Abstract
Dengue is currently regarded globally as the most important mosquito-borne viral disease. A history of symptoms compatible with dengue can be traced back to the Chin Dynasty of 265–420 AD. The virus and its vectors have now become widely distributed throughout tropical and subtropical regions of the world, particularly over the last half-century. Significant geographic expansion has been coupled with rapid increases in incident cases, epidemics, and hyperendemicity, leading to the more severe forms of dengue. Transmission of dengue is now present in every World Health Organization (WHO) region of the world and more than 125 countries are known to be dengue endemic. The true impact of dengue globally is difficult to ascertain due to factors such as inadequate disease surveillance, misdiagnosis, and low levels of reporting. Currently available data likely grossly underestimates the social, economic, and disease burden. Estimates of the global incidence of dengue infections per year have ranged between 50 million and 200 million; however, recent estimates using cartographic approaches suggest this number is closer to almost 400 million. The expansion of dengue is expected to increase due to factors such as the modern dynamics of climate change, globalization, travel, trade, socioeconomics, settlement and also viral evolution. No vaccine or specific antiviral therapy currently exists to address the growing threat of dengue. Prompt case detection and appropriate clinical management can reduce the mortality from severe dengue. Effective vector control is the mainstay of dengue prevention and control. Surveillance and improved reporting of dengue cases is also essential to gauge the true global situation as indicated in the objectives of the WHO Global Strategy for Dengue Prevention and Control, 2012–2020. More accurate data will inform the prioritization of research, health policy, and financial resources toward reducing this poorly controlled disease. The objective of this paper is to review historical and current epidemiology of dengue worldwide and, additionally, reflect on some potential reasons for expansion of dengue into the future.
Introduction
Dengue is an acute mosquito-borne viral infection that places a significant socioeconomic and disease burden on many tropical and subtropical regions of the world.Citation1,Citation2 It is currently regarded as the most important arboviral disease internationally as over 50% of the world’s population live in areas where they are at risk of the disease, and approximately 50% live in dengue endemic countries.Citation2–Citation6
Dengue virus
There are four distinct dengue virus serotypes, all of which originate from the family Flaviviridae and genus Flavivirus.Citation3,Citation7,Citation8 The serotypes are termed DENV-1, DENV-2, DENV-3, and DENV-4, and infection with any of the four viruses results in lifelong immunity to that specific serotype.Citation4,Citation9,Citation10 Each of the four serotypes has been individually found to be responsible for dengue epidemics and associated with more severe dengue.Citation8,Citation11
Dengue disease and clinical management
Dengue is a complex disease with a wide spectrum of clinical presentations, which often goes unrecognized or is misdiagnosed as other fever-causing tropical diseases.Citation12,Citation13 Following the period of incubation, most patients experience a sudden onset of fever which can remain for 2–7 days and is often accompanied with symptoms such as myalgia, arthralgia, anorexia, sore throat, headaches, and a macular skin rash.Citation7,Citation14 It is during this period that differentiating dengue from other febrile diseases proves troublesome.Citation15 The majority of people experience a self-limiting clinical course, which does not progress to the severe forms of dengue, dengue hemorrhagic fever (DHF), or dengue shock syndrome (DSS). Secondary dengue infections or particularly virulent viral strains are two factors thought to be associated with increased risk of severity.Citation2,Citation16 In severe cases, thrombocytopenia and increased vascular permeability can result in hemorrhagic and shock complications. Currently, neither a vaccine nor specific antiviral therapy exists.Citation10,Citation17,Citation18 However, with prompt case detection and appropriate clinical management, including initiation of intravenous rehydration, the case fatality of severe dengue can be lower than 1%.Citation11 At present, due to a lack of available treatment, control of dengue focuses on effective vector control methods, which are limited.Citation10,Citation19,Citation20
Dengue vector and vector control
The main arthropod vector for transmission of the dengue viruses is Aedes aegypti (A. aegypti).Citation7 The second, less effective vector, Aedes albopictus (A. albopictus), feeds on multiple species of vertebrates, but has still been shown to be responsible for some dengue transmission.Citation8 Significantly, the Aedes mosquitos are predominantly active during daylight hours, which poses difficulties in controlling the vector.Citation7,Citation21A. aegypti mosquitoes are now extensively spread in both the tropics and subtropics.Citation19 The mosquito is renowned for its efficient ‘vectorial capacity’ with a high affinity for human blood, high susceptibility to the four dengue virus serotypes, and being highly adapted to urban living.Citation8,Citation20,Citation22,Citation23A. aegypti mosquitoes breed in and around houses in regular water containers or disposed water-holding vessels.Citation24 Due to this location of development and their limited flight range, female A. aegypti tend to persist in a domesticated environment.Citation19 It is for this reason that humans are presumed the main cause of spread of dengue between communities.Citation8 The wider prevention and control of dengue is currently reliant on vector control methods. These include environmental, biological, and chemical vector control management strategies and methodologies.Citation19
The objectives of this paper are to review the current epidemiology of dengue worldwide as well as looking at its origins and history. Furthermore, we will attempt to elaborate on some of the reasons for the anticipated further expansion and increase of dengue in the future.
Dengue in the past
Dengue has been present for centuries. The first recorded symptoms compatible with dengue were noted in a Chinese medical encyclopedia in 992 AD, however originally published by the Chin Dynasty centuries earlier (265–420 AD), prior to being formally edited.Citation25 The disease was referred to as ‘water poison’ and was associated with flying insects.Citation26 Epidemics that resembled dengue, with similar disease course and spread, occurred as early as 1635 and 1699 in the West Indies and Central America, respectively.Citation27 A major epidemic occurred in Philadelphia in 1780 and epidemics then became common in the USA into the early 20th century, the last outbreak occurring in 1945 in New Orleans.Citation23,Citation27 The viral etiology and the transmission by mosquitoes were only finally determined in the 20th century.
