Abstract
Purpose
To examine the association between selective serotonin reuptake inhibitor (SSRI) use and mortality, postoperative complications, and quality of in-hospital care in hip fracture patients.
Patients and methods
The study was a nationwide cohort study based on individual-level linked, prospectively collected data from Danish population-based national registries covering all hospitals in Denmark. The health care system in Denmark is tax-funded, and all citizens have equal access to health care services. We included patients with first-time hospitalization due to hip fracture undergoing surgery from 2006–2016. We estimated the risk of 30-day mortality, any unplanned readmission, any reoperation, specific postoperative complications including cardiovascular events and major bleeding, and quality of in-hospital care using Cox and Poisson regression analyses comparing current and former SSRI users with non-users.
Results
In 68,487 hip fracture patients, 13,272 (19%) were current SSRI users, 2,777 (4%) were former SSRI users, and 52,438 (77%) were SSRI non-users. The 30-day mortality risk was 13% in current SSRI users (HR 1.16, 1.10–1.21) and 12% in former (HR 1.15, 1.04–1.27) compared with 10% in non-users. The HR for any unplanned readmission was 1.11 (1.02–1.20) in current and 1.13 (1.01–1.27) in former SSRI users and for any reoperation 1.21 (1.11–1.31) in current and 1.04 (0.84–1.28) in former SSRI users compared with non-users. The risk of venous thromboembolism, myocardial infarction, stroke, and bleeding were similar irrespective of SSRI use. No association between current and former SSRI use and quality of in-hospital care was found.
Conclusion
In patients undergoing hip fracture surgery, 30-day mortality and overall readmission risk were elevated in both current and former SSRI users compared with non-users. Those currently using SSRI had a 26% increased reoperation risk compared with non-users. However, SSRI use was not associated with increased risk of other postoperative complications and lower quality of in-hospital care. A limitation of this study was the inability to control for potential confounding of social deprivation.
Introduction
Hip fracture is a frequent surgical procedure among the elderly.Citation1 It correlates with high medical costs and health care utilizationCitation2 and confers increased risk of mortality.Citation3 Thirty-day mortality in elderly surgically treated hip fracture patients is 10% and increases to 30% within 1 year.Citation4 Patients who receive the recommended pre- and postoperative in-hospital care such as pain assessment, nutritional risk assessment, osteoporosis prophylaxis, and basic mobility assessment at admission and discharge may have a lower mortality risk compared with those who do not.Citation5 Additionally, high mortality is linked to the occurrence of postoperative complications, which affect ~20% of elderly hip fracture patients.Citation5,Citation6 The most common postoperative complication is infection.Citation4 However, patients can experience venous thromboembolism (VTE), myocardial infarction (MI), stroke, and gastrointestinal bleeding as well.Citation4,Citation7
Elderly hip fracture patients are often multimorbid and receive multiple prescription medications including selective serotonin reuptake inhibitors (SSRIs).Citation8 SSRIs are prescribed to 10% of Danish elderly aged 65 years or older.Citation9 The most common indications for SSRI prescribing are depression and anxiety.Citation10 In general, SSRI use appears to increase the risk of mortality, new cardiovascular events, and postoperative bleeding.Citation6,Citation11 Previous studies among patients undergoing major surgery, including orthopedic surgeries, reported higher risk of mortality, readmission, and blood transfusion in those using SSRIs perioperatively.Citation12,Citation13 However, a study including orthopedic patients showed no evidence that SSRI use increased the risk of receiving a blood transfusion.Citation14 Thus, existing literature examining the effect of SSRI use on surgery outcome is somewhat inconclusive. The impact of preadmission SSRI use on mortality, postoperative complications, and quality of in-hospital care among elderly and fragile hip fracture patients has not been reported previously. Therefore, we conducted a nationwide, prospective cohort study examining whether preadmission SSRI use is associated with adverse outcomes in hip fracture surgery patients.
Ethics approval
Ethical approval was not required according to the Danish Act on Research Ethics Review of Health Research Projects due to the register-based nature of the study. The study was approved by the Danish Data Protection Agency (record number: 1-16-02-467-15).
Patients and methods
Setting and design
The study is a nationwide cohort study using prospectively collected data from Danish medical registries covering all Danish citizens; approximately 5.7 million people.Citation15 The health care system in Denmark is tax-funded, and all citizens have equal access to health care services.
