?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background:
Most patients with moderate and severe chronic obstructive pulmonary disease (COPD) receive long-acting bronchodilators (LABA) for symptom control. It is, however, unclear if and what drug treatments should be added to LABAs to reduce exacerbations, which is an important goal of COPD management. Since current guidelines cannot make strong recommendations yet, our aim was to determine the relative efficacy of existing treatments and combinations to reduce the risk for COPD exacerbations.
Methods:
We included randomized clinical trials (RCTs) evaluating long-acting β2 agonists (LABA), long-acting muscarinic antagonists (LAMA), inhaled glucocorticosterioids (ICS), and the phosphodiesterase-4 (PDE4) inhibitor roflumilast, and combinations of these interventions in moderate to severe COPD populations. Our primary outcome was the event rate of exacerbations. We conducted a random-effects Bayesian mixed-treatment comparison (MTC) and applied several sensitivity analyses. In particular, we confirmed our findings using a binomial MTC analysis examining whether a patient experienced at least one exacerbation event or not during the trial. We also used an additive assumption to calculate the combined effects of treatments that were not included in the systematic review.
Results:
Twenty-six studies provided data on the total number of exacerbations and/or the mean annual rate of exacerbations among a combined 36,312 patients. There were a total of 10 treatment combinations in the MTC and 15 in the additive analysis. Compared with all other treatments, the combination of roflumilast plus LAMA exhibited the largest treatment effects, and had the highest probability (45%) of being the best first-line treatment. This was consistent whether applying the incidence rate analysis or the binomial analysis. When applying the additive assumption, most point estimates suggested that roflumilast may provide additional benefit by further reducing exacerbations.
Conclusions:
Using various meta-analytic approaches, our study demonstrates that depending on the choice of drug, combined treatments offer a therapeutic advantage.
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality throughout the world.Citation1 Predominantly caused by tobacco smoke, which causes the airways to narrow, COPD leads to a limitation of the flow of air to and from the lungs. This causes shortness of breath. COPD results in an important reduction in a patient’s quality of life and places patients at an increased risk for both pulmonary and nonpulmonary death.Citation2–Citation5
The course of COPD is characterized by exacerbations, whose frequency and severity determine much of the patients’ burden from COPD. Since exacerbations impact both on the quality of life of patients and on their prognosis an important goal of the COPD management is to prevent exacerbations or at least reduce their severity. Long-acting bronchodilators such as long-acting β2 agonists (LABA) and long-acting antimuscarinic drugs (LAMA) are central in the symptomatic management of COPD but they also prevent exacerbations by about 20%. Against a backbone of LABAs or LAMAs, the addition of inhaled corticosteroids (ICS) or, more recently, phosphodiesterase-4 (PDE4) inhibitors may provide additional protection, particularly in patients with an advanced disease state. PDE4 inhibitors provide a novel approach to the treatment of COPD. These drugs exhibit a wide range of anti-inflammatory actions. Roflumilast is the only available PDE4 inhibitor and reduces airway inflammation in COPD, as assessed with sputum neutrophil and eosinophil counts. Although six randomized trials of roflumilast have been completed,Citation6–Citation9 the relative effect of roflumilast in addition to established interventions is not well understood.
Previous meta-analysis have relied on head-to-head randomized trials to provide evidence of relative effectiveness.Citation10–Citation16 Head-to-head trials provide evidence when interventions have been simultaneously compared. Other approaches, including mixed-treatment comparisons, can provide evidence of relative effects when interventions have not been evaluated directly.Citation15,Citation16 Two mixed-treatment meta-analyses have examined the comparative effectiveness of interventions,Citation17,Citation18 but did not include roflumilast. There is also controversy about the application of meta-analysis of COPD exacerbation data as original trials may report outcomes heterogeneously.Citation19,Citation20 The controversy debates whether one should include exacerbations rates or a binomial event occurrence whereby a patient had at least one exacerbation during the course of a randomized, controlled trial (RCT) or not.
We aimed to determine the relative effectiveness of LABA, LAMA, PDE4 inhibitors, and ICS in various combinations for a specific and clinically important endpoint, ie, exacerbations. We conducted a multiple treatment meta-analysis and multiplicative analysis to determine the relative effectiveness of these interventions.
Methods
Analysis
To overcome the controversy of whether to apply rates or binomial events (ever had an event or not), we applied both analyses. Our primary analysis was based on rates and then confirmed using the binomial analysis reported as relative risks.
Eligibility criteria
We included any published randomized clinical trial evaluating patients with moderate to severe COPD as defined by the Global Initiative on Obstructive Lung Disease (GOLD) classification, in line with the American Thoracic Society and European Respiratory Society (ATS/ERS).Citation21 RCTs had to be of at least 24 weeks (6 months) duration. We considered any RCT evaluating the following therapeutic interventions: LABA (formoterol or salmeterol); LAMA (tiotropium); ICS (fluticasone or budesonide); PDE4 inhibitors (roflumilast); and combinations of these interventions. Control interventions included these active interventions or placebo. We excluded pharmacokinetic studies and proof of concept studies.
Primary outcome
The primary outcome of interest for this analysis was exacerbations rates reported in the original studies. An exacerbation is defined as “sustained worsening of the patient’s condition, from the stable state and beyond normal day-to-day variations, that is acute in onset and necessitates a change in regular medication in a patient with underlying COPD”.Citation22 Where reported, we extracted data on exacerbations as moderate and severe. Moderate is considered as “patient has an increased need for medication, and he/she feels the need to seek additional medical assistance” and severe as “patient/caregiver recognizes obvious and/or rapid deterioration in condition, requiring hospitalization”.Citation22 In a sensitivity analysis, we confirmed these findings using the binomial endpoint of a patient having had at least one exacerbation event during the course of the trial.
