Abstract
Objectives
Pancreatic cancer has a relatively low incidence but ranks fourth among cancer- related deaths in western countries. In Denmark, cancer survival generally is lower than in other countries with comparable health care systems. As a result, in 2000, a national strategy to improve cancer survival was introduced. Here we examine time trends in survival and relative mortality among pancreatic cancer patients, using Danish population and medical databases.
Methods
Using the Danish National Patient Registry (DNPR), we identified all incident pancreatic cancer patients (n = 2968) diagnosed between 1998 and 2009 in the Central and North Denmark Regions. We computed the 1-, 3-, and 5-year survival and relative mortality (MRR) and associated 95% confidence intervals (CI) adjusting for age and gender. Among surgical patients, we also computed 30-day mortality and 30-day MRR.
Results
Median age at diagnosis was approximately 71 years. The annual number of patients increased from 189 in 1998–2000 to 302 in 2007–2009. There was a slight improvement in 1-, 3-, and 5-year survival over time from 14.8% to 17.7%; 3.5% to a predicted 5.6%; and from 2.0% to a predicted 3.8%, from 1998–2000 to 2007–2009, respectively. Correspondingly, the adjusted relative mortality decreased from 1998–2000 to 2007–2009. Thirty-day post-operative mortality decreased from 12.2% in 1998–2000 to 5.8% in 2007–2009, corresponding to a 30-day MRR of 0.38, 95% CI = 0.09, 1.6 in 2007–2009.
Conclusion
There was a slight, albeit modest, improvement in survival and relative mortality in pancreatic cancer patients between 1998 and 2009. As we lacked staging information, it is not clear if this improvement is attributable to earlier stage at diagnosis. However, these improvements likely reflect the national cancer strategy which aimed to centralize cancer services and involved the introduction of palliative and adjuvant chemotherapy for pancreatic cancer in Denmark. The dismal prognosis of pancreatic cancer means that efforts to improve survival need to be intensified.
Introduction
Pancreatic cancer is a rapidly progressing disease with a dismal prognosis. It ranks as the fourth leading cause of cancer-related death in developed countries.Citation1 In 2008 alone, the standardized incidence rate (standardized to a world standard) of pancreatic cancer worldwide was 3.9 per 100,000 persons while the standardized (world standard) mortality rate was only slightly lower at 3.7 per 100,000 persons.Citation1 In Denmark, the incidence rate was 15 and 17 per 100,000 women and men, respectively,Citation2 and that of mortality was 14.4 and 16.2 per 100,000, respectively (standardized to the Danish population 2000).Citation3 The disease has an insidious onset with relatively nonspecific symptoms.Citation4 As a result, the majority of patients are diagnosed at an advanced stage,Citation5–Citation7 limiting the possibility of curative treatment.Citation8 Surgery remains the only curative treatment for pancreatic cancer.Citation9 However, research indicates that less than 20% of patients are suitable surgical candidates.Citation8
In the US, survival from most cancers has significantly improved between 1950 and 1995,Citation10 likely facilitated by technological advances enabling earlier cancer detection and more effective cancer-directed treatments.Citation11 However, survival from pancreatic cancer between 1950 and 1995 increased by only 3%, contrasting with the improvements observed for several other cancers.Citation10 Research in the Nordic countries has also indicated little change in pancreatic cancer survival between 1964 and 2006, and lowest survival among Danish patients.Citation5,Citation12 In 2000, the Danish government initiated the “National Cancer Plan I ”, with an update in 2005. The aims of the plan include enhancing cancer prevention; improving and accelerating the patient referral pathway; strengthening cancer surgery; monitoring cancer care; and implementing a multidisciplinary approach to diagnosis and treatment.Citation13 It is critical to regularly monitor cancer patient survival to evaluate the effect of this cancer plan. In the current study therefore, we examined trends in mortality and survival of pancreatic cancer patients over time using Danish population and medical databases.
Material and methods
We conducted this study in the Central and the North Denmark Regions, with a combined population of 1.8 million persons, representing approximately one-third of the Danish population. The National Health Service provides tax-supported health care for all inhabitants of Denmark, guaranteeing free access to hospitals. Virtually no pancreatic cancer patients were treated in private hospitals during the study period.
