75th, and 90th percentiles of the analyzed period sorted by the CRP value (0.2< CRP ≤1.0 mg/dL, 1.0< CRP ≤3.5 mg/dL, 3.5< CRP ≤8.5 mg/dL, and 8.5 mg/dL < CRP).
We assumed that aforementioned impaired liver and kidney functions and systemic inflammation status start at the point of the middle day in the blood examination interval. For example, when a patient satisfied impaired liver function criteria at the examination on May 5, while he/she did not satisfy the criteria at the examination just before on May 1, we assumed that his/her impaired liver function started at May 3.
NSAIDs’ use
As discussed earlier, NSAIDs is well known to cause AKI. Both NSAIDs and APAP are analgesics; thus, a correlation in their administration may exist due to background conditions. Therefore, we treated NSAIDs’ administration as a confounding factor. We used the Japanese drug code equivalent to the ATC drug code of M01AB, M01AC, M01AE, M01AG, and M01AH to determine the NSAIDs used. Similar to APAP administration, we defined a 2-day washout period.
Occurrence of AKI
We intended to examine the direct effect of APAP administration on AKI events, but the occurrence of AKI increases the incidence rate of subsequent AKI.Citation31 This means that an AKI event acted as an intermediate variable in our causal model. To the best of our knowledge, there is no firm knowledge about how long the preceding AKI affects the following ones. Therefore, we assumed a 7-day period after AKI (hereafter called the preceding AKI-affected period), to adjust for the effect of one AKI event on subsequent ones,Citation2 as shown in .
Sensitivity analysis
To confirm our results, we performed sensitivity analyses. First, we stratified patients by their gender. Next, we modified these assumptions in our analysis: the preceding AKI- affected period (1, 3, and 14 days) and washout period for APAP administration (1, 7, and 14 days).
We also calculated the incidence rate ratio of APAP administration with the model including potentially nephrotoxic agents known to cause kidney damage. These drugs could be associated with the development of AKI, but administration of these drugs, except NSAIDs, does not directly correlate to that of APAP because of the difference in their effects. Therefore, they do not necessarily act as confounding factor. The list of drugs is shown in .Citation32
Statistical analysis
All analyses used R Version 3.2.1 software,Citation33 and the results are presented with 95% confidence intervals (CIs) when appropriate. We used conditional Poisson regression to compare each patient’s risk and reference periods with Generalized Nonlinear Models package.Citation34 A two-sided P-value of <0.05 was considered statistically significant.
Results
Patient characteristics in this study are shown in . We included 1,871 patients, and 39.9% of the target population was female. The average age at the beginning of the observation was 63.3 years, and the average observation length was 139 days. The average exposure period of APAP administration was 16 days. In our population, 48.6% of patients had eGFR values >60 mL/min/1.73 m2 at the time of first blood examination, while in 32.3% of patients, the eGFR was between 30 and 60 and, in 19.1% of patients, the eGFR was between 7 and 29. As explained earlier, patients whose eGFR value was <7 mL/min/1.73 m2 were excluded.
Table 1 Patient characteristics of included patients (n=1,871)
shows the unadjusted incidence of AKI stratified by the aforementioned factors and incidence rate ratios adjusted with SCCS. There were 5,650 AKI events (33.1% of them were first time AKI) that occurred during the 260,549 person-days of observation period. Among them, 4,584 AKI events occurred during 228,036 person-days of the unexposed to APAP period, while 939 events occurred during 30,053 person-days of the exposed period and 127 events did during 2,460 person-days of washout period. The adjusted incidence rate ratio of AKI under the condition of APAP administration was 1.03 (95% CI: 0.95–1.12), and that of the washout period was 1.05 (95% CI: 0.87–1.27). Among time-varying confounders, the incidence rate ratios of systemic inflammation, kidney function impairment, liver function impairment periods, and use of NSAIDs were statistically >1.0. In particular, during the exposure to NSAIDs, the incidence rate ratio was 1.27 (95% CI: 1.14–1.41). However, that of the periods immediately after the preceding AKI event did not show statistical significance.