Search criteria
Independently, in duplicate, we searched the following electronic databases (from inception to September 2010): MedLine via PubMed; EMBASE; and Cochrane CENTRAL. We used the following terms for searching, including their MeSH terms: randomized controlled trial; controlled clinical trial; randomized; chronic obstructive pulmonary disease; long-acting beta agonist (LABA); formoterol; salmeterol; long-acting muscarinic antagonists (LAMA); tiotropium; inhaled corticosteroids (ICS); fluticasone; budesonide; and roflumilast. We searched the bibliographies of relevant previous publications. Studies were restricted to those published in English. Although we read the full manuscripts of any substudies or post-hoc evaluations, our primary analyses were based on the main published study trial reports.
Data abstraction
Two reviewers abstracted data in duplicate independently on the study characteristics, populations, and interventions. We extracted data on the primary outcome of interest, exacerbations, according to the primary definition used in each study. We extracted data on the number of exacerbations per patient arm and calculated total patient years at risk as reported in the article, or if unavailable, by the intention to treat principal by multiplying the number of participants by the planned study duration. For the binomial evaluation of rates, we extracted data on the number of patients having had at least one exacerbation in each arm over the course of the trial, regardless of how many additional exacerbations patients may have experienced.
Statistical analyses
We plotted the geometric distribution of the included trials with circles representing the interventions and lines denoting the number of trials between interventions.Citation23 We used a mixed-treatment comparison (MTC) meta-analysis framework to analyze the data provided by the studies included in our systematic review and compare the different treatment regimens with respect to the outcomes of interest.Citation24 This framework is suitable for meta-analytic situations where we wish to assess the relative effects of pairs of treatments based on direct and indirect evidence provided by randomized clinical trials,Citation24 thereby providing a generalization of meta-analysis methods because it allows comparisons of agents not addressed within any of the individual primary trials. One of the advantages of this framework, from a medical decision-making viewpoint is that, when conducted in a Bayesian setting, it affords the estimation of the probability of each treatment being the best with respect to the outcome of interest. Another advantage is that this framework can accommodate study-level covariates in order to determine to what degree these covariates may help explain potential heterogeneity in the relative effects of pairs of treatments over and above that explained by chance and helps reduce the inconsistency in the network of treatments.Citation25
Each of the studies contributed the following data to the MTC analyses conducted in this paper: i) the total number of exacerbations in COPD experienced in each treatment arm, ii) the total number of patient-years at risk per treatment arm, and iii) the total number of patients experiencing at least one exacerbation event. In order to reflect the fact that individual patients could experience multiple exacerbations in COPD over the duration of follow-up and that different trials had different durations of follow-up, we chose to model the expected rates of exacerbations in COPD per person-years. This enabled us to express the relative effects of pairs of treatments in terms of rate ratios of exacerbations in COPD.
We used the data supplied by all 26 studies to perform a primary MTC analysis, supplemented by a variety of sensitivity analyses. Our primary MTC analysis focused on comparing just the 10 interventions that were included in the 26 studies, whereas our secondary MTC analysis aimed to facilitate the comparison of all possible interventions obtained by combining the active treatments (ie, five single interventions plus 10 combinations of active single interventions). The sensitivity analyses accompanying the primary MTC analysis explored the robustness of our conclusions to changes in the nature of the data, the model or the outcome.
The primary MTC analysis used the rates of exacerbations as the outcome of interest and implemented a standard random-effects Poisson regression model that did not include any covariate, similar to the one considered by Cooper et al.Citation26 Appendix 1 provides a description of the model implementation of our primary analysis along with details concerning its WinBUGS implementation (MRC Biostatistics Unit, Cambridge, UK).
The sensitivity analyses accompanying our primary MTC analyses proceeded along the following lines. First, we examined a fixed-effects Poisson regression model; second, we applied a random-effects logistic regression model to the binomial event rates using relative risk as the pooled effect size, and third, we examined i) whether or not covariates such as severity of COPD exacerbations and study publication year could be used to explain the between-study heterogeneity in our primary MTC analysis, and ii) whether the results produced by the primary MTC analysis were insensitive to various choices of Bayesian priors for the between-study standard deviation. We also re-run our primary analysis using the same data as for the secondary analysis. In the secondary analysis, the data for one of the published trials by Calverley was replaced with that from a trial unpublished at the time of manuscript acceptance that pooled the Calverley trial with new data.Citation27 Appendix 1 displays the results of the main sensitivity analyses.
While our primary MTC analysis enabled us to derive the relative effects of the interventions directly investigated in the 26 studies included in our systematic review, it did not afford enough flexibility to facilitate comparisons between combinations of active treatments not investigated in these studies. For instance, given that roflumilast plus LABA was directly investigated in one of the 26 studies and LABA plus LAMA was directly investigated in two of the 26 studies, the relative effect of roflumilast plus LABA versus LABA plus LAMA could easily be derived on the basis of the primary MTC analysis. Nevertheless, this analysis did not support the derivation of the relative effect of roflumilast plus LABA plus LAMA versus LABA plus LAMA, as none of the 26 studies utilized in the analysis investigated the effect of roflumilast plus LABA plus LAMA relative to that of another intervention.
To overcome this limitation of our primary MTC analysis, we conducted a secondary MTC analysis. Just like the primary MTC analysis, the secondary MTC analysis used the rates of exacerbations as the outcome of interest and relied on a random-effects Poisson regression model for the intervention effects. In this model, termed an additive main-effects model, each of the single treatments of placebo, roflumilast, LABA, LAMA, and ICS was allowed to have a different mean effect, denoted by dPlacebo, dRoflumilast, dLABA, dLAMA, and dICS, respectively. Furthermore, the effect of each combination of two or more active treatments (eg, roflumilast plus LABA plus LAMA), was expressed as a sum of the relevant active component effects, dRoflumilast, dLABA, dLAMA, and dICS, for a particular intervention k. So for the intervention roflumilast plus LABA plus LAMA, one had dk = dRoflumilast + dLABA + dLAMA. More generally, for the intervention k, one had:
where the notation dRoflumilast * Ik⊃Roflumilast means that the intervention k included a roflumilast component. (In other words, Ik⊃Roflumilast was set to 1 if dk included a roflumilast component and 0 otherwise). Our additive main effects model is similar to the additive main effects models considered by Welton et alCitation28 with the difference being that we used rates of exacerbation as our outcome, rather than binary or continuous outcomes.