We used the Danish National Patient Registry (DNPR) to identify the pancreatic cancer patients included in the current study. The DNPR contains information on all admissions from nonpsychiatric hospitals in Denmark since 1977,Citation14 and outpatient and emergency room visits at these hospitals since 1995. The DNPR includes information on civil personal registration (CPR) number, dates of admission and discharge, surgical procedure(s) performed, and up to 20 diagnoses from each hospital contact. Diagnoses have been classified according to the International Classification of Diseases (ICD) 8th edition until the end of 1993 and 10th edition thereafter.
Identification of pancreatic cancer patients
We identified all patients who had an incident diagnosis of pancreatic cancer between January 1, 1998 and December 31, 2009 using the DNPR. We included all patients with an ICD-10 code of C25.x.
Identification of pancreatic cancer surgery
Surgical procedures have been classified according to a Danish classification system until the end of 1995 and according to a Danish version of the Nordic Classification of Surgical Procedures (NCSP) thereafter. We used the DNPR to identify the surgical procedures pancreatectomy (JLC.20), pancreatoduodenectomy (JLC.30), and total pancreatoduodenectomy (JLC.40) conducted within 90 days after the pancreatic cancer diagnosis.
Survival
Since 1968 the Danish Civil Registration System (DCRS) has assigned a unique 10-digit civil personal registration (CPR) number to all Danish citizens.Citation15 This number, unique to each Danish resident, is used in all Danish registries, allowing unambiguous individual-level data linkage. From the DCRS we also obtained information on vital status (dead or alive), date of death, and residence for all cancer patients.
Statistical analysis
We followed each patient from the date of pancreatic cancer diagnosis until emigration, death, or 25 June 2010, whichever came first. We constructed Kaplan–Meier survival curves to illustrate crude survival stratified by diagnostic period (1998–2000, 2001–2003, 2004–2006, and 2007–2009). In the most recent periods we estimated 1-, 3-, and 5-year survival using a hybrid analysis whereby survival was estimated using the survival experience of patients in the previous periods.Citation16 We compared mortality over time using Cox proportional hazards regression analysis with 1998–2000 as the reference period to estimate 1-, 3- and 5-year mortality rate ratios (MRRs) and associated 95% confidence intervals (CIs) adjusting for age group (15–59 years, 60–79 years, ≥80 years), and gender.
Among patients who underwent surgery, we computed 30-day mortality rates from date of surgery for the four time periods. We used Cox proportional hazards regression analysis and estimated 30-day MRRs and associated 95% CIs with 1998–2000 as the reference period, adjusting for age group and gender. We used the Cochran–Armitage trend test to evaluate the trend in 30-day mortality rates from 1998 through 2009.Citation17
All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC).
Results
A total of 2968 patients was diagnosed with pancreatic cancer between 1998 and 2009 in the Central and North Denmark regions. The number of pancreatic cancer patients increased over the study period from 607 in 1998–2000 to 702 in 2001–2003, 768 patients in 2004–2006, and 891 patients in 2007–2009. Median age at diagnosis was 71 years and varied little by period of diagnosis (). Women were, on average, older at diagnosis than men and accounted for 51% of pancreatic cancer cases ().
Figure 1 Age at diagnosis of pancreatic cancer patients in Central and Northern Denmark 1998–2009 by gender.
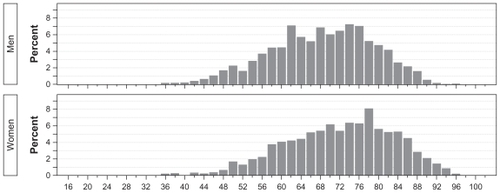
Table 1 Cumulative survival and crude and adjusted relative mortality (MRR) (and associated 95% confidence intervals) for pancreatic cancer patients diagnosed in Central and Northern Denmark, 1998–2009
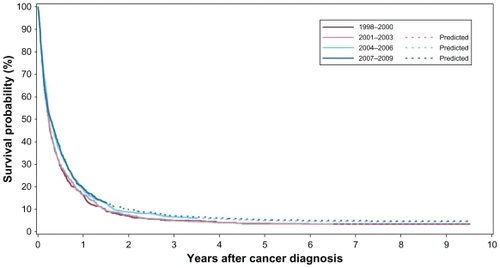
illustrates the survival curve of pancreatic cancer patients by period of diagnosis. Regardless of diagnostic period, less than 50% of patients were alive at 6 months after diagnosis. Median survival was 2.7 months for patients diagnosed in 1998–2000; 2.8 months for patients diagnosed in 2001–2003; 3.2 months for those diagnosed in 2004–2006 and 2007–2009. also outlines the cumulative proportion of patients surviving at 1, 3, and 5 years, as well as the crude and adjusted MRRs by diagnostic period, using patients diagnosed in the earliest period (1998–2000) as a reference group. Patients diagnosed in 2004–2006 and 2007–2009 had slightly better survival 1-year post-diagnosis than those in the earlier periods (17.4%, 95% CI = 14.9%, 20.2%, and 17.7%, 95% CI = 15.3%, 20.4%, versus 14.8%, 95% CI = 12.1%, 17.8% and 15.1, 95% CI = 12.6%, 17.9%, respectively). The projected estimates for 3- and 5-year survival also increased from 3.5% (95% CI = 2.2%, 5.1%) to 5.6% (95% CI = 4.2%, 7.4%) and from 2.0% (95% CI = 1.1%, 3.3%) to 3.8% (95% CI = 2.6%, 5.4%), respectively, over the study period.
