Abstract
Background
Burns are the main cause of accidental injury, and pneumonia is a common respiratory disease in humans.
Aim
The purpose of this study was to investigate the relationship between burn injury and pneumonia.
Patients and methods
A nationwide population-based cohort study was conducted using data from the National Health Insurance Research Database in Taiwan. We identified and enrolled 2,893 subjects with burn injury, who were individually matched to 2,893 subjects in the comparison group by using the propensity score. Furthermore, we used a self-controlled case-series design to estimate the temporal association between burn injury and pneumonia.
Results
Exposure to burn injury revealed a higher risk of pneumonia than that to non-burn injury within 1 year. The Cox proportional hazards model revealed that, compared with the non-burn injury, burn injury yielded a 2.39-fold (95% CI=1.44–3.96) increase in risk of pneumonia. The exposure period of burn injury within 30 days showed 2.76-fold increase in risk of pneumonia (95% CI=1.44–3.96) compared with that in the baseline period.
Conclusion
Burn injury was associated with a significant increased risk of pneumonia, especially occurring within 30 days.
Keywords:
Background
Burns are one of the major causes of traumatic injury in humans.Citation1 The etiology of burn injury is diverse, including injury from fire, boiling water, and electricity. Skin burns can be classified into three categories according to severity.Citation2 A first-degree burn involves injury to the epidermis, which may extend to the partial separation of epidermal and dermal layers. A second-degree burn extends injury to the entire epidermis and also to various parts of the dermis. A third-degree burn involves destruction of the entire epidermis and dermis and even damage to adipose tissue.Citation2,Citation3 Not only do burns affect skin tissue on the body’s surface, they can also induce pulmonary changes.Citation4 In an animal study, a burn injury covering 40% of the body surface area induced pulmonary microvascular dysfunction.Citation4 In another study, a serious burn increased pulmonary vascular permeability and decreased the PaO2:FiO2 ratio.Citation5
Pneumonia is a common respiratory infectious disease that involves the inflammation of the pulmonary parenchyma. Individuals can acquire pneumonia on the basis of various epidemiologies, pathogeneses, and risk factors. For example, community-acquired pneumonia can occur anywhere outside hospitals, such as households, schools, and work places.Citation6 By contrast, hospital-acquired pneumonia (HAP) can occur in hospitalized patients and outpatients.Citation7 Moreover, HAP occurs 48 hours or more after hospitalization and does not present on admission. For hospitalized patients, HAP can be divided into ventilator hospital-acquired pneumonia (V-HAP), in which pneumonia develops after endotracheal intubation over 48–72 hours, and nonventilator hospital-acquired pneumonia (NV-HAP).Citation7,Citation8 A similar pathogenesis may exist in patients with burn injury. Repeat hospitalization might be another risk for burn injury patients, especially the older patients, to acquire pneumonia. These patients were admitted to hospitals for many reasons such as wound coverage, sepsis, and rehabilitation. Respiratory infection was one of most diagnosis in the 30-days re- hospitalization.Citation9 Therefore, it is reasonable to expect that patients with burns have a higher risk of developing pneumonia, especially HAP. The etiologies of pneumonia include bacteria, viruses, fungi, and protozoa. For immunocompromised patients, pneumonia can be easily acquired when patients are exposed to pathogens from the air or opportunistic microbes that colonize in the buccal cavity or upper respiratory tract.Citation10 A similar pathogenesis may exist in patients with burn injury.
Pneumonia is a general clinical presentation of the respiratory system, whereas burns are always related to extensive cutaneous injury. Indeed, lung function was unable to be restored completely in burn patients, while burn injury led to impaired immune system and increased susceptibility to infectious complication.Citation11–Citation13 It is rational to expect that burn injury patients may have a higher risk to develop pneumonia. However, systemic study of the relationship between pneumonia and burn injury and the interaction between symptoms remains limited. It would be valuable to know whether burn injury increases the risk of pneumonia. We hypothesized that patients with burn injury have a higher risk of developing pneumonia than the non-burn injury patients.
Patients and methods
Study population
The Longitudinal Health Insurance Database (LHID) is managed by the Taiwan National Health Research Institutes and contains data from one million randomly sampled beneficiaries, featuring all outpatient and inpatient medical claims, including drug medications, medical operations, procedures, and fees. Moreover, the LHID does not hold any identifying patient data. The study was approved by the ethical review board of the Chung Shan Medical University Hospital (CSMU No.: 15061).