Our primary and secondary MTC analyses assumed that 1) the study-specific relative treatment effects were different yet similar enough to combine from a common population and 2) the potential heterogeneity in study-specific relative treatment effects was constant across pairwise treatment comparisons. Various sensitivity analysis models additionally assumed that potential heterogeneity in study-specific relative treatment effects could not be explained by chance alone and investigated to what extent a study-specific covariate would help explain the excess between-study variation. These models assumed that the effect of the covariate of interest on the relative effects of pairs of treatments was common across all pairwise treatment comparisons. All models took into account the correlation structure induced by the multi-arm trials, except for the random-effects logistic regression model used in the sensitivity analysis relying on binomial event rates.
For both the primary and secondary MTC analyses, we produced estimated rate ratios of exacerbations in COPD per patient-years and corresponding 95% confidence intervals for each pairwise treatment comparison. We also produced estimates of the absolute effect of each treatment – expressed as mean exacerbations per patient-years – as well as estimated probabilities that each treatment is best (in the sense of being associated with the lowest rate of exacerbations in COPD per patient-years).
We produced similar quantities for the sensitivity analyses utilizing the rates of exacerbations as an outcome. For the sensitivity analyses involving binomial event rates, we produced estimated relative risks and corresponding 95% confidence intervals for each pairwise treatment comparison, along with estimates of the absolute effect of each treatment and estimated probabilities that each treatment is best.
For all MTC analyses, we measured the goodness of fit of each of the models to the data by calculating the residual deviance and comparing it against the number of unconstrained data points, where the number of unconstrained data points was obtained by summing up the number of study arms across all studies included in our analyses. Given a model, the residual deviance is defined as the difference between the deviance for the fitted model and the deviance for the saturated model, where the deviance measures the fit of the model to the unconstrained data points using the appropriate likelihood function (eg, Poisson likelihood, binomial likelihood). Under the null hypothesis that the model provides an adequate fit to the data, the residual deviance is expected to have a mean equal to the number of unconstrained data points.Citation26 We compared the fits of the models using the deviance information criterion (DIC). A model with its DIC being at least three points lower than a second model is considered to have a better fit.Citation29
We fitted all models via a Bayesian Markov chain Monte Carlo (MCMC) method, as implemented in the freely available software WinBUGS (Version 1.4; MRC Biostatistics Unit). Given each model, we used noninformative normal priors for all model parameters except for the between-study standard deviation, for which we used an noninformative uniform prior (range 0–10). For each model, we ran two MCMC chains for 100,000 iterations with a thin parameter of 10 after a ‘burn-in’ of 20,000 in order to ensure convergence of the MCMC sampler. We conducted posterior inference after discarding the ‘burn-in’ iterations, thereby relying on 20,000 samples. The results of the model fits are also presented in Appendix 1. We checked the MTC rate outcomes to standard pairwise random-effects meta-analysis for consistency.Citation30
Results
Inclusion of studies
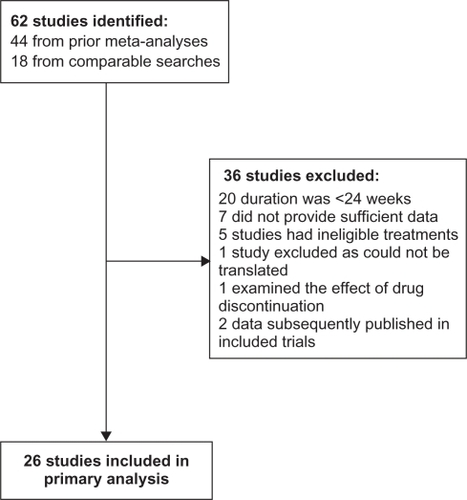
Twenty-six studies met our inclusion criteria for our primary analysis.Citation6–Citation9,Citation31–Citation54 Of the four studies each reporting on two clinical trials, three pooled the trial data together,Citation6,Citation34,Citation39 and one reported each trial separately.Citation7
Thirty clinical trials included in two previous meta-analyses assessing COPD drugsCitation17,Citation55 were excluded from our study because they did not meet our inclusion criteria.Citation56–Citation83 Eighteen of these clinical trials were excluded because the treatment duration was less than 24 weeks in length.Citation56,Citation59,Citation60,Citation62–Citation65,Citation67,Citation69,Citation70,Citation72,Citation74,Citation75,Citation77,Citation79–Citation82 Eleven were excluded because they assessed treatments that were not of interest,Citation57,Citation61,Citation66,Citation76,Citation83 they did not provide sufficient detail on exacerbations,Citation54,Citation68,Citation71,Citation73 they were published in a language other than English,Citation58 or they examined the effect of drug discontinuation.Citation78 One additional clinical trialCitation84 included in the previous meta-analyses was excluded from our study because the data was later republished together with another trial.Citation34 We considered the data from both trials as published in the second manuscript.Citation34 Five clinical trials found in our comparable search were also excluded because they did not provide sufficient detail on exacerbationsCitation2–Citation4 or the treatment duration was less than 24 weeks in length.Citation5,Citation10 displays the study flow diagram.