The origin of the primary mosquito vector, A. aegypti, is debated to be from either Africa or Asia.Citation8,Citation23 Regardless, by 1800 it was widespread throughout urban tropical coastal cities of the world due to the use of shipping vessels with commercial expansion.Citation8,Citation23,Citation28 These shipping vessels allowed transportation of breeding sites for the vector along with humans to complete the transmission cycle, allowing for slow but evident introduction of the virus and the mosquito to coastal destinations around the world.Citation28 Epidemics were spaced by 10–40 year intervals due to this shipping mode of transport.Citation23,Citation25,Citation28 Expansion of the disease heightened during World War II (WWII), when troops began to disperse inland and utilize modern transportation within and between countries; thus epidemic dengue became more far-reaching.Citation23 By the end of the war, transportation and rapid urbanization led to increased transmission of dengue and hyperendemicity (multiple serotypes present) in most South East Asian countries, with subsequent emergence of the severe forms of dengue.Citation2,Citation22
Following WWII, dengue epidemics appeared to be under control in Central and South America. The elimination of A. aegypti, due to collaborative efforts with the yellow fever disease control campaign initiated by the Pan American Health Organization (PAHO), effectively restricted the transmission of dengue throughout the American conti-nent.Citation3,Citation8,Citation22,Citation29 The lull in dengue epidemics in the Americas was short-lived, as the control campaign was discontinued in the 1970s. By the 1980s incidence had increased, and by 1995 pre-campaign levels were present in the Americas.Citation22 Geographic expansion of epidemic dengue from South East Asia in the late 20th century saw regions in the Pacific and Americas escalate from being non-endemic with no dengue serotypes circulating, to hypoendemic (one serotype present), and some hyperendemic.Citation22,Citation28
Global dengue incidence has increased precipitously over the last five decades and severe dengue cases have also expanded.Citation2,Citation4,Citation6 Prior to 1970, only nine countries had experienced severe dengue cases, a number which has since quadrupled.Citation30
Current global situation of dengue
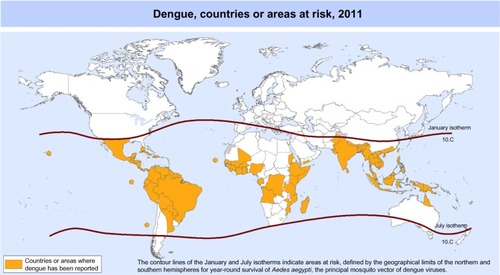
Up to 3.6 billion people are estimated to now live in tropical and subtropical areas where the dengue viruses have the potential to be transmitted.Citation2,Citation4,Citation31 Global estimates vary, but regularly approximate 50 million to 200 million dengue infections, 500,000 episodes of severe dengue (DHF/DSS), and over 20,000 dengue related deaths occur annually.Citation3,Citation29 shows the geographic distribution of dengue cases reported in 2011.
Figure 1 Countries or areas of the world where dengue was reported in 2011, as per data collected by the World Health Organization.Citation32
In 2012, dengue was once again classified by the World Health Organization (WHO) as the ‘most important mosquito-borne viral disease in the world’Citation6 due to significant geographic spread of the virus and its vector into previously unaffected areas and the subsequent costly burden of disease it brings.Citation2,Citation4,Citation11,Citation32 Disability adjusted life year (DALY) estimates differ, but a 2009 estimate of DALYs lost due to dengue globally was 700,000 per year.Citation33,Citation34 In most countries, the main burden of this morbidity and mortality lies with children.Citation35–Citation38 Dıaz-Quijano and WaldmanCitation39 conducted an ecological study investigating the determinants of the dengue mortality burden. Length of recognized endemicity, rainfall, and population density were all shown to be associated with dengue mortality in Latin America and the Caribbean.Citation39
A study which reviewed all nations in the Americas (with available data from the PAHO, 2000–2007) estimated an aggregate annual cost of dengue for the Americas at US$2.1 billion.Citation29 Approximately 60% of this cost related to indirect or ‘productivity’ losses, and the figure notably excluded prevention costs.Citation29 A study of twelve countries in South East Asia (using available data from 2001–2010) showed an aggregate annual economic burden of US$950 million amongst the studied nations, with approximately 52% of these costs coming from productivity loss.Citation40 This figure again excluded necessary prevention and vector control costs.Citation40
Due to poor disease surveillance, low level of reporting, low case fatality rate, difficulties in diagnosis, and inconsistent comparative analyses, the true incidence and impact of dengue is likely significantly higher than that which is currently reported.Citation2,Citation18,Citation41 Thus, the true global burden of disease and associated economic impact is unknown.Citation6 However, Brady et alCitation42 have conducted the first of a series of steps in evidence consensus mapping of global dengue incidence to better determine the population at risk. Their 2012 publication suggested an ‘upper bound’ total of 3.97 billion people living in 128 countries are at risk of dengue globally, 824 million in urban residences, and 763 in peri-urban residences.Citation42 The same group published again in April 2013 using cartographic approaches. These data suggested 390 million dengue infections occur annually worldwide, including both apparent and inapparent infections, almost double the highest figure regularly reported to date.Citation43
Despite the level of uncertainty on total numbers, we have evidence today that every WHO region now has dengue transmission and that there are more than 125 dengue endemic countries globally.Citation5,Citation31 Here we will review available data on dengue endemicity by WHO region.