Data sources
The Danish Multidisciplinary Hip Fracture RegistryCitation16 has routinely registered comprehensive clinical data on all patients aged 65 years or older with first-time hip fracture admitted to any orthopedic department in Denmark since 2004. Data include detailed pre- and postoperative data, as well as data on quality of in-hospital care represented by process-performance measures. The Danish Civil Registration SystemCitation17 established in 1968 holds data on date of birth, vital status, and migration on all individuals in Denmark. Every citizen has a unique civil personal registration number, which allows for individual-level linkage across all Danish registries. The Danish National Patient RegistryCitation18 contains data on civil personal registration number, hospital admission and discharge diagnosis codes, and diagnostic and surgical procedure codes from all Danish somatic hospitals since 1977. Diagnoses were coded using the ICD-8 until the end of 1993 and ICD-10 thereafter. The Danish National Database of Reimbursed PrescriptionsCitation19 tracks reimbursed medicine dispensing at all community pharmacies and hospital-based outpatient pharmacies in Denmark since 2004. The database holds data on civil personal registration number, Anatomical Therapeutic Chemical code, redemption date, item quantity, pack size, defined daily dose, dose form, and generic substitution done at pharmacy.
Participants
Patients aged 65 years or older undergoing surgical treatment for hip fracture between 2004 and 2016 were identified in the Danish Multidisciplinary Hip Fracture Registry. The study period was subsequently restricted to patients registered between January 1, 2006, and December 31, 2016, to ensure at least 2 years prescription history. Patients with missing data on operation delay (n=119) were excluded. In total, 68,487 first-time hip fracture patients who received surgery from 2006–2016 were available for analyses.
Variables
Exposure
All redeemed prescriptions for SSRIs 1 year before hip fracture surgery were identified in the Danish National Database of Reimbursed Prescriptions. Patients were classified according to SSRI use. Current SSRI users redeemed at least one prescription within 90 days, former users redeemed one prescription between 91 and 365 days, and non-users redeemed no prescriptions within 365 days before hip fracture surgery.
Outcomes
Several outcomes occurring after hip fracture surgery were examined separately. First, all-cause 30-day mortality was ascertained from the Civil Registration System. Second, postoperative complications were ascertained from the Danish National Patient Registry. The following postoperative complications were examined: 1) any unplanned readmission, 2) any reoperation, 3) cardiovascular events including VTE, MI, and stroke, and 4) major bleeding defined as intracranial bleeding, gastrointestinal bleeding, or urinary/lung bleeding within 30 days of surgery. Third, quality of in-hospital care represented by process-performance measuresCitation20 including preoperative optimization, operation delay, mobilization within 24 hours postoperatively, basic mobility assessment at admission and discharge, nutritional risk assessment, osteoporosis prophylaxis, and future fall prophylaxis were obtained from the Danish Multidisciplinary Hip Fracture Registry.
Covariates
Operation year, housing, BMI, fracture type, operation type, and operation delay information was assessed from the Danish Multidisciplinary Hip Fracture Registry. Four categories comprising housing information were created: own accommodation, residential institution, homeless, and unknown. Likewise, four categories based on BMI values were created: underweight (BMI <18.5 kg/m2), normal weight (BMI ≥18.5 <25 kg/m2), overweight or obese (BMI ≥25 kg/m2), and unknown. Age, gender, and marital status were obtained from the Danish Civil Registration System. Comorbidities were identified using the Danish National Patient Registry. Overall comorbidity was summarized according to the original Charlson Comorbidity Index (CCI) score. The CCI was categorized as low (score 0), medium (score 1–2), and high (score ≥3) comorbidity score, slightly modified compared with the original CCI.Citation21 The following medications were assessed from the Danish National Database of Reimbursed Prescriptions: non-steroidal anti-inflammatory drugs, corticosteroids, anticoagulants, statins, non-SSRI antidepressants, and antipsychotics. Use of each medication was defined as follows: current users redeemed one prescription within 90 days, former users redeemed one prescription between 91 and 365 days, and non-users redeemed no prescriptions within 365 days before hip fracture surgery. All codes defining study variables are available in –.
