Abstract
Background
The incidence and risk factors of suicide reattempts within 1 year after psychiatric hospital discharge in mood disorder patients remain uninvestigated in Thailand.
Objective
To determine incidence and risk factors of suicide reattempts within 1 year after psychiatric hospital discharge in mood disorder patients.
Methods
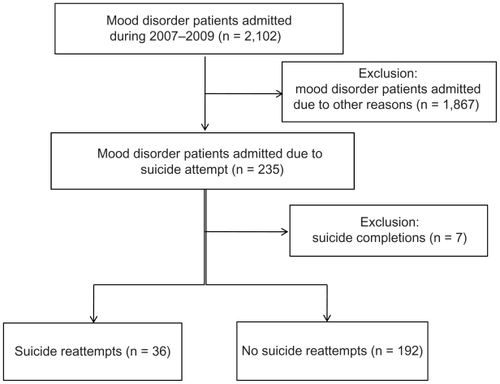
A retrospective cohort study was conducted by reviewing medical charts at Suanprung Psychiatric Hospital, Chiang Mai, Thailand. Mood disorder patients, diagnosed with the International Statistical Classification of Diseases and Related Health Problems 10th Revision codes F31.x, F32.x, and F33.x, who were admitted owing to suicide attempts between October 2006 and May 2009 were eligible. The influence of sociodemographic and clinical risk factors on suicide reattempts was investigated using Cox’s proportional-hazards regression analysis.
Results
Of 235 eligible mood disorder patients, 36 (15.3%) reattempted suicide (median 109.5 days, range 1–322), seven (3.0%) completed suicide (median 90 days, range 5–185), and 192 (84.2%) neither reattempted nor completed suicide during follow-up. Of all nonfatal suicide reattempts, 14 patients (38.9%) did so within 90 days. Among suicide completers, one (14.3%) did so 5 days after discharge, and four (57.1%) did so within 90 days. The following three risk factors explained 73.3% of the probability of suicide reattempts: over two previous suicide attempts before the index admission (adjusted hazard ratio [HR] 2.48; 95% confidence interval [CI] 1.07–5.76), being concomitantly prescribed typical and atypical antipsychotics (adjusted HR 4.79; 95% CI 1.39–16.52) and antidepressants, and taking a selective serotonin reuptake inhibitor alone (adjusted HR 5.08; 95% CI 1.14–22.75) or concomitantly with norepinephrine and/or serotonin reuptake inhibitors (adjusted HR 6.18; 95% CI 1.13–33.65).
Conclusion
Approximately 40% of suicide reattempts in mood disorder patients occurred within 90 days after psychiatric hospital discharge. For mood disorders and when there have been over two previous suicide attempts, prescribed antipsychotics or antidepressants may help predict suicide reattempts.
Introduction
Mood disorders are disturbances in a person’s mood categorized into major depressive disorder (MDD) and bipolar disorder (BD). MDD and BD appear to be the most important risk factors for lifetime suicide in any psychiatric disorder.Citation1 It has been estimated that at the time of suicide, 87.3%–98% of psychiatric disorders are from mood disorders and substance abuse.Citation2
Among mood disorder patients who attempt suicide, reattempt is more common than the first act.Citation3 The prevalence of reattempted suicide within 1 year after the index suicide attempt is 16%–40% nonfatal and 2% fatal.Citation4,Citation5 Risk of reattempted suicide following a psychiatric admission is highest during the first months after the attempt and declines over time.Citation6
Several risk factors for suicide attempts reported in MDD and BD patients include male sex,Citation7,Citation8 age,Citation5,Citation7 living alone on the day of the index attempt,Citation9 smoking,Citation10 alcohol abuse,Citation9 previous number of suicide attempts,Citation9–Citation12 method of suicide attempt,Citation9 severity of refractory or recurrent depressions,Citation10,Citation12 somatic illness,Citation9 suicide intent and treatment of mental illness,Citation7,Citation9,Citation11 hospitalization in a psychiatric department, and the use of psychopharmacological drugs during the follow-up period. Other risk factors are impulsivity, stressful life events, hopelessness, being unemployed,Citation13 comorbidity with anxiety and agitation, and reporting suicidal plans or hallucinations at the time of the index episode.Citation14
The current study was undertaken at a setting located in the upper northern part of Thailand where the suicide attempt rate of 34.1 per 100,000 population is remarkably high. The suicide completion rate was the highest in the nation at 12.4 per 100,000 population compared with 5.97 per 100,000 population countrywide in 2009. Mood disorders rank among the top five high-burden diseases in this setting every year. Among those diagnosed with mood disorders, 25% are hospitalized due to suicide attempts.Citation15 Suicide reattempts are prevalent in this vulnerable population; however, the incidence and risk factors of suicide reattempts in mood disorder patients have not yet been investigated in this area. Furthermore, consensus on suicide attempt risk factors is still unclear because of their complexity, and the generalizability of previous research may be limited due to discrepancies of cultural context, study populations, design, and data analysis. Thus, there is a need for studies of incidence and risk factors for suicide reattempts in mood disorder patients in Thailand. The present study aimed to determine incidence and explored risk factors of suicide reattempts occurring within 1 year after psychiatric hospital discharge in mood disorder patients.