WHO Southeast Asia (SEA) region
It is evident that dengue is now a worldwide concern; however, almost 75% of the global population exposed to dengue live in Asia-Pacific.Citation6,Citation8 1.3 billion of these at-risk individuals live in ten dengue endemic countries in SEA, and dengue is a leading cause of hospitalization and death in children from the region.Citation8,Citation28 The rates of disease reported in each of the SEA countries varies as they include either laboratory confirmed, probable, or suspected cases.Citation40 However, it is clearly evident from data collated by WHO that, in SEA, an overall expansion of dengue has occurred over the last decade.Citation8 In 2003, eight countries in SEA had reported cases of dengue and, by 2009, all SEA member countries excluding the Democratic People’s Republic of Korea reported indigenous cases.Citation6,Citation8 Epidemics continue to persist on regular 3–5 year cycles throughout SEA, and the number of reported cases continues to increase along with the severity of cases in many member countries.Citation40 187,333 dengue cases were reported to WHO in 2010 from the region.Citation31 Eight SEA countries are now also classified as hyperendemic with all four of the dengue virus serotypes present.Citation8 Severe dengue is endemic in most SEA countries, with rates of severe dengue being 18 times higher in this region compared with the Americas.Citation6,Citation8,Citation40
WHO Western Pacific region
The WHO Western Pacific and SEA regions combined are attributed 75% of the global dengue disease burden.Citation19,Citation31 The number of reported cases of dengue has increased continuously over the past decade in the Western Pacific.Citation44 353,907 dengue cases and 1073 deaths were reported in the region as a whole in 2010.Citation31,Citation44
In the Asian subregion of the WHO Western Pacific region, the greatest burden of dengue currently originates from Cambodia, the Lao People’s Democratic Republic, Malaysia, the Philippines, Singapore, and Vietnam.Citation44 The number of reported cases increased in each of these nations over the past ten years, and all four serotypes have been identified in these high disease-burden settings.Citation44 From the Pacific subregion, 91% of reported cases came from French Polynesia, New Caledonia, Vanuatu, and Australia.Citation44 Two dengue virus serotypes were reintroduced from the Americas to the Pacific Islands in 1964 (DENV-3) and in 1971 (DENV-2), following a 25 year absence.Citation2,Citation27 The next decade saw gradual introduction of all four serotypes from Asia, which remain in circulation today.Citation44 As a result, island nations in the Pacific show a particular susceptibility to dengue epidemics and severe dengue.Citation6 In Australia, dengue activity, including indigenous outbreaks, occur in Northern Queensland where A. aegypti is present.Citation10,Citation44 In 2009 and 2010, more than 1000 cases of dengue were reported in Australia.Citation44
WHO region of the Americas
Despite the absence of dengue transmission in the middle of the 20th century, almost all countries in the Americas now have hyperendemicity with indigenous dengue transmission.Citation6 Epidemics occur cyclically in the region every three to five years, as they do in SEA, with increasing frequency and size, particularly in Latin America.Citation19,Citation29,Citation31 In 2010, more than 1.6 million cases of dengue were reported in the Americas alone, 49,000 of these being severe dengue.Citation5 Only two countries in Latin America remain to be without indigenous transmission, Uruguay and Continental Chile.Citation45 Locally acquired cases of dengue have also now been reported in the USA.Citation31 Due to the resurgence of dengue and its vector in the Americas over recent decades, PAHO has once again launched an initiative targeting vector control and prevention in the region.Citation19 The ‘Integrated Management Strategy for Dengue Prevention’ is striving to reduce the disease and economic burden that dengue places currently on the Americas.Citation6,Citation45
WHO African region
Little has been known or reported about the situation in Africa amidst the geographic spread of dengue worldwide.Citation6,Citation13 Despite dengue not being officially reported to WHO by African countries and the probable under-recognition of dengue, evidence suggests that outbreaks are increasing in size and frequency in the region.Citation3,Citation6,Citation12 Available outbreak data suggest 22 African countries reported sporadic cases or outbreaks between 1960 and 2010.Citation6,Citation13 Amarasinghe et alCitation13 conducted a review of existing databases and literature in 2011 that showed dengue transmission is endemic in 34 countries in the African region. 22 of these countries reported local disease transmission, 20 reported lab-confirmed cases, and two reported clinical cases alone.Citation13,Citation31 No ‘local’ reports of dengue occurred in the remaining 12 countries, only in travelers returning to non-endemic countries.Citation13 All four dengue virus serotypes have been seen in Africa, however, DENV-2 appears to have caused most epidemics.Citation13 Notably, in 2009, the Cape Verde archipelago had a large dengue outbreak involving more than 17,000 cases and linked to DENV-3.Citation46,Citation47 Due to the significant endemicity of malaria throughout the African region, the majority (>70%) of ‘febrile illnesses’, including dengue, are likely to be misdiagnosed and treated as malaria.Citation13 This negatively impacts attempts to draw a comprehensive picture of the epidemiology of dengue in the region and establish regular surveillance, outbreak monitoring, and relevant prevention and control activities.Citation6,Citation13
WHO European region
The last reported epidemic of dengue in Europe was between 1926 and 1928 in Greece.Citation6 This epidemic implicated A. aegypti as the predominant vector and saw high mortality of cases. No dengue transmission had been reported since this time until A. albopictus became established in Europe in the 1990s as a result of increasing global trade of used tires.Citation5,Citation6,Citation30 Today, there is a very real and apparent threat of dengue outbreaks in Europe. Imported cases in travelers are seen frequently and, in 2010, local transmission of dengue was reported in both Croatia and France.Citation5,Citation6 The Madeira Islands of Portugal have been in the midst of an outbreak since October 2012. This outbreak had resulted in 2164 cases by February 2013, with 78 imported cases from recent travelers to Madeira detected in 13 other countries throughout Europe.Citation5,Citation48,Citation49 Thus, despite Europe being free of dengue for the majority of the 20th century, the global expansion of dengue is finally impacting the region.
WHO Eastern Mediterranean region
In the Eastern Mediterranean region, dengue is classified as an ‘emerging disease’.Citation6 Cases have only been officially reported to WHO for the last 2 decades, during which time three countries – Saudi Arabia, Pakistan, and Yemen – have had multiple outbreaks.Citation6 For example, in 2011, the city of Lahore in Pakistan experienced a major dengue outbreak associated with 21,685 confirmed cases and 350 deaths, mainly due to DENV-2.Citation50,Citation51 Smaller outbreaks involving multiple serotypes of dengue virus are now being reported more frequently from countries such as Sudan, Djibouti, and Somalia.Citation6 This highlights the probable geographic expansion of dengue within the Eastern Mediterranean Region, as with elsewhere globally.