Statistical methods
Main analyses
Patient characteristics were tabulated according to SSRI use. All patients were followed from operation date to death, any unplanned readmission, any reoperation, cardiovascular event, bleeding event, or up to 30 days. Kaplan–Meier curves of the three SSRI exposure groups were plotted depicting the absolute mortality risk over time. The cumulative incidence of postoperative complications was estimated treating death as a competing risk. Crude and adjusted HRs with 95% CIs of death and postoperative complications within 30 days were estimated using Cox regression analysis comparing current and former SSRI users with non-users. The mortality model was evaluated for effect modification by age and gender. Readmission outcome data were only available for patients operated on from January 1, 2011 onward, thus readmission analyses were restricted to patients operated on between January 1, 2011 and December 31, 2016. RRs of quality of in-hospital care were estimated using Poisson regression analysis. The process-performance measures representing quality of in-hospital care were introduced in the Danish Multidisciplinary Hip Fracture Registry at various times. Therefore, the analyses regarding the quality of in-hospital care were performed only in hip fracture patients operated on between January 1, 2015 and December 31, 2016. Potential confounder assessment was done using a directed acyclic graph ().Citation22 All adjusted analyses accounted for age, gender, marital status, operation year, comorbidities, other medication, and clustering by unit setting.
Sensitivity analysis
Two sensitivity analyses were performed to test the robustness of the results. First, missing BMI values were imputed using multiple imputation (Supplementary materials).Citation23 Missing housing data were not imputed due to lack of predictors. Second, the exposure definition was changed to address potential compliance problems; current SSRI users redeemed two prescriptions within 2 years, of which one prescription was redeemed within 8 months before hip fracture, former users redeemed two prescriptions between 8 months and 2 years, and non-users redeemed one or no prescriptions within 2 years before hip fracture. The mortality analysis was repeated including BMI in the Cox regression model and employing a new exposure definition. Cox and Poisson regression analyses were performed using Stata 14 for Windows (StataCorp LP, College Station, TX, USA). The Kaplan–Meyer plot was produced using R for Windows 3.4.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
We identified 68,487 first-time hip fracture patients between 2006 and 2016. Of these, 13,272 (19%) were current SSRI users, 2,777 (4%) former, and 52,438 (77%) non-users. presents the patient characteristics according to SSRI use. The median patient age was 84 years in current users (IQR 78–89 years) and 83 years in former users (IQR 77–88 years) and non-users (IQR 77–89 years). The current and former SSRI users had higher overall comorbidity than non-users, as well as higher prevalence of cerebrovascular disease, dementia, use of non-SSRI antidepressants, and antipsychotics. Current SSRI users had a higher prevalence of anticoagulant use than both former users and non-users ().
Table 1 Baseline characteristics of hip fracture patients (n=68,487) according to preoperative selective serotonin reuptake inhibitor use 2006–2016
In total, 13,295 patients (19%) were missing BMI data and 30,285 (44%) patients were missing housing data. From the available housing data, we observed that SSRI non-users (25,537 [49%]) more often lived in their own accommodation compared with current (4,412 [33%]) and former (1,126 [41%]) users. However, there was no difference in BMI distribution between the exposure groups ().
Mortality
Overall, 7,295 hip fracture patients died within the first 30 days following hip fracture surgery. Mortality was higher in current (13%) and former (12%) users compared with non-users (10%) ( and ). Compared with nonusers, the adjusted HR was 1.16 (1.10–1.21) in current users and 1.15 (1.04–1.27) in former users (). We found no effect modification by age and gender of the relation between SSRI use and mortality.
Figure 1 Kaplan–Meyer survival curve showing mortality in hip fracture patients according to selective serotonin reuptake inhibitor (SSRI) use 2006–2016.