Study design
This study used a retrospective cohort design. Patients aged ≥18 years with burn injury (ICD Ninth Revision Clinical Modification [ICD-9-CM] codes 940–949) which required emergency skin wound treatment or hospitalization were recruited between January 1, 2010, and December 31, 2012. The index date was defined as the first date of the burn injury. To avoid the confounding of disease history, we excluded patients who received a diagnosis of pneumonia within half a year before the index date.
A comparison group of patients who had not suffered from burn injury between 2009 and 2013 was selected. First, we performed a 1:18 age and sex matching to provide an index date corresponding to the comparison group. During matching, we excluded patients who received a diagnosis of pneumonia before the index date. Second, a propensity score matching (1:1) was performed for the comparison group according to age, sex, hypertension (ICD-9-CM codes 401–405), hyperlipidemia (ICD-9-CM codes 272.0–272.4), diabetes mellitus (ICD-9-CM codes 250), cerebrovascular disease (ICD-9-CM codes 430–438), renal disease (ICD-9-CM codes 582–582.9, 583–583.7, 585, 586, 588–588.9), liver disease (ICD-9-CM codes 571.2, 571.5, 571.6, 571.4– 571.49, 572.2–572.8, 456.0–456.21), chronic pulmonary disease (ICD-9-CM codes 490–496, 500–505, 506.4), and ischemic heart disease (ICD-9-CM codes 410–414). All diseases were defined as having been diagnosed 1 year before the index date.
Outcome measurement
The outcome was the occurrence of pneumonia (ICD-9-CM codes 481, 482, 483, 485, 486) diagnosed during an emergency visit or hospitalization. All patients were traced until the occurrence of pneumonia within 1 year after the index date, withdrawal from the social insurance system, or the end of 2013, whichever came first. Furthermore, we used the proportion of BSA to distinguish the effects of different types of burn injury on pneumonia.
In order to estimate the temporal association between burn injury and pneumonia, we used a self-controlled case-series design to verify it.Citation14 Patients with new diagnosis of pneumonia between January 1, 2010, and December 31, 2013 were recruited. We defined the exposure period as the interval of 30 days after burn injuries. The unexposed periods in the 4-year study were defined as the baseline period. Finally, we identified 151 patients with pneumonia that occurred before and after burn injury ().
Statistical analyses
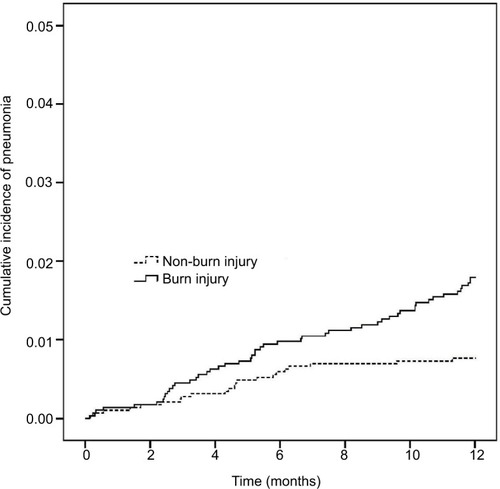
The comparison between burn injury and non-burn injury was performed using a chi-squared test or independent t-test, as appropriate. The cumulative incidence of pneumonia was performed using Kaplan–Meier analysis. The Cox proportional hazards model was used to estimate the hazard ratios of burn injury. The incidence rate ratio (IRR) of pneumonia in the exposure period compared with the baseline period was performed using a conditional Poisson regression. Statistical analyses were performed using SPSS V.18.0 (SPSS Inc., Chicago, IL, USA) and Stata V.12.0 (StataCorp LP, College Station, TX, USA).
Results
Characteristics of study patients
A total of 2,893 individuals with burn and the same number of individuals with non-burn between 2009 and 2013 were selected based on our inclusion and exclusion criteria (). After matching, the mean values of age, sex, and comorbidities were similar between the groups. Before the unmatched comparison of burn injury and non-burn injury, the patients with burn injury exhibited higher risks of the following comorbidities: hypertension, hyperlipidemia, diabetes, myocardial infarction, and chronic pulmonary diseases (). The median and interquartile range (IQR) of time to pneumonia in the burn injury group were 164 and 84–295 days, respectively. The types of pneumonia are analyzed in .
Figure 1 Flow chart for burn injury patient’s selection.
