Abstract
Background
Association between psoriasis severity and cerebro- and cardiovascular comorbidities has rarely been investigated.
Aim
We aimed to investigate differences in cerebro- and cardiovascular comorbidities by psoriasis severity.
Materials and methods
Using Swedish nationwide health-care registers, new adult users of anti-psoriatic drugs (2007–2013) with a recorded diagnosis of psoriasis/psoriatic arthritis or a filled prescription for calcipotriol were included. Psoriasis severity was based on the type of anti-psoriatic treatment (topical/mild, non-biologic systemic/moderate-to-severe, and biologics/ severe). Age standardized prevalence rates of cerebro- and cardiovascular comorbidities and their risk factors were compared between the groups.
Results
We found that severe psoriasis patients (N=2147) were younger than moderate-to-severe (N=11,919) or mild (N=70,796) patients (median 44, 52, and 55 years). Prevalence of hypertension was 29.9%, 32.6%, and 36.5%, myocardial infarction was 2.5%, 2.3%, and 1.8%, and stroke was 2.4%, 2.2%, and 1.1% in mild, moderate-to-severe, and severe psoriasis patients, respectively. Diabetes prevalence was 7.6% in mild, 8.0% in moderate-to-severe, and 10.7% in severe psoriasis.
Conclusion
Myocardial infarction and stroke were less common in patients with severe psoriasis while, despite being younger, they had a higher prevalence of diabetes and hypertension.
Introduction
Prevalence of psoriasis, a common chronic inflammatory disease, is around 0.09%–11.4% in the worldCitation1,Citation2 and 2%–4% in most developed countries.Citation2–Citation4 In recent years, psoriasis has been considered to be associated with diseases, such as cardiovascular diseases (CVDs) and metabolic disorders (MDs).Citation5–Citation7
Hypertension (HTN) has proved more common in psoriatic patients than in the general population.Citation8–Citation11 Psoriasis has also been associated with a higher risk of myocardial infarction (MI)Citation12 even after adjustment for known risk factors.Citation13 Few studies, however, have examined how these comorbidities vary based on the psoriasis severity. Armstrong and HarskampCitation14 reported that the risk of HTN is increased in patients with severe psoriasis compared with a mild condition. Mehta et alCitation13 found that the severity of psoriasis was associated with the major CVD events: MI and stroke. With respect to MDs, studies have indicated that diabetes mellitus (DM) is more prevalent among psoriatic patients,Citation12 especially among patients with severe disease.Citation11,Citation15 Psoriasis has also been found an independent risk factor of type 2 DM after controlling for age, sex, body mass index, HTN, and hyperlipidemia.Citation11
Despite this knowledge, our study aims to investigate the prevalence of cerebro- and cardiovascular comorbidities in a larger sample of psoriasis patients, as prior studies are limited due to the relatively small sizes. We used a large nationwide population of psoriasis patients, to find the prevalence of comorbidities during the 5-year period preceding treatment initiation (untreated time) for psoriasis or psoriatic arthritis.
Materials and methods
Using the National Patient Register (NPR) and the Prescribed Drug Register (PDR) covering the Swedish population, we identified patients with either a diagnosis of psoriasis/psoriatic arthritis and/or calcipotriol treatment. The first dispensing of a psoriasis medication was then identified to determine inclusion eligibility. The NPRCitation16 has recorded inpatient hospital discharge diagnoses since 1964, with complete national coverage since 1987. The current completeness of the register is >99%.Citation16 Starting in 2001, diagnoses from outpatient visits at hospital are also registered. Details on all drugs dispensed at pharmacies by personal prescriptions to the entire Swedish population are registered in the PDR since 1st July 2005.Citation17 Drugs are classified according to the Anatomical Therapeutic Chemical (ATC) classification system.Citation18 Drug treatment during inpatient hospital care and purchases of over-the-counter medications are not recorded. Migration data were retrieved from the Total Population Register, which has collected computerized demographic data since 1968.Citation19 All registers were linked using the unique personal identity number assigned to all Swedish residents since 1947.