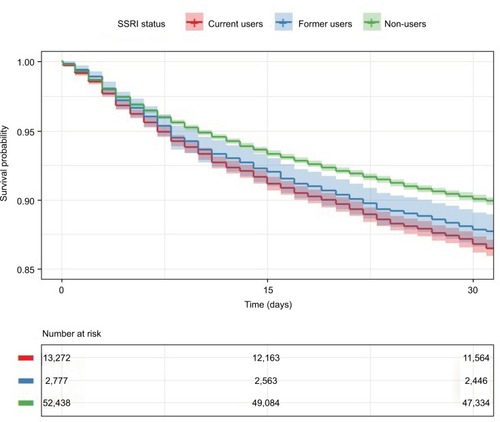
Table 2 Cumulative incidences and HRs with 95% CIs of mortality, readmission, reoperation, and postoperative complications within 30 days of hip fracture surgery according to selective serotonin reuptake inhibitor (SSRI) use 2006–2016 (N=68,487)
Readmission and reoperation
shows cumulative incidences and HRs of any unplanned readmission and any reoperation within 30 days postoperatively. In total, 6,208 of 36,356 were readmitted and 2,327 of 68,487 re-operated within 30 days after surgery. Both current (HR 1.11, 1.02–1.20) and former users (HR 1.13, 1.01–1.27) had a higher readmission risk compared with non-users. Current SSRI users had a higher reoperation risk (HR 1.21, 1.11–1.31) compared with non-users while there was no difference between former users (HR 1.04, 0.84–1.28) and non-users.
Other postoperative complications
During the first 30 days following hip fracture surgery, 573 patients experienced VTE, 546 MI, 863 stroke, and 1,011 major bleeding. shows cumulative incidences and HRs of the individual complications. Current SSRI users had a similar risk of VTE (HR 0.89, 0.67–1.17), MI (HR 1.03, 0.81–1.30), stroke (HR 0.93, 0.80–1.09), and bleeding (HR 1.06, 0.89–1.28) as non-users. Likewise, former SSRI users had a similar risk of VTE (HR 0.93, 0.64–1.35), MI (HR 0.89, 0.57–1.40), stroke (HR 0.67, 0.44–1.01), and bleeding (HR 1.06, 0.69–1.64) as non-users.
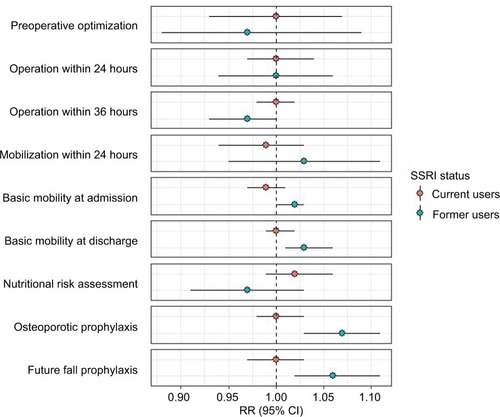
Quality of in-hospital care
The analyses included 11,363 patients operated on during 2015–2016. shows a marginally higher chance of assessment of basic mobility at discharge, osteoporosis prophylaxis, and future fall prophylaxis in former SSRI users compared with non-users. Overall, there was no association between current and former SSRI use and quality of in-hospital care ().
Figure 2 Adjusted RRs with 95% CIs of quality of in-hospital care comparing current and former selective serotonin reuptake inhibitor (SSRI) users with non-users (reference) 2015–2016 (N=11,363).
Sensitivity analysis
The HRs of mortality did not materially change after multiple imputation of missing BMI values and adjustment for BMI ( and ). Changing the exposure definition, we identified 14,530 (21%) current SSRI users, 1,116 (2%) former users, and 52,841 (77%) non-users. Patient characteristics in the new exposure groups were similar to the patient characteristics of the exposure groups used in the main analysis and the HRs of mortality were similar to the main analysis results ( and ).
Discussion
In this nationwide cohort study of hip fracture surgery patients, 30-day mortality and overall readmission were elevated for both current and former SSRI users. Those currently using SSRIs had an increased reoperation risk compared with non-users. However, SSRI use was not associated with increased risk of cardiovascular and bleeding complications and inferior quality of in-hospital care.
Strengths and limitations
The strengths of this study are the use of well-established, well-validated, and prospectively collected data from Danish population-based registries with complete follow-up.Citation19,Citation24–Citation26 The registries originate from a tax-supported and uniformly organized health care system, reducing the risk of selection bias. The validity of the hip fracture diagnosis is high,Citation27,Citation28 and the complete follow-up reduces the risk of differential misclassification. In general, our study included all elderly hip fracture patients aged 65 years or older in Denmark between 2006 and 2016. These patients are similar regarding age and gender to those included in other studies on hip fractures in the elderly.Citation4,Citation7 To date, this is the largest study examining the association between SSRI use and mortality, postoperative complications, and quality of in-hospital care in hip fracture patients.