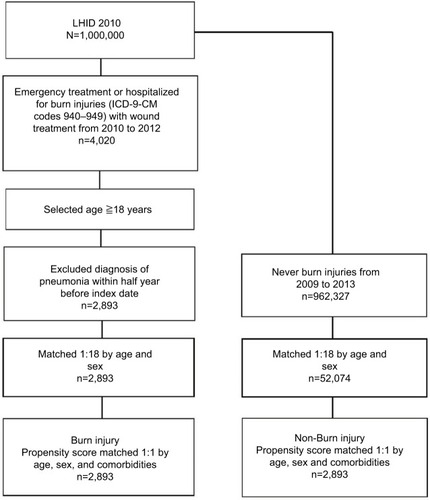
Table 1 Demographic characteristics of burn injury and non-burn injury
Risk of pneumonia and exposure to burn injury
We estimated the cumulative incidence of pneumonia cases that were exposed to burn injury. The curve of exposure for burn injury revealed a higher risk of pneumonia than that for non-burn injury (). The Cox proportional hazards model revealed a 2.39-fold increased risk of pneumonia for burn injury compared with that for non-burn injury (). For the different subgroups of age, the risk of pneumonia also increased 1.72-fold for patients aged 40–65 years and 9.97-fold for those aged ≥65 years, when compared with patients aged 18–40 years. In addition, male patients had a 1.83-fold higher risk of pneumonia compared with female patients. An increased risk of pneumonia with the following comorbidities was also noted: diabetes (adjusted hazard ratio [aHR]=2.58, 95% CI 1.44–4.64), cerebrovascular disease (aHR=2.75, 95% CI 1.42–5.31), and liver disease (aHR=2.55, 95% CI 1.15–5.65; ). In addition, when the patients were categorized into two groups according to burn surface area (BSA; ≤10% and >10%), the group with BSA ≤10% displayed a high risk of acquiring pneumonia (aHR=2.36, 95% CI 1.41–3.93). When BSA was >10%, the risk of acquiring pneumonia became higher in trend (aHR=3.01, 95% CI 0.89–10.17).
Table 2 Cox proportional hazards model of pneumonia and exposure to burn injury
Risk of pneumonia among patients with and without burn injury and subgroupspecific characteristics
We performed subgroup analysis between the burn injury group and the non-burn injury group. An increased risk of pneumonia was statistically observed in the burn injury group for patients aged ≥65 years (2.06-fold). An increased risk of pneumonia was also observed in male patients in the burn injury group (2.96-fold). Furthermore, an increased risk of pneumonia was observed with the comorbidities of ischemic heart disease in the burn injury group ().
Table 3 Subgroup analysis of Cox proportional hazards model of pneumonia between burn injury and non-burn injury groups
Temporal association between burn injury and pneumonia
For the self-controlled case-series population, the IRR of pneumonia of exposure period ≤30 days was 2.76-fold (95% CI=1.44–3.96) compared with that of the baseline period. The IRR within the exposure period between 31 and 60 days was 1.51-fold (95% CI=0.74–3.07), and the IRR within the exposure period between 61 and 90 days was 1.79-fold (95% CI=0.92–3.50; ).
Discussion
Patients with varying degrees of burn injury were recruited for observation of the risk of pneumonia within 1 year (2010). We observed that patients with burn injury were more likely to acquire pneumonia after recovery from burns. Although pneumonia was reported as a major complication in burn injury,Citation15 the present study is the first to indicate an increased risk and frequency of acquiring pneumonia after a burn injury. Burn injury exacerbates the destruction of the respiratory system and increases mortality rate.Citation15 The BSA percentage of burn injury also caused pneumonia in hospitalized patients. In one study, 27 out of 56 patients who had severe burn injury developed pneumonia.Citation16 Face and neck burns were also risk factors of respiratory infection, which developed into pneumonia. Inhalation injury and endotracheal intubation were associated with respiratory infection during hospitalization.Citation17
Burn injury can cause several sequelae, which can be affected by psychiatric or physiologic factors such as age and sex. In our study, the risk of pneumonia increased for male patients and those aged ≥65 years. Moreover, regarding the functional sequelae of burn injury, certain organs could not recover to their original function. For example, orofacial contractures after severe head and neck burns affect the ability to swallow.Citation18 Therefore, rehabilitation is required to reduce the swallowing impairment. Another burn sequela is heterotopic ossification (HO), which appears in the joints of limbs.Citation19 HO affects the flexible movement of limbs and requires surgery to excise pathologic bone tissue. The formation of HO was associated with the activation of both T- and B-lymphocytes in an animal study.Citation20 Osteomyelitis was reported in children with burn injury who were infected with fungi in their bone tissue.Citation21 A key study that agreed with ours indicated that patients who survived severe burn injury found it difficult to regain healthy lung function.Citation11 These findings might explain our result of burn injury patients having a higher risk of pneumonia.