Figure 2 Kaplan–Meier survival curves for patients with pancreatic cancer in Central and Northern Denmark regions, 1998–2009.
outlines the cumulative survival at 1, 3, and 5 years stratified by age and gender. One-year survival appeared to be best in the youngest age group, ranging from 19.7% (95% CI = 11.2%, 30.0%) to 27.5% (95% CI = 16.4%, 19.9%) in women. One-year survival was lower in women aged 60–79 years (range 13.1%, 95% CI = 8.8%, 18.1%, to 17.9%, 95% CI = 13.1%, 23.3%), and was lowest in elderly patients (age 80+) – range 8.2%, 95% CI = 3.8%, 14.6% to 10%, 95% CI = 4.7%, 17.7%). There was little change in 3- and 5-year survival estimates from 1998 through 2009. The same pattern was evident among male pancreatic cancer patients, where the cumulative proportion of men surviving 1-year after diagnosis was highest in the youngest age group, lower in the middle age group and lowest in the elderly patients.
Table 2A Cumulative survival (and associated 95% confidence intervals) for male pancreatic cancer patients diagnosed in Central and Northern Denmark, 1998–2009
Table 2B Cumulative survival (and associated 95% confidence intervals) for female pancreatic cancer patients diagnosed in Central and Northern Denmark, 1998–2009
A total of 176 pancreatic cancer patients was surgically treated within 90 days after diagnosis, accounting for a mere 5.9% of the total patient population. The median age of surgical patients was lower than that of nonsurgical patients (surgical patients median age 62.4 compared with a median age of 71.8 in nonsurgical patients). Surgical patients were slightly older in the latter two diagnostic periods than those diagnosed between 1998 and 2003. The 30-day mortality after surgery was approximately halved after the first period 1998–2001 from 12.2% to 6.8%, 5.1% and 5.8%, corresponding to an age-adjusted MRR of 0.38 (95% CI = 0.09, 1.6) in the last period compared with the first period () (2-sided P-value = 0.26).
Table 3 30-day mortality and relative mortality (and associated 95% confidence intervals) among pancreatic cancer patients diagnosed in Central and Northern Denmark, 1998–2009
Discussion
This study shows that survival of pancreatic cancer patients in Denmark marginally improved between 1998 and 2009. Although only a modest improvement, pancreatic cancer has such a low median survival, that any improvement is noteworthy. There was also a decline in 30-day mortality after surgery for pancreatic cancer, likely attributable to increasing centralization of cancer services and a multidisciplinary approach to cancer treatment.Citation18
When interpreting our findings several factors should be considered. The large size and uniformly organized health care system facilitated a population-based design with accurate survival estimates, and reduced selection bias. The use of the DCRS ensured complete follow-up.Citation15 We used the DNPR rather than the Danish Cancer Registry to obtain information on individuals with pancreatic cancer due to the delay in reporting of cancer cases to the cancer registry. As the DNPR is continuously updated, it provided an ideal setting in which to monitor any recent changes in survival. Furthermore, the sensitivity and positive predictive value of a cancer diagnosis in the DNPR is high, increasing the validity of our study.Citation14,Citation19,Citation20 Presentation of estimates of survival and mortality make the findings from this study suitable for comparison with findings from other countries. Our study also serves to highlight that data from patient registries are suitable tools to use when monitoring cancer survival.