We gathered comprehensive data on potential confounders including complete in-hospital comorbidity history com piled in the CCICitation26 and history of specific diseases. However, we did not have information on the severity of diseases included in the CCI, on diseases treated in primary care, which were not severe enough to warrant a hospital diagnosis, or information on the underlying disease indication for SSRI prescription. However, we included information on other medication, which may indicate treatment of conditions not captured in the CCI. The registries we used did not contain information on socioeconomic status, smoking, alcohol use, and other lifestyle factors. Furthermore, almost half of the patients were missing data on housing, making control of confounding difficult. Thus, we were not able to control for the potential confounding of social deprivation and lack of these data may have resulted in unmeasured and residual confounding. Information on comorbidities, other medication, marital status, and unit setting may contribute to control of confounding, but is not an adequate measure of social deprivation.
We included former SSRI users as a negative control. That is, we anticipated that former users were more similar to current users than non-users regarding potential confounding factors such as socioeconomic status and lifestyle factors. Thus, if the effect of SSRI exposure on mortality was caused by the medication itself, we would anticipate only seeing an effect in current users and not in former users. However, this was not the case, and the observed association between SSRI use and mortality may rather be caused by underlying risk factors.Citation29
We did not have information about compliance. In our study, non-compliance would cause a misclassification of non-users as users, and therefore the observed association between SSRI use and mortality, readmission, or reoperation risk might actually be higher. However, as the patients redeemed the prescriptions, our estimates most likely reflect actual drug use. Even considering misclassification, dispensed prescriptions are considered a good measure of medication intake.Citation30 Furthermore, we had no data on in-hospital medication use. This may not have influenced the outcome since hip fracture surgery is an acute procedure with short length of hospital stay.
Comparison with other studies
We observed an equally increased mortality risk in current and former SSRI users. This suggests that rather than being a risk factor in itself, SSRI use may be a marker of underlying risk factors such as psychiatric illness, socioeconomic status, and lifestyle factors (smoking, alcohol misuse, and physical inactivity). These results are consistent with those obtained by Auerbach et al, showing an increased mortality in SSRI users compared with non-users after major surgery, including approximately 2% hip fracture surgeries.Citation12 However, the association found by Auerbach et al was attenuated in patients with depression suggesting that the underlying psychiatric indication for SSRI use may explain the increased risk rather than SSRIs in itself.Citation12 A meta-analysis by Maslej et al found an increased mortality in antidepressant users compared to non-users in the general population independent of treatment indication.Citation31 The most common indications for SSRI treatment are depression and anxietyCitation10 and a systematic review by Eaton et al showed that depression and anxiety correlate with increased mortality.Citation32 Mortality in hip fracture patients may also be influenced by socioeconomic status,Citation33 and Marinacci et al found an association between lower education level and mortality.Citation34 Lower education level is further associated with increased risk of psychiatric admission due to schizophrenia, alcoholism, drug dependency, affective psychosis, neurosis, and personality disorder.Citation35 Finally, Seitz et al found no difference in 30-day mortality between current (9.1%) and former (9.4%) serotonergic antidepressant users undergoing hip fracture surgery.Citation36 However, they did not include a non-user group, which distorts the association between SSRI use and mortality.
Our findings of an increased overall readmission risk in current and former SSRI users compared with non-users is consistent with the findings reported by Auerbach et al in major surgery patients. In their study, this association persisted in patients receiving SSRIs for depression, but not in patients receiving SSRIs for other reasons.Citation12 This also suggests that SSRI use may not be a risk factor in itself but a marker of underlying disease or risk factors. A meta-analysis by Pizzi et al found no association between SSRI use and readmission in patients with coronary heart disease and depression, further supporting our results that SSRI use may not be a risk factor in itself.Citation37
Another important finding was that current SSRI users had an increased reoperation risk compared with non-users, whereas the risk was not elevated in former users. A possible explanation for this could be that SSRI use may increase the likelihood of complications necessitating reoperation. There are different reasons for performing reoperation, eg, wound dehiscence, infection, and bleeding,Citation20 and these complications may be more frequent in SSRI users. Gärtner et al found an association between SSRI use and reoperation due to bleeding after breast cancer surgery.Citation38 However, Tully et al showed no association between serotonergic antidepressant use and reoperation due to infection or bleeding after coronary artery bypass graft surgery.Citation39 Further research is needed to establish the association between SSRI use and reoperation risk due to different causes in hip fracture patients.