The total burn surface area (TBSA) was correlated with symptoms of acute respiratory distress syndrome (ARDS), inhalation injury, and sepsis.Citation22 Similarly, patients with inhalation injury exhibited high TBSA, pneumonia, ARDS, and mortality rates.Citation23 Conversely, a reduction in burn-induced inflammation could improve pulmonary function and survival.Citation24 In our study, we categorized patients with burn injury into two groups (BSA ≤10% and BSA >10%). Obviously, the group with a BSA of ≤10% displayed a high risk of acquiring pneumonia. aHR even increased furtherly in the group with BSA >10%. This result implied that BSA has a positive relationship with getting pneumonia.
In burn injury, pathogens including bacteria, viruses, and fungi can infect respiratory tissue through two major routes. One is from mechanical therapy, such as ventilation and endotracheal intubation. The second is the bloodstream.Citation25 Early pathogenic colonization in acute burn wounds may also influence infection rate.Citation26 In addition, deep burns promote the risk of developing an infection.Citation27 In a study, a high level of blood glucose elevation was discovered in patients with severe burn injury, which suggested that airway secretion also contained a high concentration of glucose. The secretion acted as a culture medium for bacteria growth and promoted respiratory infection.Citation28 This might explain why infection of the respiratory tract was established more easily in patients with burn injury. Risk factors for the development of pneumonia in elderly patients with burn injury were sex, high TBSA, and existing comorbidities.Citation29 In our study, patients aged 40 years or older had a higher risk of acquiring pneumonia. This finding was consistent with the aforementioned report that stated that aging was a crucial risk factor for patients with burn injury.Citation30
Our study had some limitations. First, although smoke inhalation injury is also a complication of burn injury – especially in fire burns – it was excluded in our study because the insufficient number of cases might have led to underestimation of the odds ratio of pneumonia for burn injury exposure. Second, the database used did not contain information regarding patients’ clinical presentations of the severity of their pneumonia, laboratory data, or microbiological culture data that might affect pneumonia occurrence. Third, Taiwan’s National Health Insurance system is based on the Taiwanese population and our data accurately reflect the situation in Taiwan. Therefore, our results may not be applicable to Western populations. Fourth, we did not have access to potentially relevant personal behavioral information, such as smoking, alcohol consumption, and body mass index. These confounding factors might have influenced the results.
Conclusion
Burn injury patients were highly associated with an increased risk of pneumonia. Aging and BSA were another vital risk fac tor of pneumonia. Especially, the potential risk of pneumonia could be observed in burn injury, which refers to pneumonia which occurred within 30 days.
Acknowledgments
This study was partly based on data from the National Health Insurance Research Database (NHIRD) provided by the NHI Administration, Ministry of Health and Welfare, and managed by the National Health Research Institutes (registration number: NHIRD-104–148). The interpretation and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare, or National Health Research Institutes. Also, this study was supported by research grants from “Association For Dental Sciences of the Republic of China”. The funders had no role in the study design data collection and analysis, decision to publish, or preparation of the manuscript.
Supplementary materials
Figure S1 Flow chart for study selection of Self Controlled Case Series.
Abbreviations: LHID, Longitudinal Health Insurance Database; ICD-9-CM, ICD Ninth Revision Clinical Modification.
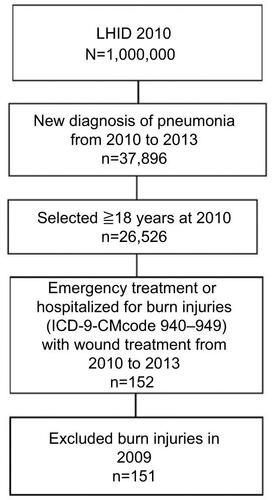
Table S1 Type of pneumonia event
Table S2 IRR for pneumonia after burn injury occurred
Disclosure
The authors report no conflicts of interest in this work.