Methods
Study population and setting
Suanprung Psychiatric Hospital is the largest tertiary psychiatric hospital (700 beds) in the upper northern region of Thailand. It is located in Chiang Mai and has been providing medical care since 1938. In 2009, the hospital provided services to 6721 inpatients and 61,561 outpatients. Mood disorder inpatient and outpatient visits for 2007, 2008, and 2009 were 9069, 10,739, and 11,482, respectively.Citation16
Eligible patients were all mood disorder patients diagnosed by psychiatrists and coded by the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Inclusion criteria were patients diagnosed with ICD-10 codes F31.x, F32.x, and F33.x and admitted to Suanprung Psychiatric Hospital owing to suicide attempts between October 2006 and May 2009.
Outcome definitions and measures
People who reattempted suicide were those mood disorder patients who reattempted nonfatal suicide within 1 year after an admission to Suanprung Psychiatric Hospital owing to attempted suicide. Eligible patients’ medical charts were examined for the main outcome of the study, which was time to suicide reattempts. Time to suicide reattempts was defined as the number of days within 1 year from the date of hospital discharge to the suicide reattempt date. Patients who did not reattempt suicide during the 1 year of follow-up or with whom contact was lost before the 1-year follow-up were considered a censor group. Their time at risk from the index date to censoring time was collected. Further, the national death registration was searched and death date and cause of death were retrieved. A cause of death was further confirmed by telephone calls to the patient’s spouse or next of kin. To determine risk factors for suicide reattempts, suicide completers were excluded from the analysis, because this population did not overlap.
Data collection
The study was designed as a retrospective cohort study. Patients’ medical files were reviewed from the day of admission and followed for 1 year after hospital discharge. The admission time was set as an index date. Patient information recorded in hospital files was routinely assessed and documented with a standardized procedure by psychiatrists, trained psychiatric nurses, and pharmacists who interviewed patients and/or their relatives. Five trained nurses working at the study site extracted data and filled in a case record form. To assure validity of the data, two meetings were held by the research team to discuss and clarify each variable in the files before data collection. Undocumented variables were considered to be missing.
Sociodemographic factors and clinical factors were the main indicators collected in the study. All factors were selected and divided into categories based on a literature review and the opinion of psychiatrists on the research team. The sociodemographic factors included were sex, age, body mass index, marital status, educational level, occupation, religion, living status (alone or with others), number of children, and summation of number of stressful life events right before or at the index episode. Social support was divided into good or excellent, moderate, and little or very little.