We found little evidence of an association between SSRI and the risk of VTE, MI, stroke, and bleeding. To our knowledge, no other studies have investigated the association between SSRI use and the previously mentioned postoperative complications following hip fracture surgery. Auerbach et al found an association between SSRI use and postoperative bleeding in major surgery patients. However, they had a broader bleeding definition, including bleeding following procedure, and they included both acute and elective operations.Citation12 Tully et al showed no association between SSRI use and MI, stroke, or bleeding after coronary artery bypass graft surgery,Citation39 supporting our findings.
The present study did not find any difference between SSRI non-users and users regarding quality of in-hospital care. This is important and in line with efforts of European governments to reduce social inequality in treatment of patients.Citation40 However, we have no information on quality of patient care outside hospital settings. Previous research suggests lower 30-day mortality in hip fracture patients who received higher quality of care.Citation5 Quality of in-hospital care may not explain the increased mortality associated with SSRI use in our study.
Implications of findings
One issue emerging from our findings is the question about discontinuation of SSRI treatment after hip fracture surgery. Since hip fracture is an acute condition, it is not possible to stop treatment before surgery. Our analysis suggests that stopping SSRI treatment after surgery would not change the mortality and overall readmission since these were similar in current and former users compared with non-users. We found that overall reoperation was augmented in current users, but not in former users compared with non-users. However, pausing SSRI treatment without a complete discussion of the risks and benefits is unwarranted. Our findings call for increased clinical awareness of hip fracture patients using SSRIs as they may have an increased risk of mortality, unplanned readmission, and reoperation. This patient group may be more prone to adverse outcomes after surgery regardless of the indication for SSRI treatment and may benefit from improved models of care. The follow-up care in Denmark is carried out by the municipality. Our findings suggest that hip fracture patients currently or formerly using SSRIs may benefit from closer follow-up and better communication between hospital, municipality, and general practitioner. However, the content and implementation of such improvements are beyond the scope of this paper. In future studies, it may be relevant to investigate how social deprivation influences surgical outcomes for these patients.
Conclusion
Thirty-day mortality and overall readmission in hip fracture patients were elevated in both current and former SSRI users compared with non-users. Those currently using SSRIs had an increased overall reoperation risk compared with nonusers. However, SSRI use was not associated with increased risk of cardiovascular and bleeding complications and lower quality of in-hospital care.
Data availability
The authors are not authorized to share the data as it were assessed via the data custodian, ie, the Danish National Data Board.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgments
We thank the staff of the hospital departments caring for patients with hip fracture for their continuous effort and contribution to acquisition of the data in the Danish Multidisciplinary Hip Fracture Registry. The Independent Research Fund Denmark (grant number 6120–00034) funded this work. The funder had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The researchers are independent from the funder. The study results were presented at the Danish Orthopedic Society Congress in October 2017 and at the PhD Day at Aarhus University in January 2018.
Supplementary materials
Sensitivity analyses
Multiple imputation
Methods
In the multiple imputation model, we included all variables that were in the subsequent analysis model: selective serotonin reuptake inhibitors (SSRIs), age, gender, marital status, operation year, BMI, comorbidities, and other medication. Further more, some auxiliary variables such as operation delay, fracture type, operation type, and postoperative complications were included. Imputation of BMI values was done using truncated regression creating 20 imputed datasets. After imputation, the association between SSRI use and mortality was estimated in each imputed dataset. The measures of association from each imputed dataset were combined using Rubin’s rule.
Figure S1 Directed acyclic graph of the possible relationship between important covariates and mortality in hip fracture patients.
Abbreviations: SSRI, selective serotonin reuptake inhibitor; CCI, Charlson Comorbidity Index.