A flow diagram of patients with psoriasis according to the inclusion and exclusion criteria for this study is shown in . Patients with a main diagnosis of psoriasis or psoriatic arthritis between 1968 and 2013 () were identified in NPR. The patients who subsequently filled at least 1 dispensing of an anti-psoriatic drug () between 1 July 2007 and 31 December 2013, without a prior dispensing of these medications since 1 July 2005, were eligible for inclusion. In order to identify psoriatic patients diagnosed in primary care (not recorded in NPR), we also included patients who filled at least 1 dispensing of calcipotriol with/without corticosteroids (ATC-codes D05AX02, D05AX52) during the same time-interval of 1 July 2007 to 31 December 2013, without such drugs dispensed between 1 July 2005 and 30 June 2007. Only patients aged >18 years at the date of the first dispensing were included. All patients from the topical treatment group who were dispensed a non-biological or a biological treatment before topical treatment index date (the first dispensing date of anti-psoriatic drugs in each treatment group) and all patients in non-biological treatment group who received a biological drug before their index date were excluded. Patients were also excluded if they migrated to/from Sweden during the 5-year period prior to therapy initiation because these patients did not have full 5-year coverage of comorbidity history in the national registers. Since we only included patients without treatment of psoriasis (or psoriatic arthritis) between 1 July 2005 and 30 June 2007, we restricted our study population to those with little or no disease activity during at least 2 years preceding the new anti-psoriatic treatment.
We classified psoriatic patients (including psoriatic arthritis) based on the type of the dispensed anti-psoriatic drugs: 1) topical group (calcipotriol with/without corticosteroids), 2) non-biological systemic group (methotrexate, cyclosporine, acitretin, or phototherapy), and 3) biological group (adalimumab, etanercept, infliximab, efalizumab, ustekinumab, certolizumab, or golimumab). These treatments have been shown to correlate with increasing psoriasis severity, ranging from mild (topical) to moderate (non-biologic systemics) to severe (biologics).Citation20,Citation21 We used calcipotriol with/without corticosteroids as the proxy to identify the mild psoriasis group since this drug is used exclusively to treat mild psoriasis.Citation22 We chose not to include drugs, such as corticosteroids, coal tar, vitamin D, etc., which are also used for other indications than psoriasis. This selection is conservative as it possibly identifies patients with psoriasis disease, but may lead to a lower sample size. Patients were allowed to be included in more than 1 treatment group if they were treated with different drug types, as long as the treatment groups followed the hierarchical treatment sequence: topical to non-biologic systemic to biologics. Concurrent use was classified to the most potent group; for example, a patient prescribed adalimumab and methotrexate on the same date, was classified into the biological group since adalimumab is used for the treatment of severe psoriasis.
Individuals with CVD comorbidities and risk factors were identified in both NPR and PDR (). CVDs, such as MI, angina pectoris, atrial fibrillation, stroke, heart failure, and hypertensive diseases were identified from NPR 5 years prior to index date. The diseases were captured from primary or secondary diagnosis in either the in- or outpatient settings. The same procedure was used for MDs, all of which are risk factors for CVDs. Data on HTN and DM were identified both in NPR and by filled prescriptions in PDR. We are limited in identifying HTN, DM, and hyperlipidemia in NPR, since these diseases are often diagnosed and treated in primary health centers. Therefore, dispensed drugs from PDR was used as a proxy to identify these comorbidities. The dispensed drugs were identified during a 2-year period prior to index date.
The study was approved by the Research Ethics Committee of Karolinska Institutet (Approval 2009/1250_31/4).