Table 2 Unadjusted incidence and adjusted incidence rate ratio of AKI in periods with each risk status
shows the incidence rate ratios under the condition of defining endpoints as stage 2 AKI- and stage 3 AKI-level creatinine elevations. When we define stage 2 AKI as the endpoint, the number of AKI events was 545 and the number of patients that satisfied the inclusion criteria was 399. The incidence rate ratio of APAP administration was 1.20 (95% CI: 0.91–1.58). When we define stage 3 AKI-level creatinine elevation as the endpoint, 108 AKI events occurred in 91 patients. The incidence rate ratio was 1.20 (95% CI: 0.62–2.31).
Table 3 Incidence rate ratio of AKI under the condition of defining events – stage 2 and stage 3 AKI-level creatinine elevation
Finally, we performed sensitivity analyses, as shown in . When we stratified patients by gender, the incidence rate ratio of APAP administration was 1.03 (men) and 1.01 (women). When we modified the assumptions as to the preceding AKI-affected period and length of the washout period, the incidence rates were ~1.01–1.03 under all assumptions. When we added potentially nephrotoxic agents into the model, the estimated incidence rate ratio was 1.04.
Table 4 Incidence rate ratio of AKI with modified assumptions: result of sensitivity analysis
Discussion
We conducted a SCCS study to examine the potential association between APAP administration at therapeutic doses and the occurrence of AKI. Our results showed that the incidence rate of AKI, in the period that patients were prescribed APAP, was slightly higher than in the period in which they were not prescribed APAP, with the conditions of controlling for kidney function, liver function, severity of systemic inflammation, and exposure to NSAIDs as time-varying confounders. However, the difference was not statistically significant over the null hypothesis that APAP administration was not associated with the development of AKI.
The analgesic action of APAP is not fully understood, while its hepatotoxicity is well acknowledged.Citation35 Several researchers have indicated that cyclooxygenase-3 might be a target enzyme of APAP,Citation36,Citation37 while other in vivo data have suggested that another metabolite, named AM404, was the key factor in the mechanism of APAP as an analgesic agent.Citation38
There are several case reports reporting that an APAP overdose causes AKI.Citation2–Citation4 Previous reviews have suggested that renal insufficiency occurs in 1–2% of patients after an APAP overdose.Citation39 Another cohort study from Taiwan showed that the overall risk of developing AKI was about twice as high in patients with APAP intoxication,Citation6 discussing that AKI may be caused by N-acetyl-p-benzoquinoneimine (NAPQI), which is a toxic intermediate metabolite of APAPCitation40 produced in excess by the saturation of normal metabolic pathways in the liver. Hence, their results are difficult to apply to the effects of APAP at therapeutic doses.
So far, there are mixed opinions about the association between therapeutic dose APAP and AKI. To our knowledge, there is no observational study examining the association between them. In the present study, we utilized SCCS with the adjustment of time-varying confounders to extract reliable associations from an easily available HIS data, which contains prescription and blood examination results. APAP is a relatively inexpensive drug to compensate costly clinical research; therefore, we believed that it was important to pursue less costly but statistically validated methods.
SCCS was originally developed for evaluating association between vaccinations and their adverse effectsCitation15 and is now commonly used for the purpose.Citation41 Recently, researchers have investigated the associations between drug administration and some events by this method using existing electronically stored databases, with examples including antipsychotic drugs and myocardial infarctionCitation42 and thiazolidinediones and fracture.Citation43 One study investigated the association between antidepressants and hip fracture using both SCCS and conventional case–control method and concluded that SCCS could perform more accurately than case–control methods,Citation44 indicating that SCCS is potentially valuable for our research purposes.
Our main analysis secondarily showed that the incidence rates of AKI associated with systemic inflammation, kidney function, liver function, and NSAIDs’ use were significantly higher than reference. These results were compatible with previous reports, indicating that the analysis program for our SCCS model was properly developed. The effect of preceding AKI events did not show statistical significance in spite of existing knowledge, but this result can be explained by the variable’s correlation to kidney function impairment.