Improvements in pancreatic cancer survival could be facilitated by detecting the cancer before local invasion or distant metastatic disease is established – when surgery is most effective. An increase in the proportion of patients with localized disease would also improve the selection of surgical candidates, thereby improving surgical outcomes. The National Cancer Strategy may have contributed to the detection and diagnosis of pancreatic cancer at an earlier stage. Unfortunately, we had no information on clinical characteristics such as cancer stage at diagnosis and cancer-directed treatment, other than cancer surgery. Therefore, we were unable to investigate the impact of these factors on pancreatic cancer survival and how possible changes in these factors may correlate with the observed changes in survival.
Although pancreatic cancer is frequently resistant to chemotherapy, randomized trials have shown that chemotherapy can be beneficial in selected groups of patients, particularly those who undergo surgical resection.Citation21 The majority of pancreatic cancer patients are elderly when diagnosed, and therefore may be considered unlikely to respond to treatment or unable to tolerate aggressive cancer-directed treatments.
Pancreatectomy is considered a complex and technically challenging procedure due to the location and inaccessibility of the pancreas.Citation22 Research suggests the procedure is underutilized in clinical practice.Citation23 The proportion of patients undergoing pancreatectomy in the current study was similar to rates observed in Ireland (7%)Citation24 and Scotland (5%),Citation25 but much lower than rates in Sweden (15%),Citation26 the Netherlands (11%),Citation27 and the US (~15%)Citation28,Citation29 over comparable diagnostic periods. Reasons for such variation in surgical rates are not clear. We incorporated information on surgery within 90 days of diagnosis; the US study incorporated surgery within 120 days; and the Irish study, based on cancer registry data, included surgeries registered within the first year after diagnosis. These differences may account for the variation in surgical rates across these countries, however given the poor survival of pancreatic cancer; it is likely that surgery with a curative intent would be given soon after diagnosis. The difference in surgical rates may also be due to the fact that patients with localized stage are considered the only potentially curable patients, and international studies have shown a more advanced stage distribution among Danish cancer patients, generally, than in other developed countries with comparable health care systems.Citation30 Nonetheless, despite the relatively low uptake of surgery, in these Danish pancreatic cancer patients we saw a decrease in postoperative mortality consistent with trends reported in the Nordic countriesCitation5 and elsewhere.Citation31–Citation33 This lower mortality may reflect the implementation of the National Cancer Plan, specifically strengthening and centralization of surgery, and a more multidisciplinary approach to cancer treatment.Citation18
Furthermore, the National Cancer Plan also aims to improve cancer diagnostics through increasing the availability of cancer scanners, for example. This may have created a “lead-time bias” in the current study, whereby patients are diagnosed at an earlier stage and so their survival appears longer. Unfortunately, we did not have information on cancer stage and so we are unable to explore this possibility further.
Smoking is one of the few established risk factors for pancreatic cancer, others being type 2 diabetes and chronic pancreatitis.Citation34 It has been estimated that smoking prevention could decrease the incidence of pancreatic cancer by as much as 20%.Citation6 Due to the poor prognosis of the disease, cancer prevention may be the only way to reduce the disease burden in the population. However, the relatively occult nature of pancreatic cancer etiology means that population-based survival and relative mortality, such as presented in the current study, are likely to remain key indicators of progress against this deadly disease.
In conclusion, this study shows a very slight improvement in pancreatic cancer survival and decreased relative mortality. These findings are consistent with findings for the Danish cancer patient population generally,Citation5,Citation12 and are likely to be a direct effect of the dissemination of the National Cancer Plan. However, the poor prognosis of this disease means that efforts at preventing, diagnosing and treating this disease need to be intensified in order to continue to improve survival.
Acknowledgments
The study received financial support from the Karen Elise Jensen Foundation, Department of Clinical Epidemiology’s Research Foundation and the Regional Clinical Epidemiological Monitoring Initiative for Central and North Denmark Regions.
Disclosure
The authors report no conflicts of interest.