Dengue in the future
Many experts hypothesize that dengue will increase in the future, including geographic expansion, incidence and reporting to WHO.Citation10,Citation23,Citation52,Citation53 It is therefore important to elaborate on some of the potential factors that drive dengue activity, as well as the global strategic direction to address this growth.
Viral evolution
Dengue viruses have been cataloged as having a low, medium, or high epidemiological impact according to their likelihood for human transmission and the clinical severity of dengue epidemics.Citation54 In other words, some viruses largely prevail in sylvatic cycles among non-human primate populations, rarely transmitting to humans, while others are the viral agents causing mild dengue fever.Citation54 Still other genotypes having higher virulence correlate with cases and epidemics characterized by more severe disease manifestations.Citation54 For instance, there are some DENV-2 and DENV-3 genotypes found more commonly in the Americas which are known to be comparatively less virulent than Asian genotypes of the same serotype, as evidenced by reduced growth in both mosquitoes and culture.Citation10,Citation54 Wang et alCitation55 demonstrated that domain III may play a role in viral adaptation to naïve hosts, whether mosquito or human, through analysis of modifications to the envelope protein postulated to correlate with endemic and/or epidemic emergence.Citation55 Genotypes with greater virulence are driving out virus strains of lesser epidemiological impact, as evidenced by phylogenetic and epidemiological analyses.Citation23,Citation54
Climate change factors
Temperature is known to play a role in adult vector survival, viral replication, and infective periods.Citation23,Citation56–Citation58 Increases of temperature may result in increased survival and or migration of vectors into previously non-endemic geographic areas outside the tropics.Citation53 As the proliferation of Aedes mosquitoes is climate dependent, climate or meteorological factors can potentially provide useful information in predictive models. Weather variability has shown to be predictive of dengue activity.Citation57–Citation61 According to the Intergovernmental Panel on Climate Change, mean temperatures are predicted to rise globally.Citation62 This may create climatic and environmental conditions conducive to the proliferation of Aedes species in areas that are currently non-endemic. The climatic suitability of many currently non-endemic areas and climatic similarity with endemic areas suggests that both A. aegypti and A. albopictus could become established or reestablished in the near future.Citation63 A study conducted in the Southwest Pacific suggested that global temperature increases observed over the last four decades corresponded with increased risk of dengue outbreaks.Citation64 Some studies on climate change and dengue show possible increase in transmission due to higher temperatures, humidity, and precipitation associated with changes in climate.Citation53,Citation61,Citation65 This supports the notion that observed climatic changes, including increased average global temperature and increased humidity, theoretically increase the epidemic potential of dengue.Citation66,Citation67 Based on long-term average vapor pressure prediction, climate change and population projections, Hales et alCitation53 predicted that approximately 50%–60% of the global population would be living in areas at risk of dengue transmission by 2085. If climate change did not occur as projected or was not taken into the model, only 35% would be at risk.Citation53
The individual role climate change plays in the last decades’ resurgence of dengue remains uncertain and is an area of current modeling research.Citation67 Some authors also argue against climate as the main driver for dengue expansion. Beebe et alCitation68 concluded from their Southeast Australian study that an increased risk of A. aegypti range expansion in Australia was due to the human adaptation of installing large domestic water storing containers as a response to persisting regional drying, rather than due to climate change itself.Citation68 Furthermore, dengue and yellow fever caused multiple epidemics in the southern parts of the USA in the 18th, 19th, and early 20th centuries. Their eventual control was not due to a change in climate, but rather due to changes with industrialization and modernization.Citation56,Citation63
Globalization, travel, and trade factors
While climate change alone may not be a comprehensive and sufficient causal factor in the current and ongoing expansion of dengue, broader ‘global change’ may be.Citation69 The ‘global change’ framework seeks to account for multiple factors of the modern world contributing to vector-borne communicable disease.Citation69 Modern contributing factors to the rapid expansion of vector-borne communicable disease include globalization factors, such as travel and trade, associated with vector accommodating trends in modern human settlement and suitable climate conditions.Citation2 The contributions of increased mobility, both of vector and human populations, may be the most important variable to explain the recent increase in dengue transmission.Citation2
Climate and human settlement factors may enable and explain the risk of introduction or reintroduction of dengue into non-endemic zones where they border areas of endemic transmission. For other areas, further outside the tropics, the slight expansion due to climate change and human-vector interactions pale in comparison to factors of globalization. Globalization has been a main contributor and result of recent global economic development, creating a global ecosystem of exchange.Citation2 The current global reality is one of international passenger travel and intercontinental exchange of goods.Citation23 By 2011, passenger air travel saw a 40-fold increase compared to the middle of the 20th century with ever increasing travel to and from dengue endemic areas.Citation2 Human travel by those infected with dengue is thought to be the main driver of global transmission and expansion of the disease.Citation2,Citation66 Modern transport accounts for importation of dengue by overcoming natural barriers of travel time and geography, which had previously limited expansion from endemic areas into non-endemic areas.Citation70 A recent model on the geospatial distribution of transmission via passenger air travel identified routes on which importation of dengue was an increased risk.Citation70 Increased risk routes between the USA and Latin America, and also between Europe and Asia, were identified, ranked, and correlated with increased geographical distribution of the secondary dengue vector, A. albopictus.Citation70 Intercontinental air travel between areas within the tropics has resulted in transmission of all four dengue virus serotypes in some areas.Citation2,Citation23 Overcrowded airports located in the tropics function as the ideal urban breeding ground and distribution point for dengue viruses within and outside current areas of transmission.Citation2,Citation70
As the global community trades and travels more and more, so too do communicable and vector-borne diseases.Citation2 Further globalization factors, which are contributing to expansion of dengue transmission and risk of importation of dengue, include not only travel, but also trade. International transport of cargo and goods, especially via commercial sea shipment, can also export and import dengue’s primary and secondary vectors, A. aegypti and A. albopictus, respectively.Citation64 Transatlantic transport of used auto tires has been linked with the introduction of exotic American mosquito varieties into Italy, which contributed to other vector-borne disease epidemics.Citation64,Citation69,Citation71 Given the vectors’ suitability to breed and survive sea travel within water collected in a tire, their transport has contributed to a major public health threat in the last few decades, and this will only increase as more automobiles are consumed globally.Citation72
Settlement and socioeconomic factors
Given the critique regarding climate as an independent factor in the observed expansion of dengue transmission, recent approaches seek to combine climate data with projected societal changes, including increased population and economic development in tropical and subtropical areas.Citation52,Citation57 While suitable climate factors are necessary to permit the resurgence and expansion of dengue transmission observed over the last 5 decades, human factors, including increasing global population, urbanization, and socioeconomic constraints on control measures, also contribute. Trends in current human settlement, together with rapidly expanded urban areas, exploding population density, and limited socioeconomic resources, suggest that the human factors, in addition to climate factors, may be necessary components in understanding current and future risks of dengue transmission.Citation2,Citation52 Settlement and socioeconomic factors combine with climatic suitably and globalized travel and trade to suggest that human populations and their collective actions strongly contribute to the transmission of dengue, in addition to mosquito vectors.