All clinical trials that met our inclusion criteria reported COPD exacerbations following treatment. All clinical trials recruited patients with a forced expiratory volume in 1 second (FEV1) <80% of the predicted value. Duration of treatment ranged from 24 weeks to 4 years. All clinical trials permitted the use of background therapy and/or rescue therapy. Twenty of the randomized trials used a placebo control,Citation6,Citation8,Citation9,Citation33–Citation42,Citation45–Citation51,Citation54 12 assessed LAMA,Citation7,Citation31,Citation34,Citation39,Citation40,Citation42,Citation45,Citation47,Citation50–Citation53 13 assessed LABA,Citation7,Citation32,Citation34,Citation36–Citation38,Citation41,Citation43,Citation44,Citation48,Citation49,Citation52,Citation54 7 assessed ICS,Citation33,Citation35–Citation38,Citation48,Citation49 3 assessed roflumilast,Citation6,Citation8,Citation9 and 13 assessed combinations of these drugs: 2 LAMA plus LABA,Citation31,Citation52 8 LABA plus ICS,Citation32,Citation36–Citation38,Citation43,Citation44,Citation49,Citation53 1 LAMA plus LABA plus ICS,Citation31 1 LAMA plus roflumilast,Citation7 and 1 LABA plus roflumilast.Citation7
Twenty-six studies provided data on the total number of exacerbations and/or the mean annual rate of exacerbations among a combined 36,312 patients.Citation6–Citation9,Citation31,Citation32,Citation34–Citation40,Citation42–Citation51,Citation53,Citation54 These data contributed to our first analysis of total exacerbations. provides the characteristics of these clinical trials. An additional three studiesCitation33,Citation41,Citation52 provided data on the proportion of patients with at least one exacerbation allowing a combined 36,657 patients. These data contributed to our second analysis of the number of patients with at least one exacerbation. provides the characteristics of these clinical trials.
Table 1A Overview of included clinical trials that provide data on the total number of exacerbations and/or the mean annual rate of exacerbations
Table 1B Overview of additional included clinical trials that provide data on the number of patients with at least one exacerbation
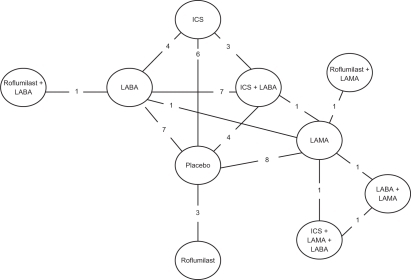
The network of treatments compared is displayed in . The treatments form a closed network, which is amenable to MTC analyses.
Figure 2 Diagram displaying the network of 10 treatments involved in the MTC analyses of the COPD data. Each treatment is a node in the network. The links between nodes are used to indicate a direct comparison between pairs of treatments. The numbers shown along the link lines indicate the number of trials comparing pairs of treatments head-to-head.
Reporting quality
We assessed the quality of reporting specific methodological items. Eighteen reported on how randomization was achieved,Citation6–Citation9,Citation31–Citation33,Citation35,Citation36,Citation38,Citation41,Citation43,Citation45,Citation46,Citation48,Citation50,Citation51,Citation53 16 reported on concealment of allocation,Citation6–Citation9,Citation31–Citation33,Citation35,Citation36,Citation38,Citation44–Citation46,Citation48,Citation50,Citation53 14 reported on blinding,Citation6–Citation9,Citation31,Citation33,Citation35,Citation36,Citation38,Citation40,Citation45,Citation46,Citation50,Citation54 20 were assumed as intention-to-treat time periods,Citation6–Citation9,Citation32,Citation33,Citation34,Citation36–Citation42,Citation45,Citation46,Citation48,Citation49,Citation52,Citation53 and 20 had greater than 20% drop-outs.Citation6,Citation9,Citation31,Citation32,Citation35–Citation40,Citation42,Citation43,Citation45,Citation47–Citation51,Citation53,Citation54
Results of the primary MTC analysis
The random-effects Poisson regression model considered in our primary MTC analysis provides a reasonable fit to the data, as evidenced by the low residual deviance (67.61) compared to the unconstrained number of data points (62).
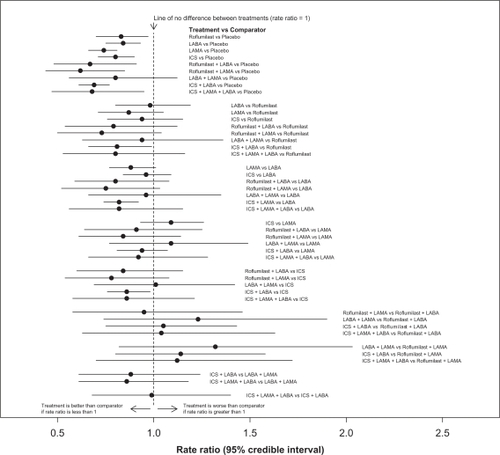
reports the estimated rate ratios of exacerbations and 95% confidence intervals for the relative effects of the 10 interventions for management of COPD investigated in the 26 studies. displays these results graphically. As can be seen from and the direct (head-to-head) evaluations reported in Appendix 1 ( and ), the studies provide consistent results.
Figure 3 Comparisons of all 10 different treatments for management of COPD. Rate ratios and associated 95% confidence intervals were obtained from a random-effects MTC model without covariates.
Appendix Table 7 Random effects, direct (head to head) evaluation using DerSimmonian Laird random-effects model. Exacerbation rates
Appendix Table 8 Random effects, direct (head to head) evaluation using DerSimmonian Laird random-effects model. Binomial model
Table 2 Estimated rate ratios and 95% CI for the relative effects of pairs of treatments, produced by the random-effects MTC model without covariates
reports the absolute treatment effects corresponding to the 10 interventions, expressed as mean exacerbations per patient-years. The findings in this table favor both current intensive therapy (ICS plus LABA plus LAMA) and also the addition of roflumilast to this therapy.
Table 3 Absolute treatment effects corresponding to the 10 treatments for the management of COPD as derived from the primary analysis
reports the probability that each treatment is best obtained on the basis of our primary analysis. Each column represents the possibility of first-line treatment, second-line, and so on. According to , the highest probability of reductions in exacerbations is found from the combination of roflumilast plus a LAMA.
Table 4 Probability each of the 10 treatments for management of COPD is best, obtained on the basis of the random-effects MTC model without covariates
Results of the additive MTC analysis
Our additive main effects model considered in our secondary MTC analysis provides adequate fit to the data, as evidenced by the low residual deviance (69.56) compared to the unconstrained number of data points (62) (slightly lower than that of the model considered in our primary MTC analysis, but still within a 3-point difference), suggesting that this model is comparable to the one used in our primary MTC analysis.
reports the estimated rate ratios of exacerbations and 95% confidence intervals for the relative effects of specific pairs of treatment combinations. Each pair is of the form “comparator plus roflumilast” vs “comparator”, with “comparator” being one of the combinations LABA plus ICS, LABA plus ICS plus LAMA, and LABA plus LAMA.