References
- BrusselaersNMonstreySVogelaersDHosteEBlotSSevere burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortalityCrit Care2010145R18820958968
- LeeKCJooryKMoiemenNSHistory of burns: the past, present and the futureBurns Trauma20142416918027574647
- IyohoANgLChanPThe development of a probabilistic dose-response for a burn injury modelMil Med2017182S120220928291474
- RothenbachPADahlBSchwartzJJRecombinant plasma gelsolin infusion attenuates burn-induced pulmonary microvascular dysfunctionJ Appl Physiol2004961253112730154
- JohanssonJSteinvallIHerwaldHLindbomLSjöbergFAlteration of leukocyte count correlates with increased pulmonary vascular permeability and decreased PaO2:FiO2 ratio early after major burnsJ Burn Care Res201536448449225501784
- KolditzMEwigSCommunity-acquired pneumonia in adultsDtsch Arztebl Int20171144983884829271341
- GiulianoKKBakerDQuinnBThe epidemiology of nonventilator hospital-acquired pneumonia in the United StatesAm J Infect Control201846332232729050905
- PhuVDNadjmBDuyNHAVentilator-associated respiratory infection in a resource-restricted setting: impact and etiologyJ Intensive Care201756929276607
- MandellSPPhamTKleinMBRepeat hospitalization and mortality in older adult burn patientsJ Burn Care Res2013341e36e4123292594
- WongJLEvansSEBacterial pneumonia in patients with cancer: novel risk factors and managementClin Chest Med201738226327728477638
- MlcakRDesaiMHRobinsonENicholsRHerndonDNLung function following thermal injury in children – an 8-year follow upBurns19982432132169677023
- KobayashiMTakahashiHSanfordAPHerndonDNPollardRBSuzukiFAn increase in the susceptibility of burned patients to infectious complications due to impaired production of macrophage inflammatory protein 1 alphaJ Immunol200216984460446612370381
- StanojcicMChenPXiuFJeschkeMGImpaired immune response in elderly burn patients: new insights into the immune-senescence phenotypeAnn Surg2016264119520226649579
- PetersenIDouglasIWhitakerHSelf controlled case series methods: an alternative to standard epidemiological study designsBMJ2016354i451527618829
- ChenMCChenMHWenBSLeeMHMaHThe impact of inhalation injury in patients with small and moderate burnsBurns20144081481148625239845
- de La CalMACerdaéEGarciéa-HierroPPneumonia in patients with severe burnsChest200111941160116511296184
- Costa SantosDBarrosFGomesNGuedesTMaiaMFace and/or neck burns: a risk factor for respiratory infection?Ann Burns Fire Disasters20162929710228149229
- ClaytonNAWardECMaitzPKIntensive swallowing and orofacial contracture rehabilitation after severe burn: a pilot study and literature reviewBurns2017431e7e17
- ManskeMCHanelDPPostburn contractures of the elbow and heterotopic ossificationHand Clin201733237538828363302
- RanganathanKAgarwalSCholokDThe role of the adaptive immune system in burn-induced heterotopic ossification and mesenchymal cell osteogenic differentiationJ Surg Res20162061536127916375
- RosanovaMTVotoCCarnovaleSOsteomyelitis in burn children: ten years of experienceArch Argent Pediatr20181161596129333820
- SteinvallIBakZSjobergFAcute respiratory distress syndrome is as important as inhalation injury for the development of respiratory dysfunction in major burnsBurns200834444145118243566
- MonteiroDSilvaIEgiptoPInhalation injury in a burn unit: a retrospective review of prognostic factorsAnn Burns Fire Disasters201730212112529021724
- IpaktchiKMattarANiederbichlerADAttenuating burn wound inflammation improves pulmonary function and survival in a burn-pneumonia modelCrit Care Med20073592139214417855827
- DevrimİKaraADüzgölMBurn-associated bloodstream infections in pediatric burn patients: time distribution of etiologic agentsBurns201743114414827615546
- ParkHSPhamCPaulEPadiglioneALoCClelandHEarly pathogenic colonisers of acute burn wounds: a retrospective reviewBurns20174381757176528602589
- Ramirez-BlancoCERamirez-RiveroCEDiaz-MartinezLASosa-AvilaLMInfection in burn patients in a referral center in ColombiaBurns201743364265328185802
- KraftRHerndonDNMlcakRPBacterial respiratory tract infections are promoted by systemic hyperglycemia after severe burn injury in pediatric patientsBurns201440342843524074819
- PhamTNKramerCBKleinMBRisk factors for the development of pneumonia in older adults with burn injuryJ Burn Care Res201031110511020061844
- RaniMSchwachaMGAging and the pathogenic response to burnAging Dis20123217118022724078