Statistical analysis
We estimated the prevalence rate of the comorbidities during 5 years before initiation of the treatment among psoriasis patients with mild, moderate-to-severe, and severe psoriasis based on anti-psoriatic treatments. In fact, our study includes only the untreated time preceding the treatment for each treatment type. We identified age and sex as confounders potentially affecting the prevalence rates of comorbidities. In order to attenuate possible differences in age between the treatment groups, we compared the prevalence rates of the comorbidities during 5 years before initiation of anti-psoriasis treatment after standardization by age. The overall Swedish age distribution in 2013 was used as the standard. Since the prevalence of CVDs is different between sexes, subgrouping was used to handle this confounding. As measure of precision 95% CIs were calculated around the prevalence rates. To compare the results between the 3 different treatment groups, we used overlaps of the 95% CIs to assess statistical significance. We moreover compared our results with the prevalence of the comorbidities in the general population, which was retrieved from other studies in Sweden or from The National Board of Health and Welfare. Analyses were carried out using SAS® version 9.4, SAS Institute, Cary, NC, USA and STATA version 12 (College Station, TX: StataCorp LP).
Results
presents the baseline characteristics of the study population by treatment group/psoriasis severity. Patients with severe psoriasis, that is, those starting a biologic treatment, were younger (median 44 years, interquartile range [IQR]: 34–55) than the patients with a moderate-to-severe psoriasis (starting a non-biologic systemic treatment) (median 52 years, IQR: 41–62) or with a mild psoriasis (starting a topical treatment) (median 55 years, IQR: 41–66). We further found that treatment with biological drugs increased – in absolute number of individuals – during the study period, while treatment with non-biological systemic drugs did not change substantially, and topical treatment decreased.
Table 1 Baseline characteristics of adult patients with psoriasis by treatment groups
The standardized rates of comorbidities at baseline in the 3 different treatment categories are presented in , with 95% CI. Major cardio- and cerebrovascular diseases were less common in patients starting biologic treatment/severe disease (point estimate [95% CI]); MI: 1.82% (1.29–2.47), Stroke: 1.07% (0.68–1.60) compared with moderate-to-severe patients starting non-biological systemic treatment; MI: 2.30% (2.03–2.58), Stroke: 2.16% (1.90–2.43) and mild patients starting topical treatment; MI: 2.50% (2.39–2.62), Stroke: 2.42% (2.31–2.53). With regard to MDs and HTN, the standardized rates were similar between the groups but higher in the population of patients starting biologic treatments, despite their younger age, for example, HTN: starters of biologic treatment: 36.47% (34.42–38.55); non-biological systemic treatment: 32.62% (31.77–33.47); and topical treatment: 29.88% (29.54–30.21); and diabetes: starters of biologic treatment: 10.67% (9.39–12.05); non-biological systemic treatment: 8.00% (7.52–8.51); and topical treatment: 7.60% (7.41–7.80).
Table 2 Age-standardized prevalence of baseline comorbidities in adult patients with psoriasis by severity of the disease
Estimating the prevalence rates by sex showed that the prevalence of MI and stroke was higher among men. However, the decreasing pattern of the prevalence of these diseases is almost the same by severity. Moreover, although the increasing pattern of the prevalence of the risk factors of CVDs: HTN and DM, by sex is similar to the overall results, the prevalence of these comorbidities is higher among females with moderate-to-severe and severe psoriasis than in men ().
Discussion
In this large population-based cross-sectional study, using Swedish national health registers, we identified >80,000 patients with psoriasis (or psoriatic arthritis) receiving anti-psoriatic treatment between 1 July 2007 and 31 December 2013. Close to 75,000 patients started a topical treatment with calcipotriol – suffering from mild psoriasis; around 12,000 patients started treatment with non-biological systemic drugs – assumed to suffer from moderate-to-severe psoriasis; and ~2200 started a biologic regimen – the patient group with presumably the most severe psoriasis. Including only naïve users and applying hierarchical classification led to a higher proportion of mild cases and a lower proportion of severe cases than observed in other studies. The 3 groups were investigated and compared with regard to cerebro- and cardiovascular comorbidities and selected early risk factors during a 5-year period before starting treatment (a 2-year period for conditions identified by dispensed prescribed drugs). We found that the standardized prevalence of the major cardio- and cerebrovascular outcomes (i.e., MI and stroke) were less frequent in patients with severe psoriasis, as would be expected since this population is younger than those with a mild or moderate-to-severe condition. On the contrary, conditions representing early risk factors for CVD events, were as common or more common in patients with severe psoriasis, despite their younger age. Therefore, at the start of biologic treatment, the more severely ill psoriasis patients appear to already suffer from early warning signs for a serious condition that has yet to manifest.