Table 5 Estimated rate ratios and 95% CI for the effects of specific pairs of treatment combinations, produced by the additive main effects model considered in our secondary MTC analysis
reports the absolute treatment effects corresponding to the 15 interventions (ie, 5 single treatments plus 10 combinations of active treatments), expressed as mean exacerbations per patient-years. The findings in this table favor both current intensive therapy (ICS plus LABA plus LAMA) and also the addition of roflumilast to this therapy (roflumilast plus ICS plus LABA plus LAMA).
Table 6 Absolute treatment effects corresponding to the 15 treatments for the management of COPD (ie, 5 single treatments plus 10 combinations of active treatments), obtained on the basis of the additive main effects model considered in our secondary MTC analysis
reports the probability that each treatment is best, obtained on the basis of our secondary analysis. The highest probability of reductions in exacerbations is found from the combination of roflumilast and the current intensive therapy (roflumilast plus ICS plus LABA plus LAMA). All data and output from this model are available from the authors upon request.
Table 7 Probability each of the 15 treatments (ie, 5 single treatments plus 10 combinations of active treatments) for management of COPD is best, obtained on the basis of the additive main effects model considered in our secondary MTC analysis
Results of the sensitivity analyses
Our first sensitivity analysis replaced the random-effects Poisson regression model used in the primary MTC analysis with a fixed-effect Poisson regression model. The results of this sensitivity analysis can be found in Appendix 1 (–). In particular, these results suggest that the fixed-effect and random-effects analyses provide consistent finding. However, the residual deviance associated with the model employed in the fixed-effect analysis is considerably higher (189.00) than that associated with the model used in the random-effects analysis, indicating that the fixed effects model provides a questionable fit to the data.
Appendix Table 1 Estimated rate ratios and associated 95% CI for the relative effects of pairs of treatments for the management of COPD, produced by the fixed-effect MTC model without covariates
Appendix Table 3 Probability that each of the 10 treatments for management of COPD is best, obtained on the basis of the fixed-effect MTC model without covariates
– and present the findings of our second sensitivity analysis examining the binomial event of ever having an exacerbation event within the intention to treat population over the study period. We found consistent effects between the primary MTC analysis using rates of exacerbation and the current sensitivity analysis using binomial outcomes. This strengthens the inference about the credibility of the analysis and the relative treatment effects of the interventions. provides similar probabilities that each treatment is best as first line therapy. The results of the sensitivity analyses examining the inclusion of previously unpublished roflumilast data (M-111 trial)Citation27 are presented in –.
Appendix Table 4 Estimated relative risks and 95% confidence intervals for all pairs of treatments produced by the random-effects MTC model without covariates. Binomial model
Appendix Table 6 Probability each of the 10 treatments for management of COPD is best, obtained on the basis of the random-effects MTC model without covariates. Binomial model
Appendix Table 9 Estimated rate ratios and associated 95% CI for the relative effects of pairs of treatments for the management of COPD, produced by random effects MTC involving previously unpublished roflumilast data (M2-111 trial)Citation28
Appendix Table 12 Estimated rate ratios and 95% CI for the effects of specific pairs of treatment combinations, produced by the additive main effects model considered in our MTC analysis including previously unpublished data (M2-111)Citation28
The results of the remaining sensitivity analyses are omitted in the interest of saving space. These analyses found that the choice of prior for the between-study standard deviation did not influence the outcome of our primary MTC analysis. Also, disease severity and study publication year were found to be insignificant modifiers of the relative treatment effects produced by the random-effects Poisson regression model. This data is available from the authors upon request.
Discussion
Our study demonstrates that there are small differing treatment effects according to the choice of treatment combinations chosen. In our analysis, combinations treatments demonstrated the largest probability of the largest therapeutic effects. Using an additive main effects analysis, whereby we create combinations that have not been compared together in the trials, we demonstrate that new combinations that include roflumilast appear to offer comparable treatment options to reduce the risk for exacerbations.
To our knowledge, our analysis is the most up to date analysis of interventions recommended in the GOLD and ATS/ERS guidelines for the treatment of COPD.Citation21 There are, of course, other treatments used in COPD, ranging from behavioral therapies to other pharmacotherapies. As with any research study, we set out our study questions, interventions of interest and populations a priori. We believe that our study findings should be of relevance to physicians working with pharmacotherapies and any recommendations for treatment should go hand in hand with individual patient advice tailored to the patient’s situation.
Our findings represent an update of two previously published mixed treatment comparisons.Citation17,Citation55 Our findings are similar to these previous reviews, but differ in two important ways. First, neither review included PDE4 inhibitors, the interventions that appeared most favorable in our analysis. Second, both reviews examined exacerbations as a binomial outcome of whether a patient ever had an exacerbation or not. This outcome is problematic depending on the study population. For example, to take an extreme example, in a population enrolling very severe patients we would expect all patients to have at least one exacerbation, thus the study would find no treatment effect even if the trial intervention importance reduced the frequency of exacerbations.
As with any analysis, there are limitations to consider when interpreting our analysis. We combined exacerbation events across trials that may have differed in terms of patient populations, exacerbation definitions, and study design features. Indeed, this issue applies to all meta-analyses and we considered a priori whether it was appropriate to pool trials and considered it appropriate.Citation85 Despite the large number of patients included in the trials, power to differentiate across interventions is potentially an issue. Indirect comparisons typically require four times the amount of data as a direct comparison and in our analysis we had several comparisons that had only one trial in them. Thus, it is possible that we were unable to identify significant effects where they may exist. The MTC approach aims to borrow power from other studies that use comparable interventions in their study arms, regardless of whether the data from all treatment arms can be utilized.Citation86 We searched thoroughly for relevant clinical trials to include, but it is possible we have missed unpublished studies. Strengths of our study include our extensive analysis that examined the impact of differing strategies of analysis on the final outcomes. Our sensitivity analyses examined both time period of publication and severity of patients and found similar treatment effects regardless of these issues. We applied both exacerbation rates and the outcome of ever having at least one event in our analyses and found almost identical effects. To our knowledge, this is the first COPD meta-analysis to examine this issue and it is reassuring that the findings are similar.