Settlement factors
Human factors, including both urban and rural settlement patterns, contribute to currently observed trends of increased incidence and expansion of dengue transmission. Rapid urbanization and population growth have been identified as strong contributing factors to the increase of global dengue transmission and geographic expansion.Citation2,Citation23 These two factors, particularly in low- and middle-income countries in tropical and subtropical regions, often precede the construction of necessary infrastructures for safe and comprehensive collection, storage, and disposal of water.Citation69 Urban and suburban development may also provide new man-made breeding sites in the built environment, prior to human inhabitants occupying them. This has been shown even in well planned and financed situations such as the urban development endeavors in Putrajaya, Malaysia.Citation73 In this manner, rapid urbanization facilitates the creation of urban breeding sites for the most potent dengue vector, A. aegypti.Citation74A. aegypti thrives in urban environments in that the mosquito breeds preferentially in the artificial containers often used in urban water collection.Citation2 The increased density of both mosquito and human populations, as part of urban population growth, compounds this effect in terms both of vector suitability and transmission of dengue.Citation2,Citation75 While current research and policy interventions often treat dengue expansion as a phenomenon associated with urban human settlement, the incidence of the disease in rural areas is also on the rise. Some studies suggest that rural dengue incidence can even surpass urban and semi-urban communities within the same region.Citation76,Citation77 One such study in Cambodia found rural incidence to be 71/1000 person-seasons compared to urban incidence of 17/1000 person-seasons during an outbreak of DENV-3 in 2007.Citation77
Previous and ongoing underestimation of rural incidence may be attributable to similar vector-suitable breeding sites between some regions’ urban-poor and rural communities. In addition, growing interconnectivity between rural and urban areas via increasing road infrastructure, combined with decreased access to diagnostics and surveillance may act as a silent conduit for rural dengue transmission and greater underestimation of rural incidence compared to more urban areas.Citation77 The significant role and mechanisms of human involvement in creating a conducive ecology for dengue transmission, in addition to climate environmental factors, is being increasingly considered and modeled in current research.Citation66,Citation67
Socioeconomic factors
Historical dengue incidence and decline in Europe and the US, among other areas, suggests the role of socioeconomic development on dengue transmission and control.Citation2,Citation53,Citation63 Multiple studies compared dengue endemicity and seroprevalence between neighboring border cities in Northern Mexico and Southern Texas. These highlight the importance of socioeconomic factors on the transmission of dengue, where climatic suitability was similar.Citation78–Citation81 In one such comparative cross-sectional study from 2004, current dengue seroprevalence was found to be 7.3% in Matamoros, Mexico, but only 2% in Brownsville, Texas, just across the border in the USA.Citation78 Another similar serosurvey in 2005 suggested an even greater disparity between dengue incidence in Matamoros and Brownsville, reporting current dengue infection in 32% and 4%, respectively, of the 273 study participants and estimating past dengue infection prevalence in 77% and 39%, respectively.Citation80 Key similarities observed among both cities included climate and geography, vector mosquito habitat and density, and human host social factors, for instance household size, use of insect screens, and basic sanitation.Citation78–Citation81 Socioeconomic and behavioral factors including income, water storage, usage of air-conditioning, waste disposal, and cross-border travel differed sustainably, as did dengue prevalence.Citation78–Citation81 In endemic areas, including the USA–Mexico border, more favorable socioeconomic factors resulting in higher utilization of air conditioning and domestic screening, as well as improved water and waste disposal infrastructure, are recommended to reduce larvae breeding sites and dengue transmission.Citation78–Citation81 Environmental management that aims to reduce, remove, and displace breeding sites from urban areas is recognized as a key mechanism to control dengue transmission.Citation69
Global strategic direction
In light of the potential for continued expansion of dengue globally, it is essential to reflect on policy and strategic direction that attempts to reduce the impact of this disease. Dengue has been classified as a ‘neglected topical disease,’ based on the historical lack of coordinated efforts, political will, and research attention despite the significant disease, social, and economic burden it places internationally.Citation6,Citation82,Citation83 This classification has encouraged prioritization of dengue via the WHO’s Global Strategy for Dengue Prevention and Control, 2012–2020.Citation6 The overall goal of this multi-sectoral strategy is ‘to reduce the burden of dengue’.Citation6 The document also defines objectives, technical elements, and enabling factors for effective implementation such as advocacy, partnership, coordination, and collaboration. The need to gain improved dengue disease burden estimates is one of three key objectives identified for dengue control with a timeframe for completion of 2015. More accurate epidemiological and surveillance data will enable further political prioritization for the currently ‘neglected’ disease.Citation6 It would also enable improved decision making and rational allocation of financial, research, and other resources to the areas of greatest need.Citation6,Citation13 For example, epidemiological data will be essential in planning funding, allocation, and distribution of dengue vaccines that could potentially become available in the next decade.Citation6,Citation19
Sustainable vector control is one technical element of the Global Strategy for Dengue Prevention and Control, 2012–2020.Citation6 In light of limited therapeutic strategies and the current lack of a vaccine, effective vector control methods are an essential component of the strategic direction to reduce dengue mortality and morbidity by 2020.Citation6,Citation19 Integrated Vector Management (IVM) is the strategic approach promoted to countries by the WHO as a rational, cost-effective, and optimal decision-making process for vector control programs.Citation6,Citation84 For dengue vectors, this involves using a combination of approaches incorporating key elements of social mobilization, integration of chemical and non-chemical control methods targeting areas of high human-vector contact, evidence based decision-making guiding research and policy, as well as capacity building.Citation84 Utilizing an effective integrated vector control strategy will aid in reduction of dengue transmission and the resulting disease burden.