Consistent with previously published studies, our study shows that the prevalence of CVDs may be influenced by severity of psoriasis. Al-Mutairi et alCitation23 conducted a case–control study on 1835 patients with psoriasis vulgaris and their matched non-psoriatic controls. They found that the prevalence of HTN was 32.0%, 40.3%, and 11.6% among those with mild-to-moderate psoriasis, severe psoriasis, and controls, respectively. Through a meta-analysis of observational studies, Armstrong et alCitation14 have concluded that patients with severe psoriasis have a higher risk of HTN compared with mild psoriatic patients. In the present study, the age-standardized prevalence of HTN was found to be 29.9%, 32.6%, and 36.5% among patients with mild, moderate-to-severe, and severe psoriasis, respectively.
Compared with the prevalence of HTN in the general population of Sweden (20%),Citation24 the results from our study show an approximately 2-fold higher prevalence of HTN in severe psoriasis patients. In this study, the prevalence of other CVDs, for example, MI or stroke was found to be 2.5%, 2.3%, and 1.8% for MI, and 2.4%, 2.2%, and 1.1% for stroke in patients with mild, moderate-to-severe, and severe psoriasis, respectively. This is higher than the prevalence of these diseases in the general population of Sweden (MI: 0.4%, stroke: 0.3%).Citation25,Citation26
Respective prevalence rates of DM in mild, moderate-to-severe, and severe psoriasis in our study were 7.6%, 8.0%, and 10.7%. The observed increasing prevalence of DM is supported by previous studies showing increased prevalence of DM with increasing severity of psoriasis. Neimann et alCitation15 have shown, through a cross-sectional study in the UK, that the prevalence of DM is 4.4% and 7.1% among patients with mild and severe psoriasis, respectively, compared with non-psoriatic controls with a prevalence of 3.3%. Al-Mutairi et alCitation23 have reported the prevalence of DM (type 2) among psoriatic patients as: 37.4% in mild-to-moderate psoriasis, 41.0% in severe psoriasis, and 16.0 % in control patients without psoriasis. Despite the similarity of the direction between the previousCitation15,Citation23 and this study, the variability observed might originate from differences in the definition of the psoriasis severity. In Neimann et alCitation15 all patients who received psoralen, phototherapy, methotrexate, azathioprine, cyclosporine, etretinate, acitretin, hydroxyurea, and mycophenolate were considered as severe psoriasis patients and biological treatments were not used in that study. Moreover, the registry used only records visits to general practitioners, while our study covers specialist clinics, hospital admissions, as well as general practitioner visits estimated from prescription claims. In Al-Mutairi et alCitation23 the Psoriasis Area Severity Index (PASI) was used to measure the severity of the psoriasis and the outcome of interest was type 2 diabetes. We also compared comorbidity rates with the general population of Sweden, and found that the prevalence of DM in our study is higher than that of the general population: a total of 7.6%, 8.0%, and 10.7% in the mild, moderate-to-severe, and severe groups, respectively, versus 6.2 %Citation27 to 6.8%Citation28 in the Swedish general population.
One explanation of higher prevalence of risk factors and lower prevalence of the major events of CVDs in the severe psoriasis group (younger patients) could be the nature of the psoriasis. Psoriasis onset at a younger age (≤40 years old) or early-onset diseaseCitation29,Citation30 has been shown to have a higher inflammatory reaction, extensive cutaneous involvement, and more severe clinical courseCitation31–Citation33 compared with older age/late onset of psoriasis. Therefore, it is reasonable to expect a higher rate of the CVD risk factors, such as HTN and DM among younger psoriasis patients due to a possible shared pathologic mechanism between CVDs and psoriasis. With regard to major cardiovascular events, such as MI or stroke, it may be that these events need a longer time to manifest. Therefore, it could be expected to find a higher rate of early risk factors of CVDs while the prevalence of the major events of CVDs is yet to manifest in our data due to right censoring.