Clinical factors included ICD-10 diagnoses of BD (coded F31.x) and MDD (coded F32.x and F33.x). Duration of treatment began from the time of the first diagnosis to the index date, and age at onset was the age at the first visit. Previous admission referred only to admission to Suanprung Psychiatric Hospital before the index date. Previous suicide attempt and previous suicidal ideation were assessed and counted from the first hospital visit to the index date. Psychotic symptoms at an index episode included hallucination and hearing voices. Psychotic comorbidity was extracted from the ICD-10 code and was recorded and grouped into alcohol/substance dependence, which was commonly found, and others. Somatic illness was any chronic disease. Smoking, alcohol use, and any substance abuse were behaviors at the index date. Medication adherence was assessed by attending pharmacists asking patients or their relatives about consistency in taking medication during the 2 weeks before the index date. It was summarized as “highly adhere,” meaning the patient always took medication or rarely missed a dose, “intermittently adhere,” meaning the patient took medication off and on, and “poorly adhere,” meaning at least seven consecutive days when the patient did not take medication. Other clinical characteristics included family history of mental disorders and family history for attempted or completed suicide.
An additional variable collected was the number and type of method(s) used for suicide attempt at the index date. The method was considered a violent method if it was (1) a method other than drug overdose or a single wrist cut or (2) a combination of different methods.Citation17 Treatments received during the admission included pharmacotherapy, electroconvulsive therapy, and psychotherapy. Pharmacotherapy was prescribed medication, which we categorized according to the mechanism of action and evidence of relation to suicide. Mood stabilizers were categorized either as lithium or others, such as carbamazepine and valproate. Antidepressants were grouped as norepinephine and/or serotonin reuptake inhibitors, such as amitriptyline and venlafaxine, or as selective serotonin reuptake inhibitors (SSRIs), such as fluoxitine and fluvoxamine. Antipsychotics were divided into typical, such as zuclopentizol and haloperidol, and atypical, such as clozapine and risperidone. Anxiolytics consisted of benzodiazepine and others, such as chlodiazepoxide. Psychotherapy included individual and group counseling, family counseling, and rehabilitation. Additionally, data on length of stays and readmission within 28 days were also collected.
Statistical analyses
Because time to suicide reattempts was an outcome of the study, Cox’s proportional-hazards regression was used for the analysis. Owing to the nature of the fitting exploration model, we determined the best parsimonious model by performing two steps of analysis. First, variables predicting suicide reattempts were explored using univariable Cox’s proportional-hazards regression. Those with a P-value less than 0.20 were selected for the last step, in which forward elimination multivariable Cox’s proportional-hazards regression was selected. The global goodness-of-fit test by Schoenfeld was used for testing the proportional-hazards assumption.Citation18 In order to assess the model prediction, we used the area under receiver operating characteristic curve method. The statistical significance level was set at 0.05. Two institutional review boards, the Faculty of Medicine at Chiang Mai University and Suanprung Psychiatric Hospital, approved the protocol of the study.
Results
A total of 235 patients’ medical folders were reviewed and included in the analysis (). Of those, 36 (15.32%) reattempted suicide (median 109.5 days, range 1–322), seven (2.98%) completed suicide (median 90 days, range 5–185), and 192 (84.21%) neither reattempted nor completed suicide during follow-up. Of all nonfatal suicide reattempts, 14 patients (38.9%) did so within 90 days. Among suicide completers, one (14.3%) did so 5 days after discharge, and four (57.1%) did so within 90 days. Total time of follow-up in each group is presented in .
Table 1 Incidence of suicide reattempts and suicide completions within 1 year after hospital discharge in mood disorder patients (n = 235)
Univariable analysis found that stressful life events, psychotic symptoms, and previous suicide attempts were significantly associated with suicide reattempts ( and ).
Table 2 Sociodemographic factors of mood disorder patients and unadjusted hazard ratio (HR) (95% confidence interval [CI]) of suicide reattempts by univariable Cox’s proportional-hazards regression analysis (n = 228)
Table 3 Clinical factors of mood disorder patients and unadjusted hazard ratio (HR) (95% confidence interval [CI]) of suicide reattempts by univariable Cox’s proportional-hazards regression analysis (n = 228)
Three risk factors that explained 73.3% of the probability of suicide reattempt were attempting suicide more than twice before the index admission (adjusted hazard ratio [HR] 2.48; 95% confidence interval [CI] 1.07–5.76], concomitantly prescribed typical and atypical antipsychotics (adjusted HR 4.79; 95% CI 1.39–16.52), or taking SSRI alone (adjusted HR 5.08; 95% CI 1.14–22.75) or with norepinephrine and/or serotonin reuptake inhibitors (adjusted HR 6.18; 95% CI 1.13–33.65). In addition, readmission within 28 days was significantly higher in the suicide reattempt group (18.8% vs 5.1%, P = 0.008) (data not shown) ().