Our data showed that the incidence rate of AKI associated with APAP administration was 1.03 times higher than the reference and was 1.05 times higher in the washout period. Point estimates were slightly >1.0, but it did not show statistical significance. Not showing statistical significance does not directly mean the absence of a relationship between APAP and AKI, but considering the distribution of the 95% CI, it could be supposed to be scarce or ignorable. In contrast to the aforementioned case reportCitation7 and the in vitro dataCitation8 indicating that therapeutic dose APAP could cause AKI, our result was consistent with the well-known physicians’ impression. At least, considering a previous report,Citation1 which showed that the AKI risk with NSAIDs’ use is 60% higher than reference, and our present data showing the association of NSAIDs’ use with AKI, we could conclude that the clinical importance of the association between APAP use and AKI is weaker than that of NSAIDs.
When we set the event as advanced AKI events, the point estimates of the incidence rate ratios were higher than that of the base case model, but they also did not show statistical significance. Though the number of patients was small and CI became wider, the difference in the incidence rate of severer AKI, part of which can be seen as severe kidney injury as requiring RRT, associated with APAP administration, could be supposed to have little clinical importance.
From the sensitivity analyses, which modified assumptions in the base case model, we obtained almost similar incidence rate ratios, indicating the robustness of our findings. Including potentially nephrotoxic agents into our model also did not show apparent change in the results. This result may be explained by the little correlation between administration of APAP and these drugs. However, it must be considered that we included all drugs grouped together on account of the difficulty in data handling when including each drug separately into the model.
AKI can sometimes be a lethal condition,Citation45 and it is also well known that those who recovered from AKI can progress to chronic kidney disease,Citation46 which is a major risk factor for cardiovascular diseases. AKI can lower patients’ quality of life,Citation47,Citation48 and therefore, prevention of AKI is very important. From our results, the clinical importance of the association between APAP and AKI seems unremarkable, or at least smaller than that of NSAIDs and AKI. Considering the side effects of other pain-killing treatment options, using APAP is a reasonable choice when physicians intend to preserve patients’ kidney function.
Limitations
There were several limitations to our study. First, unobserved confounding factors may still exist, including both those arising from the limitations of the dataset and those having intrinsically uncontrollable features. For example, we could not include the major time-varying conditions, such as post-cardiac surgery state and sepsis, due to the limitation of our dataset, which could not sufficiently acquire the existence of such conditions. In addition, the indication for APAP administration may act as an intrinsically uncontrollable time-varying confounding factor. We cannot distinguish AKI caused by APAP from AKI due to a background poor clinical condition that resulted in APAP administration. As described in the “Methods” section, those time-varying factors that correlate to APAP administration and affect the risk of AKI development can result in the observed incidence rate ratios being larger or smaller than the real value. From the clinical viewpoint, such confounders generally increase the proportion of APAP administration and also increase the incidence of AKI because severe conditions require pain control and result in high incidence of AKI. Therefore, a calculated incidence rate ratio with only observed confounders, in which APAP administration period contains more patients with unobserved confounder increasing incidence rate, shows larger values than real incidence rate ratios. Considering that our main result already showed little association between APAP and AKI, this problem may have little impact on our result, even though the possibility of an unexpected effect still remained.
Second, we used a dataset from a single facility and, therefore, potential sampling bias may exist. Third, this study restricted observation periods to those periods in which patients received blood examinations at least once in 7 days. That is to say, our results cannot directly be applied to patients who do not need such frequent blood examinations. Last, we could not fully collect APAP administration (eg, taking over-the-counter drugs). This bias can lead to erroneous estimation of the incidence rate ratio, but its effect may be small. This is because Japanese health insurance covers APAP prescription for almost all diseases, so the target population could get an APAP prescription at lower cost than buying over-the-counter drugs.
Conclusion
Using prescription and biochemical blood test data from HIS, we performed SCCS to compare the incidence rate of AKI between periods in which patients were and were not exposed to therapeutic dose APAP. We found that the incidence was slightly higher during a period with APAP administration as a point estimate; however, the difference was not statistically significant. General physicians often recognize that APAP is relatively safe for the kidneys; however, it has not been demonstrated in epidemiological data. Even though it is not necessarily a statistically precise interpretation, our research epidemiologically added supporting information to the general physicians’ impressions.
Data sharing
It is difficult for authors to share data we used, because our data contain personal identifier, prescription data, and blood examination data, which Japanese legal regulation regards as sensitive personal information not to be freely disclosed.