The strengths of our study include the population-based design, the national coverage of the registers being close to 100%, the long study period, and the large sample size compared with prior works. By use of both NPR and PDR, we were able to include as many patients as possible with psoriasis (including psoriatic arthritis) in the study, that is, patients treated in both primary care and by specialists at hospitals. This study is the first Swedish nationwide investigation on prevalence of CVD and DM among psoriatic patients. Our findings support existing information on the prevalence of these comorbidities among psoriasis patients. Our study also used a 5-year period before starting the anti-psoriatic treatments to quantify the prevalence of comorbidities. Our results could be generalized to similar populations due to its population-based design and large sample size. A limitation of our study is using treatment types to measure psoriasis severity. A more direct severity measure, such as PASI is more ideal, however, these data are not captured in Swedish national health registers. However, using anti-psoriatic treatment as a proxy for severity of the disease has been estimated to have a sensitivity and positive predictive value of more than 90% and 80%, respectively.Citation20,Citation21 A second potential limitation is the overlap between mild and moderate-to-severe treatment groups, when we use the treatment as a proxy. For example, some types of psoriasis, such as guttate psoriasis are frequently treated with cyclosporine even when these cases are considered mild. However, this did not have a major impact on our results as the prevalence of guttate psoriasis is low (around 2%)Citation34 and typically occurs in children who were excluded from this study. A third potential limitation is due to the lack of coverage of PDR for drugs prescribed at a hospital. Some drugs, such as infliximab, are prescribed in hospital and do not appear in PDR. There may be an underestimation for drugs prescribed at hospitals when we rely on the PDR to create the treatment groups. Fourth, we also lacked information on physical activity, tobacco use, diet, and central obesity as these are not available in the national Swedish registers. As the last limitation, we had no information about the indication for the drugs prescribed: both non-biological systemic drugs and biologics can be used for other indications beyond psoriasis and psoriatic arthritis. However, all patients except those identifying just in PDR (calcipotriol users in primary health care centers) had a diagnosis of psoriasis or psoriatic arthritis recorded in the NPR.
Conclusion
Despite the younger age of patients with severe psoriasis, that is, those starting a biologic treatment, the prevalence of early risk factors for cardio- and cerebrovascular disease was higher than in the older patients with a mild or moderate-to-severe psoriasis, or those starting a topical or non-biologic systemic treatment. A health policy implication from our results is that all patients suffering from severe psoriasis should be carefully monitored with regard to signs and symptoms of metabolic conditions as early signs of cerebro- and cardiovascular disease.
Author contributions
MH had full access to all data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. AS, ML, and IAB performed the study concept and design. MH performed the analysis and AS, ML, IAB, DH and MH performed the interpretation of data. MH drafted the manuscript. All co-authors performed critical revision of the manuscript for important intellectual content. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This project was funded via the public–private real world evidence collaboration between Karolinska Institutet and Janssen Pharmaceuticals (contract: 5–63/2015).
Supplementary materials
Figure S1 The patient flow diagram of creating treatment group datasets among the cohort of psoriasis patients.
Notes: aNational Patient Register. bPrescribed Drug Register. cTopical treatment: calcipotriol or calcipotriol combinations. dNon-biological systemic treatment: methotrexate, cyclosporine, acitretin and phototherapy. eBiological treatment: adalimumab, etanercept, infliximab, efalizumab, ustekinumab, certolizumab, golimumab.
Abbreviations: ATC, Anatomical Therapeutic Chemical Classification System; BMI, body mass index; CVD, cardiovascular diseases; DM, diabetes mellitus; HTN, hypertension; IQR, interquartile range; MD, metabolic disease; MI, myocardial infarction; NPR, National Patient Register; PASI, psoriasis area and surface index; PDR, Prescribed Drug Register.