Table 4 Risk factors of suicide reattempts and adjusted hazard ratio (HR) (95% confidence interval [CI]) by multivariable Cox’s proportional-hazards regression analysis (n = 228)
Discussion
To the best of our knowledge, the present study is the first to determine incidence and explore risk factors of suicide reattempts within 1 year after psychiatric hospital discharge in mood disorder patients. In this study, the incidence of suicide reattempts and suicide completions within 1 year of follow-up after attempted suicide was 15.3% and 3.0%, respectively. This finding is consistent with previous studies that reported suicide reattempts at 13.6%–16%Citation6,Citation13 and suicide completions at 1%–3%.Citation19 Although the median time of suicide reattempts in the present study was longer than in a previous study (109.5 days vs 73.5 days),Citation13 almost 40% of nonfatal suicide reattempts of the patients in this study occurred within 90 days. The reattempt rate is more likely to be clustered in time because the incidence declines throughout the year of follow-up.Citation6 Therefore, intensive surveillance, timely assessment, and effective interventions should be emphasized during the first few months and continue for 1 year after hospital discharge.
Using the best fit and simple model, we found three risk factors that indicated suicide reattempts: more than two previous suicide attempts before the index admission, concomitantly being prescribed typical and atypical antipsychotics, and taking an SSRI alone or concomitantly with norepinephrine and/or serotonin reuptake inhibitors. Previous suicide attempts before the index date is a risk factor associated with suicide reattempts found in several studies.Citation9–Citation12 In the present study, 74.4% percent of patients had at least one prior suicide attempt before the index date. The hazard ratios increased with an increasing number of previous suicide attempt(s), demonstrating that patients with more prior attempts tended to be more severe, be more impulsive, and take more risks.Citation20
Regarding the use of medication, psychopharmacological use prior to and during the follow-up period is a predictor for suicide attempt.Citation6 Suicide reattempts increased in mood disorder patients prescribed with antipsychotics or antidepressants. This is in accordance with a meta-analysis study reporting that antidepressants were not beneficial for suicidal patients.Citation21 However, in some previous studies,Citation22 long-term treatment with antidepressants was found to reduce suicides significantly when combined with lithium and antipsychotics. Antipsychotic users were more likely to reattempt suicide in this study. The ability of most antipsychotics to limit the risk of suicidal behavior remains untested in the literature.Citation23 The positive relationship results of antidepressant and antipsychotic use in this study may be due to confounding indications. Patients prescribed with more types of medication were those who were more severe and prone to a higher number of suicide reattempts.