We considered a flexible framework for comparing competing interventions by allowing for the possibility that the total effect of a combination of treatments is equal to the sum of the effects of the components entering this combination. This additive assumption may be untenable in situations where particular pairs of components may have either bigger (synergistic) or smaller (antagonistic) effects than would be expected from the sum of their effects alone. The sparsity of our data prevented us from relaxing the additivity assumption.
Our study utilized evidence from all relevant RCTs of the prespecified interventions, regardless of whether they are in current clinical use. For example, we included trials evaluating a single intervention compared with placebo, even though neither one is used alone in clinical practice. This information increases the power of our analysisCitation86 and, although this information is displayed in all results, only current combinations of clinical interest may be of use to clinicians. This issue is consistent with pairwise meta-analyses in addition to MTC analyses as it allows for increased power and determines the magnitude of treatment effects compared with inert and less effective interventions.
In conclusion, our study represents the most up-to-date analysis of COPD treatments for the reduction of exacerbations that we are aware of. Our study demonstrates consistent effects of treatments that increase in combination.
Disclosure
This study was funded in part by Merck Sharp and Dohme Ltd and Nycomed Ltd. The funders had no role in the study, analysis, interpretation or reporting of this manuscript.
References
- BarnesPJChronic obstructive pulmonary disease: a growing but neglected global epidemicPLoS Med20074e11217503959
- ZhengJYangLWuYThe efficacy and safety of combination salmeterol (50 microg)/fluticasone propionate (500 microg) inhalation twice daily via accuhaler in Chinese patients with COPDChest20071321756176317951625
- RennardSTashkinDMcElhattanJGoldmanMRamachandranSEfficacy and tolerability of budesonide/formoterol in one hydrofluoroalkane pressurized metered-dose inhaler in patients with chronic obstructive pulmonary disease: results from a 1-year randomized controlled clinical trialDrugs20096954956519368417
- LapperreTSnoeck-StrobandJGosmanMEffect of fluticasone with and without salmeterol on pulmonary outcomes in chronic obstructive pulmonary disease: a randomized trialAnn Intern Med200915151752719841453
- TashkinDPearleJIezzoniDVargheseSFormoterol and tiotropium compared with tiotropium alone for treatment of COPDCOPD20096172519229704
- CalverleyPRabeKGoehringURoflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trialsLancet200937468569419716960
- FabbriLCalverleyPIzquierdo-AlonsoJRoflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with longacting bronchodilators: two randomised clinical trialsLancet200937469570319716961
- RabeKBatemanEO’DonnellDRoflumilast – an oral anti-inflammatory treatment for chronic obstructive pulmonary disease: a randomised controlled trialLancet200536656357116099292
- CalverleyPSanchez-TorilFMcIvorAEffect of 1-year treatment with roflumilast in severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200717615416117463412
- SinDDMcAlisterFAManSFAnthonisenNRContemporary management of chronic obstructive pulmonary disease: scientific reviewJAMA20032902301231214600189
- SobierajDMWhiteCMColemanCIBenefits and risks of adjunctive inhaled corticosteroids in chronic obstructive pulmonary disease: a meta-analysisClin Ther2008301416142518803985
- NanniniLCatesCLassersonTPoolePCombined corticoster- oid and long-acting beta-agonist in one inhaler versus pla- cebo for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20074CD00379417943798
- YangIAFongKMSimEHBlackPNLassersonTJInhaled corticosteroids for stable chronic obstructive pulmonary diseaseCochrane Database Syst Rev20072CD00299117443520
- WiltTJNiewoehnerDMacdonaldRKaneRLManagement of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guidelineAnn Intern Med200714763965317975187
- NanniniLCatesCLassersonTPoolePCombined corticosteroid and long-acting beta-agonist in one inhaler versus long-acting beta-agonists for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20074CD00682917943918
- NanniniLCatesCLassersonTPoolePCombined corticoster- oid and long-acting beta-agonist in one inhaler versus inhaled steroids for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20074CD00682617943917
- PuhanMBachmannLKleijnenJTer RietGKessellsAInhaled drugs to reduce exacerbations in patients with chronic obstructive pulmonary disease: a network meta-analysisBMC Med20097219144173
- BakerWBakerEColemanCPharmacologic treatments for chronic obstructive pulmonary disease: a mixed-treatment comparison meta-analysisPharmacotherapy20092989190519637942
- AaronSDFergussonDMarksGBfor the Canadian Thoracic Society/Canadian Respiratory Clinical Research ConsortiumCounting, analysing and reporting exacerbations of COPD in randomised controlled trialsThorax20086312212817702790
- SuissaSStatistical treatment of exacerbations in therapeutic trials of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200617384284616439716
- American Thoracic Society, European Respiratory SocietyStandards for the diagnosis and management of patients with COPD Available from: http://www.thoracic.org/clinical/copd-guidelines/resources/copddoc.pdf. Accessed January 10, 2011.