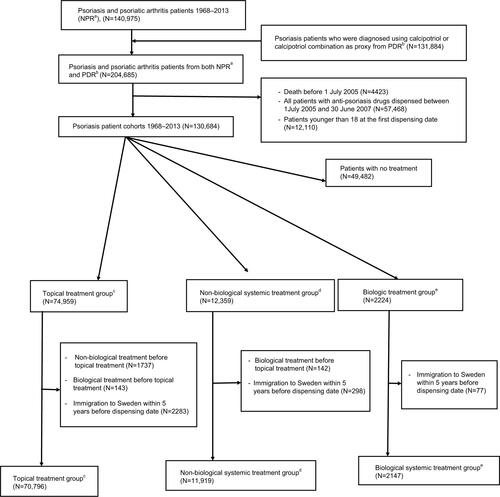
Table S2 List of ATC codes used for identifying the treatment groups
Table S3 List of the codes that were used as comorbidities in the study
Table S4 Age-standardized prevalence of baseline comorbidities in adult patients with psoriasis by severity of the disease and sex
References
- BremanderAJacobssonLTBergmanSHaglundELofvendahlSPeterssonIFSmoking is associated with a worse self-reported health status in patients with psoriatic arthritis: data from a Swedish population-based cohortClin Rheumatol201534357958325024097
- KristensenLEJorgensenTSChristensenRSocietal costs and patients’ experience of health inequities before and after diagnosis of psoriatic arthritis: a Danish cohort studyAnn Rheum Dis20177691495150128137915
- LudvigssonJFLindelofBZingoneFCiacciCPsoriasis in a nationwide cohort study of patients with celiac diseaseJ Invest Dermatol2011131102010201621654830
- OhEHRoYSKimJEEpidemiology and cardiovascular comorbidities in patients with psoriasis: A Korean nationwide population-based cohort studyJ Dermatol201744662162928191654
Disclosure
The authors report no conflicts of interest in this work.
References
- DanielsenKOlsenAOWilsgaardTFurbergASIs the prevalence of psoriasis increasing? A 30-year follow-up of a population-based cohortBr J Dermatol201316861303131023374051
- WHOGlobal report on psoriasis2016World Health Organization Available from: http://www.who.int/iris/handle/10665/204417Accessed May 1, 2018
- ChristophersEPsoriasis− epidemiology and clinical spectrumClin Exp Dermatol200126431432011422182
- ParisiRSymmonsDPGriffithsCEAshcroftDMIdentification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project teamGlobal epidemiology of psoriasis: a systematic review of incidence and prevalenceJ Invest Dermatol2013133237738523014338
- DuffinKCIdentifying and managing complications and comorbidities in patients with psoriasisPaper presented at: Seminars in Cutaneous Medicine and Surgery2015
- ShahKMellarsLChangolkarAFeldmanSRReal-world burden of comorbidities in US patients with psoriasisJ Am Acad Dermatol2017772287292.e428623046
- ThomasJKumarNAManoharanDCynthiaSPrabuSSAhmedNAA study of comorbid conditions in psoriasisJ Pak Assoc Dermatol2016194200202
- ArmestoSCoto-SeguraPOsunaCCamblorPSantos-JuanesJPsoriasis and hypertension: a case-control studyJ Eur Acad Dermatol Venereol201226678578821569114
- CohenADWeitzmanDDreiherJPsoriasis and hypertension: a case-control studyActa Derm Venereol2010901232620107721
- GottliebABDannFComorbidities in patients with psoriasisAm J Med2009122121150.e1e9
- NiCChiuMWPsoriasis and comorbidities: links and risksClin Cosmet Investig Dermatol20147119132
- YeungHTakeshitaJMehtaNNPsoriasis severity and the prevalence of major medical comorbidity: a population-based studyJAMA Dermatol2013149101173117923925466
- MehtaNNYuYPinnelasRAttributable risk estimate of severe psoriasis on major cardiovascular eventsAm J Med20111248775.e1e621787906
- ArmstrongAWHarskampCTArmstrongEJThe association between psoriasis and hypertension: a systematic review and meta-analysis of observational studiesJ Hypertens201331343344323249828
- NeimannALShinDBWangXMargolisDJTroxelABGelfandJMPrevalence of cardiovascular risk factors in patients with psoriasisJ Am Acad Dermatol200655582983517052489