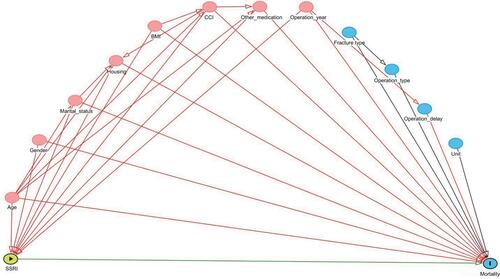
Table S1 ICD-8 and ICD-10 diagnosis codes from the Danish National Patient Registry
Table S2 Codes from the Danish Multidisciplinary Hip Fracture Registry
Table S3 Anatomical Therapeutic Chemical (ATC) codes from the Danish National Database of Reimbursed Prescriptions
Table S4 Unadjusted and adjusted RRs with 95% CIs of quality of in-hospital care according to selective serotonin reuptake inhibitor (SSRI) use 2015–2016 (N=11,363)
Table S5 Baseline characteristics of hip fracture patients (n=68,487) according to preoperative selective serotonin reuptake inhibitor (SSRI) use 2006–2016 after imputation of BMI
Table S6 Incidences and HRs with 95% CIs of mortality within 30 days of hip fracture surgery according to selective serotonin reuptake inhibitor (SSRI) use 2006–2016 (N=68,487) after imputation of BMI
Table S7 Baseline characteristics of hip fracture patients (n=68,487) according to preoperative selective serotonin reuptake inhibitor (SSRI) use 2006–2016 after changing the exposure definition
Table S8 Incidences and HRs with 95% CIs of mortality within 30 days of hip fracture surgery according to selective serotonin reuptake inhibitor (SSRI) use 2006–2016 (N=68,487) after changing the exposure definition
Disclosure
The authors report no conflicts of interest in this work.
References
- RequenaGAbbing-KarahagopianVHuertaCIncidence rates and trends of hip/femur fractures in five European countries: comparison using e-healthcare records databasesCalcif Tissue Int201494658058924687523
- PolinderSMeerdingWJvan BaarMECost estimation of injury-related hospital admissions in 10 European countriesJ Trauma20055961283129016394898
- de LuiseCBrimacombeMPedersenLSørensenHTComorbidity and mortality following hip fracture: a population-based cohort studyAging Clin Exp Res200820541241819039282
- RocheJJWennRTSahotaOMoranCGEffect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort studyBMJ20053317529137416299013
- NielsenKAJensenNCJensenCMQuality of care and 30 day mortality among patients with hip fractures: a nationwide cohort studyBMC Health Serv Res2009918619822018
- CouplandCDhimanPMorrissRArthurABartonGHippisley-CoxJAntidepressant use and risk of adverse outcomes in older people: population based cohort studyBMJ2011343d455121810886
- LawrenceVAHilsenbeckSGNoveckHPosesRMCarsonJLMedical complications and outcomes after hip fracture repairArch Intern Med2002162182053205712374513
- VieiraERPalmerRCChavesPHPrevention of falls in older people living in the communityBMJ2016353i141927125497
- Medstat.dk [homepage on the Internet]The Danish Health Data Authority Available from: http://medstat.dk/Accessed July 5, 2018
- NoordamRAartsNVerhammeKMSturkenboomMCStrickerBHVisserLEPrescription and indication trends of antidepressant drugs in the Netherlands between 1996 and 2012: a dynamic population-based studyEur J Clin Pharmacol201571336937525560052
- WuCSChangCMChenCYAssociation between antidepressants and venous thromboembolism in TaiwanJ Clin Psychopharmacol2013331313723277236
- AuerbachADVittinghoffEMaselliJPekowPSYoungJQLindenauerPKPerioperative use of selective serotonin reuptake inhibitors and risks for adverse outcomes of surgeryJAMA Intern Med2013173121075108123699725
- MovigKLJanssenMWde Waal MalefijtJKabelPJLeufkensHGEgbertsACRelationship of serotonergic antidepressants and need for blood transfusion in orthopedic surgical patientsArch Intern Med2003163192354235814581256
- van HaelstIMEgbertsTCDoodemanHJUse of serotonergic antidepressants and bleeding risk in orthopedic patientsAnesthesiology2010112363163620179499
- Statistics DenmarkStatistical Yearbook121th edCopenhagenStatistics Denmark2017
- SørensenHTChristensenTSchlosserHKPedersenLUse of Medical Databases in Clinical Epidemiology2nd edAarhusSUN-TRYK, Aarhus Universitet2009
- SchmidtMPedersenLSørensenHTThe Danish Civil Registration System as a tool in epidemiologyEur J Epidemiol201429854154924965263