- Rodriguez-RoisinRToward a consensus definition for COPD exacerbationsChest2000117398S401S10843984
- SalantiGKavvouraFKIoannidisJPExploring the geometry of treatment networksAnn Intern Med200814854455318378949
- LuGAdesAECombination of direct and indirect evidence in mixed treatment comparisonsStat Med2004233105312415449338
- SuttonAAdesAECooperNAbramsKUse of indirect and mixed treatment comparisons for technology assessmentPharmacoeconomics20082675376718767896
- CooperNJSuttonAJLuGKhuntiKMixed comparison of stroke prevention treatments in individuals with nonrheumatic atrial fibrillationArch Intern Med20061661269127516801509
- RennardSICalverleyPMGoehringUMBredenbrokerDMartinezFJReduction of exacerbations by the PDE4 inhibitor roflumilast – the importance of defining different subsets of patients with COPDRespir Res2011121821272339
- WeltonNJCaldwellDMAdamopoulosEVedharaKMixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart diseaseAm J Epidemiol20091691158116519258485
- SpiegelhalterDJBestNGCarlinBPvan der LindeABayesian measures of model compexity and fitJournal of the Royal Statistical Society200264583639
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials198671771883802833
- AaronSVandemheenKFergussonDTiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trialAnn Intern Med200714654555517310045
- AnzuetoAFergusonGFeldmanGEffect of fluticasone propionate/salmeterol (250/50) on COPD exacerbations and impact on patient outcomesCOPD2009632032919863361
- BourbeauJRouleauMBoucherSRandomised controlled trial of inhaled corticosteroids in patients with chronic obstructive pulmonary diseaseThorax1998534774829713447
- BrusascoVHodderRMiravitllesMHealth outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPDThorax20035839940412728159
- BurgePCalverleyPJonesPRandomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ20003201297130310807619
- CalverleyPAndersonJCelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med200735677578917314337
- CalverleyPBoonsawatWCsekeZMaintenance therapy with Budesonide and Formoterol in chronic obstructive pulmonary diseaseEur Respir J20032291291914680078
- CalverleyPPauwelsRVestboJCombined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trialLancet200336144945612583942
- CasaburiRMahlerDJonesPA long-term evaluation of once-daily inhaled Tiotropium in chronic obstructive pulmonary diseaseEur Respir J20021921722411866001
- ChanCMaltaisFSigouinCA randomized controlled trial to assess the efficacy of Tiotropium in Canadian patients with chronic obstructive pulmonary diseaseCan Respir J20071446547218060091
- ChapmanKArvidssonPChuchalinAThe addition of salmeterol 50 microg bid to anticholinergic treatment in patients with COPD: a randomized, placebo controlled trial. Chronic obstructive pulmonary diseaseCan Respir J2002917818512068339
- DusserDBravoMIaconoPThe effect of tiotropium on exacerbations and airflow in patients with COPDEur Respir J20062754755516507855
- FergusonGAnzuetoAFeiREffect of fluticasone propionate/salmeterol (250/50 microg) or salmeterol (50 microg) on COPD exacerbationsRespir Med20081021099110818614347
- KardosPWenckerMGlaabTVogelmeierCImpact of Salmeterol/fluticasone propionate versus salmeterol on exacerbations in severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200717514414917053207
- NiewoehnerDRiceKCoteCPrevention of exacerbations of chronic obstructive pulmonary disease with Tiotropium, a once-daily inhaled anticholinergic bronchodilator: a randomized trialAnn Intern Med200514331732616144890
- PaggiaroPDahleRBakranIMulticentre randomised placebo-controlled trial of inhaled fluticasone propionate in patients with chronic obstructive pulmonary disease. International COPD Study GroupLancet19983517737809519948
- PowrieDWilkinsonTDonaldsonGEffect of tiotropium on sputum and serum inflammatory markers and exacerbations in COPDEur Respir J20073047247817504798
- StockleyRChopraNRiceLAddition of salmeterol to existing treatment in patients with COPD: a 12 month studyThorax20066112212816443706
- SzafranskiWCukierARamirezAEfficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary diseaseEur Respir J200321748112570112
- TashkinDCelliBSennSA 4-year trial of tiotropium in chronic obstructive pulmonary diseaseN Engl J Med20083591543155418836213
- TonnelAPerezTGrosboisJEffect of tiotropium on health-related quality of life as a primary efficacy endpoint in COPDInt J Chron Obstruct Pulmon Dis2008330131018686739
- VogelmeierCKardosPHarariSFormoterol mono- and combination therapy with tiotropium in patients with COPD: a 6-month studyRespir Med20081021511152018804362
- WedzichaJCalverleyPSeemungalTThe prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromideAm J Respir Crit Care Med2008177192617916806
- RossiAKristufekPLevineBComparison of the efficacy, tolerability, and safety of formoterol dry powder and oral, slow-release theophylline in the treatment of COPDChest20021211058106911948033
- BakerWBakerEColemanCPharmacologic treatments for chronic obstructive pulmonary disease: a mixed-treatment comparison meta-analysisPharmacotherapy20092989190519637942
- BarnesNQiuYPavordIAnti-inflammatory effects of salmeterol/fluticasone propionate in chronic obstructive lung diseaseAm J Respir Crit Care Med200617373674316424444
- BaumgartnerRHananiaNCalhounWNebulized arformoterol in patients with COPD: a 12-week, multicenter, randomized, double-blind, double-dummy, placebo- and active-controlled trialClin Ther20072926127817472819
- BeehKBeierJBuhlREfficacy of tiotropium bromide (Spiriva) in patients with chronic-obstructive pulmonary disease (COPD) of different severitiesPneumologie20066034134616761228
- BoydGMoriceAPounsfordMAn evaluation of salmeterol in the treatment of chronic obstructive pulmonary disease (COPD)Eur Respir J1997108158219150318
- CalverleyPLeeATowseLEffect of tiotropium bromide on circadian variation in airflow limitation in chronic obstructive pulmonary diseaseThorax20035885586014514937
- CampbellMElirazAJohanssonGFormoterol for maintenance and as-needed treatment of chronic obstructive pulmonary diseaseRespir Med2005991511152016199148
- CasaburiRBriggsDJrDonohueJThe spirometric efficacy of once-daily dosing with tiotropium in stable COPD: a 13-week multicenter trial. The US Tiotropium Study GroupChest20001181294130211083677
- CelliBHalpinDHepburnRSymptoms are an important outcome in chronic obstructive pulmonary disease clinical trials: results of a 3-month comparative study using the Breathlessness, Cough and Sputum Scale (BCSS)Respir Med200397S35S4312564609
- CovelliHBhattacharyaSCassinoCConoscentiCKestenSAbsence of electrocardiographic findings and improved function with once-daily tiotropium in patients with chronic obstructive pulmonary diseasePharmacotherapy2005251708171816305289