Author contributions
SH and TT contributed to the research idea and study design. SH contributed to the data acquisition. SH and HY analyzed the data. KY and NK contributed to the statistical analysis. SH and HY contributed to the article writing. TM and HT contributed to the mentorship. MY and TK contributed to the supervision. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Dr Hideki Yokoi, for the valuable advice with regard to nephrology affairs. We gratefully acknowledge Ms Kaori Shiomi, Yoko Hara, and Yuko Furu-sawa for their secretarial assistance. We also would like to thank Editage (www.editage.jp) for English language editing. This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI grant number JP5549881 and Ministry of Health, Labor and Welfare Research grant number H29-Seisaku-Shitei-005.
Supplementary material
Table S1 The list of potentially nephrotoxic agents we used in sensitivity analysis
Disclosure
The authors report no conflicts of interest in this work.
References
- GriffinMRYaredARayWANonsteroidal antiinflammatory drugs and acute renal failure in elderly personsAm J Epidemiol2000151548849610707917
- MazerMPerroneJAcetaminophen-induced nephrotoxicity: pathophysiology, clinical manifestations, and managementJ Med Toxicol2008412618338302
- LohCPonampalamRNephrotoxicity associated with acute paracetamol overdose: a case report and review of the literatureHong Kong J2006132105110
- BlakelyPMcDonaldBRAcute renal failure due to acetaminophen ingestion: a case report and review of the literatureJ Am Soc Nephrol19956148537579069
- StollingsJLWheelerAPRiceTWIncidence and characterization of acute kidney injury after acetaminophen overdoseJ Crit Care20163519119427481758
- ChenYGLinCLDaiMSRisk of acute kidney injury and long-term outcome in patients with acetaminophen intoxication: a nationwide population-based retrospective cohort studyMedicine20159446e204026579812
- KatoHFujigakiYInoueRTherapeutic dose of acetaminophen as a possible risk factor for acute kidney injury: learning from two healthy young adult casesInt Med2014531415311534
- YuYLYiangGTChouPLDual role of acetaminophen in promoting hepatoma cell apoptosis and kidney fibroblast proliferationMol Med Rep2014962077208424682227
- ChouRQaseemASnowVDiagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain SocietyAnn Intern Med2007147747849117909209
- PhamPCKhaingKSieversTM2017 update on pain management in patients with chronic kidney diseaseClin Kidney J201710568869728979781
- DavisonSNCurhanGCManagement of Chronic Pain in Chronic Kidney DiseaseWaltham, MAUpToDate2017 Available from: https://www.uptodate.com/contents/management-of-chronic-pain-in-chronic-kidney-diseaseAccessed January 2, 2018
- NKF [webpage on the Internet]Pain Medicines (Analgesics)2017 Available from: https://www.kidney.org/atoz/content/painmeds_analgesicsAccessed December 23, 2017
- KaplowitzNAcetaminophen hepatoxicity: what do we know, what don’t we know, and what do we do next?Hepatology2004401232615239082
- Medical Package LeafletAcetaminophen Tab. 200mg “TEVA”2016 Available from: http://www.info.pmda.go.jp/downfiles/ph/PDF/400813_1141007F1179_1_03.pdfAccessed July 28, 2017
- FarringtonCPRelative incidence estimation from case series for vaccine safety evaluationBiometrics19955112282357766778
- WhitakerHJFarringtonCPSpiessensBMusondaPTutorial in biostatistics: the self-controlled case series methodStat Med200625101768179716220518
- LanganSMMinassianCSmeethLThomasSLRisk of stroke following herpes zoster: a self-controlled case-series studyClin Infect Dis201458111497150324700656
- PetersenIDouglasIWhitakerHSelf controlled case series methods: an alternative to standard epidemiological study designsBMJ2016354i451527618829
- CooperBABranleyPBulfoneLA randomized, controlled trial of early versus late initiation of dialysisN Engl J Med2010363760961920581422
- Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work GroupKDIGO Clinical Practice Guideline for Acute Kidney Injury. Summary of recommendation statementsKidney Int Suppl201221812
- McIlroyDRWagenerGLeeHTBiomarkers of acute kidney injury: an evolving domainAnesthesiology20101124998100420216399