Some researchers suggest dengue prioritization has now evolved and query how long it will be classified a ‘neglected’ disease.Citation73,Citation82 Furthermore, the impact of dengue has now progressed beyond those living in poverty as wealthier urbanized populations also have endemic dengue.Citation6,Citation73,Citation82,Citation85,Citation86 Whilst this expands the experience and relevance of dengue to a broader group, the resulting impact on dengue control and future epidemiology is currently unknown.Citation82 Irrespective, the poverty-promoting aspects of dengue, such as reduced economic potential with days off school and work, persist in the majority of dengue endemic settings.Citation34 Perhaps, with continued expansion alongside improved epidemiological information, further prioritization and coordination of resources will be encouraged and we may see the objectives of the WHO ‘Global Strategy’ met by 2020.
Conclusion
Dengue is now endemic in more than 125 countries globally.Citation5,Citation31 Reasons for the currently observed and predicted expansion are multifactorial. They may include climate change, virus evolution, and societal factors such as rapid urbanization, population growth and development, socioeconomic factors, as well as global travel and trade.Citation23,Citation52
There is no antiviral therapy or vaccination available for dengue at this time, leaving only early detection and symptomatic treatment with fluid resuscitation essential for management of severe cases.Citation19 As a result of limited therapeutic strategies, effective vector control methods are essential and are therefore promoted globally by the WHO through the strategic approach of IVM.Citation6,Citation84 For dengue, this approach targets the Aedes genus of mosquito in settings where high levels of human-vector contact occur.Citation84 The WHO Global Strategy for Dengue Prevention and Control, 2012–2020, highlights the need for improved estimates of the true burden of dengue disease globally due to the currently presumed under-representation.Citation6 Surveillance and reporting is paramount for effective dengue control, and more accurate quantification of the impact of dengue globally will allow improved political, financial, and research prioritization as well as informed decision making and enhanced modeling.Citation2,Citation18,Citation40,Citation43,Citation87
The known social, economic, and disease burden of dengue internationally is alarming and it is evident that the wider impact of this disease is grossly underestimated.Citation2,Citation29 An international multi-sectoral response, such as that outlined in the WHO Global Strategy for Dengue Prevention and Control, 2012–2020, is now essential to reduce the significant influence this disease projects globally.Citation6
Disclosure
The authors report no conflicts of interest in this work.
References
- GuzmanMGKouriGDengue: an updateLancet Infect Dis200221334211892494
- GublerDJDengue, Urbanization and Globalization: The Unholy Trinity of the 21(st) CenturyTrop Med Health201139Suppl 431122500131
- GublerDJThe global emergence/resurgence of arboviral diseases as public health problemsArch Med Res200233433034212234522
- WHO TDR Global Alert and Repsonse Dengue/Dengue Haemorrhagic Fever [webpage on the Internet]GenevaWorld Health Organization (WHO)2013 [cited March 3, 2013]. Available from: http://www.who.int/csr/disease/dengue/en/index.html
- Dengue and severe dengue: Fact Sheet No 117 [webpage on the Internet]GenevaWorld Health Organization (WHO)2012 [cited March 4, 2013]. Available from: http://www.who.int/mediacentre/factsheets/fs117/en/index.html
- World Health Organization (WHO)Global Strategy for Dengue Prevention and Control, 2012–2020GenevaWHO Press2012
- International Travel and Health DENGUE [webpage on the Internet]GenevaWorld Health Organization (WHO)2013 [cited March 5, 2013]; Available from: http://www.who.int/ith/diseases/dengue/en/index.html
- WHO Regional Office for South-East AsiaComprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever, Revised and Expanded EditionNew DelhiWorld Health Organisation South East Asia Regional Office2011
- HalsteadSBEtiologies of the experimental dengues of Siler and SimmonsAm J Trop Med Hyg19742359749824615598
- Wilder-SmithAOoiEEVasudevanSGGublerDJUpdate on dengue: epidemiology, virus evolution, antiviral drugs, and vaccine developmentCurr Infect Dis Rep201012315716421308524
- GibbonsRVVaughnDWDengue: an escalating problemBMJ200232473531563156612089096
- GublerDJSatherGEKunoGCabralJRDengue 3 virus transmission in AfricaAm J Trop Med Hyg1986356128012843789276
- AmarasingheAKuritskJNLetsonGWMargolisHSDengue virus infection in AfricaEmerg Infect Dis20111781349135421801609
- Rigau-PerezJGClarkGGGublerDJReiterPSandersEJVorndamAVDengue and dengue haemorrhagic feverLancet199835291329719779752834
- CaoXTNgoNTWillsBEvaluation of the World Health Organization standard tourniquet test and a modified tourniquet test in the diagnosis of dengue infection in Viet NamTrop Med Int Health2002712513211841702
- EndyTPAndersonKBNisalakADeterminants of inapparent and symptomatic dengue infection in a prospective study of primary school children in Kamphaeng Phet, ThailandPLoS Negl Trop Dis201153e97521390158
- Wilder-SmithAFooWEarnestASremulanathanSPatonNISeroepidemiology of dengue in the adult population of SingaporeTrop Med Int Health20049230530815040570