Stressful life events and psychotic symptoms were two risk factors associated with suicide reattempts found in the univariable analysis but not in the multivariable analysis. This is possibly because of the intercorrelation with one or more other variables. A previous study indicated that stressful life events play an important role in suicide attempts in patients with mood disorders, particularly MDD patients.Citation24 We found that having psychotic symptoms at the time of admission reduced the probability of suicide attempts, which is consistent with a previous study that suggested that psychosis may impair planning for suicide attempts.Citation25
Currently, there are a few studies that determine risk factors of suicide reattempts in mood disorders. Most of the research reports risk factors associated with suicide attempts in MDD or BD separately. Therefore, inconsistencies between our findings and previous studies are partially due to the difference in population, methodology, assessment tools, statistical analysis, and small samples of some variables in this study. Other studies have found risk factors for suicide attempts that include male sex;Citation7,Citation8 increasing age (ie, 50 years or older);Citation5,Citation7 living alone on the day of the index attempt;Citation9 the method used in the index attempt;Citation9,Citation26 prior admission for suicide reattempt;Citation8,Citation9,Citation19 family history of mental disorders;Citation27 previous suicidal ideation;Citation25 somatic illness, such as cardiovascular disease and malignancies;Citation7,Citation28 abuse of psychopharmacological agents, alcohol, or substances;Citation28,Citation29 bipolar,Citation30,Citation31 depressed, and mixed episodes among BD patients; recurrent or refractory MDD, including those with psychosis;Citation32 a positive family history of suicidal behaviors;Citation27 not taking lithium; and short-term effects from electroconvulsive therapy.Citation33
There are some limitations of the present study. First, the generalizability of the study results may be limited to mood disorder patients visiting psychiatric hospitals. Those with severe physical injuries resulting from the attempted suicide were likely to be referred to a general hospital. Their characteristics, such as lethality of the method used and severity of psychiatric illness, may be different. Second, data collected from medical folders were subject to incompleteness or missing variables, which caused a lack of power to identify associations. Third, the data relied exclusively on patient interview. Some information, such as drug and alcohol use, can be under-reported. Additionally, the effect of some variables, such as psychotic disease in family members or a family history of suicide, could be underestimated. These variables may be missed because patients were unaware of them, or they may remain unspoken due to stigma. Some factors were not assessed in this study by instruments used in other studies (eg, hopelessness and impulsiveness). Thus, their potential risk was not directly detected. Fourth, we used variables at the admission index date as risk factors. However, some factors can change over time and occur during follow-up, such as marital status, employment situation, development of depression, and medication adherence. These may have affected our findings. However, the aim of the study was to examine factors at one specific point in time that predict a high risk of repeated suicide attempts and thus possibly guide treatment. Finally, we found a final model that moderately explained the probability of suicide reattempts (73.3%). A larger sample size is required in future research to increase statistical power and should be prospectively used to confirm the study results.
In spite of some limitations, risk factors of suicide reattempts in mood disorder patients were identified. For future research, risk factors for long-term suicide reattempts must be investigated, because they may differ somewhat from the short-term risk factors found in the present study. Furthermore, risk factors categorized by subgroup of mood disorders (ie, MDD and BD) must be separately investigated to enable clinicians to provide intervention specifically directed for each subgroup. Finally, this study lacks statistical power to investigate risk factors for suicide completion and suicidal ideation. Future research on those issues is warranted.
Conclusion
Almost 40% of suicide reattempts in mood disorder patients in this study occurred within 90 days after their discharge from a psychiatric hospital. Factors placing patients at high risk for suicide reattempts were over two previous suicide attempts before the index admission, concomitantly being prescribed typical and atypical antipsychotics and antidepressants, and taking an SSRI alone or concomitantly with norepinephrine and/or serotonin reuptake inhibitors.
Acknowledgment
This study was financially supported in part by the Faculty of Medicine and the Graduate School, Chiang Mai University.