- DananGBenichouCCausality assessment of adverse reactions to drugs – I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuriesJ Clin Epidemiol19934611132313308229110
- MitchWEWalserMBuffingtonGALemannJJrA simple method of estimating progression of chronic renal failureLancet1976279991326132863803
- ChawlaLSEggersPWStarRAKimmelPLAcute kidney injury and chronic kidney disease as interconnected syndromesN Engl J Med20143711586624988558
- Moo ParkKExperimental evidence that preexisting chronic kidney disease is a risk factor for acute kidney injuryKidney Res Clin Prac20143327172
- KelkarMClevesMAFosterHRHoganWRJamesLPMartinBCAcute and chronic acetaminophen use and renal disease: a case-control study using pharmacy and medical claimsJ Manag Care Pharm201218323424622468732
- HenrichWLAgodoaLEBarrettBAnalgesics and the kidney: summary and recommendations to the Scientific Advisory Board of the National Kidney Foundation from an Ad Hoc committee of the National Kidney FoundationAm J Kidney Dis19962711621658546133
- No authors listedChapter 1: definition and classification of CKDKidney Int Suppl2013311962
- WangHEMuntnerPChertowGMWarnockDGAcute kidney injury and mortality in hospitalized patientsAm J Nephrol201235434935522473149
- Cartin-CebaRKashiourisMPlatakiMKorDJGajicOCaseyETRisk factors for development of acute kidney injury in critically ill patients: a systematic review and meta-analysis of observational studiesCrit Care Res Prac20122012691013
- PazhayattilGSShiraliACDrug-induced impairment of renal functionInt J Nephrol Renovasc Dis2014745746825540591
- NaughtonCADrug-induced nephrotoxicityAm Fam Physician200878674375018819242
- R Foundation for Statistical Computing [homepage on the Internet]A language and environment for statistical computingR Foundation for Statistical Computing2015 Available from: https://www.R-project.org/Accessed January 3, 2018
- TurnerHFirthDGeneralized Nonlinear Models in R: An Overview of the gnm Package2015 Available from: http://CRAN.R-project.org/package=gnmAccessed January 3, 2018
- HinsonJARobertsDWJamesLPMechanisms of acetaminophen-induced liver necrosisHandb Exp Pharmacol2010196369405
- BottingRMMechanism of action of acetaminophen: is there a cyclooxygenase 3?Clin Infect Dis200031suppl 5S202S21011113024
- BottingRAyoubSSCOX-3 and the mechanism of action of paracetamol/acetaminophenProstaglandins Leukot Essent Fatty Acids2005722858715626590
- HogestattEDJonssonBAErmundAConversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous systemJ Biol Chem200528036314053141215987694
- PrescottLFParacetamol overdosage. Pharmacological considerations and clinical managementDrugs19832532903146343056
- da RochaBARitterAMAmesFQAcetaminophen-induced hepatotoxicity: preventive effect of trans anetholeBiomed Pharm201786213220
- WeldeselassieYGWhitakerHJFarringtonCPUse of the self-controlled case-series method in vaccine safety studies: review and recommendations for best practiceEpidemiol Infect2011139121805181721849099
- BrauerRSmeethLAnaya-IzquierdoKAntipsychotic drugs and risks of myocardial infarction: a self-controlled case series studyEur Heart J2015361698499225005706
- DouglasIJEvansSJPocockSSmeethLThe risk of fractures associated with thiazolidinediones: a self-controlled case-series studyPLoS Med200969e100015419787025
- HubbardRFarringtonPSmithCSmeethLTattersfieldAExposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fractureAm J Epidemiol20031581778412835289
- WaldRQuinnRRLuoJChronic dialysis and death among survivors of acute kidney injury requiring dialysisJAMA2009302111179118519755696
- PonteBFelipeCMurielATenorioMTLianoFLong-term functional evolution after an acute kidney injury: a 10-year studyNephrol Dial Transplant200823123859386618632586
- JamesMTGhaliWATonelliMAcute kidney injury following coronary angiography is associated with a long-term decline in kidney functionKidney Int201078880380920686453
- PerlmanRLFinkelsteinFOLiuLQuality of life in chronic kidney disease (CKD): a cross-sectional analysis in the Renal Research Institute-CKD studyAm J Kidney Dis200545465866615806468