- SchmidtMSchmidtSASandegaardJLEhrensteinVPedersenLSørensenHTThe Danish National Patient Registry: a review of content, data quality, and research potentialClin Epidemiol2015744949026604824
- JohannesdottirSAHorváth-PuhóEEhrensteinVSchmidtMPedersenLSørensenHTExisting data sources for clinical epidemiology: The Danish National Database of Reimbursed PrescriptionsClin Epidemiol2012430331323204870
- Centre for Clinical Epidemiology and Biostatistics NorthThe Danish Multidisciplinary Hip Fracture Register - National Annual Report 2017: The Danish Clinical Registries2017 Available from: https://www.sund-hed.dk/content/cms/62/4662_hofte-fraktur-%C3%A5rsrapport_2017.pdfAccessed August 7, 2018 Danish
- CharlsonMEPompeiPAlesKLMackenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- ShrierIPlattRWReducing bias through directed acyclic graphsBMC Med Res Methodol2008817018973665
- PedersenABMikkelsenEMCronin-FentonDMissing data and multiple imputation in clinical epidemiological researchClin Epidemiol2017915716628352203
- SundbøllJAdelborgKMunchTPositive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation studyBMJ Open2016611e012832
- WildenschildCMehnertFThomsenRWRegistration of acute stroke: validity in the Danish Stroke Registry and the Danish National Registry of PatientsClin Epidemiol20146273624399886
- ThygesenSKChristiansenCFChristensenSLashTLSørensenHTThe predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of PatientsBMC Med Res Methodol2011118321619668
- BaronJALu-YaoGBarrettJMclerranDFisherESInternal validation of Medicare claims dataEpidemiology1994555415447986870
- HudsonMAvina-ZubietaALacailleDBernatskySLixLJeanSThe validity of administrative data to identify hip fractures is high--a systematic reviewJ Clin Epidemiol201366327828523347851
- LawlorDATillingKDavey SmithGTriangulation in aetiological epidemiologyInt J Epidemiol20164561866188628108528
- SchneeweissSAvornJA review of uses of health care utilization databases for epidemiologic research on therapeuticsJ Clin Epidemiol200558432333715862718
- MaslejMMBolkerBMRussellMJThe mortality and myocardial effects of antidepressants are moderated by preexisting cardiovascular disease: a meta-analysisPsychother Psychosom201786526828228903117
- EatonWWMartinsSSNestadtGBienvenuOJClarkeDAlexandrePThe burden of mental disordersEpidemiol Rev20083011418806255
- ThorneKJohansenAAkbariAWilliamsJGRobertsSEThe impact of social deprivation on mortality following hip fracture in England and Wales: a record linkage studyOsteoporos Int20162792727273727098537
- MarinacciCGrippoFPappagalloMSocial inequalities in total and cause-specific mortality of a sample of the Italian population, from 1999 to 2007Eur J Public Health201323458258723302766
- TiikkajaSSandinSMalkiNModinBSparénPHultmanCMSocial class, social mobility and risk of psychiatric disorder--a population-based longitudinal studyPLoS One2013811e7797524260104
- SeitzDPBellCMGillSSRisk of perioperative blood transfusions and postoperative complications associated with serotonergic antidepressants in older adults undergoing hip fracture surgeryJ Clin Psychopharmacol201333679079824091859
- PizziCRutjesAWCostaGMFontanaFMezzettiAManzoliLMeta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart diseaseAm J Cardiol2011107797297921256471
- GärtnerRCronin-FentonDHundborgHHUse of selective serotonin reuptake inhibitors and risk of re-operation due to post-surgical bleeding in breast cancer patients: a Danish population-based cohort studyBMC Surg201010320096133
- TullyPJCardinalTBennettsJSBakerRASelective serotonin reuptake inhibitors, venlafaxine and duloxetine are associated with in hospital morbidity but not bleeding or late mortality after coronary artery bypass graft surgeryHeart Lung Circ201221420621422285303
- World Health Organization EuropeParma Declaration on Environment and Health. Fifth Ministerial Conference on Environment and HealthParmaItaly2010 Available from: http://www.euro.who.int/__data/assets/pdf_file/0011/78608/E93618.pdfAccessed August 07, 2018