- GublerDJThe economic burden of dengueAm J Trop Med Hyg201286574374422556068
- WHODengue: Guidelines for Diagnosis, Treatment, Prevention and Control New edition 2009GenevaWorld Health Organization2009
- MorrisonACZielinski-GutierrezEScottTWRosenbergRDefining challenges and proposing solutions for control of the virus vector Aedes aegyptiPLoS Med200853e6818351798
- HawleyWAThe biology of Aedes albopictusJ Am Mosq Control Assoc Suppl198811393068349
- GublerDJClarkGGDengue/dengue hemorrhagic fever: the emergence of a global health problemEmerg Infect Dis19951255578903160
- Wilder-SmithAGublerDJGeographic expansion of dengue: the impact of international travelMed Clin N Am20089261377139019061757
- MammenMPPimgateCKoenraadtCJSpatial and temporal clustering of dengue virus transmission in Thai villagesPLoS Med2008511e20518986209
- GublerDJDengue/dengue haemorrhagic fever: history and current statusNovartis Found Symp200627731617319151
- GublerDDengue and Dengue Hemorrhagic FeverClin Microbiol Rev19981134804969665979
- GublerDJDengue and Dengue Hemorrhagic Fever: Its History and Resurgence as a Global Public Health ProblemGublerDJKunoGDengue and Dengue Hemorrhagic FeverLondonCAB International1997122
- GublerDJEpidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st centuryTrend Microbiol2002102100103
- ShepardDSCoudevilleLHalasaYAZambranoBDayanGHEconomic impact of dengue illness in the AmericasAm J Trop Med Hyg201184220020721292885
- Global Alert and Response – Impact of DengueGenevaWorld Health Organization (WHO)2013 Available from: http://www.who.int/csr/disease/dengue/impact/en/
- FerreiraGLGlobal dengue epidemiology trendsRev Inst Med Trop Sao Paulo201254Suppl 18S5S623011450
- Dengue, countries or areas at risk, 2011GenevaWorld Health Organization (WHO)2012 Available from: http://gamapserver.who.int/mapLibrary/Files/Maps/Global_DengueTransmission_ITHRiskMap.pngAccessed July 30, 2013
- CattandPGuzmánMGJanninJTropical Diseases Lacking Adequate Control Measures: Dengue, Leishmaniasis, and African TrypanosomiasisJamisonDTBremanJGMeashamARDisease Control Priorities in Developing Countries2nd edNew YorkOxford University Press2006451466
- HotezPJFenwickASavioliLMolyneuxDHRescuing the bottom billion through control of neglected tropical diseasesLancet20093731570157519410718
- HammondSNBalmasedaAPerezLDifferences in dengue severity in infants, children, and adults in a 3-year hospital-based study in NicaraguaAm J Trop Med Hyg20057361063107016354813
- EggerJRColemanPGAge and clinical dengue illnessEmerg Infect Dis200713692492517553238
- KittigulLPitakarnjanakulPSujiraratDSiripanichgonKThe differences of clinical manifestations and laboratory findings in children and adults with dengue virus infectionJ Clin Virol2007392768117507286
- GuzmanMGKouriGBravoJValdesLVazquezSHalsteadSBEffect of age on outcome of secondary dengue 2 infectionsInt J Infect Dis20026211812412121599
- Díaz-QuijanoFAWaldmanEAFactors associated with dengue mortality in Latin America and the Caribbean, 1995–2009: an ecological studyAm J Trop Med Hyg20118632833422302870
- ShepardDSUndurragaEAHalasaYAEconomic and disease burden of dengue in Southeast AsiaPLoS Negl Trop Dis201372e205523437406
- BeattyMEBeutelsPMeltzerMIHealth economics of dengue: a systematic literature review and expert panel’s assessmentAm J Trop Med Hyg201184347348821363989
- BradyOJGethingPWBhattSRefining the global spatial limits of dengue virus transmission by evidence-based consensusPLoS Negl Trop Dis201268e176022880140
- BhattSGethingPWBradyOJThe global distribution and burden of dengueNature201349650450723563266
- ArimaYMatsuiuTEpidemiologic update of dengue in the western Pacific region, 2010Western Pac Surveill Response J20112215
- San MartinJLBrathwaiteOZambranoBThe epidemiology of dengue in the Americas over the last three decades: a worrisome realityAm J Trop Med Hyg201082112813520065008
- GuzmanMGHalsteadSBArtsobHDengue: a continuing global threatNat Rev Microbiol20108Suppl 12S7S1621079655
- FrancoLDi CaroACarlettiFRecent expansion of dengue virus serotype 3 in West AfricaEuro Surveill2010157
- Outbreak Notice – Dengue in Madeira, Portugal [webpage on the Internet]Atlanta, GACenters for Disease Control and Prevention (CDC)2013 [cited March 9, 2013]. Available from: http://wwwnc.cdc.gov/travel/notices/outbreak-notice/dengue-madeira-portugal.htm
- Epidemiological update: Outbreak of dengue in Madeira, Portugal [webpage on the Internet]StockholmEuropean Centre for Disease Prevention and Control (ECDC)2013 [cited March 7, 2013]. Available from: http://www.ecdc.europa.eu/en/press/news/Lists/News/ECDC_DispForm.aspx?List=32e43ee8-e230-4424-a783-85742124029a&ID=845&RootFolder=%2Fen%2Fpress%2Fnews%2FLists%2FNews
- RasheedSBButlinRKBootsMA review of dengue as an emerging disease in PakistanPublic Health20131271111723219263
- KhanMAEllisEMTisseraHAEmergence and diversification of dengue 2 cosmopolitan genotype in Pakistan, 2011PloS One201383e5639123520453
- AstromCRocklovJHalesSBeguinALouisVSauerbornRPotential distribution of dengue fever under scenarios of climate change and economic developmentEcohealth20129444845423408100
- HalesSde WetNMaindonaldJWoodwardAPotential effect of population and climate changes on global distribution of dengue fever: an empirical modelLancet2002360933683083412243917