Disclosure
All authors have no conflicts of interest in this research.
References
- SimonRIHalesRESuicide Risk: Assessing the Unpredictable1st edSimonRIHalesREArlington, VAAmerican Psychiatric Publishing, Inc2006
- HarrisCEBarracloughBMSuicide as an outcome for mental disordersBr J Psychiatry19971702052289229027
- KerkhofAAttempted Suicide: Patterns and Trends1st edHawtonKvan HeeringenKNew YorkJohn Wiley & Sons, Ltd2000
- HawtonKFaggJSuicide, and other causes of death, following attempted suicideBr J Psychiatry19881523593663167371
- NordströmPSamuelssonMÅsbergMSurvival analysis of suicide risk after attempted suicideActa Psychiatr Scand1995a91336340
- ChristiansenEJensenBFRisk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysisAust N Z J Psychiatry20074125726517464707
- SoukasJSuominenKIsometsäELong-term risk factors for suicide mortality after attempted suicide: findings of a 14-year follow-up studyActa Psychiatr Scand200110411712111473505
- SkogmanKAlsénMÖjehagenASex differences in risk factors for suicide after attempted suicide: a follow-up study of 1052 suicide attemptersSoc Psychiatry Psychiatr Epidemiol20043911312015052392
- CooperJKapurNWebbRSuicide after deliberate self-harm: a 4-year cohort studyAm J Psychiatry200516229730315677594
- OquendoMAGalfalvyHRussoSProspective study of clinical risk factors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorderAm J Psychiatry20041611433144115285970
- OwensDWoodCGreenwoodDCMortality and suicide after non-fatal self-poisoning: 16-year outcome studyBr J Psychiatry200518747047516260824
- OquendoMACurrierDMannJJProspective studies of suicidal behavior in major depressive and bipolar disorders: what is the evidence for predictive risk factors?Acta Psychiatr Scand2006114315115816889585
- KapurNCooperJKing-HeleSThe repetition of suicidal behavior: a multicenter cohort studyJ Clin Psychiatry200667101599160917107253
- SchneiderBPhilippMMullerMJPsychopathological risk factors of suicide in patients with major depression during a 5-year follow-upEur Psychiatry200116528328811514130
- Suanprung Psychiatric HospitalSuanprung’s outpatient and inpatient services treat most psychiatric illnessesChiang Mai, Thailand2010 [updated 2010]. Available from: http://www.suanprung.go.th/eng/top_five.phpAccessed November 7, 2011
- Suanprung Psychiatric HospitalSuanprung psychiatric hospital report number of patients between 2007 to 2009Chiang Mai, Thailand2010 [updated 2010]. Available from: http://www.suanprung.go.th/statt/index.htmlAccessed November 7, 2011
- TräskmanLÅsbergMBertilssonLSjöstrandLMonoamine metabolites in CSF and suicidal behaviourArch Gen Psychiatry1981386316366166274
- GreenlandSIntroduction to Regression Modeling. Modern Epidemiology3rd edRothmanKJPhiladelphiaLippincott Williams & Wilkins2008418455
- SakinofskyITreating suicidality in depressive illness. Part I: current controversiesCan J Psychiatry2007526 Suppl 171S84S17824354
- CorrubleEDamyCGuelfiJDImpulsivity: a relevant dimension in depression regarding suicide attemptsJ Affect Disorders19995321121510404706
- StoneMLaughrenTJonesMLRisk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug AdministrationBMJ2009339b288019671933
- AngstFStassenHHClaytonPJAngstJMortality of patients with mood disorders: follow-up over 34–38 yearsJ Affect Disord2002682–316718112063145
- BaldessariniRJPompiliMTondoLSuicide in bipolar disorder: risks and managementCNS Spectr200611646547116816785
- SuppapitipornSThe risk factors of suicidal attempt in depressed patientsChulalongkorn University2002 [updated 2002; cited November 26, 2009]; Thesis (MSc) – Chulalongkorn University, 2002]. Available from: http://cuir.car.chula.ac.th/dspace/handle/123456789/6093Accessed November 7, 2011
- OquendoMASuicidal behavior in bipolar mood disorder: clinical characterisic of attempters and nonattempetrsJ Affect Disord20005910711710837879
- SuominenKIsometsäESuokasJCompleted suicide after a suicide attempt: a 37-year follow-up studyAm J Psychiatry2004161563564
- LizardiDSherLSullivanGMAssociation between familial suicidal behavior and frequency of attempts among depressed suicide attemptersActa Psychiatr Scand2009119540641019367777
- NielsenBWangAGBille-BraheUAttempted suicide in Denmark. IV. A five-year follow-upActa Psychiatr Scand1990812502542343748
- MurphyGEWetzelRDThe lifetime risk of suicide in alcoholismArch Gen Psychiatry1990473833922181963
- BottlenderRJaegerMStraussAMöllerHJSuicidality in bipolar compared to unipolar depressed inpatientsEur Arch Psychiatry Clin Neurosci2000250525726111097169
- FiedorowiczJGDo risk factors for suicide behavior differ by affective disorder polarity?Psychol Med200939576377118667100
- ScoliersGPortzkyGvan HeeringenKAudenaertKSociodemographic and psychopathological risk factors for repetition of attempted suicide: a 5-year follow-up studyArch Suicide Res200913320121319590995
- SharmaVRetrospective controlled study of inpatient ECT: does it prevent suicide?J Affect Disord1999562–318318710701475