References
- FerlayJShinHRBrayFEstimates of worldwide burden of cancer in 2008: GLOBOCAN 2008Int J Cancer20101272893291721351269
- SundhedsstyrelsenCancer Incidence in Denmark in 20092010
- SundhedsstyrelsenDanish Cause of Death in 20092010
- HollyEAChalihaIBracciPMSigns and symptoms of pancreatic cancer: a population-based case-control study in the San Francisco Bay areaClin Gastroenterol Hepatol2004251051715181621
- KlintAEngholmGStormHHTrends in survival of patients diagnosed with cancer of the digestive organs in the Nordic countries 1964–2003 followed up to the end of 2006Acta Oncol20104957860720491524
- TeiblumSThygesenLCJohansenCSixty-one years of pancreatic cancer in Denmark from 1943 to 2003: a nationwide studyPancreas20093837437819287331
- NagenthirajaKEwertzMEngholmGIncidence and mortality of pancreatic cancer in the Nordic countries 1971–2000Acta Oncol2007461064106917952708
- MichalskiCWWeitzJBuchlerMWSurgery insight: surgical management of pancreatic cancerNat Clin Pract Oncol2007452653517728711
- BergenfeldtMHansenCPMortensenMBSurgical treatment of pancreatic cancerUgeskr Laeger20101721358136020444404
- WelchHGSchwartzLMWoloshinSAre increasing 5-year survival rates evidence of success against cancer?JAMA20002832975297810865276
- JemalACleggLXWardEAnnual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survivalCancer200410132715221985
- ColemanMPFormanDBryantHCancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry dataLancet200137712713821183212
- SundhedsstyrelsenNational kræftplan. Status og forslag til initiativer i relation til kræftbehandlingen1161SundhedsstyrelsenKøbenhavn2000
- AndersenTFMadsenMJorgensenJThe Danish National Hospital Register. A valuable source of data for modern health sciencesDan Med Bull19994626326810421985
- PedersenCBGotzscheHMollerJOThe Danish Civil Registration System. A cohort of eight million personsDan Med Bull20065344144917150149
- BrennerHRachetBHybrid analysis for up-to-date long-term survival rates in cancer registries with delayed recording of incident casesEur J Cancer2004402494250115519525
- AgrestiACategorical Data AnalysisNew York, NYJohn Wiley and Sons, Inc1990
- StormHHGislumMEngholmGCancer survival before and after initiating the Danish Cancer Control planUgeskr Laeger20081703065306918822235
- TetscheMSNorgaardMSkriverMVAccuracy of ovarian cancer ICD-10 diagnosis in a Danish population-based hospital discharge registryEur J Gynaecol Oncol20052626627015991523
- NorgaardMSkriverMVGregersenHThe data quality of haematological malignancy ICD-10 diagnoses in a population-based hospital discharge registryEur J Cancer Prev20051420120615901987
- YipDKarapetisCStricklandAChemotherapy and radiotherapy for inoperable advanced pancreatic cancerCochrane Database Syst Rev20063CD00209316855985
- ShaibYDavilaJNaumannCThe impact of curative intent surgery on the survival of pancreatic cancer patients: a US Population-based studyAm J Gastroenterol20071021377138217403071
- EloubeidiMADesmondRAWilcoxCMPrognostic factors for survival in pancreatic cancer: a population-based studyAm J Surg200619232232916920426
- SharpLCarsinAECronin-FentonDPIs there under-treatment of pancreatic cancer? Evidence from a population-based study in IrelandEur J Cancer2009451450145919268569
- ParksRWBettschartVFrameSBenefits of specialisation in the management of pancreatic cancer: results of a Scottish population-based studyBr J Cancer20049145946515226766
- LinderSBostromLNilssonBPancreatic cancer in sweden 1980–2000: a population-based study of hospitalized patients concerning time trends in curative surgery and other interventional therapiesJ Gastrointest Surg20061067267816713540
- Van OostFJLuitenEJvan de Poll-FranseLVOutcome of surgical treatment of pancreatic, peri-ampullary and ampullary cancer diagnosed in the south of The Netherlands: a cancer registry based studyEur J Surg Oncol20063254855216569495
- ShaversVLHarlanLCJacksonMRacial/ethnic patterns of care for pancreatic cancerJ Palliat Med20091262363019594347
- CressRDYinDClarkeLSurvival among patients with adenocarcinoma of the pancreas: a population-based study (United States)Cancer Causes Control20061740340916596292
- StormHHDickmanPWEngelandADo morphology and stage explain the inferior lung cancer survival in DenmarkEur Respir J1343043510065693
- SchmidtCMChoiJPowellESPancreatic fistula following pancreaticoduodenectomy: clinical predictors and patient outcomesHPB Surg2009404520
- NakeebALillemoeKDGrosfeldJLSurgical techniques for pancreatic cancerMinerva Chir20045915116315238889
- GeerRJBrennanMFPrognostic indicators for survival after resection of pancreatic adenocarcinomaAm J Surg19931656872 discussion 72–638380315
- MaisonneuvePLowenfelsABEpidemiology of pancreatic cancer: an updateDig Dis20102864565621088417