- LudvigssonJFAnderssonEEkbomAExternal review and validation of the Swedish national inpatient registerBMC Public Health201111145021658213
- WettermarkBHammarNForedCMThe new Swedish prescribed drug register-opportunities for pharmacoepidemiological research and experience from the first six monthsPharmacoepidemiol Drug Saf200716772673516897791
- WHOWHO collaborating center for Drug Statistics Methodology2016 Available from: https://www.whocc.no/atc_ddd_indexAccessed June 26, 2016
- LudvigssonJFAlmqvistCBonamyAKRegisters of the Swedish total population and their use in medical researchEur J Epidemiol201631212513626769609
- EgebergAGyldenloveMZachariaeCSkovLValidation of psoriasis severity classification based on use of topical or systemic treatmentJ Eur Acad Dermatol Venereol2018321e4e528646609
- LoftNSkovLBryldLEGislasonGEgebergATreatment history of patients receiving biologic therapy for psoriasis – a Danish nationwide studyJ Eur Acad Dermatol Venereol2017318e362e36328168750
- NorlinJMSteen CarlssonKPerssonUSchmitt-EgenolfMResource use in patients with psoriasis after the introduction of biologics in SwedenActa Derm Venereol201595215616124819980
- Al-MutairiNAl-FaragSAl-MutairiAAl-ShiltawyMComorbidities associated with psoriasis: an experience from the Middle EastJ Dermatol201037214615520175849
- LindbladUEkJEcknerJLarssonCAShanGRåstamLPrevalence, awareness, treatment, and control of hypertension: rule of thirds in the Skaraborg projectScand J Prim Health Care2012302889422643153
- HammarNAlfredssonLRosenMSpetzCLKahanTYsbergASA national record linkage to study acute myocardial infarction incidence and case fatality in SwedenInt J Epidemiol200130Suppl 1S30S3411759848
- MalkiNKoupilIElorantaSTemporal trends in incidence of myocardial infarction and ischemic stroke by socioeconomic position in Sweden 1987–2010PLoS One201498e10527925170919
- CarlssonACWändellPÖsbyUZarrinkoubRWettermarkBLjunggrenGHigh prevalence of diagnosis of diabetes, depression, anxiety, hypertension, asthma and COPD in the total population of Stockholm, Sweden–a challenge for public healthBMC Public Health201313167023866784
- AnderssonTAhlbomACarlssonSDiabetes prevalence in Sweden at present and projections for year 2050PLoS One20151011e014308426619340
- RahmanPSchentagCTGladmanDDImmunogenetic profile of patients with psoriatic arthritis varies according to the age at onset of psoriasisArthritis Rheum199942481882310211900
- SmithAEKassabJYRowland PayneCMBeerWEBimodality in age of onset of psoriasis, in both patients and their relativesDermatology199318631811868453143
- FerrándizCPujolRMGarcía-PatosVBordasXSmandíaJAPsoriasis of early and late onset: a clinical and epidemiologic study from SpainJ Am Acad Dermatol200246686787312063483
- KwonHHKwonIHYounJIClinical study of psoriasis occurring over the age of 60 years: is elderly-onset psoriasis a distinct subtype?Int J Dermatol2012511535822182378
- MelskiJWSternRSThe separation of susceptibility to psoriasis from age at onsetJ Invest Dermatol19817764744777310171
- LangleyRGKruegerGGGriffithsCEPsoriasis: epidemiology, clinical features, and quality of lifeAnn Rheum Dis200564Suppl 2ii18ii2315708928