- DahlRGreefhorstLNowakDInhaled formoterol dry powder versus ipratropium bromide in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200116477878411549532
- Dal NegroRPomariCTognellaSMichelettoCSalmeterol and fluticasone 50 microg/250 microg bid in combination provides a better long-term control than salmeterol 50 microg bid alone and placebo in COPD patients already treated with theophyllinePulm Pharmacol Ther20031624124612850128
- FreemanDLeeAPriceDEfficacy and safety of tiotropium in COPD patients in primary care – the SPiRiva Usual CarE (SPRUCE) studyRespir Res200784517605774
- HananiaNDarkenPHorstmanDThe efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus inhaler for the treatment of COPDChest200312483484312970006
- HattotuwaKGizyckiMAnsariTJefferyPBarnesNThe effects of inhaled fluticasone on airway inflammation in chronic obstructive pulmonary disease: a double-blind, placebo-controlled biopsy studyAm J Respi Crit Care Med200216515921596
- LittnerMIlowiteJTashkinDLong-acting bronchodilation with once-daily dosing of tiotropium (Spiriva) in stable chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20001611136114210764302
- Llewellyn-JonesCHarrisTStockleyREffect of fluticasone propionate on sputum of patients with chronic bronchitis and emphysemaAm J Respir Crit Care Med19961536166218564107
- MahlerDDonohueJBarbeeREfficacy of salmeterol xinafoate in the treatment of COPDChest199911595796510208192
- MahlerDWirePHorstmanDEffectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20021661084109112379552
- O’DonnellDFlugeTGerkenFEffects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPDEur Respir J20042383284015218994
- O’DonnellDSciurbaFCelliBEffect of fluticasone propionate/salmeterol on lung hyperinflation and exercise endurance in COPDChest200613064765616963658
- PaggiaroPVagagginiBDi FrancoAEfficacy of nebulized flunisolide combined with salbutamol and ipratropium bromide in stable patients with moderate-to-severe chronic obstructive pulmonary diseaseRespiration20067360360916293958
- RennardSAndersonWZuWallackRUse of a long-acting inhaled beta2-adrenergic agonist, salmeterol xinafoate, in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20011631087109211316640
- Van der ValkPMonninkhofEvan der PalenJZielhuisGvan HerwaardenCEffect of discontinuation of inhaled corticosteroids in patients with chronic obstructive pulmonary disease: the COPE studyAm J Respir Crit Care Med20021661358136312406823
- Van NoordJAumannJJanssensEComparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPDEur Respir J20052621422216055868
- Van NoordJde MunckDBantjeTLong-term treatment of chronic obstructive pulmonary disease with salmeterol and the additive effect of ipratropiumEur Respir J20001587888510853852
- VerkindreCBartFAguilaniuBThe effect of tiotropium on hyperinflation and exercise capacity in chronic obstructive pulmonary diseaseRespiration20067342042716484769
- WadboMLöfdahlCLarssonKEffects of formoterol and ipratropium bromide in COPD: a 3-month placebo-controlled studyEur Respir J2002201138114612449166
- WeirDBaleGBrightPBurgePA double-blind placebo-controlled study of the effect of inhaled beclomethasone dipropionate for 2 years in patients with nonasthmatic chronic obstructive pulmonary diseaseClin Exp Allergy19992912512810421835
- DonohueJvan NoordJBatemanEA 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterolChest2002122475512114338
- MoayyediPMeta-analysis: Can we mix apples and oranges?Am J Gastroenterol2004992297230115571572
- HigginsJPWhiteheadABorrowing strength from external trials in a meta-analysisStat Med199615273327498981683
Appendix 1
Description and WinBUGS implementation of primary analysis model. Let A, B, C, D, E, F, G, H, I and J denote the treatments placebo, roflumilast, LABA, LAMA, ICS, roflumilast + LABA, roflumilast + LAMA, LABA + LAMA, ICS + LABA and ICS + LAMA + LABA, respectively. Assume that A is the reference (or baseline) treatment for the analysis. For each trial j, denote the total number of exacerbations in COPD observed for the njk patients allocated to treatment k by rjk. Also, let pyjk denote the patient-years of follow-up in trial j on treatment k.
Using this notation, the random-effects Poisson regression model used in our primary analysis can be expressed as:
Here, λjk is the expected number of exacerbations in COPD in trial j for treatment k and represents the mean of the Poisson distribution in trial j under treatment k. Also, μjA is the log rate of an exacerbation in COPD in trial j on the baseline treatment A, and δjkA is the trial-specific log rate ratio of the active treatment k relative to the baseline treatment A. These trial-specific log rate ratios are drawn from a random effects distribution: δjkA ∼ Normal(dkA, σ2). The pooled log rate ratios dkA for treatment k relative to the baseline treatment A are “baseline” parameters which are used to derive the “functional parameters” dkl representing the pooled log rate ratios of the active treatment k relative to the active treatment l via the consistency equation dkl = dlA − dkA. The between-study variance σ2 is a heterogeneity parameter that quantifies the extent of the variation between the results of the different studies included in the analysis. Note that this variance is assumed constant for all pairwise treatment comparisons.
The above model was fitted to the data using WinBUGS (Version 1.4; MRC Biostatistics Unit). For this model, two MCMC chains were run for 100,000 iterations after a ‘burn-in’ of 20,000 in order to ensure convergence of the MCMC sampler. Posterior inference was conducted after discarding the ‘burn-in’ iterations, based on 20,000 samples. The prior distributions placed on parameters in this model were vague and were specified as follows:
Appendix Table 2 Absolute treatment effects corresponding to the 10 treatments for the management of COPD, as derived from the fixed-effect MTC model without covariates
Appendix Table 5 Absolute treatment effects obtained from the random-effects MTC model on binomial model
Appendix Table 10 Absolute treatment effects obtained from the random-effects MTC model including previously unpublished roflumilast data (M2-111 trial)Citation28
Appendix Table 11 Probability each of the 15 treatments (ie, 5 single treatments plus 10 combinations of active treatments) for management of COPD is best, obtained on the basis of the additive main effects model considered in our secondary MTC analysis. This table includes previously unpublished roflumilast data (M2-111 trial)Citation28