- Rico-HesseRMicroevolution and virulence of dengue virusesAdv Virus Res20035931534114696333
- WangENiHXuREvolutionary relationships of endemic/epidemic and sylvatic dengue virusesJ Virol20007473227323410708439
- ReiterPClimate change and mosquito-borne diseaseEnviron Health Perspect2001109Suppl 114116111250812
- GublerDJReiterPEbiKLYapWNasciRPatzJAClimate variability and change in the United States: potential impacts on vector- and rodent-borne diseasesEnviron Health Perspect2001109Suppl 222323311359689
- PatzJAReisenWKImmunology, climate change and vector-borne diseasesTrends Immunol200122417117211274908
- EarnestATanSBWilder-SmithAMeteorological factors and El Nino Southern Oscillation are independently associated with dengue infectionsEpidemiol Infect201214071244125121906411
- WuPCGuoHRLungSCLinCYSuHJWeather as an effective predictor for occurrence of dengue fever in TaiwanActa Trop20071031505717612499
- HiiYLRocklovJNgNTangCSPangFYSauerbornRClimate variability and increase in intensity and magnitude of dengue incidence in SingaporeGlob Health Action20092
- Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate ChangeClimate Change 2007: The Physical Science BasisCambridge, New YorkCambridge University Presss2007
- ReiterPYellow fever and dengue: a threat to Europe?Euro Surveill201015101950920403310
- BanuSHuWHurstCTongSDengue transmission in the Asia-Pacific region: impact of climate change and socio-environmental factorsTrop Med Int Health201116559860721320241
- SouzaSSSilvaIGSilvaHHAssociation between dengue incidence, rainfall and larval density of Aedes aegypti, in the State of GoiásRev Soc Bras Med Trop201043215215520464144
- RussellRCCurrieBJLindsayMDMackenzieJSRitchieSAWhelanPIDengue and climate change in Australia: predictions for the future should incorporate knowledge from the pastMed J Aust2009190526526819296793
- Van KleefEBambrickHHalesSThe geographic distribution of dengue fever and the potential influence of global climate changeTropIKA.net[serial on the Internet]352013http://www.tropika.net/svc/review/Chinnock-20110328-Review-Dengue-Climate
- BeebeNWCooperRDMottramPSweeneyAWAustralia’s dengue risk driven by human adaptation to climate changePLoS Negl Trop Dis200935e42919415109
- SutherstRWGlobal change and human vulnerability to vector-borne diseasesClin Microbiol Rev200417113617314726459
- GardnerLMFajardoDWallerSTWangOSarkarSA predictive spatial model to quantify the risk of air-travel-associated dengue importation into the United States and europeJ Trop Med2012201210367922523497
- NapoliCSalcuniPPompaMGDeclichSRizzoCEstimated imported infections of Chikungunya and Dengue in Italy, 2008 to 2011J Travel Med201219529429722943269
- ReiterPAedes albopictus and the world trade in used tires, 1988–1995: the shape of things to come?J Am Mosq Control Assoc199814183949599329
- MulliganKElliottSJSchuster-WallaceCThe place of health and the health of place: dengue fever and urban governance in Putrajaya, MalaysiaHealth Place201218361362022310527
- MendoncaHFFerreiraALSantosCBBreeding sites of Aedes aegypti in metropolitan vacant lots in Greater Vitoria, State of Espirito Santo, BrazilRev Soc Bras Med Trop201144224324621552743
- PadmanabhaHDurhamDCorreaFDiuk-WasserMGalvaniAThe interactive roles of Aedes aegypti super-production and human density in dengue transmissionPLoS Negl Trop Dis201268e179922953017
- RellerMEBodinayakeCNagahawatteAUnsuspected dengue and acute febrile illness in rural and semi-urban southern Sri LankaEmerg Infect Dis20121825626322304972
- VongSKhieuVGlassODengue incidence in urban and rural Cambodia: results from population-based active fever surveillance, 2006–2008PLoS Negl Trop Dis20104e90321152061
- BrunkardJMRobles LopezJLRamirezJDengue fever seroprevalence and risk factors, Texas-Mexico border, 2004Emerg Infect Dis200713101477148318257990
- BrunkardJMCifuentesERothenbergSJAssessing the roles of temperature, precipitation, and ENSO in dengue re-emergence on the Texas-Mexico border regionSalud Publica Mex200850322723418516370
- RamosMMMohammedHZielinski-GutierrezEEpidemic dengue and dengue hemorrhagic fever at the Texas-Mexico border: results of a household-based seroepidemiologic survey, Dec 2005Am J Trop Med Hyg200878336436918337327
- ClarkGGDengue and dengue hemorrhagic fever in northern Mexico and south Texas: do they really respect the border?Am J Trop Med Hyg200878336136218337325
- AdamsPDengue: neglected no more?TropIKA.net [serial on the Internet]12011 [cited May 24, 2013]http://www.tropika.net/svc/review/Adams-20110110_Review_Dengue_2
- WHO TDR Neglected Tropical Disease Research [webpage on the Internet]GenevaWorld Health Organization (WHO)2013 [cited May 24, 2013]. Available from: http://www.who.int/tdr/research/ntd/en/
- Dengue Control – Control Strategies [webpage on the Internet]GenevaWorld Health Organization (WHO)2013 [cited March 2, 2013]. Available from: http://www.who.int/denguecontrol/control_strategies/en/
- CapraraALimaJWMarinhoACCalvasinaPGLandimLPSommerfeldJIrregular water supply, household usage and dengue: a bio-social study in the Brazilian NortheastCad Saude Publica200925Suppl 1S125S13619287857
- CanyonDVHistorical analysis of the economic cost of dengue in AustraliaJ Vect Borne Dis200845245248
- BeattyMEStoneAFitzsimonsDWBest practices in dengue surveillance: a report from the Asia-Pacific and Americas Dengue Prevention BoardsPLoS Negl Trop Dis2010411e89021103381